Abstract
Objectives:
This study examined the effects of age, gender, and retirement on the subjective frequency of various sleep problems in individuals on a normal work schedule.
Design:
Data were taken from the VISAT study (Aging, Health, – Work), which allowed both cross-sectional and longitudinal aspects of age-related changes to be examined.
Setting:
Various sorts of companies in southern France.
Participants:
The cohorts comprised 623 male and female, employed and retired, wage earners who were 32, 42, 52, and 62 years old at the time of the first measurement (t1, 1996), and who were seen again 5 (t2) and 10 (t3) years later.
Interventions:
N/A.
Measurements and Results:
Subjective ratings of the frequency of sleep problems and hypnotic usage were recorded on all 3 occasions, as was the employment status of the individuals. After controlling for age and gender, an effect of decade was observed for difficulty falling asleep and difficulty maintaining sleep, indicating that the frequency of these sleep problems was rated higher in 2006 than in 1996 by people of the same age at both measurement occasions. The perceived frequency of difficulty maintaining sleep, difficulty getting back to sleep, and premature awakening was found to increase up to the mid-50s but to then remain relatively constant, or even in the case of premature awakening to reduce, up to the age of 72. There was also a significant improvement in premature awakening among those individuals who changed from being active to being retired during the study period (n = 111). In contrast, the rated frequency of difficulty falling asleep and hypnotic usage increased fairly linearly over the entire age range.
Conclusions:
Sleep complaints were reported early in the workers’ lives, and were more frequent with age, but some of them improved after retirement, especially the complaint of premature awakening.
Citation:
Marquiáe JC; Folkard S; Ansiau D; Tucker P. Effects of age, gender, and retirement on perceived sleep problems: results from the VISAT Combined Longitudinal and Cross-Sectional Study. SLEEP 2012;35(8):1115-1121.
Keywords: Age, sleep, gender, retirement, longitudinal study
INTRODUCTION
Ageing is known to affect sleep and circadian rhythms.1 However, what we have learned about ageing and sleep up to now comes mainly from studies comparing young adults with elderly people (> 65 or 70 years). With a few exceptions,2 these studies have somewhat neglected sleep changes in middle age. Yet ageing is a developmental process which takes place throughout adulthood, while the midlife years correspond to an individual’s occupational life. This period may be important because of both the possible consequences of sleep changes on work behavior and the influence that work may exert on sleep. The failure of studies to examine these middle years means that it is unclear whether changes in habits, sleep length, and the quality of sleep with age occur gradually throughout an individual’s lifespan, or whether major changes only occur in later years.
The combined effects of the endogenous circadian changes that start in midlife,3 and the more or less durable impact of occupational experiences such as job stress and retirement may result in significant sleep changes taking place during the middle years of life. However, as Monk2 has stressed, the magnitude and precise nature of these changes need elucidation, as do their determinants. However, the extreme diversity of peoples’ ways of life and working conditions, individual differences in the sensitivity to these environmental factors4 and the complexity of the processes which result from the conjunction of circadian and homeostatic mechanisms5 are all likely to influence sleep parameters. This complexity may explain why so many issues regarding sleep changes and their consequences in adults remain unanswered. The effects of ageing on sleep complaints are further complicated by potential societal, economic, cultural, and medical changes over time. These influences may lead to historical differences in the manner in which individuals perceive, and hence report, their sleep problems. Thus, even if we control for age, we might find that the level of sleep complaints reported today may differ from that reported 10 years ago, i.e., there may be an effect of “decade.” Thus the growing demand for enhanced quality of life and health in our modern society might lower the threshold for sleep complaint tolerance. Examining the various time-related factors involved in long-term sleep changes, such as historical context, cohort effect, and the ageing process requires specific methodologies, based on the follow-up of cohorts over a long period.
The cross-sequential design of the current study, combining both cross-sectional and longitudinal methods allowed us to address these issues. It also enabled us to examine the impact of retirement, an important factor which is normally confounded with age, on sleep problems. There is a paucity of literature on the effects of retirement on sleep, and the findings to date have been inconsistent,7 perhaps reflecting the difficulty of distinguishing the effects of retirement from those of ageing and decade.
METHODS
Participants
The data were taken from the cross-sectional and longitudinal phases of the VISAT study.6 The initial sample was composed of 3,237 present and former wage earners born in 1964, 1954, 1944, or 1934. They were exactly 32, 42, 52, and 62 years old at the time of the first data collection (1996, t1). Eighty-three percent of the participants born in 1934 were retirees at t1. Participants were randomly drawn from the client lists of 94 occupational physicians in 3 southern regions of France, and the questionnaires were administered during the mandatory annual check-up. The participation rate at t1 was 76%. More than two-third of participants (n = 2,288; 70.68%) were seen again at the first follow-up (t2) 5 years later (2001). The second follow-up (t3) took place in 2006 and examined 1,308 participants (40.40%), including 51 participants who were not seen at t2.
