Abstract
Objective:
To estimate the prevalence of sleep problems and the effect of potential correlates in low-income settings from Africa and Asia, where the evidence is lacking.
Design:
Cross-sectional.
Setting:
Community-wide samples from 8 countries across Africa and Asia participating in the INDEPTH WHO-SAGE multicenter collaboration during 2006-2007. The participating sites included rural populations in Ghana, Tanzania, South Africa, India, Bangladesh, Vietnam, and Indonesia, and an urban area in Kenya.
Participants:
There were 24,434 women and 19,501 men age 50 yr and older.
Interventions:
N/A.
Measurements and Results:
Two measures of sleep quality, over the past 30 days, were assessed alongside a number of sociodemographic variables, measures of quality of life, and comorbidities. Overall, 16.6% of participants reported severe/extreme nocturnal sleep problems, with a striking variation across the 8 populations, ranging from 3.9% (Purworejo, Indonesia and Nairobi, Kenya) to more than 40.0% (Matlab, Bangladesh). There was a consistent pattern of higher prevalence of sleep problems in women and older age groups. In bivariate analyses, lower education, not living in partnership, and poorer self-rated quality of life were consistently associated with higher prevalence of sleep problems (P < 0.001). In multivariate logistic regression analyses, limited physical functionality or greater disability and feelings of depression and anxiety were consistently strong, independent correlates of sleep problems, in both women and men, across the 8 sites (P < 0.001).
Conclusions:
A large number of older adults in low-income settings are currently experiencing sleep problems, which emphasizes the global dimension of this emerging public health issue. This study corroborates the multifaceted nature of sleep problems, which are strongly linked to poorer general well-being and quality of life, and psychiatric comorbidities.
Citation:
Stranges S; Tigbe W; Gómez-Olivé FX; Thorogood M; Kandala NB. Sleep problems: an emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. SLEEP 2012;35(8):1173–1181.
Keywords: Sleep, aging, quality of life, comorbidities, correlates, epidemiology, global health
INTRODUCTION
There is growing evidence, mostly from populations in Western countries,1–10 pointing to downward trends in the average duration of sleep and increasingly higher prevalence of insomnia and other sleep disturbances. For example, data from nationwide surveys in Canada and the United States indicate that more than 20% of the general adult population suffer from insomnia, and this number is likely to increase over the next few decades.2,3 These percentages are consistent with prevalence figures of short sleep duration reported in population-based studies across different Western countries over the past 3 decades.4,6,7,8,9–10 More broadly, problems with falling asleep or daytime sleepiness and fatigue affect even larger segments of the population, imposing a considerable burden in terms of morbidity and mortality outcomes, as well as substantial cost implications for society in developed settings.11–13
It is well known that many populations from low-income countries are undergoing a rapid demographic and epidemiologic transition.14,15 These countries are facing multiple disease burdens with an unfinished agenda of undernutrition, a high burden of infectious disease, and an emerging burden of noncommunicable diseases. Sleep problems might represent an unrecognized public health issue in many developing countries, especially among older adults, given the ongoing aging of the population at the global level.16 However, evidence on the burden of sleep problems in low-income settings is lacking.
The publicly available data from the International Network for the Demographic Evaluation of Populations and Their Health (INDEPTH) and the World Health Organization (WHO) Study on Global Ageing and Adult Health (SAGE) multicenter collaboration on global aging and adult health (http://www.globalhealthaction.net/index.php/gha/article/view/5302) offers a unique opportunity to fill this gap by examining the prevalence of sleep problems among adults age 50 yr and older in 8 countries from Africa and Asia.17,18 Sleep habits are multifaceted and result from a complex interplay between genetics, environment, and social factors, as well as the presence of comorbidities.5,8,9,19 Factors contributing to sleep problems in older adults from low-income countries may differ from those characteristic of Western societies.19–21 We report the relationship of sleep problems with a number of potential correlates including sociodemographic variables, measures of quality of life, and comorbidities in 8 countries from Africa and Asia.
METHODS
Study Population
The study is based on the INDEPTH WHO-SAGE study. The study background has been described in detail in previous reports.17,18 This multicenter INDEPTH WHO-SAGE study was conducted during 2006–2007 in 8 Health and Demographic Surveillance System (HDSS) sites in Africa and Asia: Agincourt (South Africa), Ifakara (Tanzania), Nairobi (Kenya), Navrongo (Ghana), Filabavi (Vietnam), Matlab (Bangladesh), Purworejo (Indonesia), and Vadu (India).
Except for 1 (Nairobi, Kenya), all centers cover rural populations that are reasonably typical of their locations. The HDSS sites were selected to include different geographic and socioeconomic contexts. A total of 93,347 individuals age 50 yr and older were identified from the surveillance databases across all 8 field sites. In 6 sites, all adults 50 yr and older were targeted for a face-to-face interview; in the other 2 sites (Navrongo and Matlab) a random sample of households with at least 1 member age 50 yr and older was selected. Older individuals had a known nonzero probability of selection. A total of 58,004 respondents age 50 yr and older were invited to participate and the overall response rate was 80%, resulting in a final total sample of 46,269, ranging from 2,072 in Nairobi to 12,395 in Purworejo. A total of 2,334 respondents (5.0%) were later excluded from the analysis because of incomplete sociodemographic information (item nonresponse: age [n = 11]; education [n = 450]; socioeconomic status [n = 1,627]; marital status [n = 121]; living arrangements [n = 125]), leaving a total sample of 43,935 for the current analysis.
Data Collection and Measurements
The study questionnaire was developed through a consultative process between INDEPTH and WHO-SAGE with the goal of integrating a feasible number of useful SAGE modules into routine surveillance update activities with minimum effect on existing HDSS procedures. It included questions on self-health assessment, physical functionality, sleep and energy, depression and anxiety, well-being, and quality of life. The questionnaire was translated and backtranslated into 8 local languages. Standardized training, interview protocols, and quality assurance procedures were used across all participating sites. Centralized training was provided to principal investigators from each site, who in turn trained their respective survey teams. Site-based training averaged 4.5 days in duration across the sites. Mean interview time was 20 min. Three sites integrated the INDEPTH WHO-SAGE module into their routine HDSS surveillance, whereas the remaining 5 sites conducted the INDEPTH WHO-SAGE study as a separate data collection activity. Detailed descriptions of instruments, survey protocols, and quality control measures have been described in previous reports.17,18
A number of potential correlates of sleep problems, which were identified in the published literature,5,8,9 were selected for the current analysis. Age at interview was calculated from the recorded date of birth or the self-reported age, and categorized in 4 groups, 50-59, 60-69, 70-79, and 80 yr and older. Education was categorized according to the WHO levels: no formal education; less than 6 yr of formal education; and 6 yr or more of formal education. Marital status was categorized into 2 groups: (1) currently married or living in partnership and (2) single, including anyone without a current partner (i.e. those who had never married, or were separated, divorced, or widowed). The household socioeconomic status in each site was based on a locally derived wealth index; all households in a site were allocated to wealth quintiles that were developed using principal component factor analysis22 on a range of asset variables including dwelling characteristics and household possessions (such as type and size of dwelling, access to water and electricity; appliances and livestock owned; and transport available).
