Abstract
Study Objective:
This study evaluated the effect of accommodating adolescent sleep-wake patterns by altering the timing of the major sleep period of US Army recruits.
Design:
The quasi-experimental study compared recruits assigned to one of two training companies: one with a customary sleep regimen (20:30 to 04:30) while the other employed a phase-delayed sleep regimen (23:00 to 07:00), the latter aligning better with biologically driven sleep-wake patterns of adolescents.
Setting:
The study was conducted during Basic Combat Training (BCT) at Fort Leonard Wood, Missouri.
Trainees:
The study included 392 trainees: 209 received the intervention, while 183 composed the Comparison group.
Measurements and Results:
Demographic and psychophysiological measures were collected on all trainees. Weekly assessments of subjective fatigue and mood, periodic physical fitness, marksmanship scores, and attrition rates from BCT were studied. Actigraphy was collected on approximately 24% of trainees. Based on actigraphy, trainees on the phase-delayed sleep schedule obtained 31 m more sleep/night than trainees on the customary sleep schedule. The Intervention group reported less total mood disturbance relative to baseline. Improvements in marksmanship correlated positively with average nightly sleep during the preceding week when basic marksmanship skills were taught. No differences were seen in physical fitness or attrition rates. In contrast to the Intervention group, the Comparison group was 2.3 times more likely to experience occupationally significant fatigue and 5.5 times more likely to report poor sleep quality.
Conclusions:
Accommodating adolescent sleep patterns significantly improves mental health and performance in the training environment.
Citation:
Miller NL; Tvaryanas AP; Shattuck LG. Accommodating adolescent sleep-wake patterns: the effects of shifting the timing of sleep on training effectiveness. SLEEP 2012;35(8):1123-1136.
Keywords: Adolescent sleep patterns, learning and skill acquisition, timing of sleep, marksmanship, military training
INTRODUCTION
Obtaining adequate sleep is a challenge for those serving in the military and is especially difficult for individuals in military training environments. As today's military mission has grown increasingly complex, initial indoctrination and training curricula have responded by increasing the number of contact hours with recruits in an attempt to increase the amount of information and skills covered. All too often, this increased training time comes at the expense of sleep, as trainers attempt to squeeze more skills and information into a restricted time period.
Military training regimes often include some degree of sleep deprivation, whether it is by design or unintentional. Several studies have demonstrated that sleep deprivation is prevalent in military training and education programs. For example, Killgore et al.1 used actigraphy to determine sleep amounts in soldiers attending military training at the Noncommissioned Officer Academy and the Warrant Officer Candidate School. Their study found that these individuals obtained 5.8 h of sleep per night on average. Miller and colleagues2,3 reporting on the preliminary results of a 4-year longitudinal study of sleep in U.S. Military Academy (USMA) cadets based on actigraphy data, found that cadets averaged only 5.4 h of sleep per night. Additionally, once they report for their military education, cadets receive over 2 h less sleep per night than they did prior to their arrival at USMA.4 Findings from these training environments show that individuals in military training regimes receive considerably less than the 8 h of sleep per night recommended for healthy adults to maintain cognitive effectiveness.5
Almost all military recruits are adolescents or young adults in their late teens or early twenties, whose naturally occurring sleep-wake patterns often conflict with the organizational schedules of contemporary military training. When left to their own devices, these military recruits, like adolescents in the civilian population, experience delayed bedtimes, later awakenings, and longer sleep periods. Researchers have found a marked tendency for adolescents and young adults to go to bed later and to awaken much later than their adult counterparts, reflecting patterns in their naturally occurring melatonin levels.6–8 Since the majority of military recruits fall into this adolescent and young adult age group, they may actually require from 8.5 to 9.25 h of sleep per night for optimal performance. Throughout this paper, we refer to this requirement for additional sleep in the adolescent and young adult population as an “adolescent sleep/wake pattern,” acknowledging that these patterns extend into the early twenties for many individuals.
While adequate sleep is important for performance in any environment, it is crucial for individuals who are learning new skills and information. Sleep debt and fatigue accumulates with multiple nights of less than 8 h of sleep, with consequences such as decreased vigilance, adverse mood changes, perceptual and cognitive decrements, impaired judgment, and increased risk taking.9 Well-controlled laboratory experiments have demonstrated a convincing dose-response relationship between sleep deprivation and degraded cognitive performance.10–14 In two studies, sleep deprivation has also resulted in decreased marksmanship.15,16
In terms of academic performance, research has clearly demonstrated that the ability of individuals to learn and retain information is impaired by sleep deprivation. In particular, scientists have examined the critical role of sleep in memory consolidation and latent learning.17–20 This degraded ability of individuals to learn and retain information under sleep restriction is evident in military training environments. Andrews21 and Miller and colleagues22 conducted a retrospective comparison of the academic performance of Navy recruits before and after the training command leadership changed the sleep regimen from 6 to 8 h per night. On tests covering standardized instructional material, recruits who received 8 h of sleep per night scored 11% higher on average than their counterparts who received only 6 h of sleep.
In another study of performance in military training, Killgore and colleagues,23 evaluating the effectiveness of actigraphy as a predictor of cognitive performance, found significant positive correlations between academic exam scores in six military education programs (i.e., programs of instruction at the Noncommissioned Officer Academy and Warrant Officer Candidate School at Fort Rucker, AL) and the average hours of sleep per night and hours slept in the 24 and 48 h periods preceding an exam. They report that the average amount of sleep obtained by soldiers accounted for approximately 40% of the variance in exam scores—a finding that underscores the impact of fatigue on learning and memory. A similar result was reported by Trickel et al.,24 who found that sleep habits accounted for most of the variance in the academic performance of freshman college students.
Physical health is an equally important concern in military recruit populations, particularly because the close living conditions are conducive to the spread of communicable disease. Individual physical health, and in turn, public health, also depends on individuals receiving adequate amounts of sleep. Research has shown that disturbances of sleep-wake homeostasis are accompanied by alterations in the immunological, neuroendocrine, and thermoregulatory functions of the body, and hence, contribute to pathological processes such as infectious disease.25 Lange et al.26 also report that sleep enhances antibody production and the immune response to vaccination. Besides illness, sleep deprivation threatens health by increasing the risk for injuries resulting from accidents. For example, Thorne et al.27 demonstrated that frequency of accidents in a simulated driving task increased progressively as sleep duration decreased to 7, 5, and 3 h per night over a period of one week.
The Present Study
This study explored the influence of sleep scheduling on trainees' mastery of basic US Army standards and combat skills. The study also examined the direct effect of sleep scheduling on amount of sleep, mood state, performance in training, and physical fitness while controlling for such individual differences as sleep habits, personality, and personnel aptitudes.
Hypotheses
Given the preceding discussion, the following hypotheses guided this study:
Participants on the modified, phase-delayed sleep schedule would obtain more daily sleep than participants following the standard Basic Combat Training sleep schedule.
Participants on the modified sleep schedule would have less decrement in mood state than participants following the standard Basic Combat Training sleep schedule.
Participants on the modified sleep schedule would exhibit greater improvement in basic rifle marksmanship scores than participants following the standard Basic Combat Training sleep schedule.
Participants on the modified sleep schedule would exhibit greater improvement in physical fitness scores than participants following the standard Basic Combat Training sleep schedule.
The likelihood of participants on the modified sleep schedule reporting occupationally significant fatigue would be lower than that for participants following the standard Basic Combat Training sleep schedule.
The likelihood of participants on the modified sleep schedule reporting poor sleep quality would be lower than that for participants following the standard Basic Combat Training sleep schedule.
The likelihood of participants on the modified sleep schedule attriting from training would be lower than that for participants following the standard Basic Combat Training sleep schedule.
METHODS
Study Design
The study used a quasi-experimental design embedded within the existing U.S. Army's 63-d Basic Combat Training (BCT) program of instruction at Fort Leonard Wood, Missouri. The study protocol was approved by the Naval Postgraduate School Institutional Review Board. The Intervention and Comparison groups were selected without random assignment, although group assignment to the treatment condition was random. The research team took the groups as they were created by the U.S. Army based on their normal mode of operations for managing BCT. The intervention modified the timing of sleep and wake periods; no change was made to the content, instructional methods, or sequence of BCT events. The Intervention group used a phase-delayed (23:00-07:00) sleep regimen with midday naps when the opportunity presented, while the Comparison group maintained the standard (20:30-04:30) sleep regimen with limited opportunity for naps. The barracks used by the Intervention group were modified with blackout curtains to mitigate the effect of morning light; no modifications were made to the barracks used by the Comparison group, as their sleep occurred during natural darkness.
Data Collection Instruments and Study Variables
Actigraphy
All measures of sleep reported in this article were based on activity counts using wrist-worn actigraphic recording devices. Actigraphic recordings of 95 study trainees were made using the Actiwatch (Model AW-64, Philips Respironics, Bend, Oregon). Epoch length was set to one minute, and sensitivity used was the factory default settings.
Basic Rifle Marksmanship
Rifle marksmanship skill was assessed based on “record fire” scores. During a BCT record fire, trainees were given an M16/M4 series rifle and 40 rounds of ammunition and presented with 40 timed target exposures at ranges from 50 to 300 meters. While wearing a helmet and load-bearing equipment, 20 targets were engaged with 20 rounds from the prone supported position, 10 targets were engaged with 10 rounds from the prone unsupported position, and 10 targets were engaged with 10 rounds from the kneeling position. The standard was ≥ 23 target hits on the 40 targets exposed. Trainees completed a practice record fire on days 29 and 30 of BCT and an official record fire on day 32 of BCT, for a total of 3 sequential record fires.28
General Technical Aptitude
Objective evaluation of individual aptitude was made based on General Technical (GT) score as derived from the Armed Services Vocational Aptitude Battery (ASVAB). The ASVAB is a 216-item inventory containing 9 separately scored subtests: General Science, Arithmetic Reasoning, Word Knowledge, Paragraph Comprehension, Auto and Shop, Mathematics Knowledge, Mechanical Comprehension, Electronics Information, and Assembling Objects. The ASVAB is not an intelligence test, but rather is specifically designed to measure an individual's aptitude to be trained in specific jobs. GT score is a composite of the Arithmetic Reasoning, Word Knowledge, and Paragraph Comprehension subtests, and it is often a major determinant of the occupational specialty for which a person can be considered in the military.
Mood State
Subjective evaluation of mood was made with the Profile of Mood States (POMS).29 The POMS is a 65-item questionnaire that measures affect or mood on 6 scales: (1) tension-anxiety (T-factor), (2) depression-dejection (D-factor), (3) anger-hostility (A-factor), (4) vigor-activity (V-factor), (5) fatigue-inertia (F-factor), and (6) confusion-bewilderment (C-factor). An aggregate total mood disturbance (TMD) score is calculated by summing the scores on the 6 scales and negatively weighting the vigor-activity score.
Personality
A personality assessment was accomplished using the Neuroticism-Extroversion-Openness Five-Factor Inventory (NEO-FFI).30 The NEO-FFI is essentially a short form of the Revised NEO Personality Inventory (NEO-PI-R). It consists of 60 items from the NEO-PI-R that are used to score the 5 domains of personality: (1) neuroticism, (2) extraversion, (3) openness, (4) agreeableness, and (5) conscientiousness. It does not contain the items for assessing the facets within each domain. The NEO-FFI is designed for use in circumstances in which time is too limited to present the entire NEO-PI-R or only scores on the 5 domains are required.31
Physical Fitness
Objective evaluation of physical fitness was made based on Army Physical Fitness Test (APFT) score. Trainees completed a physical fitness assessment consisting of 3 measured events: push-ups, sit-ups, and a timed 2-mile run. Raw scores were scaled for both age and gender. Trainees must earn a score of ≥ 150 points on the end-of-training APFT with ≥ 50 points in each event to graduate from BCT.28 Trainees completed 2 diagnostic APFTs during the third and sixth weeks of BCT and a final APFT in the eighth week of training.