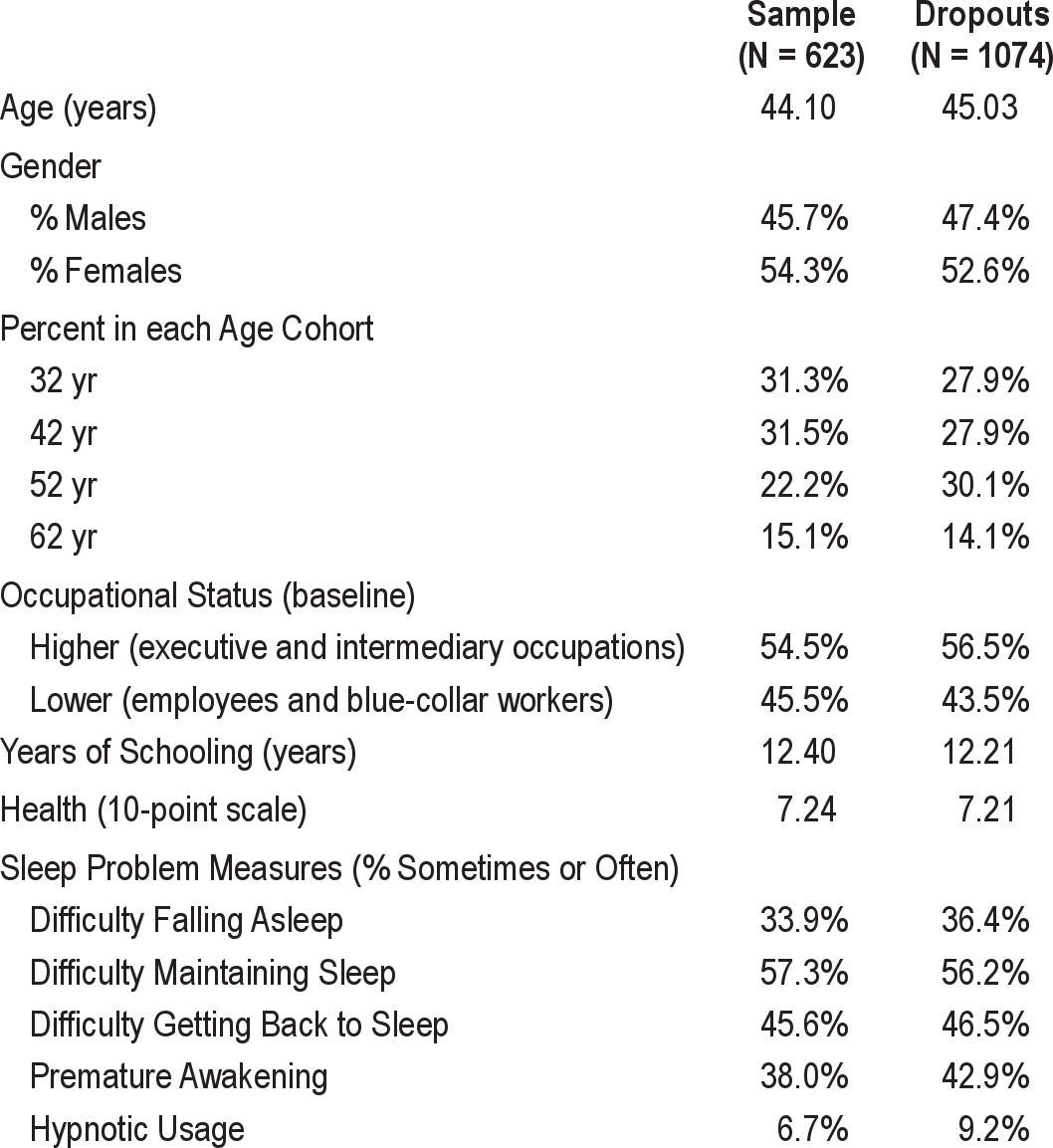
In the present paper we consider only those 623 participants who were seen on 3 measurement occasions and who claimed at t3 that they had never worked on rotating shifts or an abnormal work schedule. The main characteristics of these participants are shown in Table 1. In order to check for potential biases in this selected sample, we conducted comparisons between these participants and those who had never worked on an abnormal schedule at time 1, but had either dropped out or had worked on an abnormal work schedule by time 3 (“dropouts,” see Table 1). The use of a t-test indicated that there was a suggestion that the selected sample was slightly younger than the dropouts (t1695 = 1.77, P = 0.076]. Chi-square tests did not reveal any significant difference between current participants and dropouts in terms of job status (higher vs. lower) or gender (P > 0.30 in both cases). Nor was there any difference in the number of years of schooling (t1695 = 1.013, P = 0.31) between the selected sample and the dropouts or in the self-assessed overall health status (10-point scale, with 10 = excellent; t1694 = 0.336, P = 0.74). These nonsignificant differences suggest that the selected participants did not differ from the dropouts at baseline (t1) in terms of gender, job status, years of schooling, or self-assessed health.
Table 1.