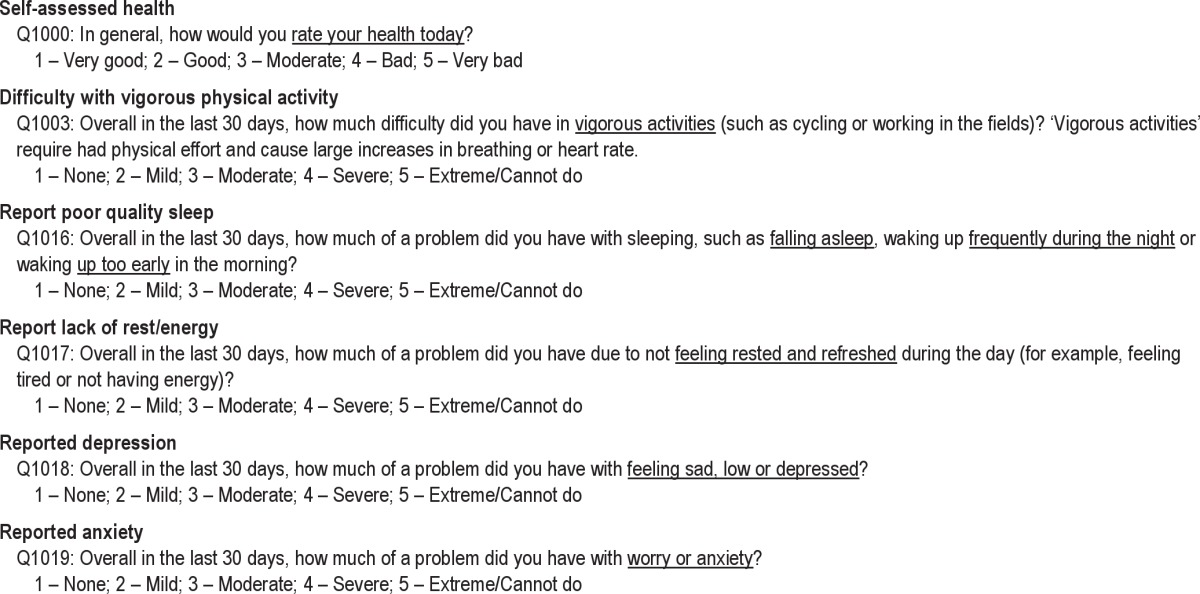
Self-rated quality of life was measured using the World Health Organization Quality of Life (WHOQOL) scale assessing the person’s satisfaction with his or her life, whereas physical functionality or disability of each participant was measured using the World Health Organization Disability Assessment Schedule (WHODAS) scale. For both scales, the higher the score the poorer the outcome (WHOQOL ranging from 8 to 40, WHODAS from 1 to 100). Further details on these instruments can be found in previous reports.23,24 Feelings of depression and anxiety were elicited using the following questions: (1) 'Overall in the last 30 days, how much of a problem did you have with feeling sad, low, or depressed? (2) Overall in the last 30 days, how much of a problem did you have with worry or anxiety? Responses were collapsed in 2 categories: none/mild/moderate and severe/extreme.
Sleep problems were assessed by 2 questions: (1) 'Overall in the last 30 days, how much of a problem did you have with sleeping, such as falling asleep, waking up frequently during the night, or waking up too early in the morning?’ (Q1016 of the questionnaire, see Appendix); (2) 'Overall in the last 30 days, how much of a problem did you have due to not feeling rested and refreshed during the day (e.g., feeling tired or not having energy)?’ (Q1017 of the questionnaire, see Appendix).
The 1st question describes the frequency of nocturnal sleep problems; the 2nd question denotes frequency of difficulty related to daytime function. Both questions had 5 possible responses: none, mild, moderate, severe, and extreme. Responses were collapsed in 2 categories: none/mild/moderate and severe/extreme.
Statistical Analysis
Data were entered using the CSPro 3.1 data entry program, which includes validation checks (http://www.census.gov/ipc/www/cspro/index.html). Data were weighted based on the reference population for each of the 8 HDSS sites, similar to a previous report from the same study.18
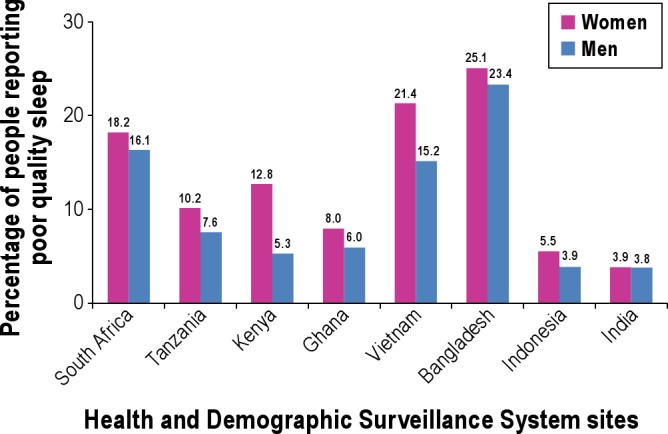
For descriptive purposes, all the selected variables were 1st analyzed in both women and men across the 8 HDSS sites (Table 1). We also showed the percentage of female and male participants, for each country, who reported severe/extreme problems with both falling asleep (Q1016) and not feeling rested and refreshed during the day (Q1017). These data are displayed separately in Figures 1 and 2. Bivariate models were then used to determine the statistical significance (χ2 tests) of any difference in the distribution of nocturnal sleep problems across the selected correlates within each population, in both women and men (Table 2).
Table 1.
