Abstract
Thrombotic microangiopathy (TMA) is a pathological process involving thrombocytopenia, microangiopathic haemolytic anaemia and microvascular occlusion. TMA is common to haemolytic uraemic syndrome (HUS) associated with shiga toxin or invasive pneumococcal infection, atypical HUS (aHUS), thrombotic thrombocytopenic purpura (TTP) and other disorders including malignant hypertension. HUS complicating infection with shiga toxin-producing Escherichia coli (STEC) is a significant cause of acute renal failure in children worldwide, occurring sporadically or in epidemics. Studies in aHUS have revealed genetic and acquired factors leading to dysregulation of the alternative complement pathway. TTP has been linked to reduced activity of the ADAMTS13 cleaving protease (typically with an autoantibody to ADAMTS13) with consequent disruption of von Willebrand factor multimer processing. However, the convergence of pathogenic pathways and clinical overlap create diagnostic uncertainty, especially at initial presentation. Furthermore, recent developments are challenging established management protocols. This review addresses the current understanding of molecular mechanisms underlying TMA, relating these to clinical presentation with an emphasis on renal manifestations. A diagnostic and therapeutic approach is presented, based on international guidelines, disease registries and published trials. Early treatment remains largely empirical, consisting of plasma replacement/exchange with the exception of childhood STEC-HUS or pneumococcal sepsis. Emerging therapies such as the complement C5 inhibitor eculizumab for aHUS and rituximab for TTP are discussed, as is renal transplantation for those patients who become dialysis-dependent as a result of aHUS.
Keywords: HUS, TTP, complement, kidney, eculizumab
Introduction
Thrombotic microangiopathy (TMA) describes a pathological process of microvascular thrombosis, consumptive thrombocytopenia and microangiopathic haemolytic anaemia (MAHA), leading to end-organ ischaemia and infarction affecting particularly the kidney and brain. Patients may present with acute renal failure and/or cerebral dysfunction, although cardiac, gastrointestinal and other organ involvement can also occur. TMA is a feature of a number of clinical disorders including haemolytic uraemic syndrome (HUS) either due to shiga toxin-producing bacteria, including Escherichia coli (STEC) and Shigella dysenteriae Type I, or due to invasive infection with Streptococcus pneumoniae (pneumococcal- or p-HUS). Rare but important TMA-related disorders include non-shiga toxin-mediated, non-pneumococcal, hence ‘atypical’, haemolytic uraemic syndrome (aHUS), and thrombotic thrombocytopenic purpura (TTP). TMA may also occur in other conditions including malignant hypertension (HT), pregnancy, and renal transplantation (rejection or drug toxicity). Several molecular mechanisms mediating TMA have been elucidated in the past decade via human gene association studies, and in both in vitro experiments and animal models. However, challenges remain in distinguishing specific causes of TMA in the presence of overlapping clinical features. We review the pathophysiology of TMA and provide a guide to diagnosis and treatment drawing on existing guidelines. These recommend ‘urgent and empirical’ therapeutic plasma exchange (TPE), provided that childhood STEC and invasive pneumococcal infection have been excluded [1].
Laboratory features of TMA
The term TMA was coined in 1952 to describe post-mortem findings of ‘widely disseminated thrombosis of the smallest calibre blood vessels’ [2]. It was clear that laboratory features (Table 1) could identify TMA ante-mortem, though recognition that MAHA indicated ‘direct contact between red cells and the diseased blood vessels’ came later [3]. Endothelial damage and thrombosis within the microvasculature create abnormally high shear stress, leading to platelet aggregation and red cell destruction. As the haemolysis is not immune-mediated, the Coombs test (or ‘direct antiglobulin test’) should be negative. However, a positive Coombs test may be seen in associated autoimmune conditions such as systemic lupus erythematosus (SLE), or alloimmunity (e.g. following blood product transfusion). The Coombs test may also be positive in neuraminidase-mediated p-HUS. Elevated serum lactate dehydrogenase (LDH) reflects haemolysis and/or tissue ischaemia and is useful both diagnostically and in monitoring disease activity. Disseminated intravascular coagulation is usually distinguishable from TMA on the basis of abnormal clotting parameters and typically less marked thrombocytopenia [4].
Table 1.