Comparison of selected sample and dropouts characteristics at baseline (t1)
Questionnaires
Sleep quality was assessed by asking the participants to rate on a 4-point scale (never, seldom, sometimes, often) the frequency in the last month of 5 sleep complaints, namely: (1) difficulty falling asleep, (2) difficulty maintaining sleep, (3) difficulty getting back to sleep, (4) premature awakening, and (5) hypnotic medication use. These items were the same as those used in the previous sleep-related VISAT cross sectional study,8 and the same as, or quite similar to earlier studies on perceived sleep difficulties.9
Procedure and Data Analysis
Data were collected during the mandatory annual medical examination, which formed part of the health screening program that took place within the company. The authorization from the appropriate ethics committee was obtained. The mean interval between t1 and t2 data collections was 61.57 months (SD = 3.99; median = 61.0, mode = 60.0), and the mean interval between t2 and t3 was 59.84 months (SD = 4.36; median = 60.0, mode = 60.0). Questionnaires were self-administered but validated in a face-to-face interview. Retired workers, who were no longer monitored by the occupational physicians, were invited specially for the purpose of the study.
The data were analyzed using multinomial logistic regressions. Likelihood ratio tests were used for effects or interaction significance testing. For each model, all interactions between main effects have been explored through a backward selection algorithm. Only statistically significant interactions have been kept in the models aside from the main effects which were systematically forced in the models.
RESULTS
The “Decade” Effect
Preliminary inspection of the data indicated clear evidence of a “Decade” effect (i.e., an effect of the historical context of measurement) in some of the sleep problem measures, such that at the ages of 42, 52, and 62, sleep complaints were consistently rated as higher in 2006 (t3) than in 1996 (t1). Thus, for example, people in the youngest cohort rated their difficulty falling asleep as “Often” more frequently when they were 42 years old at t3 (in 2006) than did the 42-year-old cohort at t1 (1996). In order to examine this Decade effect in greater detail, a multinomial regression was conducted on each sleep problem measure that examined the between subject factors of Decade (1996 vs 2006), Age (42, 52, and 62), and Gender. It should be noted that some individuals contributed to 2 of the 6 cells (e.g., to the 42-year-olds in 1996 and to the 52-year-olds in 2006), and hence that the use of an entirely between-subject design is somewhat conservative. The results of these analyses are shown in Table 2.
Table 2.
Summary of significance levels in multinomial logistic regression models of Decade, Age, and Gender for each of the sleep problem measures
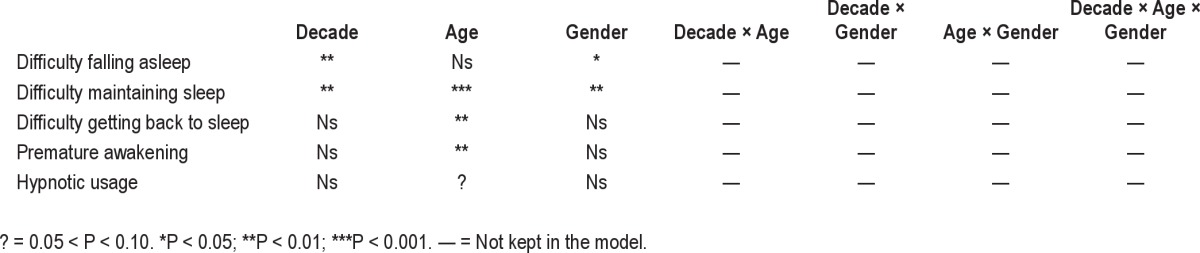
Inspection of Table 2 indicates that difficulty falling asleep and difficulty maintaining sleep both showed a significant main effect of Decade. No main effect of Decade was found significant for the other sleep scales. The effects of Age and Gender will be considered in greater detail below. The Decade effect is displayed in Figure 1.
Figure 1.
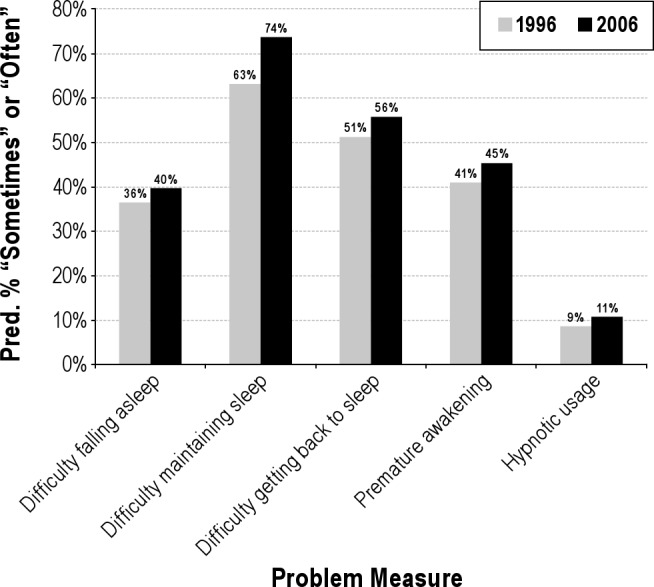
The Decade effect for each of the 5 sleep problem measures (mean predicted % of “Sometimes” plus mean predicted % of “Often”).
Cohort and Measurement Occasion
Separate multinomial regressions were performed for each sleep problem measure that examined Cohort (32, 42, 52, or 62 years old at t1), Gender, and Measurement Occasion (t1, t2, or t3). The results of these analyses are summarized in Table 3.
