Abstract
OBJECTIVES
The use of an open vein harvesting (OVH) technique for saphenous vein harvesting (SVH) is associated with wound complications and delayed patient mobilization. This has led to the development of minimally invasive vein harvesting (MIVH) techniques, such as standard bridging and endoscopic SVH (EVH). This randomized trial was established to assess immediate clinical outcome and patient satisfaction in our centre.
METHODS
A total of 150 consecutive patients were prospectively randomized into three groups. Group 1 consisted of 50 patients who underwent OVH, Group 2 consisted of 50 patients who underwent a standard bridging technique (SBT) and Group 3 consisted of 50 patients who underwent EVH. Each group was assessed for the incidence of wound infection, postoperative pain and satisfaction and the number of vein repairs using previously validated scoring systems.
RESULTS
The MIVH techniques reduced the pain at hospital (P < 0.001) and at 6 weeks (P < 0.001), and improved cosmesis (P < 0.001), compared with the OVH group. Patient satisfaction was greatest in the EVH group followed by the SBT and then the OVH group. The clinical markers of inflammation were reduced with an MIVHt. There were more vein repairs in the EVH compared with the OVH (P < 0.001) and the SBT (P = 0.04) groups.
CONCLUSIONS
This study demonstrates that MIVH reduces wound morbidity. We believe that each technique has advantages and disadvantages, which should be considered during the selection of a harvesting procedure by both the patient and the surgeon.
Keywords: Coronary artery bypass, Saphenous vein, Minimally invasive, Tissue and organ harvesting/adverse effects, Tissue and organ harvesting/methods, Wound healing
INTRODUCTION
Coronary artery disease is a major cause of morbidity and mortality [1]. There is currently no consensus regarding the type of graft used for coronary artery bypass grafting (CABG) and the optimum harvesting technique. The great saphenous vein (GSV) remains one of the most commonly used conduits due to its ease of harvest, availability and versatility [2]. However, the open vein harvesting (OVH) technique, which involves an extended leg incision, is associated with a significant morbidity [3]. Minimally invasive (MIVH) techniques, including the standard bridging technique (SBT) and endoscopic vein harvesting (EVH), have therefore been developed to reduce post-CABG leg wound complications. The SBT involves frequent short incisions along the length of the vein [4] rather than a single continuous incision, whereas the EVH uses CO2 inflation and an endoscope to remove the GSV via a single small incision. Although the long-term graft patency following EVH has been questioned [5], the other large cohort studies have reported that the technique is safe [6] and effective. This randomized study aimed to assess postoperative pain, wound healing, patient satisfaction, cosmesis and length of the hospital stay in each vein harvesting group.
MATERIALS AND METHODS
One hundred and fifty patients listed for CABG at the University Hospital of South Manchester were prospectively enrolled. Computer block randomization assigned the patients to undergo an EVH (n = 50), OVH (n = 50) or SBT (n = 50). Other minimally invasive techniques, such as the Mayo stripper, were not assessed as our centre has not adopted this procedure. The assignment number was concealed in an envelope separately for each patient. The exclusion criteria included redo-CABG, emergency surgery or a contraindication to a technique, including GSV varicosities, small legs and a superficial GSV. All patients were operated on by a single surgical care practitioner, with previous experience of >1000 procedures using the OVH, >500 with the SBT and 20 of EVH. All patients were prepared using Alcoholic Iodine (Ecolab UK Ltd) as a perioperative skin preparation. Wound assessment was completed daily by a wound specialist nurse and a research team for the first 5 days, at discharge and at 6 weeks. All patients were appropriately informed and they provided written consent. This study was approved by the National Research Ethics Committee.
Pain assessment
Leg pain was assessed daily at rest and movement before analgesia, using the Likert pain rating scale ranging from 0 (no pain) to 10 (unbearable pain) [7]. An analgesic dose was also recorded.
Wound healing assessment
Wound healing was rated using a modified Asepsis score system [8]. Erythema, exudates, bruising, wound approximation and haematoma were recorded from Day 2 after the dressing and bandages were removed. A clinical infection was recorded and graded for leg incisions; the assessment criteria included positive wound cultures and antibiotic prescription following a clinical diagnosis of infection. Patients were monitored following discharge by a telephone interview regarding general practitioner (GP) visits and district nurse referrals.
Saphenous neuropathy
The incidence of numbness around the wound site was assessed by a research team at Week 6. A tactile sensation was assessed via the use of soft cotton wool and a pointed needle for exaggerated pain sensitivity [4].