Resilience
Assessment of resilience to stress was accomplished using the Response to Stressful Experiences Scale (RSES).32 The RSES was developed by researchers with the National Center for Post Traumatic Stress Disorder to rate psychological traits that promote resilience, which is the ability to undergo stress and still retain mental health and well-being. It consists of 22 items and identifies 6 factors that are key to psychological resilience: (1) positive outlook, (2) spirituality, (3) active coping, (4) self-confidence, (5) learning and making meaning, and (6) acceptance of limits. The RSES, while not a thoroughly validated instrument, has been tested on more than 1,000 active-duty military personnel and is gaining greater acceptance in the research community.33
Sleep Habits
Subjective assessments of sleep habits were made using 3 validated survey instruments. The first instrument was the Pittsburgh Sleep Quality Index (PSQI), a self-rated questionnaire designed to measure sleep quality in clinical populations by looking at sleep in the previous month. Nineteen individual items generate the following 7 scores: (1) subjective sleep quality, (2) sleep latency, (3) sleep duration, (4) habitual sleep efficiency, (5) sleep disturbances, (6) use of sleeping medications, and (7) daytime dysfunction. A review of this survey's reliability asserts that the PSQI is useful in both psychiatric clinical practice and research activities.34
The second instrument was the Epworth Sleepiness Scale (ESS),35 an 8-item scale commonly used to diagnose sleep disorders and considered a valid and reliable self-report of sleepiness. Respondents use an integer number from 0 to 3, corresponding to the likelihood (never, slight, moderate, and high, respectively) that they would fall asleep in 8 situations such as sitting and reading, watching television, or as a passenger in a car for an hour. Cumulative ratings above 10 out of a possible 24 are cause for referral for evaluation for an underlying sleep disorder.
The third instrument was the Morningness-Eveningness Questionnaire (MEQ) published by Horne and Ostberg,36 which contains 19 questions aimed at determining when, during the daily temporal span, individuals have the maximum propensity to be active. Most questions are preferential, in the sense that the respondent is asked to indicate when they would prefer, rather than when they actually do, wake up or begin sleep. Questions are multiple-choice; each answer is assigned a value such that their sum gives a score ranging from 16 to 86, with lower values corresponding to evening chronotypes and higher values indicating morning chronotypes.
Study Questionnaire
The study questionnaire contained 10 questions aimed to capture information about potential covariates that could influence study outcomes. The first four questions asked trainees for their age, sex, height, and weight. One question asked trainees to quantify their frequency of exercise during the preceding month, both in terms of the number and duration of exercise sessions. Another question asked whether trainees regularly used firearm(s), and if so, to characterize the type of firearm(s), reason(s) for use, and frequency of use. Three questions addressed the use of caffeinated beverages, tobacco, and medications. The last question asked trainees to quantify the amount of sleep per day they required to feel ready to start the day.
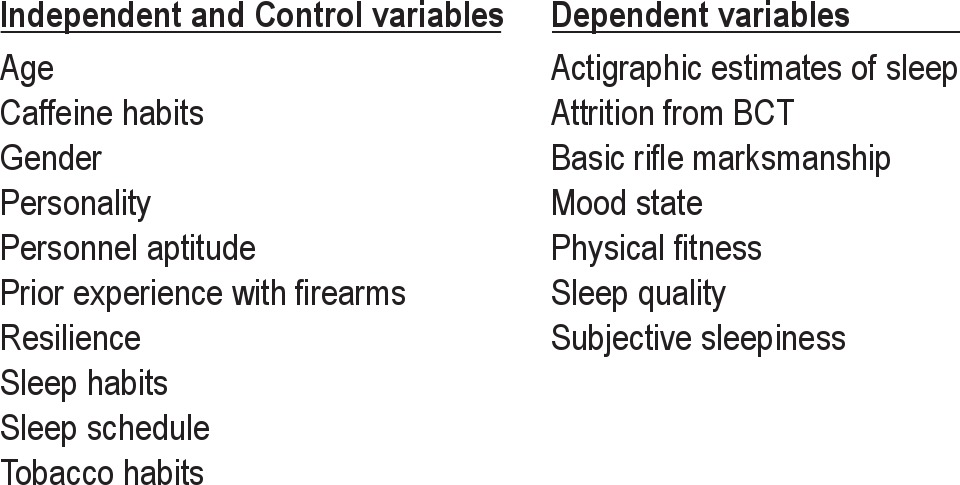
Table 1 lists covariates of the study, i.e., factors which are assumed to play a role in daytime functioning. The inclusion of these individual characteristics was important to this study because we predicted that the timing of sleep would have a small but measurable influence on daytime functioning, even after controlling for the contributions of the usual variables thought to affect mood state and performance.
Table 1.
Study variables
Procedures
General
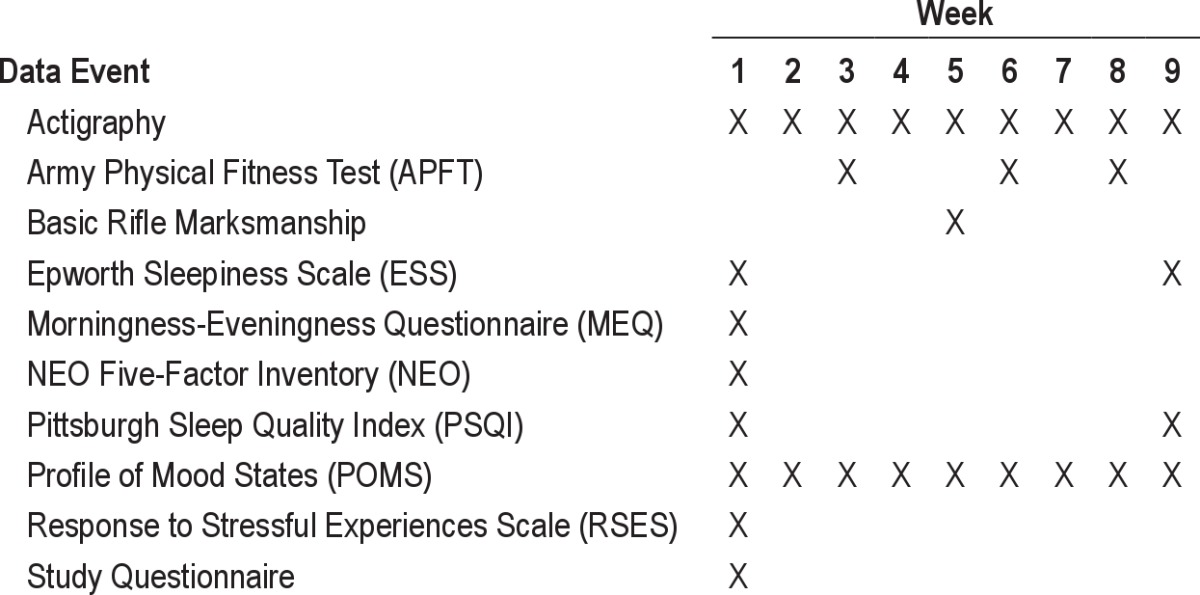
Prior to beginning the study, each trainee was briefed on the purposes of the study and assurances given about the confidentiality of their data. Once informed consent was obtained, each trainee completed the pre-study questionnaire followed by the ESS, PSQI, MEQ, RSES, POMS, and NEO-FFI (Table 2). At weekly intervals, study participants were asked to identify their mood state over the prior week of training. Mood state was defined by the 6 general factors identified in the POMS.29 The study also examined 3 major performance outcomes of concern to the military training organization: attrition, basic rifle marksmanship, and physical fitness. Table 2 shows the schedule followed for data collection.
Table 2.
Data collection schedule
Actigraphy
A random sample of 20% of the participants in both study groups was selected for actigraphic data collection. Trainees agreeing to actigraphic data collection were issued an Actiwatch on Day 1 to track sleep and activity patterns. They were asked to wear the Actiwatch continuously on the wrist of their nondominant hand during all waking and sleeping periods and not to remove it for showering. Actigraphic epoch length was set to one minute. Participants turned in their Actiwatches during Week 4 (Intervention group) or Week 5 (Comparison group) for downloading of data and reinitialization of the devices. Once the BCT period was complete, the remaining data were downloaded and analyzed using the Actiware version 5.57.0006 software with factory default settings.
Statistical Analysis
Microsoft Office Excel 2007 was used to populate the study database. All data were analyzed with the Statistical Package for the Social Sciences (SPSS) version 11. Separate univariate and repeated measures analyses of covariance (ANCOVAs) were used to test major hypotheses involving measures with one dependent variable. Repeated measures were analyzed using a univariate approach with a fixed effect for time when there were a substantial number of unit nonresponses, thereby reducing the danger of biased repeated measures estimates of treatment effects caused by ignoring records with missing responses.37,38 ANCOVA results were examined to determine whether there were sphericity violations of sufficient magnitude to warrant the use of Huynh-Feldt adjusted degrees of freedom. Multivariate analysis of covariance (MANCOVA) was used to test hypotheses involving measures with more than one dependent variable. Box's and Levene's tests were used to assure the multivariate assumptions of equality of covariance matrices and that equality of error variances across groups were not violated. Logistic regression was used to test major hypotheses involving measures with a binary dependent variable.
RESULTS
Descriptive Statistics
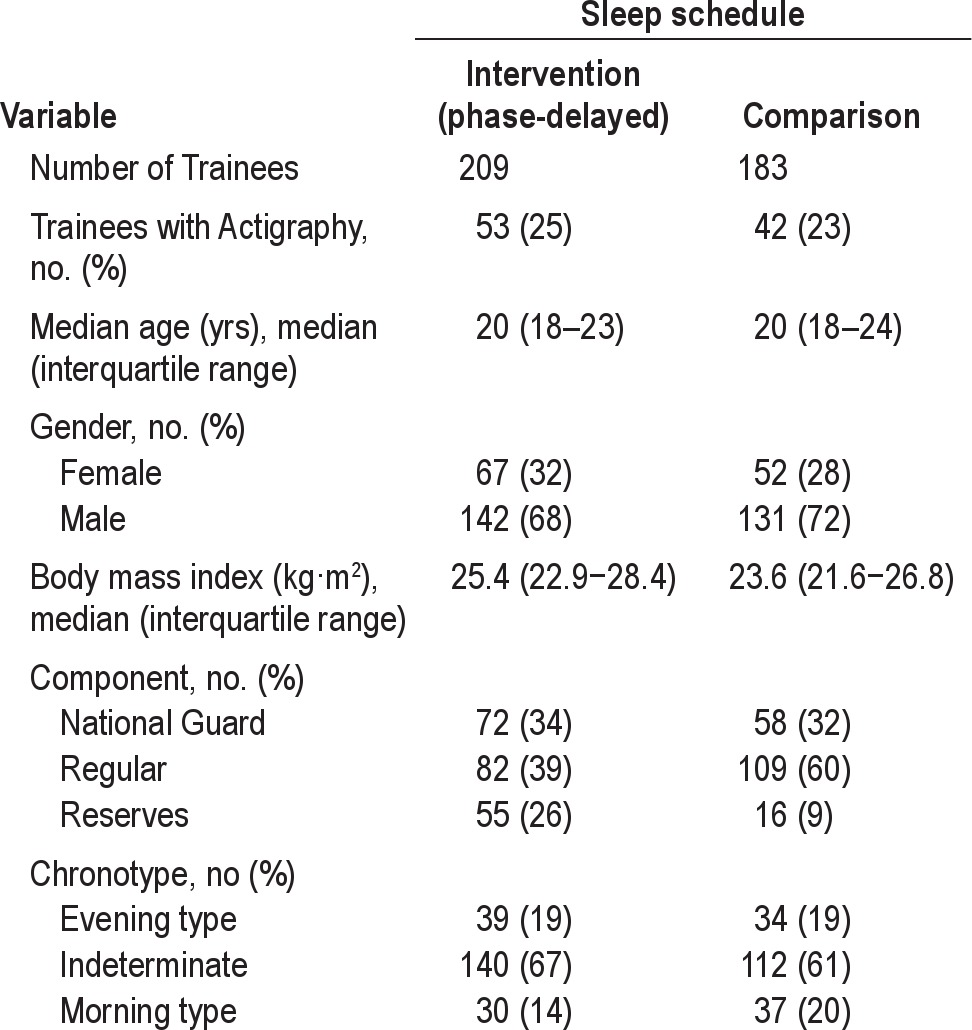
Table 3 displays descriptive statistics among variables in the study. At the start of the study, participants in the two training companies were fairly comparable. However, participants in the Intervention group tended to have a higher body mass index (BMI) (Mann Whitney U = 15461, P = 0.002) and were more likely to be entering the National Guard/Reserves (χ2 (2df) = 25.111, P < 0.001) at the outset of the study.