Laboratory features of TMA
| Full blood count: severe thrombocytopenia and anaemia |
| Blood film: red cell fragmentation (‘schistocytosis’ >1%), also polychromasia (reticulocytosis), absent or giant platelets |
| Coombs test: negative |
| Haemolysis screen: hyperbilirubinaemia (unconjugated), elevated LDH and reticulocyte count, low serum haptoglobins, free haemoglobin in serum and urine |
| Liver enzymes and coagulation screen: normal |
| Serum creatinine: elevated in renal involvement |
Renal biopsy features of TMA
Renal histological features of TMA on light microscopy include arteriolar and/or glomerular intracapillary thrombosis, often with accumulation of fragmented erythrocytes within capillary lumens, and focally ischaemic or congested glomerular tufts. Severe arterial and arteriolar injury may be seen with or without widespread thrombosis, usually in the setting of malignant HT. However, renal biopsy is rarely performed in patients with renal manifestations of TMA as little aetiological or prognostic information is added to that obtained from basic laboratory tests. One exception is post-renal transplantation, where a biopsy may be required to distinguish antibody-mediated rejection from other potential causes of TMA. Native renal biopsy may also be of value where an alternative (or coexistent) lesion is suspected (e.g. glomerulopathy). In chronic TMA, a membranoproliferative pattern with ‘double contours’ of the glomerular basement membrane may develop, usually lacking the immune deposits characteristic of glomerulonephritis.
Clinical disorders associated with TMA
TTP [5] and HUS [6] were initially described as distinct clinical entities, both manifesting TMA. A paradigm arose whereby TMA with significant dysfunction of the central nervous system (CNS), severe thrombocytopenia, fever and relative renal sparing was designated as TTP, while the term HUS was applied to cases with predominant renal involvement without neurological features. One autopsy series appeared to support this distinction, suggesting that HUS-associated renal lesions were more severe and contained fibrin-rich thrombi, as opposed to the platelet-rich thrombi seen in TTP [7]. However, it has become apparent that considerable clinical overlap exists, prompting the use in some publications of the composite term ‘HUS/TTP’. Advances in the biological understanding of TMA suggest that an aetiological classification (rather than one based on clinical features) should provide a better guide to prognosis and therapy. The system proposed by the European Paediatric Research Group for HUS [8] incorporates both defined aetiologies and disease ‘associations’ where causality is not yet firmly established (Table 2).
Table 2.
Classification of HUS, TTP and other TMA-associated disorders
| Established aetiologies |
| Infection-induced |
| Shiga toxin-associated: E. coli (STEC), Shigella dysenteriae Type 1 and other bacteria |
| Invasive infection with Streptococcus pneumoniae (p-HUS) |
| Complement dysregulation |
| Genetic |
| Acquired |
| ADAMTS13 protease deficiency |
| Genetic |
| Acquired (including ticlopidine) |
| Defective cobalamin (B12) metabolism |
| Quinine |
| Disease associations |
| HIV and other viral infections |
| Malignancy, cancer chemotherapy, ionizing radiation |
| Transplantation |
| Allogeneic HSCT |
| Solid-organ transplantation |
| Calcineurin inhibitors |
| Pregnancy |
| HELLP syndrome |
| Oral contraceptive pill |
| Connective tissue disorders |
| SLE |
| Antiphospholipid syndrome |
| Glomerulopathy |
| Pancreatitis |
| Malignant hypertension |
| VEGF-inhibitors |
| Other familial |
Adapted from Besbas et al. [8].
This review addresses the major aetiologies of TMA, and the inherent difficulties in linking disease mechanisms to clinical phenotypes. Although a predominant renal picture is characteristic of STEC-HUS, CNS complications can occur [9], with the same being true of aHUS related to complement dysregulation [10]. Conversely, TTP associated with severe deficiency of ADAMTS13 may sometimes present with renal failure and/or without neurological features [11, 12]. Disease ‘associations’ of TMA are also discussed, although in some cases it is unclear whether these are causative of TMA or precipitants in a genetically or immunologically susceptible individual. The importance of triggering factors is exemplified by the frequent occurrence of preceding illnesses including gastroenteritis and upper respiratory tract infections in large cohorts of patients presenting with aHUS [13–15]. Malignant HT may be either a cause of TMA or a manifestation of renal involvement from an underlying disorder such as aHUS [15]. The interplay of constitutional defects and environmental triggers necessitates broad aetiological consideration in patients presenting with features of TMA, and testing for defects in complement regulation and von Willebrand factor (vWF) processing.