Patient satisfaction
Patient satisfaction with the wound appearance was recorded using a visual analogue scale at 6 weeks [9]. Patients rated their satisfaction with overall wound appearance on a 100-mm line, with 100 mm indicating complete satisfaction. Patients rated their appearance with regards to colour, size and visibility of the scar.
Cosmetic appearance of the scar
The cosmetic appearance of the scar was assessed by a research team using a Hollander scale (step-off borders, contour irregularities, margin separation, edge inversion and excessive distortion) during the hospital stay. The scarring and cosmetic outcome were measured by a blinded specialist nurse using a modified patient and observer scar assessment scale (POSAS).
SURGICAL METHODS
Open vein harvesting
The GSV was identified two fingers proximal to the medial malleolus according to the standard practice. The OVH technique is not performed in the thigh due to the increased difficulty of finding the vein and increased adipose tissue. The vein was harvested using metzenbaum scissors, and a continuous incision was made along the route of the vein. Care was taken not to traumatize the nerve, vein or its branches. Vein branches were ligated with 4-0 vicryl ties (Ethicon, J&J Medical Ltd, USA) and titanium clips. For each harvesting technique, the wound was closed in layers with continuous 2-0 polysorb sutures (Coviden Ltd, UK) and 3-0 skin sutures. The wound was covered with Opsite postoperative dressing. A pressure bandage was applied for 24–48 h according to the local protocol.
Bridging
A 2 to 3-cm longitudinal incision was made proximal to the medial malleolus and the GSV was identified according to the standard practice. As with the OVH technique, the SBT is not performed in the thigh due to the increased difficulty of finding the vein and increased adipose tissue. The vein was then exposed and dissected through tunnels using West and Langenbeck retractors (Anetic Aid, UK) with a 5 to 6-cm gap between incisions. Dissection was performed using Metzenbaum scissors and a vein hook; side branches were closed using titanium clips. Care was taken not to damage the saphenous nerve.
Endoscopic vein harvesting
The EVH was performed using the Vasoview Hemopro® system (Maquet). The vein was identified on the medial tibial border using a west retractor through a 2 cm incision just below the knee, as per the standard practice. It is significantly easier to harvest the vein conduits via EVH from the thigh due to the size and positioning of the endoscopic equipment and hence the ease of access to the vein. Once the vein was identified, 5000-U IV Heparin was administered to avoid the intraluminal clot strand formation [10]. The incision site was sealed using a balloon port to create a tunnel inside the leg. CO2 insufflation was then commenced at 12 mmHg of pressure with a 3 l/min flow rate. A dissection tip cannula was introduced inside the tunnel to isolate the vein and its branches. A second unit with hemoprobe cautery was inserted via the port to cut and seal the tributary branches. A 1 cm skin incision was made near the groin to ligate the distal end of the LSV and remove the vein, which was checked for leakage. The branches were tied with 4-0 vicryl ties, and necessary repairs were performed using 7-0 prolene sutures.
Statistics
Results were analysed using SPSS 15.0. Non-parametric data were analysed using the Mann–Whitney U-test. The parametric data were analysed using the independent t-test. The discrete data were analysed with the χ2 test. The length of the hospital stay was analysed by the Kaplan–Meier survival test. P-values <0.05 were statistically significant.
RESULTS
Demographics
Patient demographics are displayed in Table 1. Owing to simple block randomization, there was a significant difference in age (P = 0.023) and gender (P = 0.025) between the groups. A significant difference was observed in the incidence of peripheral vascular disease between the groups (P < 0.001). Unfortunately, two patients died in hospital following CABG (one EVH and one SBT), but from causes unrelated to wound infection or myocardial infarction. Three EVH patients required a conversion to OVH technique, as a result of the loss of vision due to blood in the tunnel, and were excluded from the study. There was no difference in the mean number of vein grafts between the groups (P = 0.254).