Table 3.
Description of the two companies at outset of study
Actigraphy Data
Histograms were developed for the actigraphy data by study group using all daily observations that were obtained. A total of 2968 observations were available for participants in the Intervention group; 2146 observations were available for participants in the Comparison group. Based on these observations, it was determined that nightly sleep episodes in the Intervention group tended to be longer (mean 5.889 ± 1.208 h, median 6.050 h) than those in the Comparison group (mean 5.333 ± 1.176 h, median 5.417 h), a statistically significant difference (P < 0.001 based on Mann Whitney U test). Sleep efficiency was calculated as the ratio of a participant's total sleep time to total time in bed; it represents the proportion of time that a participant was assumed to be “in bed” or attempting sleep that was actually spent asleep. Sleep efficiency for participants in the Intervention group (mean 0.821 ± 0.101, median 0.841) was similar to that in the Comparison group (mean 0.812 ± 0.099, median 0.831). Activity counts reflect movements during sleep and may be a function of the stage of sleep. Mean activity counts for participants in the Intervention group (mean 66.682 ± 110.704, median 30.566) were also similar to those in the Comparison group (68.161 ± 81.591, median 35.038). Naps were not included in the sleep analysis for either the Intervention or Comparison group because operational requirements provided few opportunities for either group to nap.
Hypothesis Testing
Sleep
The relationship between daily total sleep (based on actigraphy) and treatment condition over the course of BCT was examined while accounting for potential covariates and the aforementioned differences between the study groups. However, any approach to analyzing total sleep time needed to address the issue that participants did not necessarily have valid Actiware scores for every day of BCT. This issue was remedied by first computing a weekly average sleep for each participant and then analyzing the dataset as a repeated cross-section design rather than a within-participant repeated measures design. A 1% significance level (α 0.01) was also used to decrease the probability of a type I error (i.e., mistakenly rejecting the null hypothesis). Table 4 provides the results of the univariate analysis of weekly average sleep.
Table 4.
Univariate tests for weekly average sleep (estimated using actigraphy)
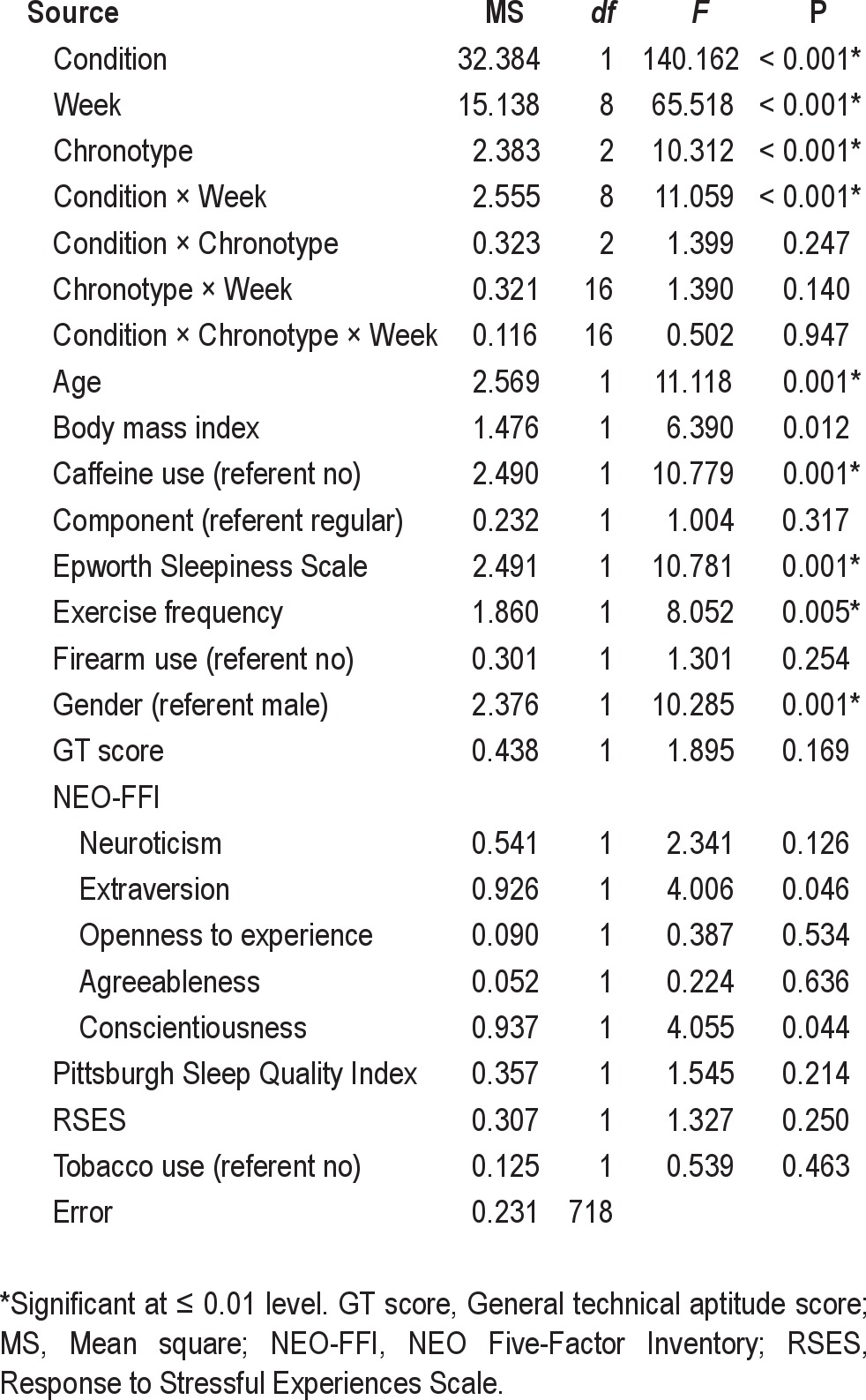
Hypothesis 1 predicted that trainees on the modified, phase-delayed sleep schedule would obtain more daily sleep than trainees following the standard schedule. This hypothesis was supported (F1,718 = 140.162, P < 0.001). The estimated marginal mean sleep for the Intervention group was 5.876 h (99% CI: 5.806, 5.945) versus 5.359 h (99% CI: 5.276, 5.442) for the Comparison group. That is, controlling for other variables, the Intervention group obtained 31 min more sleep than the Comparison group.
There was also a significant fixed effect of circadian chronotype (F2,718 = 10.312, P < 0.001), with differences in sleep occurring between morning chronotype (mean 5.767 h, 99% CI: 5.652, 5.882) versus both evening (mean 5.515 h, 99% CI: 5.422, 5.607) and indeterminate chronotypes (mean 5.570 h, 99% CI: 5.508, 5.635). That is, morning-type participants obtained significantly more sleep than participants in either of the other 2 categories.
As displayed in Figure 1, sleep differed across weeks of BCT (F8,718 = 65.518, P < 0.001), and there was a significant interaction effect between treatment condition and week (F8,718 = 11.059, P < 0.001), with participants in the Intervention group getting more sleep than those in the Comparison group during the first 6 weeks of training. During the latter 3 weeks of training, participants in the Intervention group got considerably less sleep than they had received before, such that there was no longer a difference in sleep amount between the Intervention and Comparison groups for the final 3 weeks in BCT. This pattern was attributed to the field training that was conducted during weeks 6, 8, and 9. Both groups spent the first part of week 6 in the field where they ate, trained and slept. Some of their training was conducted at night which accounts for the drop in sleep shown in Figure 1 (week 6). During week 7, both groups returned to their normal garrison routines and slept in the barracks. During week 8 and the first part of week 9, both groups were on field exercises again. The drop in sleep during weeks 8 and 9 occurred because the groups were required to stand guard duty at night while they were in the field. A minimum of 25% of each group had to be awake at any given time.
Figure 1.
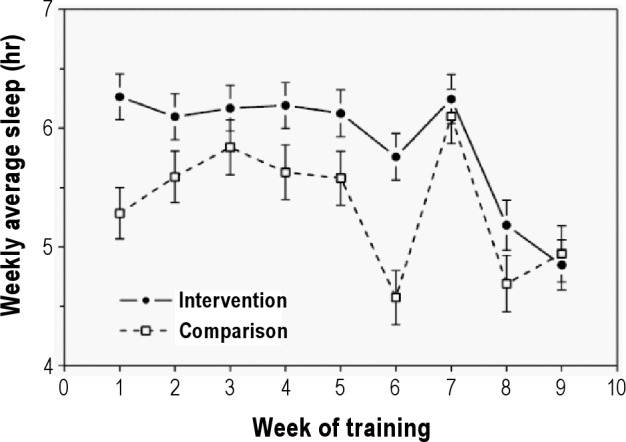
Estimated marginal means for average weekly sleep at night by treatment condition and week of training (error bars are for 99% confidence intervals).
Profile of Mood States
The relationship between mood and treatment condition over the course of BCT was examined while accounting for potential covariates and the known differences between the study groups. However, any approach to modeling the POMS factor scores needed to address several issues. First, a MANCOVA of the pre-study POMS factor scores found a significant effect for treatment condition (Wilks' λ = 0.769, F6,367 = 18.393, P < 0.001), suggesting that the 2 groups were not directly comparable at baseline in terms of subjective mood (further analysis and displays of the results are available in the full technical report, which can be downloaded from http://faculty.nps.edu/nlmiller/docs/NPS-OR-10-011_Signed.pdf).39 This issue was remedied by calculating the “delta from baseline” score for each factor—that is, subtracting a participant's pre-study POMS factor score from all their subsequent POMS factor scores. This subtraction had the effect of making all participants' pre-study POMS factor scores zero, while still preserving the magnitude and directionality of variations in their subsequent POMS factor scores. Another issue was the observation that most participants (70.4%) did not have a POMS questionnaire for every week of training. This issue was addressed by analyzing the POMS dataset as a repeated cross-section design rather than a within-participant repeated measures design and using a 1% significance level to decrease the probability of a type I error. Table 5 provides the results of the multivariate analysis of the POMS delta from baseline factor scores.
Table 5.