Shiga toxin-associated HUS
Clinical features
HUS complicating enteric infection with shiga toxin-producing bacteria was identified in 1983 [16] and is an important cause globally of acute renal failure in childhood. STEC is the main pathogen in developed countries, accounting for over 90% of HUS cases [17]. STEC-HUS (also called diarrhoea-positive, D+HUS) typically presents as renal failure following a bloody diarrhoeal prodrome. The prognosis in children is generally favourable with supportive measures (including dialysis) [18], in contrast to p-HUS where mortality among infants is around 25% despite treatment [19]. The largest recorded outbreak of STEC-HUS was centred in Germany in May 2011. The epidemic was notable for adult predominance (especially females) and high mortality during the acute phase of illness, with 36 deaths among the 845 cases (4.3%) [20]. In addition to renal failure, a significant proportion of patients developed neurological sequelae late in the disease [21]. Available information suggests that children (representing around 12% of cases) were less severely affected, with one death among over 90 cases [22].
Pathophysiology
The natural reservoirs of STEC are sheep and cattle intestines, with bacterial transmission to humans occurring predominantly through consumption of raw or undercooked food products, or contaminated water. STEC O157:H7 is the serotype most commonly identified in HUS cases, easily distinguished after the culture of stool or rectal swab owing to its inability to ferment sorbitol when plated on MacConkey agar. Non-O157 serotypes behave less characteristically on culture media, and hence, the identification of shiga toxin using molecular techniques is often required for diagnosis [23]. During the German outbreak, toxicological assays for shiga toxin and/or polymerase chain reaction (PCR) of the shiga toxin gene preceded serotyping of the unexpected causative strain, STEC O104:H4. This serotype is non-zoonotic, and the source for human transmission was eventually traced to bean sprouts [24].
Once ingested, STEC adheres to intestinal mucosa, secreting shiga toxin which enters the bloodstream and is transported by leucocytes to target organs [17]. Shiga toxin exerts its cytotoxic and apoptotic effects after attaching to high-affinity globotriaosylceramide 3 receptors which are highly expressed on glomerular endothelial cells (ECs). Injury to the endothelium produces a prothrombotic EC phenotype, leading to the activation of platelets, leucocytes, and the coagulation cascade. Shiga toxin-mediated activation of the alternative pathway (AP) of complement may be an additional factor in the pathogenesis of STEC-HUS [17]. As HUS occurs in a minority of STEC-infected individuals, its development could be influenced by constitutive abnormalities in complement regulation. This has been reported in a patient with HUS following infection with STEC, in whom an aHUS-associated mutation was detected [25]. However, mutations were not identified in three children treated successfully for STEC-HUS with the anti-C5 complement agent eculizumab [26]. No systematic evaluation of complement genetics in patients with STEC-HUS has yet been published.
Atypical haemolytic uraemic syndrome
Clinical phenotype
aHUS is a rare disease associated which genetic or acquired factors that cause defective regulation of the alternative complement pathway [27]. Clinical features of aHUS are indistinguishable from other causes of TMA, renal involvement being predominant but extrarenal (including severe neurological [10] or cardiac [28]) manifestations also prominent in some patients. Although aHUS often presents in childhood, at least one series found that the initial presentation in 36% of genetically predisposed individuals was in adulthood (including an 86 year old) [14]. While a diarrhoeal prodrome is less common than in STEC-HUS, a preceding episode of gastroenteritis is reported in one-quarter of childhood aHUS episodes [13, 15], with similar findings in adult aHUS [29]. Individuals sometimes present with relapsing disease and/or a family history of aHUS. The prognosis of aHUS is poor compared with STEC-HUS, with a 3-year composite endpoint of death and end-stage kidney disease (ESKD) occurring in 53% (significantly worse in adults than in children) [14].
Pathophysiology: complement dysregulation
The complement system comprises over 30 proteins pivotal to innate immunity and inflammation. Complement activation occurs by proteolysis in three pathways: the classical pathway, lectin pathway and AP (Figure 1). The AP is unique in that continuous, low-level activation occurs in the circulation due to spontaneous hydrolysis of C3 (so-called ‘C3 tickover’). C3 activation produces the anaphylatoxin C3a and an opsonic fragment, C3b, which tags microbial or altered host cell surfaces for phagocytosis. C3b is also able to bind complement factor B, forming the catalytic C3 convertase of the AP (C3bBb). The AP C3 convertase amplifies C3 activation via a positive feedback mechanism both in the circulation (‘fluid-phase’) and, following deposition of C3b, on cell surfaces. Binding of additional C3b fragments to the AP C3 convertase generates a C5 convertase, responsible for the activation of C5. C5 activation yields the anaphylatoxin and chemoattractant C5a together with C5b, which initiates assembly of the terminal complement pathway C5b-9 (or membrane attack complex, MAC). MAC forms lytic pores on cell surfaces, while on ECs, sublytic levels of MAC can impair cellular function, culminating in a prothrombotic phenotype [30].