Table 3.
Summary of significance levels in multinomial logistic regression models of Cohort, Gender, and Measurement occasion for each of the sleep problem measures
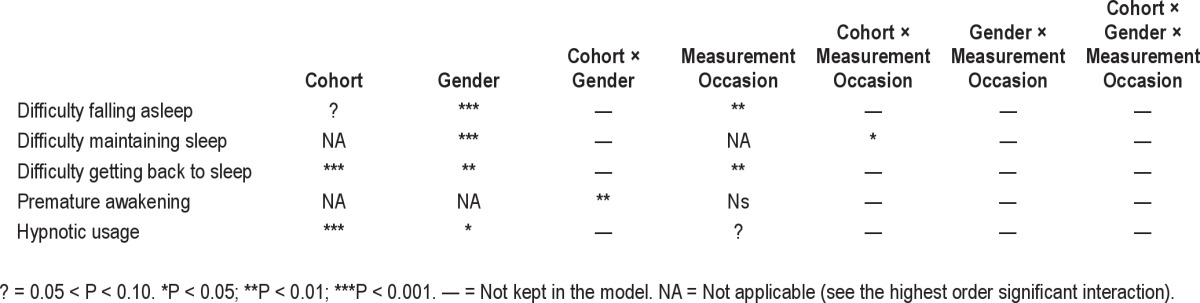
Inspection of Table 3 indicates that each sleep problem measure showed a different pattern of significant results. The effect of Cohort on difficulty falling asleep did not reach significance, and there was no significant interaction between Cohort and Measurement Occasion. There was, however, a significant main effect of Measurement Occasion (P < 0.01) and Gender (P < 0.001). Sleep difficulty increased between t2 and t3, and was reported as higher in females than in males, as shown in Figure 2. Note that, for clarity in this and subsequent figures, Cohort and Measurement Occasion have been collapsed into the underlying dimension of age, as both variables are surrogates of age.
Figure 2.
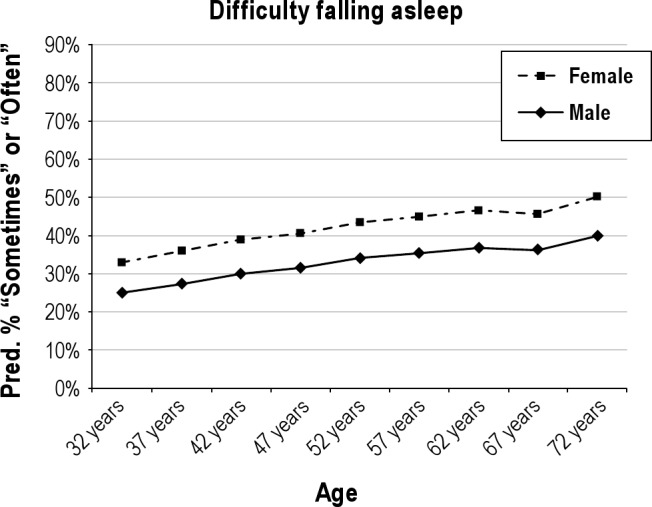
Difficulty falling asleep as a function of age and gender (mean predicted % of “Sometimes” plus mean predicted % of “Often”). The solid line shows the values for men and the dashed line those for women.
Difficulty maintaining sleep showed again a highly significant main effect of Gender (P < 0.001), but differed from difficulty falling asleep in that an interaction between the Cohort and Measurement Occasion (P < 0.05) was found. Difficulty maintaining sleep increased up to the age of about 52, but then remained relatively constant (see Figure 3).
Figure 3.
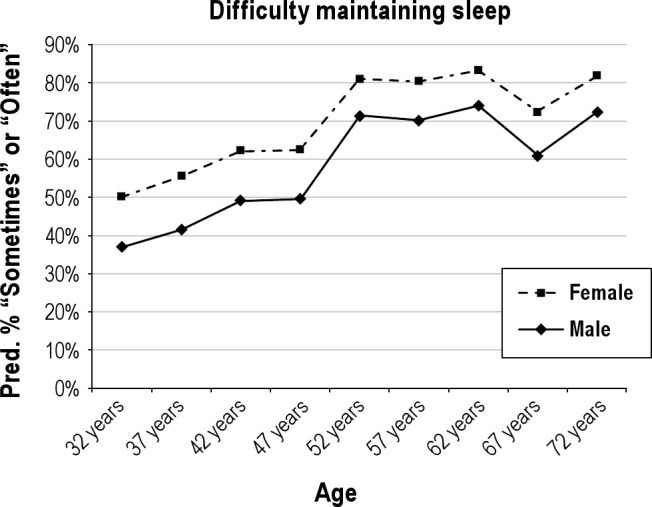
Difficulty maintaining sleep as a function of age and gender (mean predicted % of “Sometimes” plus mean predicted % of “Often”). The solid line shows the values for men and the dashed line those for women.