Characteristicsa of the study populations, among women and men (age range: 50-106 yr), in 8 Health and Demographic Surveillance System (HDSS) sites in Africa and Asia, 2006–2007
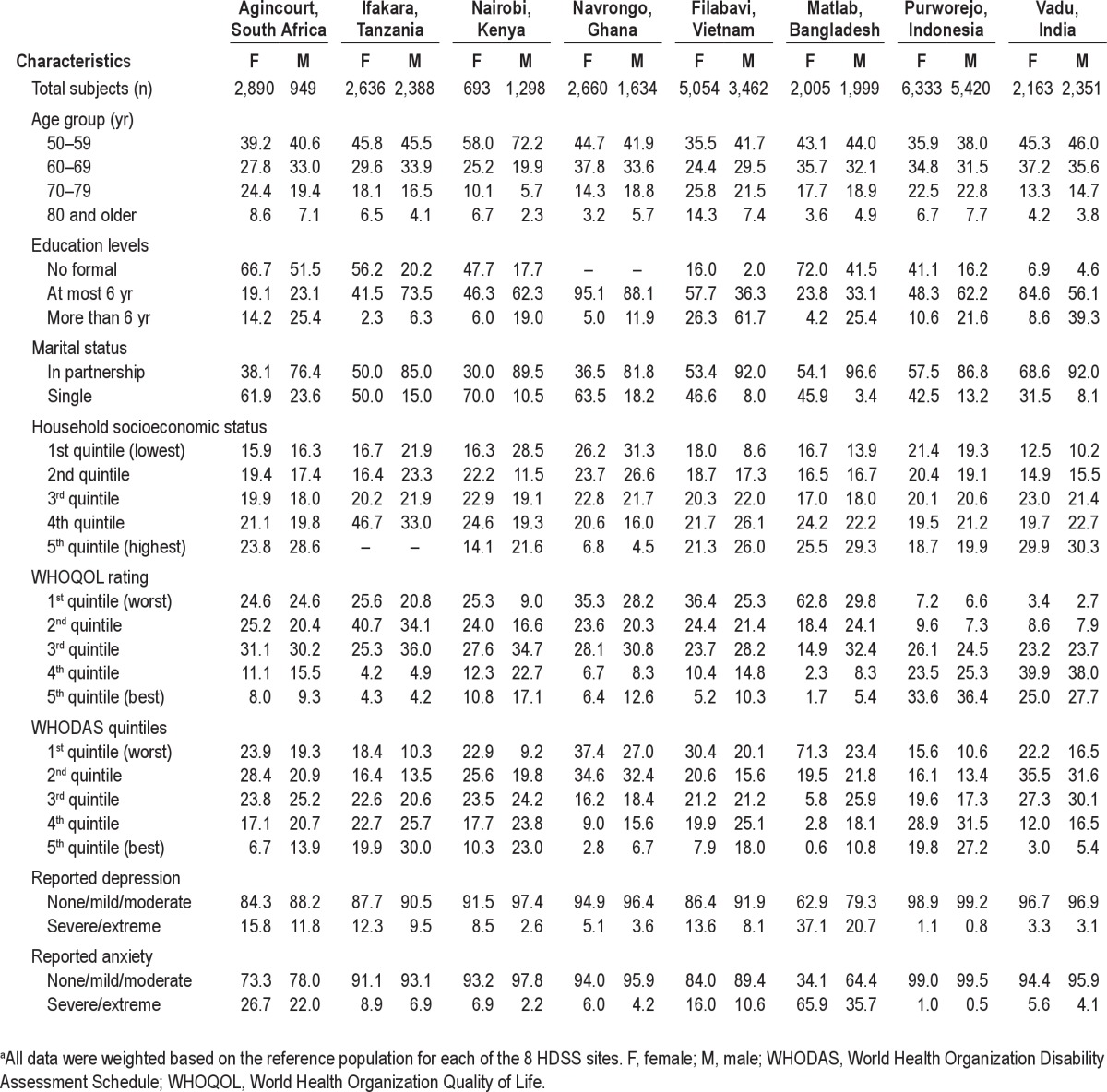
Figure 1.
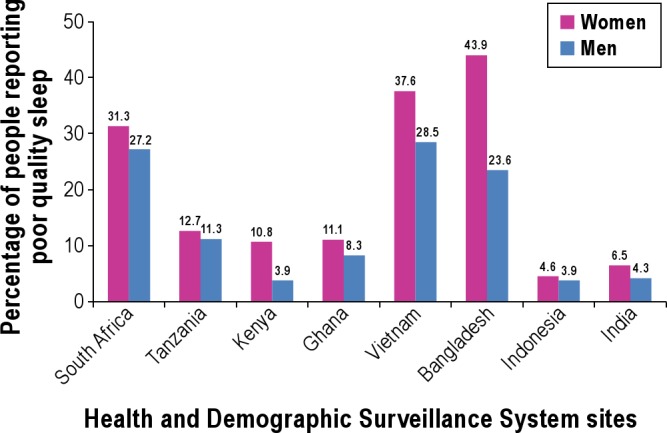
Weighted prevalence of self-reported nocturnal sleep problems by sex in 8 Health and Demographic Surveillance System sites in Africa and Asia, 2006-2007. Percentage of female and male participants, for each country, who reported severe/extreme problems with falling asleep (Q1016).
Figure 2.
Weighted prevalence of self-reported difficulty related to daytime function by sex in 8 Health and Demographic Surveillance System sites in Africa and Asia, 2006-2007. Percentage of female and male participants, for each country, who reported severe/extreme problems with not feeling rested and refreshed during the day (Q1017).