Table 1:
Demographics of patients assigned to each group
| EVH | OVH | SBT | P-value | |
|---|---|---|---|---|
| Mean age (years) | 64.3 | 67.9 | 69.2 | 0.023 |
| Male (%) | 90 | 78 | 72 | 0.025 |
| Female (%) | 10 | 22 | 28 | |
| Diabetic [(diet) yes/no] | 1/49 | 1/49 | 4/46 | 0.127 |
| Diabetic [(tablet) yes/no] | 4/46 | 5/45 | 4/46 | 1.000 |
| Diabetic [(insulin) yes/no] | 5/45 | 6/44 | 11/39 | 0.091 |
| Mean body mass index (BMI) | 28.19 | 28.50 | 28.03 | 0.865 |
| Peripheral vascular disease (yes/no) | 1/49 | 5/45 | 14/36 | <0.001 |
| Surgery (CABG/CABG + other) | 49/1 | 48/2 | 50/0 | 0.202 |
CABG: coronary artery bypass grafting; EVH: endoscopic vein harvesting; OVH: open vein harvesting; SBT: standard bridging technique.
Postoperative pain
The OVH group was associated with greatest postoperative pain followed by EVH and then the SBT. The SBT and EVH had significantly reduced pain compared with the OVH group at Days 1 (P < 0.001) and 5 (P < 0.001) at rest and movement. By Week 6, this reduction in pain with the SBT and EVH was significant with movement only (P = 0.005 and <0.001, respectively) (Figs 1 and 2). The SBT reduced pain compared with EVH during the hospital stay (P = 0.010 and 0.004 at rest and movement on Day 1; P = 0.002 and 0.014 at rest and movement on Day 5, respectively), however, this benefit was lost after 6 weeks (P = 0.460 and 0.286, respectively).
Figure 1:
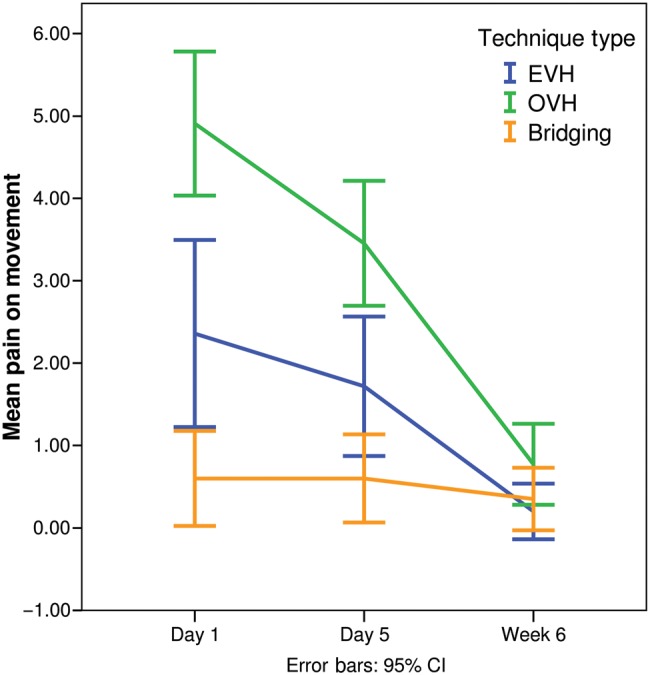
The effect of technique on the average pain with movement measured at Day 1, Day 5 and at the 6-week follow-up. EVH: endoscopic vein harvesting; OVH: open vein harvesting; SBT: standard bridging technique.
Figure 2:
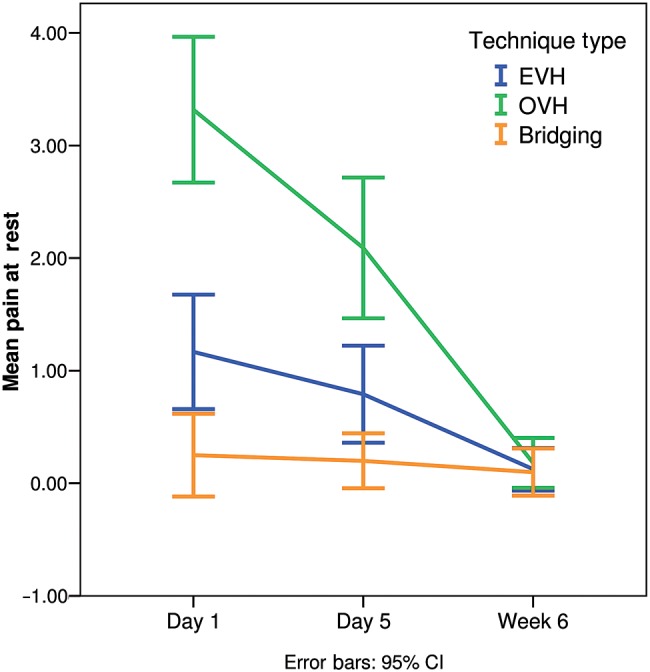
The effect of technique on the average rest pain measured at Day 1, Day 5 and at the 6-week follow-up. EVH: endoscopic vein harvesting; OVH: open vein harvesting; SBT: standard bridging technique.