Multivariate tests for POMS delta from baseline factor scores
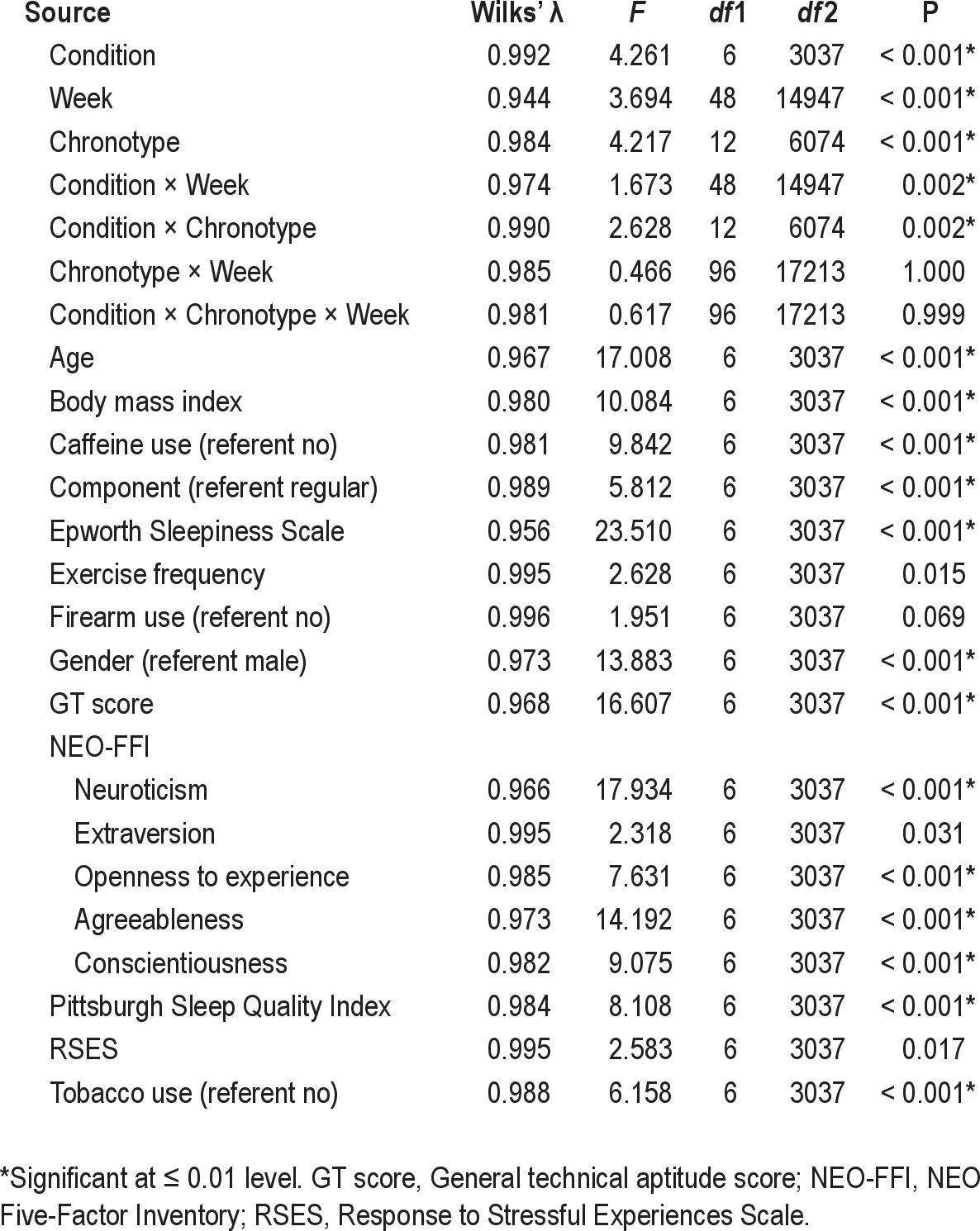
Hypothesis 2 predicted that trainees on the modified, phase-delayed sleep schedule would have less decrement in mood state than trainees following the standard schedule. This hypothesis was partially supported (Wilks' λ = 0.992, F6,3037 = 4.261, P < 0.001), with subsequent univariate tests revealing a significant fixed effect for treatment condition only for the POMS vigor-activity (V-factor) (F1,3042 = 10.232, P = 0.001). The estimated marginal mean V-factor score for the Intervention group was 1.229 (99% CI: 0.830, 1.628) versus 0.098 (99% CI: −0.347, 0.543) for the Comparison group. That is, controlling for other variables, the Intervention group exhibited a mood of greater relative vigor and ebullience and higher energy than the Comparison group.
There was a significant fixed effect of week of training on mood (Wilks' λ = 0.944, F48,14947 = 3.694, P < 0.001). Subsequent univariate analyses revealed that, irrespective of treatment condition, the general trend was for participants to report decreased feelings of tension-anxiety (T-factor) (F8,3042 = 7.521, P < 0.001), depression-dejection (D-factor) (F8,3042 = 9.015, P < 0.001), anger-hostility (A-factor) (F8,3042 = 8.172, P < 0.001), fatigue-inertia (F-factor) (F8,3042 = 10.362, P < 0.001), and confusion-bewilderment (C-factor) (F8,3042 = 11.383, P < 0.001) over the course of BCT. In contrast, there was no effect of week of training on vigor-activity. Further details of the univariate analyses are available in the aforementioned on-line technical report.39
There was a significant fixed effect of chronotype on mood (Wilks' λ = 0.984, F12,6074 = 4.217, P < 0.001), with subsequent univariate analyses revealing an effect for chronotype only for POMS vigor-activity (F2,3042 = 14.911, P < 0.001). The estimated marginal mean V-factor score for evening chronotype was 1.881 (99% CI: 1.193, 2.569) versus 0.240 (99% CI: −0.126, 0.605) for indeterminate and 0.761 (99% CI: 0.006, 1.516) for morning chronotypes. Thus the significant difference was between evening and indeterminate chronotypes.
There were significant interaction effects between treatment condition and week (Wilks' λ = 0.974, F48,14947 = 1.673, P = 0.002). Subsequent univariate analyses revealed significant interaction effects between treatment condition and week for POMS anger-hostility (F8,3042 = 2.676, P = 0.006) and fatigue-inertia (F8,3042 = 4.217, P < 0.001) scores. In the case of the treatment condition and week interaction, the Comparison group started out with higher delta from baseline scores on the A-factor and F-factor but had a greater rate of decrease in scores over training as compared to the Intervention group.
A similar analysis was conducted for the subsample of participants for whom actigraphy data was available. Again, a multivariate analysis of the POMS delta from baseline factor scores was accomplished using treatment condition, chronotype, and week of training as fixed effects and including average weekly sleep as a covariate (Table 6). There was no significant fixed effect of treatment condition or week, but there was a significant fixed effect of chronotype (Wilks' λ = 0.863, F12,1372 = 8.749, P < 0.001) as well as a significant interaction effect between treatment condition and chronotype (Wilks' λ = 0.874, F12,1372 = 7.945, P < 0.001). There was also a significant multivariate effect of the covariate (Wilks' λ = 0.971, F6,686 = 3.458, P = 0.002), average weekly sleep, but the covariate was not significant in any of the subsequent univariate tests.
Table 6.
Multivariate tests for POMS delta from baseline scores for actigraphy subsample
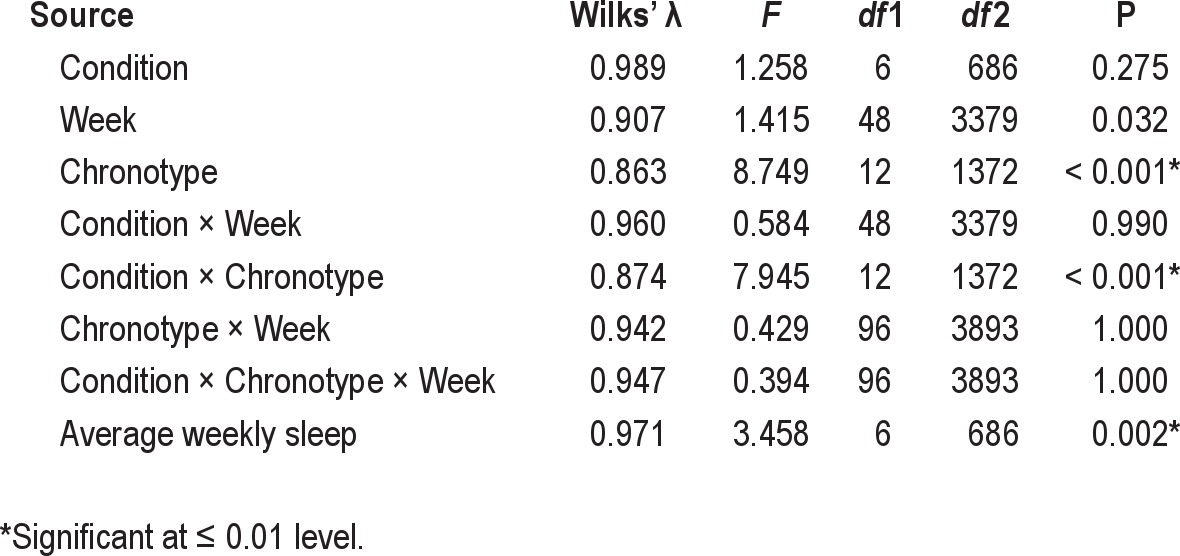
The analysis of the respective univariate tests revealed significant fixed effects of chronotype for T-factor (F2,691 = 15.888, P < 0.001), D-factor (F2,691 = 14.710, P < 0.001), A-factor (F2,691 = 9.508, P < 0.001), V-factor (F2,691 = 7.730, P < 0.001), F-factor (F2,691 = 16.262, P < 0.001), and C-factor (F2,691 = 21.489, P < 0.001). The pattern of differences between chronotypes varied across the POMS factors; the interested reader should refer to the aforementioned on-line technical report for further analysis and displays of the results.
The univariate tests also revealed significant interaction effects between treatment condition and chronotype for T-factor (F2,691 = 14.882, P < 0.001), D-factor (F2,691 = 18.472, P < 0.001), A-factor (F2,691 = 6.264, P = 0.002), V-factor (F2,691 = 9.716, P < 0.001), and C-factor (F2,691 = 19.404, P < 0.001). Again, the interested reader is referred to the on-line full technical report for further analysis and displays of the results.39
Basic Rifle Marksmanship
Hypothesis 3 predicted that trainees on the modified sleep schedule would exhibit greater improvement in basic rifle marksmanship scores than trainees following the standard sleep schedule. This hypothesis was supported indirectly after accounting for initial differences between the groups and addressing the variability in the number of record fires accomplished by each participant.
A total of 372 participants, 201 in the Intervention group (90% of the initial cohort) and 171 in the Comparison group (87% of the initial cohort), had ≥ 2 observations recorded in the marksmanship databases. Because not every participant accomplished the available maximum number of record fires, marksmanship scores were analyzed using a simple pre/post repeated measures design in which the first recorded marksmanship score for each participant was denoted as the initial score and the last score was denoted as the final score. A repeated-measures ANCOVA of marksmanship score was accomplished using practice as a within-participant effect and treatment condition and chronotype as fixed between-participant effects. Given the smaller number of observations, a 5% significance level (or α 0.05) was used for the subsequent analyses.
There was no significant within-participant effect for practice or an interaction effect between practice and chronotype. However, there was a significant interaction effect between practice and treatment condition (F1,313 = 9.737, P = 0.002). The analysis revealed that the Intervention and Comparison groups differed from each other on their initial score, with a mean marksmanship score for the Intervention group of 22.565 (95% CI: 21.384, 23.745) versus 25.876 (95% CI: 24.600, 27.152) for the Comparison group. Participants in the Intervention group had greater improvement in marksmanship scores with practice, such that their final scores were equivalent to those of participants in the Comparison group (Intervention group mean score 27.184 [95% CI: 26.124, 28.235]; Comparison group mean score 26.974 [95% CI: 25.833, 28.115]). In terms of between-participant effects, there was a significant fixed effect for treatment condition (F1,313 = 4.183, P = 0.042), with an estimated marginal mean score for the Intervention group of 24.872 (95% CI: 23.973, 25.453) versus 26.425 (95% CI: 25.772, 27.397) for the Comparison group. The fixed effect of chronotype was not significant, nor was there an interaction effect between treatment condition and chronotype. The only significant covariates were prior use of firearms (F1,313 = 4.719, P = 0.031) and gender (F1,313 = 11.838, P = 0.001).