Table 2.
Weighted prevalence (%) of self-reported nocturnal sleep problems (Q1016)a, across selected correlates, among women and men (age range: 50-106 yr), in 8 Health and Demographic Surveillance System (HDSS) sites in Africa and Asia, 2006–2007
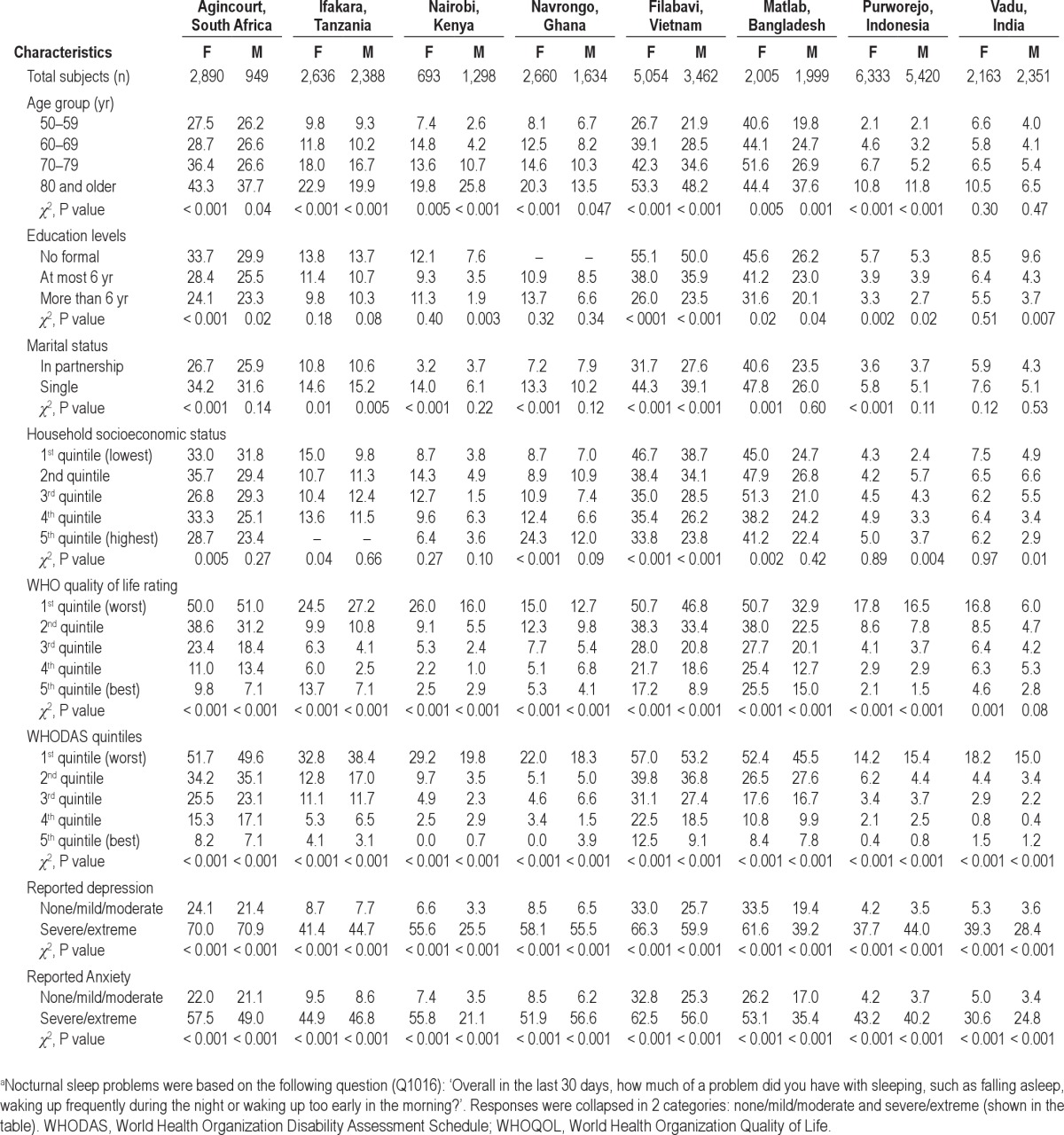
Next, we performed multivariate logistic regression analyses to estimate the risk of sleep problems (severe/extreme category versus none/mild/moderate for both questions) across the selected correlates within each population, for both women and men (Tables 3 and 4, supplementary Tables S1 and S2). Reference categories were as follows: 50-59 yr (age); > 6 yr (education); living in partnership (marital status); 5th quintile (household socioeconomic status); 5th quintile (WHOQOL and WHODAS); none/mild/moderate (depression and anxiety). These analyses were adjusted for the full set of selected covariates (sociodemographics, WHOQOL, WHODAS, depression, and anxiety). All statistical analyses were conducted with STATA Version 10.0 (StataCorp LP, College Station, TX, USA).25
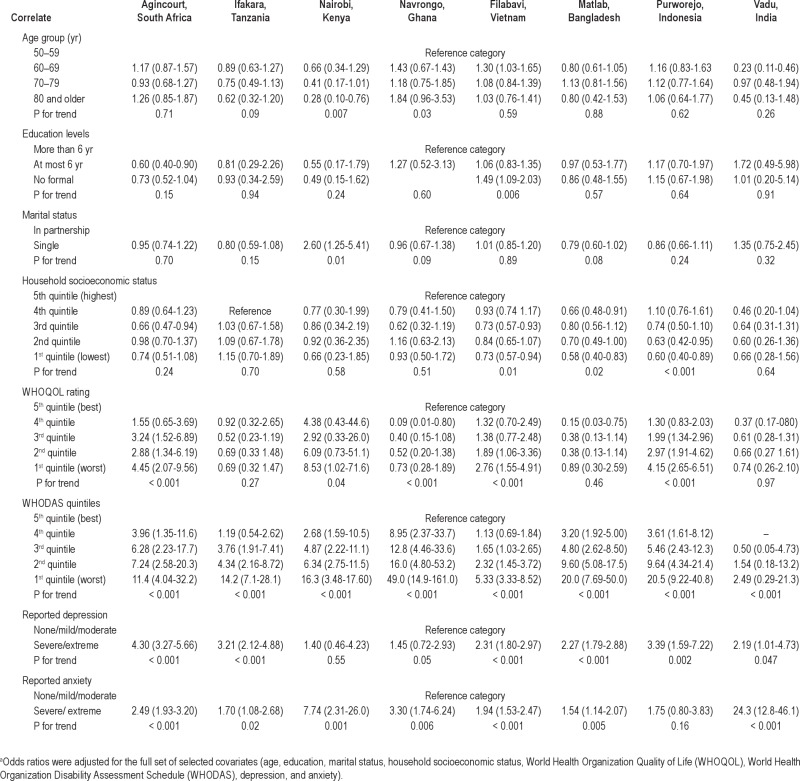
Table 3.
Fully-adjusted odds ratiosa for severe/extreme nocturnal sleep problems, across selected correlates, among women (age range: 50-106 yr), in 8 Health and Demographic Surveillance System (HDSS) sites in Africa and Asia, 2006-2007
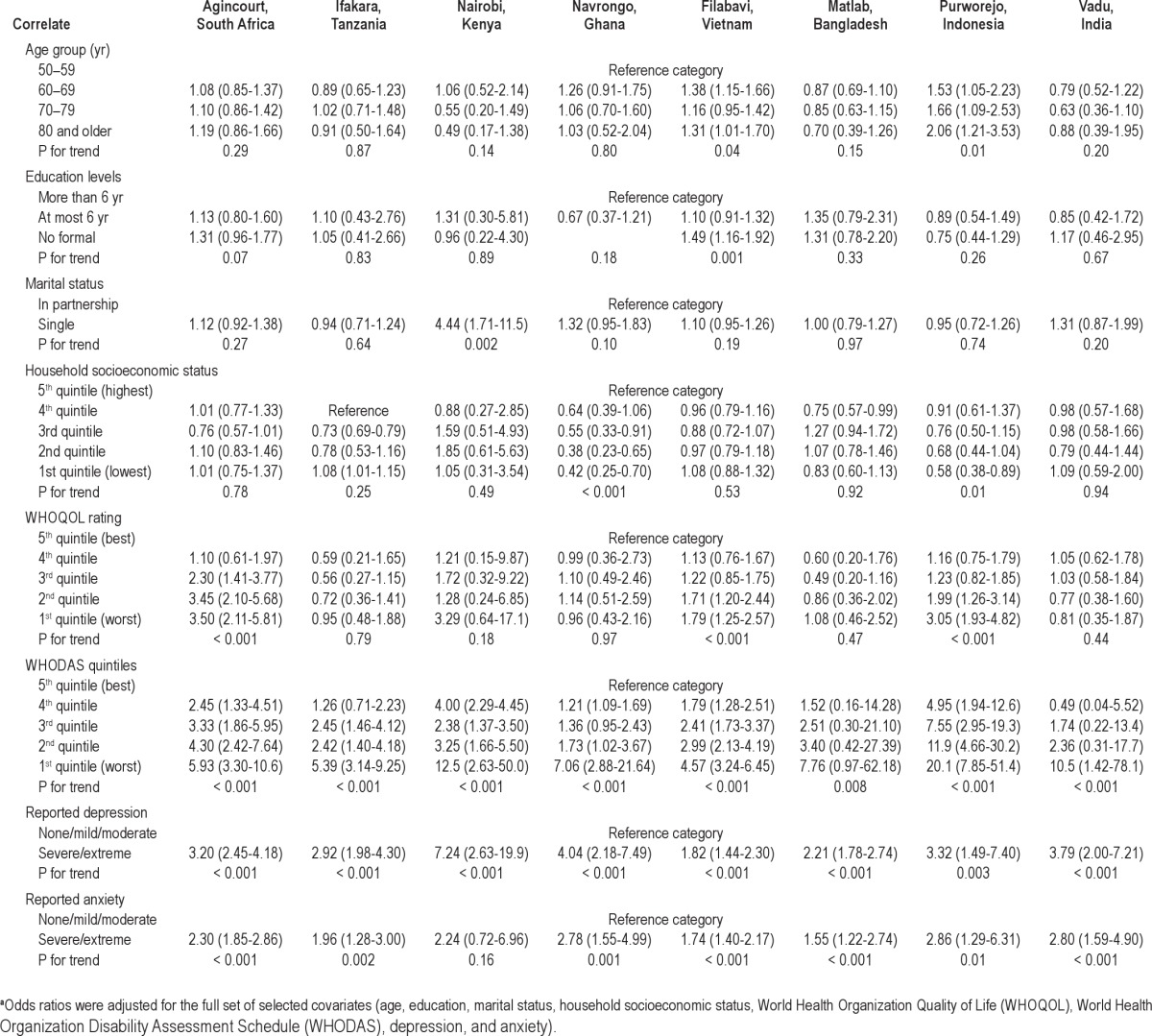
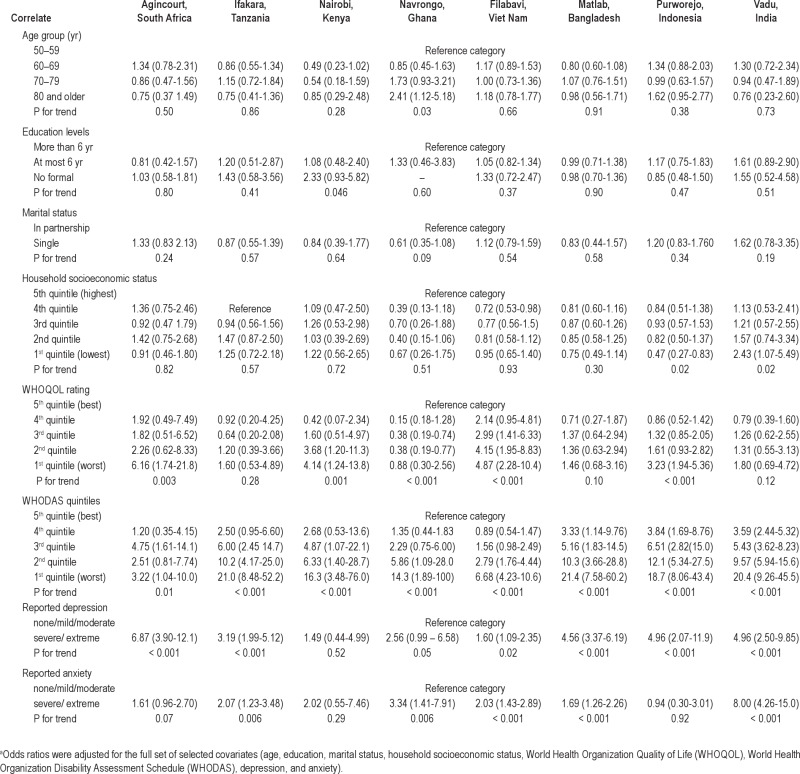
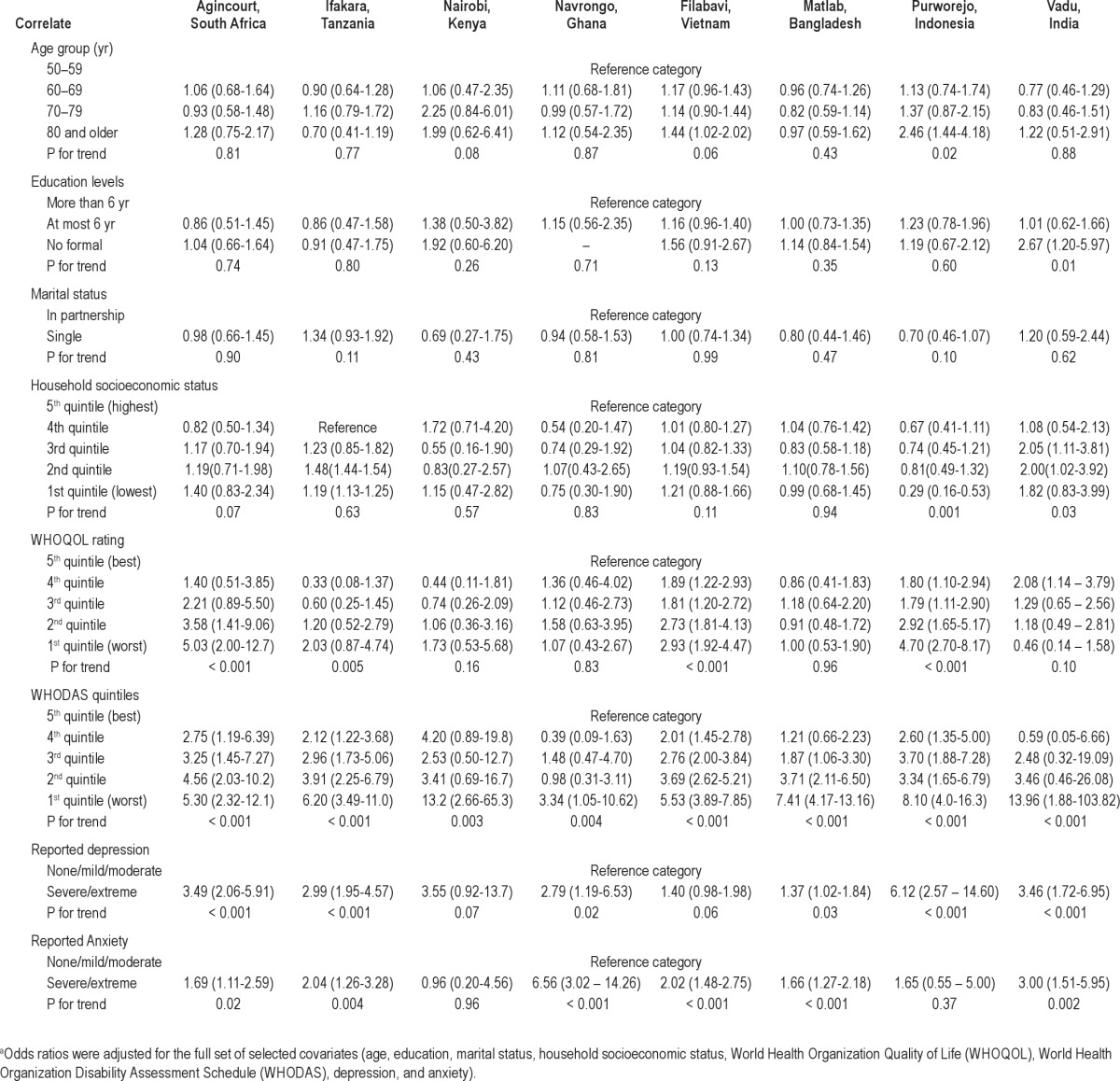
Table 4.