Difficulty getting back to sleep showed a fairly similar pattern of results to difficulty maintaining sleep (see Figure 4), with significant main effects of Cohort (P < 0.001), Gender (P < 0.01), and Measurement Occasion (P < 0.01), but no evidence of any interaction. Difficulty getting back to sleep increased up to the age of about 57 but then remained relatively constant. It was also higher in females than in males at all ages.
Figure 4.
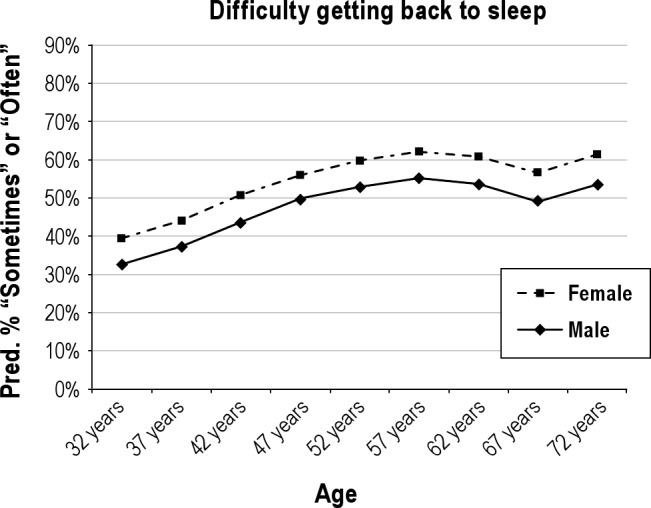
Difficulty getting back to sleep as a function of age and gender (mean predicted % of “Sometimes” plus mean predicted % of “Often”). The solid line shows the values for men and the dashed line those for women.
Premature awakening showed a rather different pattern of results with no effect of Measurement Occasion (see Figure 5). However, there was a significant interaction between the Cohort and Gender (P < 0.01), reflecting the fact that ratings of premature awakening differed between males and females as a function of age. Males reported a lower premature awakening frequency at the youngest ages, but their ratings showed a faster increase up to the 50s and were then similar to those of females.
Figure 5.
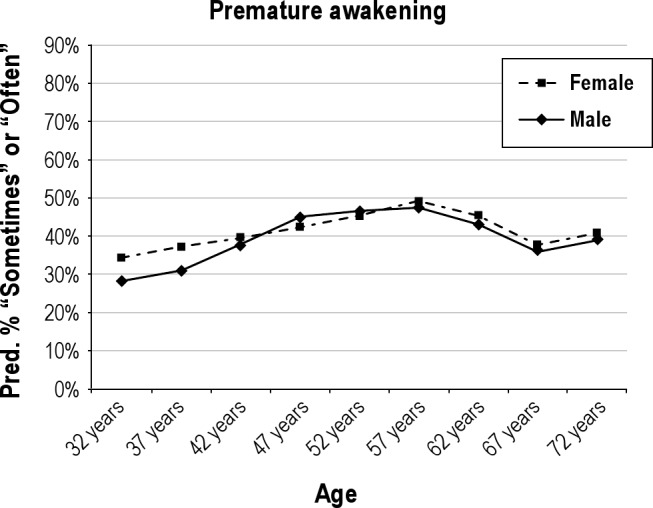
Premature awakening as a function of age and gender (mean predicted % of “Sometimes” plus mean predicted % of “Often”). The solid line shows the values for men and the dashed line those for women.
Finally, hypnotic usage showed significant main effects of both Cohort (P < 0.001) and Gender (P < 0.05), but no other significant effects. It is clear from inspection of Figure 6 that hypnotic usage showed a fairly linear increase with age and was at a higher level among females than males.
Figure 6.
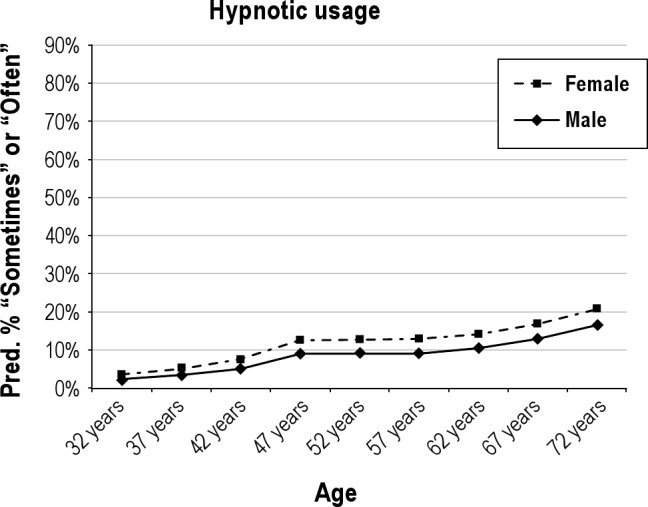
Hypnotic usage as a function of age and gender (mean predicted % of “Sometimes” plus mean predicted % of “Often”). The solid line shows the values for men and the dashed line those for women.