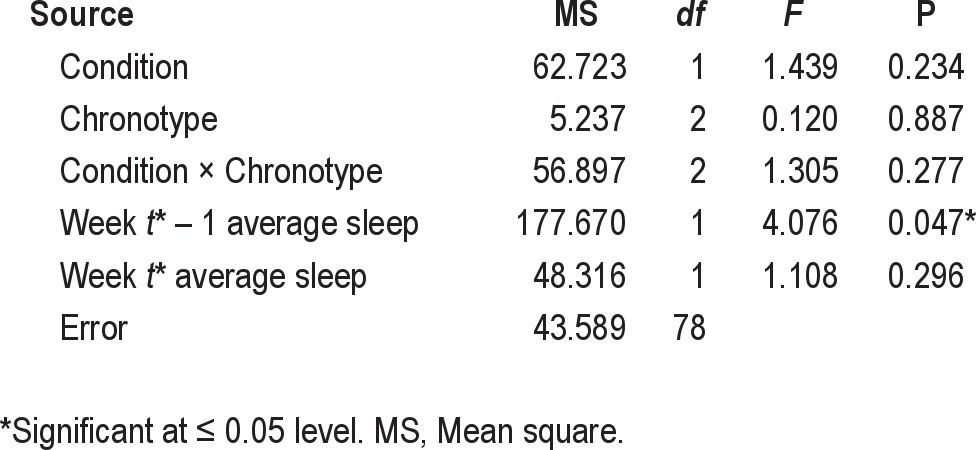
A similar analysis was conducted for the subsample of participants for whom actigraphy data was available. Again, a repeated-measures ANCOVA of marksmanship score was accomplished using practice as a within-participant effect and treatment condition and chronotype as fixed between-participant effects. Since marksmanship fundamentals were taught during the week prior to the record fires, the average hours slept during the week prior to (t* − 1) and the week of (t*) the record fires were used as the covariates. A total of 90 participants, 52 (98% of the initial sub-cohort) in the Intervention group and 38 (93% of the initial sub-cohort) in the Comparison group, had ≥ 2 observations recorded in the marksmanship databases.
There was no significant within-participant effect for practice or an interaction effect between practice and chronotype, but there was a significant interaction effect between practice and treatment condition (F1,78 = 6.003, P = 0.017). In contrast to the earlier analysis, these groups did not differ in terms of mean initial marksmanship scores (Intervention group mean score 21.450 [95% CI: 19.264, 23.636]; Comparison group mean score 25.119 [95% CI: 22.627, 27.612]) and final marksmanship scores (Intervention group mean score 26.792 [95% CI: 25.162, 28.421]; Comparison group mean score 26.316 [95% CI: 24.458, 28.173]). However, there was a trend for participants in the Intervention group to improve more with practice than participants in the Comparison group. In terms of the between-participant model (Table 7), there was no significant fixed effect of treatment condition in the presence of the sleep covariates. Additionally, there was no significant fixed effect for chronotype, nor was there an interaction effect between treatment condition and chronotype. There was, however, a significant effect for the covariate, week t* − 1 average sleep (F1,78 = 4.076, P = 0.047), but not week t* average sleep. The degree of improvement in performance over serial record fires was positively correlated (r = 0.341, P = 0.001) with average sleep during the week preceding the record fires, when the basic rifle marksmanship tasks were being learned. Further analysis and displays of the results are available from the aforementioned on-line technical report.39
Table 7.
Between-participant effects for marksmanship score for the actigraphy subsample
Physical Fitness
Hypothesis 4 predicted that trainees on the modified phase-delayed sleep schedule would exhibit greater improvement in physical fitness scores than trainees following the standard sleep schedule. This hypothesis was not supported. The analysis revealed that the Intervention and Comparison groups differed from each other on their initial fitness at week 3, with a mean fitness score for the Intervention group of 197.140 (99% CI: 187.532, 206.748) versus 220.749 (99% CI: 211.643, 229.855) for the Comparison group. While the Intervention group did improve such that the 2 groups did not differ on the subsequent 2 fitness tests at weeks 6 and 8, analysis of the subsample of participants for which actigraphy data were available revealed no correlation between average nightly sleep per week and fitness scores. Consequently, the differences observed in the pattern of the results of the physical fitness data were concluded to be a “regression to the mean” phenomenon, whereby physical conditioning was most effective in those who were most out of shape. Further analysis and displays of results for the physical fitness data are available in the aforementioned on-line technical report.39
Sleep Survey Instruments
Both the pre-study and post-study questionnaires assessed participant sleep using 2 standardized survey instruments: the ESS and the PSQI. The effect of the treatment intervention on ESS and PSQI scores was assessed using a pre/post study design. Because of participant attrition, there were missing post-study questionnaires for 44 participants (21%) in the Intervention group and 31 participants (17%) in the Comparison group. Given the smaller number of observations, a 5% significance level (or α 0.05) was used for the subsequent analyses.
Hypothesis 5 predicted that the likelihood of trainees on the modified sleep schedule reporting occupationally significant fatigue would be lower than that for trainees following the standard sleep schedule. This hypothesis was supported. Scores > 10 on the ESS are indicative of excessive sleepiness and are a cause for concern with respect to performance. Applying this standard to the study sample, the odds ratio for a participant reporting excessive sleepiness being in the Comparison relative to the Intervention group was 1.198 (95% CI: 0.765, 1.874) prior to training and 2.331 (95% CI: 1.478, 3.679) at the completion of training. There was no difference in the odds of participants in the Intervention and Comparison groups being excessively sleepy at the start of training. However, participants in the Comparison group were approximately 1.5 to 3.5 times more likely to be excessively sleepy by the conclusion of training, indicative of their sleep debt accrual throughout the course of BCT.
A repeated measures ANCOVA of ESS scores was accomplished using time as a within-participant effect and treatment condition and chronotype as fixed between-participant effects. There was no significant within-participant effect of time, nor was there a significant interaction effect between time and chronotype. There was a significant interaction effect between time and treatment condition (F1,296 = 18.943, P < 0.001). ESS scores increased significantly for participants in the Comparison group over the course of training (pre-training mean score 8.829 [95% CI: 8.116, 9.541]; post-training mean score 13.654 [95% CI: 12.750, 14.559]) but remained unchanged for those in the Intervention group (pre-training mean score 8.189 [95% CI: 7.438, 8.940]; post-training mean score 9.768 [95% CI: 8.815, 10.721]). Consequently, the groups' mean scores differed significantly at the post-study assessment with the Comparison group reporting greater sleepiness than their counterparts in the Intervention group.
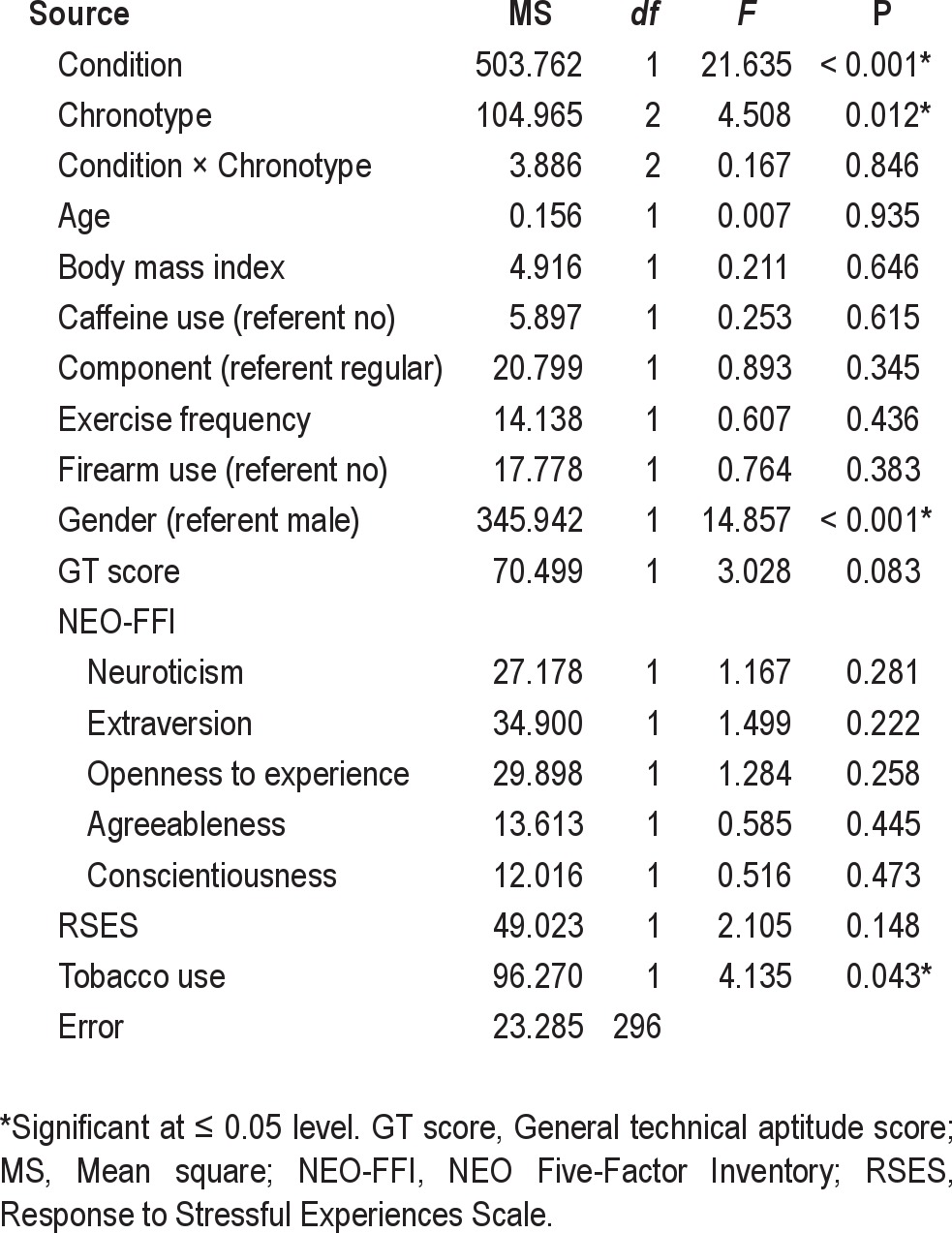
Table 8 provides the results of the analysis of between-participant effects for ESS scores. There was a significant fixed effect of treatment condition (F1,296 = 21.635, P < 0.001), with an estimated marginal mean ESS score of 8.978 (95% CI: 8.297, 9.659) in the Intervention group versus 11.242 (95% CI: 10.595, 11.888) in the Comparison group. There was also a significant fixed effect of chronotype (F2,296 = 4.508, P = 0.012) with the difference in ESS score occurring between evening and morning chronotypes: evening chronotype mean score 11.077 (95% CI: 10.151, 12.003), indeterminate chronotype mean score 10.243 (95% CI: 9.770, 10,717), and morning chronotype mean score 9.010 (95% CI: 8.040, 9.972).
Table 8.
Between-participant effects for Epworth Sleepiness Scale score
Hypothesis 6 predicted that the likelihood of trainees on the modified sleep schedule reporting poor sleep quality would be lower than that for trainees following the standard sleep schedule. This hypothesis was supported. Scores > 5 on the PSQI are indicative of poor sleep quality. Applying this standard to the study sample, the odds ratio for a participant having poor quality sleep being in the Comparison relative to the Intervention group was 1.684 (95% CI: 1.106, 2.565) prior to training and 5.477 (95% CI: 3.343, 8.972) at the completion of training. Moreover, the odds of a participant having poor sleep quality decreased in the Intervention group from pre-training (odds = 0.791; 95% CI: 0.659, 0.950) to post-training (odds = 0.470; 95% CI: 0.377, 0.586). In contrast, the odds of a participant having poor sleep quality increased in the Comparison group from pre-training (odds = 1.332; 95% CI: 1.047, 1.696) to post-training (odds = 2.574; 95% CI: 1.889, 2.509).