Fully-adjusted odds ratiosa for severe/extreme nocturnal sleep problems, across selected correlates, among men (age range: 50-106 yr), in 8 Health and Demographic Surveillance System (HDSS) sites in Africa and Asia, 2006-2007
RESULTS
Table 1 shows the general characteristics of the study populations, for both female and male participants, across the 8 HDSS sites. The age-sex distribution varied considerably across the 8 sites. In Agincourt, South Africa, the smaller number of males reflects long-standing practices connected with migrant labor.26 In Nairobi, Kenya, the site was located in an urban slum area with better employment opportunities, and thus younger males dominated the population structure.27 In general, female participants and those from African sites had lower education levels than male participants and those from Asian sites. There were no consistent differences in self-reported health status between sexes, but participants from Asian sites reported, in general, a better health status than those from African sites. Overall, female participants reported worse self-rated quality of life (WHOQOL) and physical functionality or more disability (WHODAS) than their male counterparts.
There was a large variation in self-reports of depression and anxiety across sites, with the highest prevalence in Bangladesh and the lowest in Indonesia. Women were consistently more likely than men to report severe/extreme feelings of depression and anxiety.
Importantly, there was a striking variation in the prevalence of people reporting severe/extreme nocturnal sleep problems (Figure 1) across the 8 populations, ranging from 3.9% (male participants in Purworejo, Indonesia and Nairobi, Kenya) to 43.9% (female participants in Bangladesh). However, there was a consistent higher prevalence of self-reported sleep problems in women than men across the 8 sites. Overall, 16.6% of participants (19.8% women, 12.8% men) reported nocturnal sleep problems. Similar patterns were observed for the prevalence of people reporting severe/extreme difficulty related to daytime function (Figure 2) across the 8 sites.
Table 2 shows the prevalence of nocturnal sleep problems, across selected correlates, in women and men across the 8 HDSS sites. In general, the frequency of sleep problems increased with increasing age across the 8 populations. Lower education levels and not living in partnership were consistently associated with higher prevalence of sleep problems, whereas there was no consistent pattern of association between household socioeconomic status and sleep problems. Furthermore, poorer self-rated quality of life, greater disability, and feelings of depression and anxiety were all significantly associated with higher prevalence of sleep problems, both in women and men, across the 8 sites (P < 0.001). There was a similar pattern of associations for the prevalence of difficulty with daytime function (data not shown).
In Tables 3 and 4, we show odds ratios for nocturnal sleep problems, across selected correlates, in women and men, respectively, from multivariate logistic regression analyses. Results were adjusted for the full set of selected covariates (age, education, marital status, household socio-economic status, WHOQOL, WHODAS, depression, and anxiety).
Associations of age, lower education, not living in partnership, and poorer self-rated quality of life (WHOQOL) with higher frequency of sleep problems, observed in bivariate analyses, were somewhat attenuated and not fully consistent, across the 8 sites, after multivariate adjustment.
By contrast, limited physical functionality or greater disability (WHODAS) and feelings of depression and anxiety were consistently strong, independent correlates of sleep problems, in both women and men, across the 8 sites. In particular, there were consistent higher odds of sleep problems associated with a greater degree of disability and with reporting of severe/extreme feeling of depression, in both sexes and across populations (P for linear trend < 0.001). There was a similar pattern of associations with regard to difficulty with daytime function (Supplementary Tables S1 and S2).
DISCUSSION
To our knowledge, this is the first report on sleep problems and associated factors in a large number of older adults across 8 populations from low-income settings in Africa and Asia. Overall, 16.6% of adults age 50 yr and older reported sleep problems in this study. Assuming this multicenter community-wide sample across Africa and Asia is approximately representative of older people within the United Nations definition of less-developed countries,28 population estimates for people age 50 yr and older in low-income countries in 2010 total nearly 900 million, 16.6% of which would be approximately 150 million. This number is likely to increase over the next few decades, given the ongoing demographic and epidemiologic transition occurring in these populations.14–16 By 2030, the number of older adults in these settings is projected to rise to 1.578 million, corresponding to more than 260 million people possibly experiencing sleep problems. Therefore, these estimates suggest that sleep disturbances may represent a significant and unrecognized problem among older people in low-income settings. These findings further emphasize the global dimension of sleep problems as an emerging public health issue.
In the current study, there was a striking variation in the prevalence of self-reported sleep problems across the 8 populations, ranging from 3.9% (male participants in Indonesia and Kenya) to more than 40% (female participants in Bangladesh, 1 of the poorest countries in the INDEPTH group).
However, within these large intercountry differences, we could rank these populations in 3 groups based on the increasing prevalence of self-reported sleep problems in the study: low (India and Indonesia), medium (Kenya, Ghana, and Tanzania), and high (Bangladesh, South Africa, and Vietnam). There is very little published evidence on sleep problems from rural populations in Africa and Asia. Therefore, any explanation for the observed differences or similarities in the prevalence of self-reported sleep problems across countries currently is highly speculative. These differences are intriguing and may hold clues to the etiology of sleep problems, and certainly warrant further research. They do approximately match the observed patterns for our questions on depression and anxiety, so that may be part of the explanation, but it is also difficult to understand why levels of reported depression and anxiety vary so much in our study. Moreover, these differences cannot be entirely explained by poverty. Although India and Indonesia are among the wealthiest sites in the INDEPTH network and seem to have fewer sleep problems, this is not true for South Africa, the wealthiest country in this study but with a high prevalence of sleep problems.29 On the other hand, Bangladesh is the 2nd poorest country in the INDEPTH network and had the highest prevalence of sleep problems in our study; however, Tanzania, which is even poorer than Bangladesh and Vietnam, had fewer sleep problems.29 Also, the observed sex difference is more marked in Kenya than elsewhere and Kenya is the only urban slum site, attracting labor migrants, and where men outnumber women and the population in general is younger.27
Furthermore, a previous study from Bangladesh suggests a high prevalence of psychiatric disorders including sleep problems, especially among women.30 In that study, more than 1,000 people age 18 yr and older, from an urban community in Dhaka, Bangladesh, were screened for psychiatric disorders. The authors reported a striking sex difference in the prevalence of these disturbances, including sleep problems, with almost half of the female population in the study affected by mental disorders compared with 13.5% of males. Although not entirely comparable with that study, our findings showed that 43.9% of women from a rural community in Matlab (Bangladesh) reported sleep problems, compared with 23.6% of males (Figure 1).
In our study the prevalence of self-reported sleep problems was consistently higher in women than men. There are a number of additional potential explanations for these sex differences in sleep problems, such as different physiology, greater burden of psychologic comorbidity (anxiety, depression) in women, gender-specific roles such as mothering and related stresses, disparities in socioeconomic status and social role, and differential self-reporting of sleep habits between men and women.31 These gender differences may have important public health implications, given the reported association between sleep problems and cardiovascular risk specifically in women.32–35
We also examined the relationship of sleep problems with a number of sociodemographic variables, measures of quality of life, and comorbidities. Aging, not living in partnership, lower education levels, poorer quality of life, limited physical functionality or greater disability, and feelings of anxiety and depression were all strong correlates of sleep problems. These 1st-time findings from resource-poor settings are in general agreement with studies of determinants of quantity and quality of sleep in populations from higher-income countries,4–10,36–43 strengthening the external validity and generalizability of our findings.