Fig. 1.
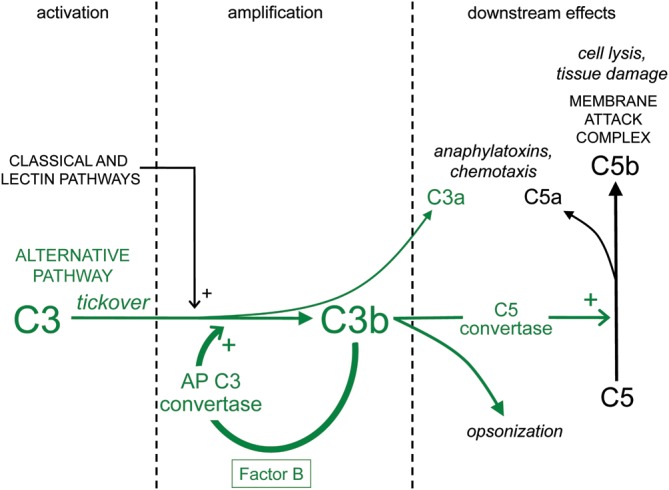
Initiation of complement activation, with amplification and downstream effects of the AP.
Several regulatory proteins inhibit amplification of the AP (Figure 2). Complement factor H blocks the formation of the AP C3 convertase and accelerates its breakdown. Factor H is also a cofactor for complement factor I-mediated proteolysis of C3b to generate the ‘inactivated’ fragment iC3b, which is unable to bind factor B to form the AP C3 convertase. In addition to fluid-phase activity, factor H can attach to negatively charged molecules on cell membranes to perform its regulatory function on the cell surface. Membrane cofactor protein (MCP/CD46) is expressed exclusively on cell surfaces, where it provides additional cofactor activity for factor I. AP complement dysregulation involves uncontrolled complement activation as a result of deficient or functionally impaired regulatory proteins, or hyperactive AP C3 convertase components. The fenestrated endothelium of the glomerulus may be particularly susceptible to AP complement dysregulation [30], explaining the renal predilection of TMA in aHUS. However, the precise mechanisms by which microvascular thrombosis ensues are not yet fully known.
Fig. 2.
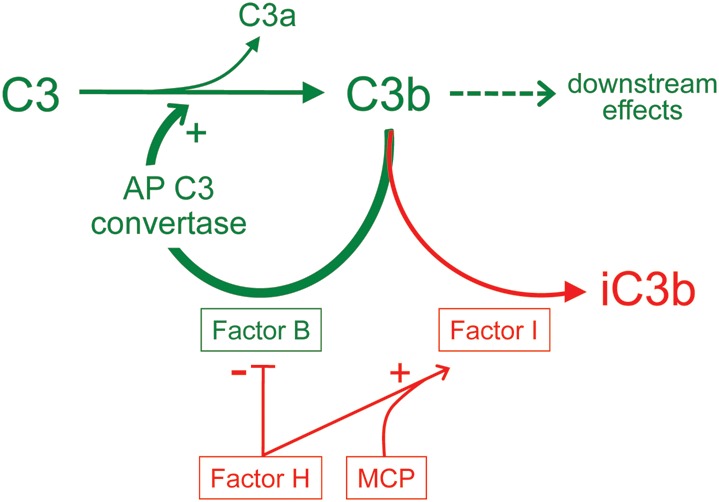
Regulation of the AP of complement.