Wound healing
Clinical markers of inflammation (exudates, erythema, bruising and haematoma) were elevated with the OVH group compared with the SBT and EVH (Table 2). Interestingly, the EVH induced greater haematoma formation than the other techniques (P < 0.001). All patients were heparinized for CABG without a drain insertion into the EVH tunnel, which contributed to the haematoma formation [11]. There was no significant difference in antibiotic prescription for clinically diagnosed wound infection between the groups (P = 0.318). There was only one confirmed culture positive infection in the study, occurring in the EVH group that required the evacuation of the surgical haematoma at the end of Week 1. No significant difference was observed in the incidence of numbness between the groups. However, the OVH group experienced greater hyperaesthesia at 6 weeks.
Table 2:
Inflammation markers measured between the groups
| EVH | OVH | SBT |
P-value |
||||
|---|---|---|---|---|---|---|---|
| Three-way comparison | EVH versus OVH | EVH versus SBT | OVH versus SBT | ||||
| Exudates none/serous/blood/pus | 50/0/0/0 | 38/12/0/0 | 7/0/43/0 | <0.001 | <0.001 | <0.001 | <0.001 |
| Erythema yes/no | 35/15 | 45/5 | 48/1 | <0.001 | 0.012 | <0.001 | 0.056 |
| Bruising none/bruising/haematoma | 26/12/12 | 24/25/1 | 40/8/2 | <0.001 | 0.204 | 0.001 | 0.006 |
EVH: endoscopic vein harvesting; OVH: open vein harvesting; SBT: standard bridging technique.
Patient satisfaction
Patient satisfaction at discharge was greatest with the EVH followed by the SBT and then the OVH group (P < 0.001) (Fig. 3). Collectively, the MIVH techniques resulted in greater patient satisfaction compared with OVH.
Figure 3:
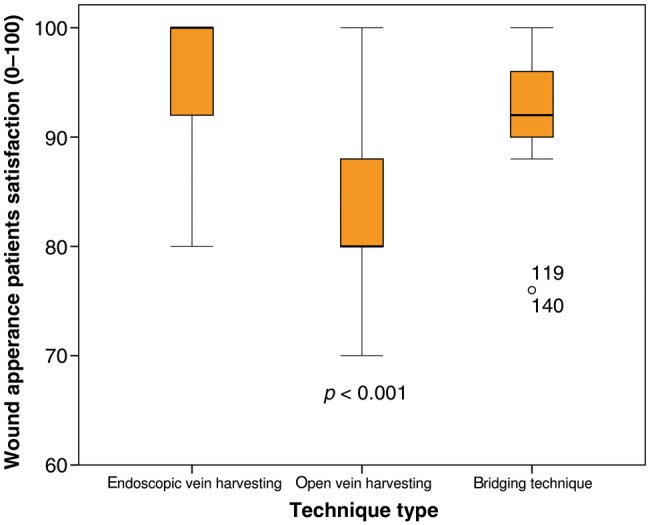
The change in satisfaction as measured by the visual analogue scale with the harvesting technique. The white circle represents outliers in the data set.
Cosmetic scarring
There was no significant difference using the Hollander scale during the hospital stay (P = 0.078). However, cosmetic scarring at 6 weeks was significantly improved (Fig. 4) in the MIVH groups compared with the OVH when assessed using a modification of the POSAS (P < 0.001).
Figure 4:
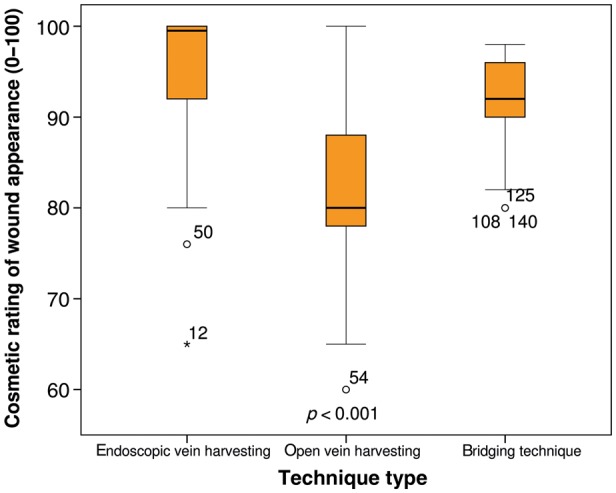
The cosmetic appearance of the scar between the three techniques. The white circles and asterisk represent outliers in the data set.