All the study participants were age 50 yr and older, but within that age range, people in older age groups generally reported higher prevalence of sleep problems across sites, although these associations were somewhat attenuated after multivariate adjustment. These findings are consistent with previous reports of an increased prevalence of sleep disturbances or increased use of sedative hypnotic agents in older adults.4,19,44–46 Physiologic studies have documented changes in sleep structure associated with healthy aging.47–49 Age-related changes in sleep may also be the consequence of chronic physical and psychologic comorbidities, which are common in the elderly.8,46
Although information on chronic comorbidities was not available, we used measures of self-reported quality of life and disability as a proxy for chronic comorbidities, and these were all strongly associated with higher prevalence of sleep problems. Furthermore, we found a strong, consistent relationship between sleep problems and self-reported depression and anxiety. Similar findings have been reported in previous cross-sectional analyses from different populations worldwide.4,8,39
The current study has several strengths, primarily the large multicenter community-wide population; however, the cross-sectional design does not allow us to address causality and temporality of the observed associations. Moreover, data on chronic comorbidities and lifestyle behaviors were not collected, preventing any analysis adjusting for these variables. Furthermore, information about sleep problems was self-reported, which could produce misclassification of true sleep patterns.50–53
In addition, our sleep questions were not ideal. For example, 1 particular problem is that persons who feel fatigued due to health problems not related to sleep may have endorsed the 2nd question.51 Also, these questions might be interpreted differently by persons in different cultures,54 which could account for some of the large differences seen across sites. However, self-reports of problems related to sleep quality may be less prone to misclassification than self-reported sleep duration. Furthermore, to increase specificity of our tool, we only included those reporting severe and extreme sleep problems, leaving out those with mild and moderate sleep problems. In addition, sleep quality may represent a more comprehensive measure of sleep patterns than sleep duration, and is strongly associated with measures of general well-being and quality of life.55
In conclusion, sleep disturbances might represent a significant and unrecognized public health issue among older people, especially women, in low-income settings. This is the 1st large multicenter study on sleep problems and associated factors in populations from less developed countries and rural regions, where environmental factors that are known to influence sleep, such as exposure to a 24-hr “lifestyle” via media/internet/economy, seasonal photoperiod, and temperature differ appreciably from developed Western societies.19–21 Despite these differences, our study suggests that sleep problems are highly prevalent in some, but not all, low-income countries. Without comparable data from earlier reports, it is not possible to identify trends in sleep problems in these settings. Nevertheless, given the overwhelming evidence linking sleep problems to morbidity and mortality outcomes, these findings call for public health initiatives to raise awareness about sleep problems in low-income countries.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the INDEPTH Network, Accra, Ghana and the Health Statistics and Informatics from the World Health Organization, Geneva, Switzerland for publicly providing the INDEPTH WHO-SAGE multicenter study data. The authors also thank the study participants, field team, and district health authorities. The study was funded by the National Institute on Aging of the National Institutes of Health, USA and by the Wellcome Trust, UK (Grant number 058893/Z/99/A and 069683/Z/02/Z). It was carried out in collaboration with the World Health Organization, Study on Global Ageing and Adult Health (SAGE), and the INDEPTH Network, Accra, Ghana. The authors acknowledge with appreciation the continuing contribution of Somnath Chatterji and Paul Kowal of the Multi-Country Studies Measurement and Health Information Systems (MHI) World Health Organization.
Appendix
List of outcome measures from questionnaire of the WHO/INDEPTH Study on Global Ageing and Adult Health (SAGE) 2006-2007 used in the current study
Footnotes
A commentary on this article appears in this issue on page 1035.
SUPPLEMENTAL MATERIAL
Fully-adjusted odds ratiosa for severe/extreme difficulty related to daytime function, across selected correlates, among women (age range: 50-106 yr), in 8 Health and Demographic Surveillance System (HDSS) sites in Africa and Asia, 2006–2007
Fully-adjusted odds ratiosa for severe/extreme difficulty related to daytime function, across selected correlates, among men (age range: 50-106 yr), in 8Health and Demographic Surveillance System (HDSS) sites in Africa and Asia, 2006–2007
REFERENCES
- 1.Bonnet MH, Arand DL. We are chronically sleep deprived. Sleep. 1995;18:908–11. doi: 10.1093/sleep/18.10.908. [DOI] [PubMed] [Google Scholar]
- 2.Sutton DA, Moldofsky H, Badley EM. Insomnia and health problems in Canadians. Sleep. 2001;24:665–70. doi: 10.1093/sleep/24.6.665. [DOI] [PubMed] [Google Scholar]
- 3.Hossain JL, Shapiro CM. The prevalence, cost implications, and management of sleep disorders: an overview. Sleep Breath. 2002;6:85–102. doi: 10.1007/s11325-002-0085-1. [DOI] [PubMed] [Google Scholar]
- 4.Groeger JA, Zijlstra FR, Dijk DJ. Sleep quantity, sleep difficulties and their perceived consequences in a representative sample of some 2000 British adults. J Sleep Res. 2004;13:359–71. doi: 10.1111/j.1365-2869.2004.00418.x. [DOI] [PubMed] [Google Scholar]
- 5.Hale L. Who has time to sleep? J Public Health (Oxf) 2005;27:205–11. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 6.Kronholm E, Harma M, Hublin C, Aro AR, Partonen T. Self-reported sleep duration in Finnish general population. J Sleep Res. 2006;15:276–90. doi: 10.1111/j.1365-2869.2006.00543.x. [DOI] [PubMed] [Google Scholar]
- 7.Kronholm E, Partonen T, Laatikainen T, et al. Trends in self-reported sleep duration and insomnia-related symptoms in Finland from 1972 to 2005: a comparative review and re-analysis of Finnish population samples. J Sleep Res. 2008;17:54–62. doi: 10.1111/j.1365-2869.2008.00627.x. [DOI] [PubMed] [Google Scholar]
- 8.Stranges S, Dorn JM, Shipley MJ, et al. Correlates of short and long sleep duration: cross-cultural comparison between UK and US. The Whitehall II Study and the Western New York Health Study. Am J Epidemiol. 2008;168:1353–64. doi: 10.1093/aje/kwn337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169:1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hillman DR, Murphy AS, Pezzullo L. The economic cost of sleep disorders. Sleep. 2006;29:299–305. doi: 10.1093/sleep/29.3.299. [DOI] [PubMed] [Google Scholar]
- 12.Ozminkowski RJ, Shaohung SW, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30:263–73. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- 13.Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32:55–64. [PMC free article] [PubMed] [Google Scholar]
- 14.Salomon JA, Murray CJL. The epidemiologic transition revisited: compositional models for causes of death by age and sex. Popul Dev Rev. 2002;28:205–28. [Google Scholar]