A repeated measures ANCOVA of PSQI scores was accomplished using time as a within-participant effect and treatment condition and chronotype as fixed between-participant effects. There was no significant within-participant effect of time, nor was there a significant interaction effect between time and chronotype. There was a significant interaction effect between time and treatment condition (F1,296 = 24.125, P < 0.001). PSQI scores increased significantly for participants in the Comparison group over the course of training (pre-training mean score 6.853 [95% CI: 6.304, 7.401]; post-training mean score 8.226 [95% CI: 7.668, 8.785]) and decreased significantly for those in the Intervention group (pre-training mean score 6.684 [95% CI: 6.106, 7.262]; post-training mean score 5.481 [95% CI: 4.893, 6.069]). Consequently, the groups' mean scores differed significantly at the post-study assessment, with the Comparison group reporting poorer sleep quality than their counterparts in the Intervention group.
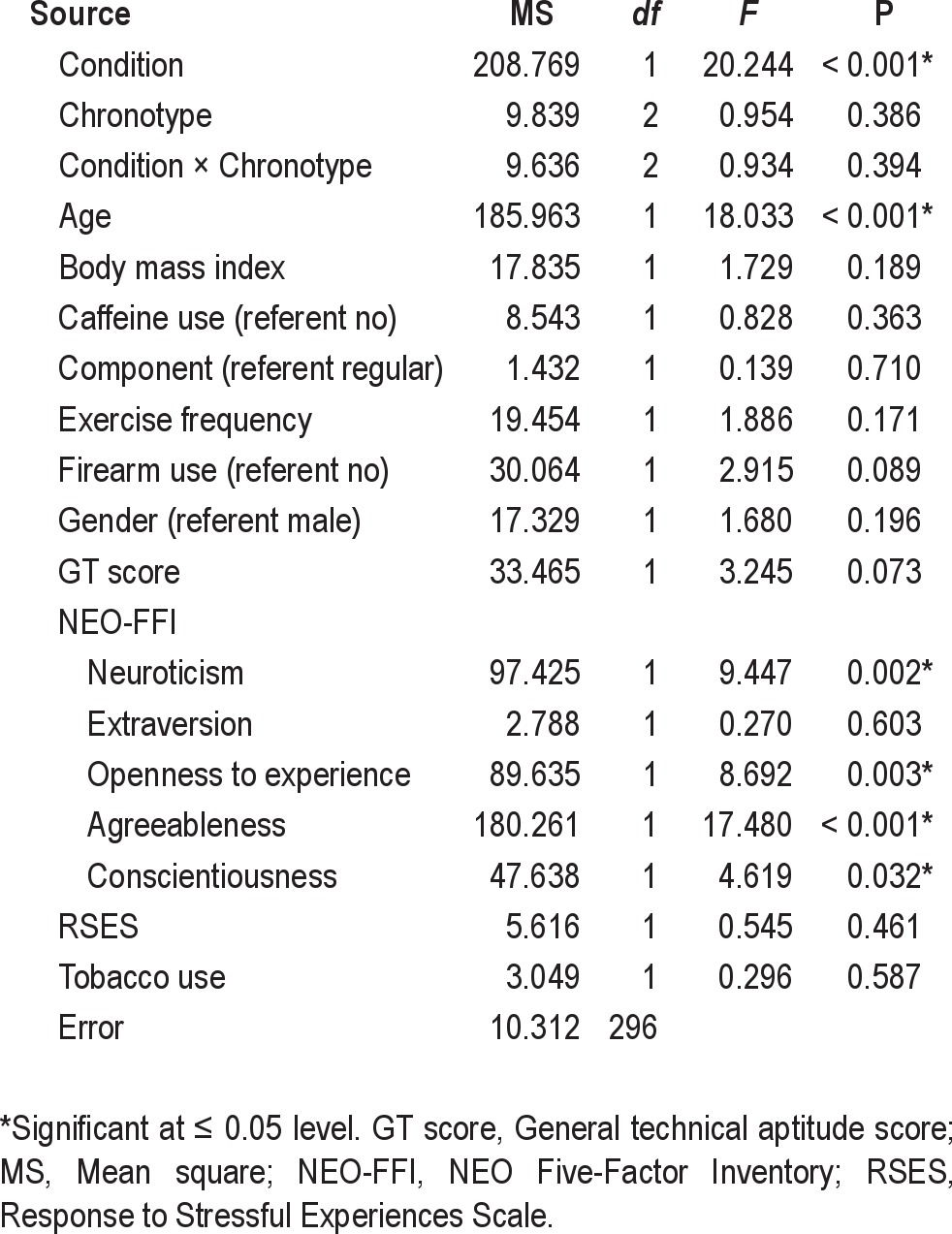
Table 9 displays the results of the analysis of between-participant effects for PSQI scores. There was a significant fixed effect of treatment condition (F1,296 = 20.244, P < 0.001), with an estimated marginal mean PSQI score of 6.082 (95% CI: 5.629, 6.536) in the Intervention group versus 7.539 (95% CI: 7.109, 7.970) in the Comparison group. There was no significant fixed effect of chronotype, nor was there a significant interaction effect between treatment condition and chronotype.
Table 9.
Between-participant effects for Pittsburgh Sleep Quality Index score
Attrition
Hypothesis 7 predicted that the likelihood of trainees on the modified sleep schedule attriting from training would be lower than that for trainees following the standard sleep schedule. This hypothesis was not supported. Overall, 35 (16.7%) participants in the Intervention group failed to graduate with their cohort as compared to 33 (18.1%) participants in the Comparison group, a nonsignificant difference (= 0.130, P = 0.718). The likelihood of a participant not graduating with their initial training cohort was analyzed using a simple binary logistic regression model and limiting the covariates to those measured during the initial study enrollment. There was no significant effect of treatment condition on the likelihood of failure to graduate. However, female gender (OR = 4.545; 95% CI: 2.456, 8.411), increased body mass index (OR = 1.110; 95% CI: 1.1040, 1.184), higher scores of neuroticism as assessed using the NEO-FFI (OR = 1.040; 95% CI: 1.006, 1.074), and depressed mood or sense of inadequacy as measured on the POMS (OR = 1.024; 95% CI: 1.002, 1.046) were all associated with an increased likelihood of failure to graduate.
DISCUSSION
Most studies of training effectiveness in military environments have concerned themselves primarily with activities that occur during the waking hours. The studies tend to examine the relationship between time expended in various training modalities and measures of individual or system performance—the archetype being the classic transfer of training study. The current study took a decidedly different approach, instead concerning itself primarily with the importance of time spent sleeping and its relation to measures of trainee performance and other indicators of individual functioning during BCT. Recognizing that adolescents comprise the majority of military accessions, this study evaluated the impact of accommodating adolescent alterations in sleep/wake patterns.
In particular, the scheduled timing of sleep during training was adjusted to account for the developmental phase delay of the circadian cycle in adolescents. The results of this study indicate that, even after controlling for factors contributing to individual differences, adjusting the scheduled sleep period in a phase delayed direction was associated with increased daily total sleep and modest improvements in some indicators of daytime functioning. These results were less evident in the latter portion of basic training due to the operational requirements imposed by the field exercises. These findings suggest several operationally relevant effects of accommodating adolescent sleep physiology that military planners may wish to consider in developing future training programs of instruction and associated training schedules. In addition, the findings have generalizability to the larger population of adolescents and young adults: the timing of the major sleep episode is important.
A. Actigraphic Measures of Sleep
We predicted that trainees on the modified, phase-delayed sleep schedule would obtain more daily sleep than trainees following the standard Basic Combat Training schedule. We found that trainees on the modified sleep schedule obtained approximately 31 more minutes of total sleep per night than those on the standard sleep schedule. This finding is consistent with that of other studies, such as the School Transition Study,40 which found that early start times are associated with truncated sleep in adolescents. The reduction in sleep with early start times is attributed to the developmental phase delay of the circadian cycle in adolescents, which makes it particularly difficult for adolescents to advance the evening retiring time to obtain an adequate amount of sleep. Additionally, Carskadon and colleagues7 have demonstrated that adolescents do not readily adapt or habituate their circadian cycle to early rising times, although the mechanism underlying this observation is not well understood. The current results are consistent with findings from a study reported by Miller and colleagues in which 31 US Navy recruits were assigned to two consecutive 8-hour sleep conditions (21:00 to 05:00 and 22:00 to 06:00) in a crossover study design.41,42 Navy recruits in that study obtained an additional 22 m of sleep when on the 1-hour phase-delayed sleep schedule. It is also interesting to note that a similar phenomenon has been described in adult shift workers with very early morning starts who tend to experience long sleep latencies when attempting to get compensatory sleep in the early evening.43
This study demonstrates that scheduling the sleep period of adolescents and young adults to better align with the phase delay in their circadian cycle results in a significant improvement in total daily sleep without any concomitant adjustment to the quantity of time scheduled for sleep. Regardless of differences in the timing of sleep between the two schedules, morning chronotype trainees averaged approximately 15 minutes more sleep than those trainees who were evening chronotype. This pattern is consistent with that described by Wolfson44 for adolescent students transitioning to a school with an earlier start time: evening chronotype students had more difficulty adjusting to the earlier start time and had less total sleep than did morning chronotype students. The implication is that even with the phase-delayed schedule used in this study, evening chronotype trainees experienced greater difficulty adjusting to their new start time. This result is not surprising given the trainees' self-reported wake times prior to Basic Combat Training, which suggest that the transition to military life necessitated earlier start times for the majority of trainees. It is also worth noting that the average quantity of sleep obtained by trainees was only approximately 60% of the 9.2 hours of daily sleep reportedly needed by adolescents.44,45 Lastly, the observation that sleep was reduced for trainees using the modified schedule after the sixth week of training is an artifact caused by the onset of the field exercise portion of Basic Combat Training.
B. Mood States
We predicted that trainees on the modified sleep schedule would have less decrement in mood state than trainees following the standard Basic Combat Training sleep schedule. There was weak support for this hypothesis based on the analysis of the entire study sample, which necessarily excluded consideration of a total daily sleep variable in the models. Irrespective of treatment condition, the general trend was for trainees to report decreased feelings of tension-anxiety, depression-dejection, fatigue-inertia, and confusion-bewilderment over the course of Basic Combat Training. Trainees in the Intervention group reported more stable feelings of anger-hostility and exhibited steadier total mood disturbance scores than trainees in the Comparison group. Trainees in the Intervention group also tended towards less anger-hostility and lower total mood disturbance scores relative to the Comparison group early in training, although these differences declined during Basic Combat Training. Trainees in the Intervention group reported significantly greater feelings of vigor than those in the Comparison group throughout training, but the effect size of treatment condition was modest in this case. Overall, there was no evidence that circadian chronotype significantly affected trainees' mood states.