Hospital stay
There was a significant reduction in the length of hospital stay with EVH compared with the OVH (P = 0.002). However, there was no difference between the EVH and SBT (P = 0.128) or the SBT and OVH (P = 0.122). Wound infection accounted for a prolonged stay in only a single patient.
Vein repair
The OVH provided the highest vein quality, with no repairs required (Table 3). The number of vein repairs was greatest in the EVH group followed by the SBT group.
Table 3:
Clinical outcomes of each group
| EVH | OVH | SBT | P-value | |
|---|---|---|---|---|
| Number of vein grafts (mean) | 2.00 | 2.18 | 2.16 | 0.254 |
| Number of vein repairs (0/1/2) | 32/17/1 | 50/0/0 | 41/9/0 | 0.014 |
| Infection in hospital (yes/no) | 0/50 | 1/49 | 2/48 | 0.624 |
| GP visit (yes/no) | 7/42* | 11/39 | 7/49* | 0.651 |
| District nurse referral (yes/no) | 2/47* | 8/42 | 5/44* | 0.742 |
| Antibiotics given (yes/no) | 7/42* | 10/40 | 5/44* | 0.318 |
| Numbness (yes/no) | 1/48* | 10/40 | 2/47* | 0.780 |
GP: general practitioner; EVH: endoscopic vein harvesting; OVH: open vein harvesting; SBT: standard bridging technique. *Missing value is due to mortality prior to collection.
Operating time
The choice of the surgical technique significantly influenced the operation duration (P < 0.001). The average time for EVH was 0:42:13, OVH 0:51:59 and SBT 1:08:03.
General practitioner and district nurse visits
The frequency of GP visits or district nurse referrals did not vary between the groups (P = 0.651 and 0.742, respectively). A post-operative prescription of antibiotics was also equivalent between the groups (P = 0.318).
DISCUSSION
The use of the MIVH techniques improves wound healing and cosmesis. During the initial stages of wound healing, we observed more serous exudates in the OVH group, and more blood exudates in the SBT, compared with the EVH. There was a significant difference in erythema between the EVH and other groups. This is mainly due to the length and the frequency of incisions. This is reflected by improvement in cosmetic satisfaction with the EVH, which we regard as highly important.
Pain was also significantly lower in the MIVH groups compared with the OVH group, in concordance with previous findings [12]. This reduction is conducive to the increased mobilization and the quality of life, contributing to an improved patient satisfaction [13]. An improved mobilization also shortens the duration of mechanical ventilation in the ICU and ultimately reduces hospitalization [14], potentially explaining the reduced length of the hospital stay with the EVH.
An immediate satisfaction is important when assessing the vein harvesting techniques; however, the conduit quality and the prognostic implications must be the primary outcome. The EVH required more frequent vein repairs than the SBT or OVH technique. The MIVH techniques reduce visualization of the graft and are more technically complex, potentially leading to reduced vessel integrity. Given the recent findings by Lopes et al. [5] that EVH may be associated with reduced graft patency, this represents a potentially important finding. Yet, another large cohort study reported no midterm effect on mortality associated with EVH [6]. Although the SBT was associated with more minor repairs than the OVH technique, it has more thorough long-term follow-up and equivalent long-term outcomes [15]. This indicates that reduced vessel integrity and subsequent vein repair does not impact on the clinical outcome, although the formal histological assessment of this is clearly required.
Acknowledging the learning curve associated with EVH and providing enhanced training will potentially lead to greater vein quality. We aim to assess this in a formal EVH training study.
The limitations of this study are the small sample size and the lack of statistical power, due to the pilot nature of the work, which represents the initial findings of a large randomized study between these three groups. Also, the practitioner did not have much experience with EVH compared with the other groups. However, significant benefits were still observed, despite the lack of experience.
In conclusion, an MIVH is associated with reduced pain and improved patient satisfaction compared with the OVH technique. Of the MIVH techniques, EVH is associated with increased satisfaction and significantly reduced the length of hospital stay compared with the OVH group. However, patients undergoing the SBT have less pain in the early postoperative period compared with EVH. The OVH technique has the greatest long-term follow-up data indicating no problems with long-term patency and was associated with the least vein repairs in this cohort. We believe each technique has advantages and disadvantages that should be considered during procedure selection by both the patient and the clinician.