The Effects of Retirement
A potential explanation for the levelling off, or even reduction, in some perceived sleep problems following the age of 52 is simply reduced pressures to sleep at fixed times due to retirement. Thus, in the present sample, 99.1% were working at age 52, but this had reduced to 85.5% at age 57, to 15.5 % at age 62, and to 0% at ages 67 and 72, reflecting the “normal” retirement age of 60 in this population. In the 52 year old (at t1) cohort, 97 (50 males, 47 females) changed from being active in 2001 to being inactive in 2006, while 19 (8 males, 11 females) were inactive on both measurement occasions. A single individual changed from being inactive in 2001 to being active in 2006 and was omitted from these analyses. Further, in the 62-year-old cohort, 14 (3 males, 11 females) changed from being active in 1996 at age 62 to being inactive in 2001 at age 67, while the remaining 80 (42 males, 38 females) were inactive on both measurement occasions.
Multinomial regressions were conducted on each sleep problem measure that examined the factors of Age (57 or 62 on the first of the 2 measurement occasions considered), Activity Pattern (i.e., Active-Retired and Retired-Retired), and of Measurement Occasion (2 occasions in this case). Note that because of the small numbers in some of the cells, gender was ignored in these analyses. The results are shown in Table 4 from which it can be seen that only in the case of premature awakening was there any evidence of the interaction of interest, namely that between Activity Pattern and Measurement Occasion, which is present here in the 3-way interaction between Activity Pattern, Age, and Measurement Occasion. As can be seen in Figure 7, premature awakenings reduced in those who changed from being active to being retired from the first to the second measurement occasions, while they increased in the other group. The 3-way interaction reflected the fact that, among the Active-Retired subjects, the 62-year-old group received larger benefits of retirement than the 52-year-old group, maybe because their initial ratings of sleep difficulty were higher.
Table 4.
Summary of significance levels in multinomial logistic regression models of Age, Activity Pattern, and Measurement occasion for each of the sleep problem measures
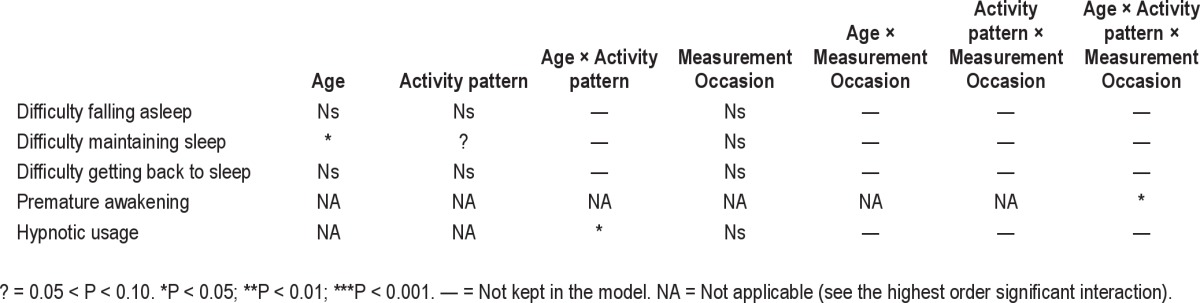
Figure 7.
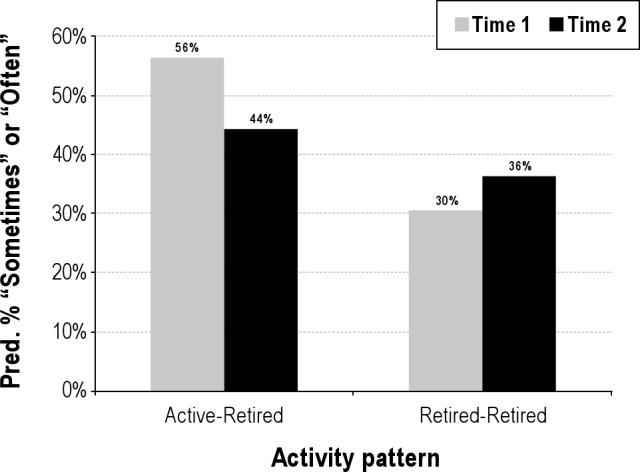
The interaction between activity pattern and measurement occasion for premature awakening (mean predicted % of “Sometimes” plus mean predicted % of “Often”).
DISCUSSION
The “cross-sequential” design of the VISAT study allowed us to identify clear evidence of a decade effect such that, after controlling for age, ratings of sleep complaint frequency made in 2006 were consistently higher than those made in 1996. While this is a major advantage of this type of design over more traditional longitudinal ones in which decade and ageing effects would be totally confounded, we are unable to distinguish between two potential interpretations. Our examination of the decade effect was necessarily confounded with measurement occasion, and hence we are unable to rule out the possibility that sleep complaint frequencies are simply rated as higher with repeated testing. An alternative interpretation is that it reflects a genuine decade effect, such that the population as a whole perceived themselves as suffering from more sleep problems in 2006 than they had a decade earlier in 1996. Such an effect might, for example, reflect on greater media coverage (and hence awareness) of sleep problems. The fact that the decade effect was only significant for difficulty falling asleep and maintaining sleep provides some support for an interpretation in terms of increased awareness or decreased tolerance of these sleep problems over time, as it would not be clear otherwise why repeated testing would only affect these two sleep problems.