Genetics of aHUS: factor H
The association between aHUS and AP complement dysregulation was first noted in 1973 when low plasma C3 levels were detected in some affected patients [31]. The occurrence of aHUS in multiple members of the same family (first noted in concordant monozygous twins [32]) suggested a genetic basis for disease. A linkage study in three kindreds with the aHUS phenotype localized the defect to the regulators of complement activation (RCA) region on chromosome 1q32 [33]. A candidate gene approach identified mutations in the CFH gene encoding factor H (low levels of which had been noted in affected families [34]). It is now recognized that sporadic aHUS significantly outnumbers familial cases and that heterozygous CFH mutations are the most common cause. The majority are missense, single-point mutations in exons encoding the C-terminus domain responsible for factor H binding to ECs and to surface-bound complement fragments [35]. Such mutations cause loss of complement regulation at the glomerular surface, whereas fluid-phase regulation is maintained by circulating factor H. The pathogenic role of mutant factor H with impaired surface binding is supported by a transgenic mouse model in which expression of only factor H lacking the C-terminal region led to spontaneous TMA [36]. Less commonly, aHUS-associated CFH mutations affect the N-terminus protein domain resulting in defective binding to C3b or reduced cofactor activity for factor I [37]. Mutations leading to reduced levels of circulating factor H may also cause aHUS, typically accompanied by low C3 levels [34]. However, the complete absence of fluid-phase regulation as a consequence of homozygous factor H deficiency is associated with dense deposit disease [38].
Autoantibodies that bind the C-terminal portion of factor H have also been identified as a cause of aHUS [39], producing a functional defect mimicking CFH mutations [40]. These autoantibodies may be found in isolation, or accompanying homozygous deletion of the genes encoding complement factor H-related proteins [41, 42] (especially CFHR1 [43]) or occasionally other mutations [44]. The five CFHR genes are positioned adjacent to CFH in the RCA region, where a high degree of sequence homology predisposes to genomic rearrangements including deletions and the formation of rare hybrid CFH-CFHR genes [45, 46] in association with aHUS.
Genetics of aHUS: registry data
The frequency of CFH mutations, factor H autoantibodies, and mutations in other complement-related genes in a number of aHUS cohorts has been published (Table 3). The Italian-based International Registry of Recurrent and Familial HUS/TTP [14] (comprising 273 adult and paediatric patients) and several paediatric series [13, 15, 47] also provide detailed clinical outcome data. CFH mutations, in addition to being the most common, are associated with the highest rate of adverse outcomes. Despite significant response of CFH-aHUS to plasma therapy, ESKD and death have been reported in the first year in 50–70% of patients (increasing thereafter). Patients with MCP mutations [48, 49] typically have no response to plasma therapy, remit spontaneously and have a better long-term prognosis, despite multiple relapses. CFI mutations [50] are associated with a variable prognosis intermediate between that of CFH and MCP mutations. This phenomenon may be explained by the high proportion of patients with CFI mutations having an additional mutation in another complement-related gene associated with a more severe phenotype [51]. Recently, factor I autoantibodies have been identified in three patients with aHUS, although their role in disease is uncertain [52]. A single patient is reported with aHUS and a familial mutation in the CLU gene on chromosome 8p21 encoding clusterin [53]. Mutant clusterin displayed a reduced ability to inhibit MAC formation in vitro, although aHUS in this individual may equally have been attributable to a coexisting MCP mutation. In addition to ‘loss-of-function’ mutations in regulatory proteins, ‘gain-of-function’ mutations in the genes encoding C3 [54] and factor B [55] have been reported in aHUS patients. These produce AP C3 convertase components that are hyperfunctional or resistant to inhibition by complement regulatory proteins.
Table 3.
Mutations in aHUS registries
| Abnormality | Gene (locus) | Proportion of aHUS cases (%) |
|---|---|---|
| Factor H | CFH (RCA: 1q32) | 11–29 [15, 14, 61, 64, 70, 171–174] |
| Membrane cofactor protein (MCP/CD46) | MCP (RCA) | 3–17 [15, 14, 61, 64, 70, 171–174] |
| Factor I | CFI (4q25) | 2–17 [13, 15, 14, 51, 61, 64, 70, 171–174] |
| C3 | C3 (19p13) | 2–17 [15, 14, 64, 172, 174] |
| Factor B | CFB (6p21) | 0–5 [15, 14, 64, 171–174] |
| Thrombomodulin | THBD (20p11) | 0–5 [15, 14, 174] |
| Hybrid gene | CFH-CFHR (RCA) | 0–2 [14, 41, 70, 171, 172] |
| Combined mutations | 3–17 [15, 14, 51, 64, 171–174] | |
| Factor H autoantibodies | 4–13 [15, 14, 41, 43, 44, 171–173] |
Mutations in the THBD gene encoding thrombomodulin have also been demonstrated in aHUS cohorts, in association with comparatively poor outcomes [56]. Thrombomodulin is a membrane-bound protein expressed on all vascular ECs that has anticoagulant and anti-inflammatory properties [57]. Originally identified as a cofactor for thrombin-mediated activation of protein C, it accelerates the degradation of anaphylatoxins C3a and C5a after binding thrombin to generate the fibrinolysis inhibitor procarboxypeptidase B (or ‘thrombin activatable fibrinolysis inhibitor’). As yet, the functional basis for THBD mutations as a cause of aHUS has not been demonstrated, with limited data indicating that loss of thrombomodulin-mediated complement regulation via factor I cofactor activity may be important [56]. In any event, thrombomodulin is an example of potentially important interactions between the complement and coagulation systems in TMA pathogenesis [58].