There was partial support for the effects of chronotype on mood, when the analysis was restricted to the actigraphy subsample and a variable for total daily sleep was included in the models. Irrespective of treatment condition, evening chronotype trainees reported more vigor throughout training than morning chronotype trainees. However, evening chronotype trainees in the Intervention group exhibited less self-reported feelings of tension-anxiety, depression-dejection, anger-hostility, and confusion-bewilderment than their morning chronotype counterparts. The opposite pattern occurred in the Comparison group, with evening chronotype trainees reporting greater feelings of tension-anxiety, depression-dejection, anger-hostility, and confusion-bewilderment than their morning chronotype counterparts. In terms of total mood disturbance score, evening chronotype trainees in the Intervention group had lower scores than their morning chronotype counterparts, while a trend in the opposing direction was observed for trainees in the Comparison group. Taken together, these findings suggest that the phase-delayed sleep schedule preferentially impacted, in a positive direction, the mood state of evening chronotype trainees. The operational significance of this finding is evident when one considers that the majority of military accessions are adolescents who, as a demographic group, tend to exhibit a biological predisposition for eveningness.40
The rather modest impact of the sleep schedule intervention on subjective mood in this study contrasts with other research that has shown that manipulations of the duration and timing of sleep episodes can have marked impacts on mood.46–52 For example, Boivin and colleagues47 demonstrated that even moderate changes in the timing of the sleep-wake cycle led to profound effects on mood. Similarly, Danilenko et al.48 showed that advancing the sleep-wake cycle daily by just 20 minutes for a week led to significant decrements in subjective mood ratings relative to a control group with stable sleep. Interestingly, Selvi and colleagues50 showed that phase preference modified the effect of partial sleep deprivation on mood, with morning chronotypes exhibiting less sensitivity of mood. A pattern similar to that described by Selvi and colleagues was observed, at least for the subsample of the study population who had actigraphy data.
Several hypotheses are suggested to explain the small observed effect of the sleep schedule intervention on subjective mood in this study. Mood is largely a function of situational factors,53 and the Basic Combat Training environment represents a complex milieu of such factors. Throughout Basic Combat Training, the military instructor cadre is working to actively shape and influence the mood state of their trainees as a means of achieving organizational training objectives. Many factors, such as leader-subordinate and peer-to-peer dynamics, unit morale, and individual perceptions of acute physical and mental stressors, likely contributed to differences in subjective mood among trainees. Given the aggregate of observed and unobserved factors in this study, the relationship between sleep and subjective mood was most likely reduced to having a small, but still measurable, effect size. Additionally, while the phase-delayed sleep schedule resulted in increased total daily sleep for trainees in the Intervention group, the shortfall in daily sleep relative to known adolescent sleep needs for both groups was still large (i.e., on the order of 3-4 h). Consequently, trainees in both groups may have had a significant partial sleep deprivation that then blunted the observed effect of the schedule intervention. Finally, the phase-delayed sleep schedule, while a marked improvement over the standard Basic Combat Training sleep schedule in terms of accommodating adolescent sleep-wake patterns, was still significantly out of phase with trainees' baseline patterns as inferred from trainee responses on the pre-training Pittsburgh Sleep Quality Index. Such an assertion is supported by Carskadon's study of adolescent students,40 which found that school start times around 07:00 were difficult for adolescent students, and students tended to do better when start times were delayed until 08:00 or later.
C. Basic Rifle Marksmanship
We predicted that trainees on the modified sleep schedule would exhibit greater improvement in basic rifle marksmanship scores than those following the standard Basic Combat Training sleep schedule. This hypothesis was supported by the study results, although the analysis of marksmanship performance turned out to be far from straightforward given differences between training companies in initial performance on the first record fire and variability in the number of record fires accomplished by each trainee. Despite all this variability, however, it was possible to demonstrate that the degree of improvement in marksmanship performance over the serial record fires was significantly predicted, in part, by a sleep-related variable.
It is noteworthy that sleep during the week preceding the record fires, when basic marksmanship tasks and subtasks were being learned, was more strongly correlated with subsequent performance than sleep during the week of the record fires. This finding suggests the possibility that sleep was acting as a modifier of training effectiveness. Such an assertion is consistent with research showing that procedural memories improve with subsequent early slow wave sleep (SWS) and late rapid eye movement (REM) sleep, although there is some debate regarding the relative importance of the various stages of sleep. Nevertheless, increasing evidence supports the role of sleep in memory consolidation and latent learning.17–20,54,55 For example, Gais and colleagues18 observed that memories are, on average, more than three times improved after sleep containing both SWS and REM sleep than after a period of early sleep alone. Thus, the phase-delayed schedule, which was associated with increased total daily sleep, likely increased the opportunity for late REM sleep and thereby potentiated the learning and recall of marksmanship skills.
D. Physical Fitness
We predicted that trainees on the modified sleep schedule would exhibit greater improvement in physical fitness scores than trainees following the standard Basic Combat Training sleep schedule. This hypothesis was not supported by the study results. As in the case of the marksmanship data, the use of nonrandomized groups led to significant baseline differences between the Intervention and Comparison groups, with the Intervention group exhibiting higher physical fitness scores early in training. However, these differences diminished over the course of training such that the groups were equivalent on the final physical fitness assessment. Thus, the overall pattern suggested a regression to the mean phenomenon—an assertion that is supported by the absence of any correlation between fitness scores and average total daily sleep for trainees in the actigraphy subsample. On the flip side, altering the timing of physical fitness training to accommodate the change in timing of sleep did not appear to harm the performance of trainees in the Intervention group. Additionally, trainees in the Intervention group generally expressed a preference for the later timing of their physical fitness training, while trainees in the Comparison group, on average, preferred the earlier timing of their physical fitness training.
These findings are consistent with reports in the scientific literature examining the effect of sleep deprivation on exercise performance. Studies of exercise performance after periods of sleep deprivation of up to 72 hours have consistently demonstrated that muscle strength and exercise performance are not affected by sleep debt.56–59 While Martin56 was able to show that sleep loss reduced work time to exhaustion by an average of 11 percent, this change was attributed to the psychological effects of acute sleep debt because subjects' ratings of exertion were dissociated from any cardiovascular changes. A smaller body of research has also examined the influence of chronotype on diurnal changes in muscle strength. For example, Tamm et al.60 found that evening chronotype individuals could produce a stronger maximum voluntary muscle contraction in the evening, while morning chronotype individuals exhibited no significant change in strength throughout the day. However, the results of this study failed to show any significant effect of chronotype for the strength-based fitness assessments.
E. Sleepiness and Sleep Patterns
We predicted that for trainees whose sleep schedules were modified, the odds of reporting occupationally significant fatigue (defined as an Epworth Sleepiness Scale score > 10) would be lower than that for trainees following the standard Basic Combat Training sleep schedule. This hypothesis was supported by the study results, with trainees in the Comparison group being 2.3 times more likely to have occupationally significant fatigue at the end of training—a finding with important safety and health implications. At the beginning of the study, trainees in the Intervention and Comparison groups had comparable subjective sleepiness as assessed based on ESS scores. Over the course of training, trainees in the Comparison group exhibited a significant increase in reported sleepiness, while those in the Intervention group reported no change in subjective sleepiness. Overall, evening chronotype trainees reported greater sleepiness than morning chronotype trainees. This result suggests that the modified sleep schedule, while an improvement over the standard schedule, still did not fully accommodate the developmental phase delay of the adolescent and young adult circadian cycle, particularly in trainees with a strong evening chronotype.
We also predicted that for trainees whose sleep schedules were modified, the odds of reporting poor sleep quality (defined as Pittsburgh Sleep Quality Index [PSQI] score > 5) would be lower than that for trainees following the standard Basic Combat Training sleep schedule. This hypothesis was supported by the study results, with trainees in the Comparison group being 5.5 times more likely to report poor sleep quality at the end of training. Trainees in the Intervention and Comparison groups had comparable sleep quality as assessed based on PSQI score at the start of the study. Over the course of training, trainees in the comparison group exhibited a significant degradation in sleep quality, while those in the Intervention group exhibited a trend towards improved sleep quality. Additionally, the odds of trainees reporting poor quality sleep actually decreased for those in the Intervention group relative to their scores at the start of the study. This finding suggests that the phase-delayed sleep schedule was an improvement over trainees' baseline sleep schedule—or in other words, the schedule used by the trainees in the Intervention group actually improved their sleep patterns.
To summarize, trainees in the Intervention group graduated from Basic Combat Training in a better rested state than their counterparts in the Comparison group. The operational significance of this finding can be inferred from research on school age adolescents linking sleep patterns to academic performance.8,61 Thus, trainees in the Intervention group, by way of having improved wake-sleep patterns and increased total daily sleep, were better prepared to undertake the more academically rigorous secondary military occupation-specific training that follows Basic Combat Training. Additionally, trainees in the Intervention group can be expected to be at lower risk for future lost training days or injuries.62
F. Attrition
The study also examined whether trainees in the Intervention group were less likely to drop out of training than the trainees in the Comparison group. This hypothesis was not supported by the study results. The single largest risk factor for attrition from Basic Combat Training was gender, with females more likely to attrite than their male counterparts, followed by body mass index (BMI) (i.e., trainees with a higher BMI were more likely to attrite; likely, BMI is a surrogate for physical fitness), neurotic personality characteristics, and depressed subjective mood. Given that most attrition tends to occur earlier rather than later in training, it is more likely that preexisting conditions or vulnerabilities were the major determinant of attrition.
CONCLUSION
In summary, increasing sleep had a small but measurable influence on various indicators of trainee functioning, even after controlling for a variety of factors that affect performance. Although trainees' responses to the sleep schedule intervention were modest, it should be appreciated that physical fitness scores and attrition rates, two important outcome measures in BCT, are not highly sensitive to the effects of fatigue. The most important finding of the study may be the impact of the schedule intervention on sleep quality during BCT—that is, trainees completing BCT using the phase-delayed sleep schedule had significant improvements in sleep patterns such that they graduated from training in a better rested state than when they started. The significance of this finding may not be fully appreciated until trainees' subsequent performance is assessed during the more cognitively demanding secondary military occupational specialty training courses.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors acknowledge the following people and organizations: the US Army Maneuver Support Center and Fort Leonard Wood, Missouri; the Army Research Laboratory Human Research and Effectiveness Directorate's Maneuver and Mobility Branch at Fort Leonard Wood, Missouri; and the officers, drill sergeants, and soldiers of Bravo and Charlie Companies, 3rd Battalion, 10th Infantry Regiment, 3rd Chemical Brigade.