Our main analyses examined the effects of age, gender, and working versus retired, but were unable to examine or control for other potential confounders such as sleep apnea. Nevertheless, the main results of this study clearly suggested that the perceived frequency of most sleep problems increased from the age of 32 to 52 but then remained relatively constant, or even reduced, up to the age of 72. It should be noted that the range of sleep problems addressed fall within subclinical levels of poor sleep quality, but we consider them important in view of their potential adverse effects on the workers’ quality of life and job security.
This pattern of increase and then stabilization in sleep complaints with age was observed for difficulty maintaining sleep, difficulty getting back to sleep, and premature awakening. For difficulty maintaining sleep our result contrasts with those of the cross-sectional study of Klink and Quan10 who reported that “disorders of intitiating and maintaining sleep” showed a fairly linear increase from < 40 years, through 40-64 years, to > 64 years. Our results suggest that difficulties in falling asleep and hypnotic usage regularly increase with age, whereas other sleep problem measures plateau, or even decline, after age 52. Comparing results between the two studies is, however, difficult due to the cross-sectional nature of the Klink and Quan study and their combining four sleep problem ratings similar to ours into a single score of “disorders of intitiating and maintaining sleep.”
Our results are, however, consistent with those of Doi et al.,11 who studied a middle-aged (20- to 59-year-old) sample of Japanese white-collar employees and found lower levels of complaints about sleep quality in people in their fifties than in younger people. In their study, again, sleep quality was assessed through a global score, namely the Pittsburgh sleep quality index, which does not provide information about which specific sleep difficulties are most affected with increased age. Further, Monk2 failed to show any age differences between young and older participants in sleep efficiency and perceived sleep quality in a sample of the same age-range, while all other subjectively (diary studies) and objectively (polysomnography) recorded sleep measures showed the expected sleep superiority of those in their twenties. This suggests that environmental factors (perhaps the occupational and non-occupational stress factors hypothesised by Doi et al.11) and the gradual adjustment of subjective criteria may influence the assessment of sleep quality.
In the present study, the clearest evidence for a reduction in the frequency of sleep complaints after age 52 was found for premature awakening, and it is noteable that this was the only measure in which we found evidence for an effect of retirement. Indeed, the magnitude of the effect of retirement was such that it might wholy account for the reduction after age 52 in this measure. Thus, from the age of 52 onwards, individuals reported little if any increase in the frequency of most of their sleep complaints, but were neverthless increasingly likely to report difficulty falling asleep and usage of hypnotic drugs.
The finding of a reduction in sleep complaints in the fifties and sixties is consistent with results obtained in two earlier studies, namely those of Kronholm and Hyyppa12 and the more recent longitudinal study of Vahtera et al.13 The latter study showed a substantial decrease in sleep disturbances over the 7 years studied after retirement, which was attributed to a combination of the removal from work-related harmful exposures and preretirement risk factors such as poor physical and mental health. This interpretation is supported by earlier studies suggesting that poor sleep, which is common in older people, may be secondary to comorbidities rather than to age per se.11,14
Our findings on the effect of retirement are perhaps the most interesting and extend those of Vahtera et al.13 by specifying which type of perceived sleep problem, namely premature awakening, is more likely to be affected by retirement, since they used a single item to assess overall sleep quality. However our findings are clearly limited by the relatively small numbers available to us when examining these effects. Nevertheless, they contrast with the findings of Ito et al.,15 who reported subjectively assessed sleep quality to be lower in retirees than still-employed individuals of the same age. However, the age of their sample (65-year-old residents of a Japanese city) suggests that this finding may have reflected a “healthy-survivor” effect, since those still employed at the age of 65 may be healthier than retirees of the same age.
With respect to gender, our findings are in agreement with those of earlier studies showing higher rates of sleep disturbances in women than in men.10,16–18 In the current study, women rated the frequency of their difficulties in falling asleep, maintaining sleep, and getting back to sleep as higher than males of the same age. As in earlier studies, women were also higher users of hypnotics than men in the present study.19,20 The gender difference was observed at all ages, indicating that although at a higher level, age-related changes in women’s sleep complaints are similar to those of men. The effect of gender on premature awakening differed as a function of age. In the youngest cohort, females reported more problems than males, but there were no gender differences in the other cohorts. One possibility is that the different pattern of results found for men and women in premature awakening reflects on women’s child care duties at younger ages.
The similar patterns observed in males and females later in life contrast with the findings of Vahtera et al.,13 who showed that sleep improved substantially less in retired women than in their male counterparts. Unfortunately, the size of the subsample used to analyze the retirement effect in the current study did not allow us to examine gender differences in this respect.
The results of this study revealed that the frequency of perceived sleep problems may start to increase in workers as early as in their thirties but then stabilizes, or even reduces, over subsequent decades for most of them. Retirement resulted in a reduced frequency of premature awakenings, while having little if any impact on the other sleep problems. Despite the stabilization of most sleep problems after age 52, the reported frequency of hypnotic usage continued to increase.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work was funded by grants from the French Agence Nationale de la Recherche (ANR 2006 SEST 041 01), the Institute of Occupational Safety – Health (United Kingdom), and the Direction Gáenáerale de la Santáe (DGS), la Caisse Nationale d’Assurance Maladie des Travailleurs Salariáes (CNAMTS), du Ráegime Social des Indáependants (RSI) et de la Caisse Nationale de Solidaritáe pour l’Autonomie (CNSA), as part of the call for projects launched by Institut de Recherche en Santáe Publique (IReSP) in 2009. We are grateful to the occupational physicians and other researchers of the VISAT group who contributed to the VISAT program. We also thank Catherine Gentil for her statistical assistance.