Funding
The study was funded by the local NHS Research and Development Directorate at the University Hospital of South Manchester.
Conflict of interest: none declared.
REFERENCES
- 1.Allender S, Peto V, Scarborough P, Kaur A, Rayner M. Coronary Heart Disease Statistics. Oxford: British Heart Foundation. 2008:12–42. [Google Scholar]
- 2.Raja SG, Haider Z, Ahmad M, Zaman H. Saphenous vein grafts: to use or not to use? Heart Lung Circ. 2004;13:403–9. doi: 10.1016/j.hlc.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Athanasiou T, Aziz O, Skapinakis P, Perunovic B, Hart J, Crossman MC, et al. Leg wound infection after coronary artery bypass grafting: a meta-analysis comparing minimally invasive versus conventional vein harvesting. Ann Thorac Surg. 2003;76:2141–6. doi: 10.1016/s0003-4975(03)01435-8. [DOI] [PubMed] [Google Scholar]
- 4.Khan UA, Krishnamoorthy B, Najam O, Waterworth P, Fildes JE, Yonan N. A comparative analysis of saphenous vein conduit harvesting techniques for coronary artery bypass grafting—standard bridging versus the open technique. Interact Cardiovasc Thorac Surg. 2010;10:27–31. doi: 10.1510/icvts.2009.209171. [DOI] [PubMed] [Google Scholar]
- 5.Lopes RD, Hafley GE, Allen KB, Ferguson TB, Peterson ED, Harrington RA, et al. Endoscopic versus open vein-graft harvesting in coronary-artery bypass surgery. N Engl J Med. 2009;361:235–44. doi: 10.1056/NEJMoa0900708. [DOI] [PubMed] [Google Scholar]
- 6.Ouzounian M, Hassan A, Buth KJ, MacPherson C, Ali IM, Hirsch GM, et al. Impact of endoscopic versus open saphenous vein harvest techniques on outcomes after coronary artery bypass grafting. Ann Thorac Surg. 2010;89:403–8. doi: 10.1016/j.athoracsur.2009.09.061. [DOI] [PubMed] [Google Scholar]
- 7.Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37:378–81. doi: 10.1136/ard.37.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson AP, Weavill C, Burridge J, Kelsey MC. The use of the wound scoring method ‘ASEPSIS’ in postoperative wound surveillance. J Hosp Infect. 1990;16:297–309. doi: 10.1016/0195-6701(90)90002-6. [DOI] [PubMed] [Google Scholar]
- 9.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–36. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 10.Brown EN, Kon ZN, Tran R, Burris NS, Gu J, Laird P, et al. Strategies to reduce intraluminal clot formation in endoscopically harvested saphenous veins. J Thorac Cardiovasc Surg. 2007;134:1259–65. doi: 10.1016/j.jtcvs.2007.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krishnamoorthy B, Al-Fagih OS, Madi MI, Najam O, Waterworth PD, Fildes JE, et al. Closed suction drainage improves clinical outcome in patients undergoing endoscopic vein harvesting for coronary artery bypass grafting. Ann Thorac Surg. 2012;93:1201–5. doi: 10.1016/j.athoracsur.2011.12.060. [DOI] [PubMed] [Google Scholar]
- 12.Tennyson C, Young CP, Scarci M. Is it safe to perform endoscopic vein harvest? Interact CardioVasc Thorac Surg. 2010;10:625–9. doi: 10.1510/icvts.2009.227090. [DOI] [PubMed] [Google Scholar]
- 13.Jamison RN, Ross MJ, Hoopman P, Griffin F, Levy J, Daly M, et al. Assessment of postoperative pain management: patient satisfaction and perceived helpfulness. Clin J Pain. 1997;13:229–36. doi: 10.1097/00002508-199709000-00008. [DOI] [PubMed] [Google Scholar]
- 14.O'Connor ED, Walsham J. Should we mobilise critically ill patients? A review. Crit Care Resusc. 2009;11:290–300. [PubMed] [Google Scholar]
- 15.Aziz O, Athanasiou T, Panesar SS, Massey-Patel R, Warren O, Kinross J, et al. Does minimally invasive vein harvesting technique affect the quality of the conduit for coronary revascularization? Ann Thorac Surg. 2005;80:2407–14. doi: 10.1016/j.athoracsur.2005.04.009. [DOI] [PubMed] [Google Scholar]