- 15.Mathers C, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:2011–30. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Byass P. Towards a global agenda on ageing. Glob Health Action. 2008;1 doi: 10.3402/gha.v1i0.1908. 10.3402/gha.v1i0.1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kowal P, Kahn K, Ng N, et al. Ageing and adult health status in eight lower-income countries: the INDEPTH WHO-SAGE collaboration. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5302. 10.3402/gha.v3i0.5302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ng N, Kowal P, Kahn K, et al. Health inequalities among older men and women in Africa and Asia: evidence from eight Health and Demographic Surveillance System sites in the INDEPTH WHO-SAGE Study. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5420. 10.3402/gha.v3i0.5420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferrie JE, Kumari M, Salo P, Singh-Manoux A, Kivimäaki M. Sleep epidemiology: a rapidly growing field. Int J Epidemiol. 2011;40:1431–7. doi: 10.1093/ije/dyr203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bliwise DL. Invited commentary: cross-cultural influences on sleep--broadening the environmental landscape. Am J Epidemiol. 2008;168:1365–6. doi: 10.1093/aje/kwn336. [DOI] [PubMed] [Google Scholar]
- 21.Bixler E. Sleep and society: an epidemiological perspective. Sleep Med. 2009;10:S3–6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 22.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal component analysis. Health Policy. 2006;21:459–68. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 23.Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Qual Life Res. 1993;2:153–9. [PubMed] [Google Scholar]
- 24.The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–9. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 25.StataCorp. College Station, TX: StataCorp LP; 2007. Stata Statistical Software: Release 10. [Google Scholar]
- 26.Xavier Gómez-Olivé F, Thorogood M, Clark BD, Kahn K, Tollman SM. Assessing health and well-being among older people in rural South Africa. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2126. 10.3402/gha.v3i0.2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kyobutungi C, Egondi T, Ezeh A. The health and well-being of older people in Nairobi’s slums. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2138. 10.3402/gha.v3i0.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.United Nations, Department of Economic and Social Affairs, Population Division, World Population Prospects: The 2010 Revision. New York; 2011. [Google Scholar]
- International Monetary Fund, World Economic Outlook Database, 2011 Sep [Google Scholar]
- 30.Islam MM, Ali M, Ferroni P, Underwood P, Alam MF. Prevalence of psychiatric disorders in an urban community in Bangladesh. Gen Hosp Psychiatry. 2003;25:353–7. doi: 10.1016/s0163-8343(03)00067-7. [DOI] [PubMed] [Google Scholar]
- 31.Baldwin CM, Kapur VK, Holberg CJ, Rosen C, Nieto FJ. Associations between gender and measures of daytime somnolence in the Sleep Heart Health Study. Sleep. 2004;27:305–11. doi: 10.1093/sleep/27.2.305. [DOI] [PubMed] [Google Scholar]
- 32.Meisinger C, Heier M, Lowel H, Schneider A, Doring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: the MONICA/KORA Augsburg cohort study. Sleep. 2007;30:1121–7. doi: 10.1093/sleep/30.9.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cappuccio FP, Stranges S, Kandala NB, et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension. 2007;50:693–700. doi: 10.1161/HYPERTENSIONAHA.107.095471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stang A, Moebus S, Mohlenkamp S, Erbel R, Jockel KH. Gender-specific associations of short sleep duration with prevalent hypertension. Hypertension. 2008;51:e15–6. doi: 10.1161/HYPERTENSIONAHA.107.108456. [DOI] [PubMed] [Google Scholar]
- 35.Stranges S, Dorn JM, Cappuccio FP, et al. A population-based study of reduced sleep duration and hypertension: the strongest association may be in premenopausal women. J Hypertens. 2010;28:896–902. doi: 10.1097/HJH.0b013e328335d076. [DOI] [PubMed] [Google Scholar]
- 36.Sickel AE, Moore PJ, Adler NE, Williams DR, Jackson JS. The differential effects of sleep quality and quantity on the relationship between SES and health. Ann N Y Acad Sci. 1999;896:431–4. doi: 10.1111/j.1749-6632.1999.tb08162.x. [DOI] [PubMed] [Google Scholar]
- 37.Ohayon MM, Zulley J. Correlates of global sleep dissatisfaction in the German population. Sleep. 2001;24:780–7. [PubMed] [Google Scholar]
- 38.Ohayon MM, Hong SC. Prevalence of insomnia and associated factors in South Korea. J Psychosom Res. 2002;53:593–600. doi: 10.1016/s0022-3999(02)00449-x. [DOI] [PubMed] [Google Scholar]
- 39.Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005;6:23–7. doi: 10.1016/j.sleep.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 40.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29:85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- 42.Sekine M, Chandola T, Martikainen P, Marmot M, Kagamimori S. Work and family characteristics as determinants of socioeconomic and sex inequalities in sleep: The Japanese Civil Servants Study. Sleep. 2006;29:206–16. doi: 10.1093/sleep/29.2.206. [DOI] [PubMed] [Google Scholar]
- 43.Arber S, Bote M, Meadows R. Gender and socio-economic patterning of self-reported sleep problems in Britain. Soc Sci Med. 2009;68:281–9. doi: 10.1016/j.socscimed.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 44.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18:425–32. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 45.Glass J, Lanctot KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ. 2005;331:1169. doi: 10.1136/bmj.38623.768588.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56:497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 47.Van Cauter E, Leproult R, Plat L. Age-related changes in slow wave sleep and REM sleep and relationship with growth hormone and cortisol levels in healthy men. JAMA. 2000;284:861–8. doi: 10.1001/jama.284.7.861. [DOI] [PubMed] [Google Scholar]
- 48.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 49.Dijk DJ, Groeger JA, Stanley N, Deacon S. Age-related reduction in daytime sleep propensity and nocturnal slow wave sleep. Sleep. 2010;33:211–23. doi: 10.1093/sleep/33.2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Silva GE, Goodwin JL, Sherrill DL, et al. Relationship between reported and measured sleep times: the sleep heart health study (SHHS) J Clin Sleep Med. 2007;3:622–30. [PMC free article] [PubMed] [Google Scholar]
- 51.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res. 1999;8:175–83. doi: 10.1046/j.1365-2869.1999.00155.x. [DOI] [PubMed] [Google Scholar]
- 53.Signal TL, Gale J, Gander PH. Sleep measurement in flight crew: comparing actigraphic and subjective estimates to polysomnography. Aviat Space Environ Med. 2005;76:1058–63. [PubMed] [Google Scholar]
- 54.King G, Murray CJL, Salomon JA, Tandon A. Enhancing the validity and cross-cultural comparability of measurement in survey research. Am Polit Sci Rev. 2004;98:191–207. [Google Scholar]
- 55.Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: relationships between sleep and measures of health, well-being and sleepiness in college students. J Psychosom Res. 1997;42:583–96. doi: 10.1016/s0022-3999(97)00004-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fully-adjusted odds ratiosa for severe/extreme difficulty related to daytime function, across selected correlates, among women (age range: 50-106 yr), in 8 Health and Demographic Surveillance System (HDSS) sites in Africa and Asia, 2006–2007
Fully-adjusted odds ratiosa for severe/extreme difficulty related to daytime function, across selected correlates, among men (age range: 50-106 yr), in 8Health and Demographic Surveillance System (HDSS) sites in Africa and Asia, 2006–2007