REFERENCES
- 1.Van Someren EJW. Circadian rhythms and sleep in human aging. Chronobiol Int. 2000;17:233–43. doi: 10.1081/cbi-100101046. [DOI] [PubMed] [Google Scholar]
- 2.Monk TH. Subjectively and objectively recorded sleep measures in the middle years of life. Trav Hum. 2003;67:7–19. [Google Scholar]
- 3.Carrier J, Monk TH, Buysse DJ, Kupfer DJ. Sleep and morningness-eveningness in the “middle” years of life (20y-50y) J Sleep Res. 1997;6:230–7. doi: 10.1111/j.1365-2869.1997.00230.x. [DOI] [PubMed] [Google Scholar]
- 4.Hüarmüa MI. Individual differences in tolerance to shiftwork: a review. Ergonomics. 1993;36:101–9. doi: 10.1080/00140139308967860. [DOI] [PubMed] [Google Scholar]
- 5.Cajochem C, Müunch M, Knoblauch V, Blatter K, Wirz-Justice A. Age-related changes in the circadian and homeostatic regulation of human sleep. Chronobiol Int. 2006;23:461–74. doi: 10.1080/07420520500545813. [DOI] [PubMed] [Google Scholar]
- 6.Marquiáe JC, Jansou P, Baracat B, et al. Ageing, health, work: overview and methodology of the VISAT prospective study. Trav Hum. 2002;65:243–60. [Google Scholar]
- 7.Mehra R. Retire for better sleep? Commentary on Vahtera et al. Sleep. 2009;32:1410–1. doi: 10.1093/sleep/32.11.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marquiáe JC, Foret J. Sleep, age, and shiftwork experience. J Sleep Res. 1999;8:297–304. doi: 10.1046/j.1365-2869.1999.00170.x. [DOI] [PubMed] [Google Scholar]
- 9.Kecklund G, Akerstedt T. The psychometric properties of the Karolinska Sleep Questionnaire. J Sleep Res. 1992;1(suppl1):113. [Google Scholar]
- 10.Klink M, Quan SF. Prevalence of reported disturbances in a general adult population and their relationship to obstructive airways diseases. Chest. 1987;91:540–6. doi: 10.1378/chest.91.4.540. [DOI] [PubMed] [Google Scholar]
- 11.Doi Y, Minowa M, Tango T. Impact and correlates of poor sleep quality in Japanese white-collar employees. Sleep. 2003;26:467–71. doi: 10.1093/sleep/26.4.467. [DOI] [PubMed] [Google Scholar]
- 12.Kronholm E, Hyyppa MT. Age-related sleep habits and retirement. Ann Clin Res. 1985;17:257–64. [PubMed] [Google Scholar]
- 13.Vahtera J, Westerlundt H, Hall M, et al. Effect of retirement on sleep disturbances: the GAZEL prospective cohort study. Sleep. 2009;32:1459–66. doi: 10.1093/sleep/32.11.1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults. Results of the 2003 National Sleep Foundation sleep in America survey. J Psychosom Res. 2004;56:497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 15.Ito Y, Tamakoshi A, Yamaki K, et al. Sleep disturbances and its correlates among elderly Japanese. Arch Gerontol Geriatr. 2000;30:85–100. doi: 10.1016/s0167-4943(99)00054-0. [DOI] [PubMed] [Google Scholar]
- 16.Leger D, Guilleminault C, Dreyfus JP, Delahaye C, Paillard M. Prevalence of insomnia in a survey of 12,778 adults in France. J Sleep Res. 2000;9:35–42. doi: 10.1046/j.1365-2869.2000.00178.x. [DOI] [PubMed] [Google Scholar]
- 17.Lindberg E, Janson C, Gislason T, Bjüornsson E, Hetta J, Boman G. Sleep disturbances in a young adult population: can gender differences be explained by differences in psychological status? Sleep. 1997;20:381–7. doi: 10.1093/sleep/20.6.381. [DOI] [PubMed] [Google Scholar]
- 18.Roth T. Prevalence, associated risks, and treatment patterns of insomnia. J Clin Psychiatry. 2005;66:10–3. [PubMed] [Google Scholar]
- 19.Jacquinet-Salord M, Lang T, Fouriaud C, Nicoulet I, Bingham A. Sleeping tablet consumption, self-reported quality of sleep, and working conditions. J Epidemiol Community Health. 1993;47:64–8. doi: 10.1136/jech.47.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quera-Salva MA, Orluc A, Goldenberg F, Guilleminault C. Insomnia and use of hypnotics: study of a French population. Sleep. 1991;14:386–91. doi: 10.1093/sleep/14.5.386. [DOI] [PubMed] [Google Scholar]