REFERENCES
- 1.Killgore WD, Estrada A, Wildzunas RM, Balkin TJ. Sleep and performance measures in soldiers undergoing military relevant training. Presented at the 26th Army Science Conference; Orlando, FL. 2008. [Google Scholar]
- 2.Miller NL, Matsangas P, Shattuck LG. Fatigue and its effect on performance in military environments. In: Hancock P, Szalma JL, editors. Performance under stress. Vol. 2007. Burlington, VT: Ashgate Publishing Company; pp. 231–49. [Google Scholar]
- 3.Miller NL, Shattuck LG, Matsangas P. Longitudinal study of sleep patterns of United States Military Academy cadets, Sleep. 2010;33:1623–31. doi: 10.1093/sleep/33.12.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller NL, Shattuck LG. Sleep patterns of young men and women enrolled at the United States Military Academy: results from year one of a four-year longitudinal study. Sleep. 2005;28:837–41. doi: 10.1093/sleep/28.7.837. [DOI] [PubMed] [Google Scholar]
- 5.Anch AM, Browman CP, Mitler M, Walsh JK. Sleep: a scientific perspective. Englewood Cliffs, NJ: Pearson Prentice-Hall, Inc; 1988. [Google Scholar]
- 6.Carskadon MA, Acebo C, Richardson GS, Tate BA, Seifer R. An approach to studying circadian rhythms of adolescent humans. J Biol Rhythms. 1997;12:278–89. doi: 10.1177/074873049701200309. [DOI] [PubMed] [Google Scholar]
- 7.Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21:871–81. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- 8.Wolfson AR, Carskadon MA. Understanding adolescents' sleep patterns and school performance: a critical appraisal. Sleep Medicine Reviews. 2003;7:491–506. doi: 10.1016/s1087-0792(03)90003-7. [DOI] [PubMed] [Google Scholar]
- 9.Killgore WD, Balkin TJ, Wesensten NJ. Impaired decision making following 49 h of sleep deprivation. J Sleep Res. 2006;15:7–13. doi: 10.1111/j.1365-2869.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- 10.Belenky G, Wesensten NJ, Thorne DR, Thomas ML, Sing HC, Redmond DP, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 11.Driskell JE, Hughes SC, Willis RC, Cannon-Bowers J, Salas E. Stress, stressor, and decision-making; Technical Report for the Naval Training Systems Center. Orlando, FL: Naval Training Systems Center; 1991. [Google Scholar]
- 12.Driskell JE, Salas E, editors. Stress and human performance. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. [Google Scholar]
- 13.Hursh SR, Bell GB. Human performance cognitive model for Air Force information operations; Technical Report for the Air Force Research Laboratory. Brooks Air Force Base, TX: Air Force Research Laboratory; 2001. [Google Scholar]
- 14.Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:2. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 15.Tharion WJ, Shukitt-Hale B, Lieberman HR. Caffeine effects on marksmanship during high-stress military training with 72 hour sleep deprivation. Aviat Space Environ Med. 2003;74:309–14. [PubMed] [Google Scholar]
- 16.McLellan TM, Kamimori GH, Bell DG, Smith IF, Johnson D, Belenky G. Caffeine maintains vigilance and marksmanship in simulated urban operations with sleep deprivation. Aviat Space Environ Med. 2005;76:39–45. [PubMed] [Google Scholar]
- 17.Fenn KM, Nusbaum HC, Margoliash D. Consolidation during sleep of perceptual learning of spoken language. Nature. 2003;425:614–6. doi: 10.1038/nature01951. [DOI] [PubMed] [Google Scholar]
- 18.Gais S, Plihal W, Wagner U, Born J. Early sleep triggers memory for early visual discrimination skills. Nat Neurosci. 2000;3:1335–9. doi: 10.1038/81881. [DOI] [PubMed] [Google Scholar]
- 19.Stickgold R, James L, Hobson A. Visual discrimination learning requires sleep after training. Nature Neuroscience. 2000;3:1237–8. doi: 10.1038/81756. [DOI] [PubMed] [Google Scholar]
- 20.Walker MP, Brakefield T, Hobson JA, Stickgold R. Dissociable stages of human memory consolidation and reconsolidation. Nature. 2003;425:616–20. doi: 10.1038/nature01930. [DOI] [PubMed] [Google Scholar]
- 21.Andrews CH. The relationship between sleep regimen and performance in United States Navy recruits. Monterey, CA: Naval Postgraduate School; 2004. [Google Scholar]
- 22.Miller NL, Dyche J, Andrews CH, Lucas T. Navy boot camp: test score changes after two hour increase in sleep time. Philadelphia, PA: Proceedings of the Association of Professional Sleep Societies; 2004. Jun, [Google Scholar]
- 23.Killgore WD, Estrada A, Wildzunas RM, Balkin TJ. Sleep and performance measures in soldiers undergoing military relevant training. Presented at the 26th Army Science Conference; Orlando, FL. 2008. [Google Scholar]
- 24.Trickel MT, Barnes MD, Egget DL. Health-related variables and academic performance among first-year college students: implications for sleep and other behaviors. Journal of American College Health. 2000;49:125–31. doi: 10.1080/07448480009596294. [DOI] [PubMed] [Google Scholar]
- 25.Moldofsky H. Sleep and the immune system. Int J Immunopharmacol. 1995;17:649–54. doi: 10.1016/0192-0561(95)00051-3. [DOI] [PubMed] [Google Scholar]
- 26.Lange T, Perras B, Fehm HL, Born J. Sleep enhances the human antibody response to Hepatitis A vaccination. Psychosom Med. 2003;65:831–5. doi: 10.1097/01.psy.0000091382.61178.f1. [DOI] [PubMed] [Google Scholar]
- 27.Thorne DR, Thomas ML, Russo MB, et al. Performance on a driving-simulator divided attention task during one week of restricted nightly sleep. Sleep. 1999;22(Suppl 1):301. [Google Scholar]
- 28.Directorate Basic Combat Training Doctrine and Training Development. Program of instruction for basic combat training (Version 5) Fort Jackson, SC: Author; 2008. [Google Scholar]
- 29.McNair DM, Lorr M, Droppleman LF. Manual for the profile of mood states. San Diego, CA: Educational and Industrial Testing Services; 1981. [Google Scholar]
- 30.Costa PT, McCrae RR. Revised NEO personality inventory (NEO-PI-R) and NEO five-factor inventory (NEO-FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- 31.Weiner IB, Greene RL. Handbook of personality assessment. Hoboken, NJ: John Wiley & Sons; 2008. [Google Scholar]
- 32.Johnson DC, Polusny MA, Erbes C, et al. The response to stressful experiences scale (RSES) U.S. Department of Veterans Affairs National Center for PTSD; 2008. [Google Scholar]
- 33.Naval Center for Combat and Operational Stress Control Resilience: what is it? Retrieved July 16, 2009. from http://www.med.navy.mil/sites/nmcsd/nccosc/Resilience/Documents/Resilience_What_Is_It.pdf.
- 34.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 35.Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 36.Horne JA, Ostberg O. A self assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 37.Kim JO, Curry J. The treatment of missing data in multivariate analysis. Sociol Methods Res. 1977;6:216–40. [Google Scholar]
- 38.Brick JM, Kalton G. Handling missing data in survey research. Stat Methods Med Res. 1996;5:215–38. doi: 10.1177/096228029600500302. [DOI] [PubMed] [Google Scholar]
- 39.Shattuck NL, Shattuck LG, Tvaryanas AP, Matsangas P. Effects of sleep on training effectiveness in soldiers at Fort Leonard Wood, Missouri. NPS Technical Report, NPS-OR-10-011, November 2010. Downloadable from http://faculty.nps.edu/nlmiller/docs/NPS-OR-10-011_Signed.pdf.
- 40.Carskadon MA. Factors influencing sleep patterns of adolescents. In: Carskadon MA, editor. Adolescent sleep patterns: biological, social, and psychological influences. Vol. 2001. New York, NY: Cambridge University Press; pp. 4–26. [Google Scholar]
- 41.Baldus BR. Sleep patterns in U.S. Navy recruits: an assessment of the impact of changing sleep regimens. Monterey, CA: Naval Postgraduate School; 2002. [Google Scholar]
- 42.Miller NL, Baldus BR, Coard HF, Sanchez S, Redmond DR. Timing of the major sleep period as a fatigue countermeasure in U.S. Navy recruits. Proceedings of the Aerospace Medical Association; May 2003; San Antonio, TX. [Google Scholar]
- 43.Rosa RH. What can the study of work scheduling tell us about adolescent sleep? In: Carskadon MA, editor. Adolescent sleep patterns: biological, social, and psychological influences. Vol. 2001. New York, NY: Cambridge University Press; pp. 159–71. [Google Scholar]
- 44.Wolfson AR. Bridging the gap between research and practice: what will adolescents' sleep-wake patterns look like in the 21st century? In: Carskadon MA, editor. Adolescent sleep patterns: biological, social, and psychological influences. Vol. 2001. New York: Cambridge University Press; pp. 198–219. [Google Scholar]
- 45.Mercer PW, Merritt SL, Cowell JM. Differences in reported sleep need among adolescents. J Adolesc Health. 1998;23:259–63. doi: 10.1016/s1054-139x(98)00037-8. [DOI] [PubMed] [Google Scholar]
- 46.Birchler-Pedross A, Schröder CM, Münch M, et al. Subjective well-being is modulated by circadian phase, sleep pressure, age, and gender. J Biol Rhythms. 2009;24:232–42. doi: 10.1177/0748730409335546. [DOI] [PubMed] [Google Scholar]
- 47.Boivin DB, Czeisler CA, Dijk DJ, et al. Complex interaction of the sleep-wake cycle and circadian phase modulates mood in healthy subjects. Arch Gen Psychiatry. 1997;54:145–52. doi: 10.1001/archpsyc.1997.01830140055010. [DOI] [PubMed] [Google Scholar]
- 48.Danilenko KV, Cajochen C, Wirz-Justice A. Is sleep per se a zeitgeber in humans? J Biol Rhythms. 2003;18:170–8. doi: 10.1177/0748730403251732. [DOI] [PubMed] [Google Scholar]
- 49.Monk TH, Buysse DJ, Reynolds CF, Jarrett DB, Kupfer DJ. Rhythmic vs. homeostatic influences on mood, activation, and performance in young and old men. J Gerontol. 1992;47:221–7. doi: 10.1093/geronj/47.4.p221. [DOI] [PubMed] [Google Scholar]
- 50.Selvi Y, Gulec M, Agargun MY, Besiroglu L. Mood changes after sleep deprivation in morningness-eveningness chronotypes in healthy individuals. J Sleep Res. 2007;16:241–4. doi: 10.1111/j.1365-2869.2007.00596.x. [DOI] [PubMed] [Google Scholar]
- 51.Taub JM, Berger RJ. Performance and mood following variations in the length and timing of sleep. Psychophysiology. 1973;10:559–70. doi: 10.1111/j.1469-8986.1973.tb00805.x. [DOI] [PubMed] [Google Scholar]
- 52.Wood C, Magnello ME. Diurnal changes in perceptions of energy and mood. J R Soc Med. 1992;85:191–4. doi: 10.1177/014107689208500404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chamorro-Premuzic T. Personality and individual differences. Malden, MA: Blackwell Publishing; 2007. [Google Scholar]
- 54.Karni A, Tanne D, Rubenstein BS, Askenasy JJM, Sagi D. Dependence on REM sleep of overnight improvement of perceptual skill. Science. 1994;265:679–82. doi: 10.1126/science.8036518. [DOI] [PubMed] [Google Scholar]
- 55.Wilson MA, McNaughton BL. Reactivation of hippocampal ensemble memories during sleep. Science. 1994;265:676–9. doi: 10.1126/science.8036517. [DOI] [PubMed] [Google Scholar]
- 56.Martin BJ. Effect of sleep deprivation on tolerance of prolonged exercise. Eur J Appl Physiol. 1981;47:345–54. doi: 10.1007/BF02332962. [DOI] [PubMed] [Google Scholar]
- 57.Martin BJ, Gaddis, GM Exercise after sleep deprivation. Med Sci Sports Exerc. 1981;13:220–3. doi: 10.1249/00005768-198104000-00002. [DOI] [PubMed] [Google Scholar]
- 58.Reilly T, Deykin T. Effects of partial sleep loss on subjective states, psychomotor and physical performance tests. J Human Movement Studies. 1983;9:157–70. [Google Scholar]
- 59.Van Helder T, Radomski MW. Sleep deprivation and the effect of exercise performance. Sports Med. 1989;7:235–47. doi: 10.2165/00007256-198907040-00002. [DOI] [PubMed] [Google Scholar]
- 60.Tamm AS, Lagerquist O, Ley AL, Collins DF. Chronotype influences diurnal variations in the excitability of the human motor cortex and the ability to generate torque during a maximum voluntary contraction. J Biol Rhythms. 2009;24:211–24. doi: 10.1177/0748730409334135. [DOI] [PubMed] [Google Scholar]
- 61.Acebo C, Carskadon MA. Influence of irregular sleep patterns on waking behavior. In: Carskadon MA, editor. Adolescent sleep patterns: biological, social, and psychological influences. Vol. 2001. New York, NY: Cambridge University Press; pp. 220–35. [Google Scholar]
- 62.Acebo C, Wolfson AR, Carskadon MA. Relations among self-reported sleep patterns, health, and injuries in adolescents. Sleep Res. 1997;26:149. [Google Scholar]