Genetics of aHUS: complotype
Genetic variants within the RCA cluster that are common on a population basis are also important in determining an individual's propensity to complement activation [59]. Single-nucleotide polymorphisms (SNPs) have been identified predisposing to aHUS in the CFH [60], MCP [61] and CFHR1 [43] genes as well as the C4BPA gene [62] encoding C4b-binding protein. The latter displayed reduced AP regulatory function via factor I cofactor activity in vitro, although classical pathway regulation (its main physiological role) was unimpaired. Two complement haplotypes (or ‘complotypes’) have been described comprising multiple SNPs in CFH [36], one increasing the risk of aHUS and the other being protective. MCP haplotypes have also been identified conferring either increased risk [63] or protection [64].
Complement assessment in aHUS
Low plasma/serum C3 (not usually C4) is consistent with a diagnosis of aHUS, but not specific (also found in some cases of STEC-HUS, dense deposit disease, SLE etc.). It is also insensitive, given that the most common CFH mutations are associated with normal circulating C3 and factor H levels, while MCP mutations also do not affect C3 levels. However, most MCP mutations result in reduced cell surface expression of MCP, detectable on peripheral blood mononuclear cells (PBMCs) using flow cytometry (FACS analysis). In contrast, low C3 levels are invariably seen in aHUS patients with C3 mutations, most with CFI mutations and around half with factor H autoantibodies [47].
Due to the insensitivity of complement protein levels, genetic and autoimmune tests are often required to identify a complement-related defect in patients with aHUS. Utilizing the current array of diagnostic assays, up to three-quarters of the Italian-based cohort had an identifiable aetiological factor [14] (considerably greater than in some other registries). In pregnancy-associated aHUS, the yield of mutational analysis is especially high (18 of 21 patients in one cohort having a mutation identified [65]), with a pathogenic link to AP complement dysregulation also established for pre-eclampsia [66] and HELLP (Haemolysis, Elevated Liver enzymes and Low Platelets) syndrome [67]. However, the presence of a mutation in an individual with aHUS does not prove causation, with several mutations described that lack functional significance [68]. This includes an important analysis of two CFH mutations widely cited in the aHUS literature, but more likely to represent rare, non-pathogenic polymorphisms [69].
Another complicating factor in genetic assessment is the incomplete penetrance of aHUS-associated mutations, exemplified by family studies in which only half those carrying the identical mutation to the proband manifested disease [14, 70]. This suggests that several genetic risk factors may be required for phenotypic expression (the ‘multiple hit’ hypothesis). One pedigree is described in which only those family members possessing all three inherited abnormalities in complement-related genes had aHUS [71]. The cumulative impact of combined mutations, compound heterozygosity [72], at-risk SNPs/haplotypes, and autoantibodies on disease expression is increasingly recognized. Yet, a majority of aHUS patients have an additional, environmental trigger such as infection, pregnancy or drug exposure that precipitates the onset of aHUS. In some cases, this involves direct endothelial toxicity or an immune process promoting complement activation. An additional mechanism is suggested by the development of TMA after therapeutic blockade of vascular endothelial growth factor (VEGF) [73], involving loss of the endothelial protection normally provided by podocyte expression of VEGF [74].
Thrombotic thrombocytopenic purpura
Pathophysiology and clinical features
TTP is an uncommon TMA-related disorder occurring predominantly in adults [75], in which relapses are common and mortality remains 15–20% despite TPE [76]. It has been most closely associated with acquired (or rarely genetic) severe deficiency of the cleaving protease for vWF, ADAMTS13 (a disintegrin and metalloprotease with thrombospondin type 1 domains, member 13 of the family). vWF is important for primary haemostasis, inducing platelet aggregation and thrombus formation at sites of endothelial injury. Initially secreted by ECs as large multimers, vWF is degraded into progressively smaller circulating forms by ADAMTS13 under the influence of shear stress. An association between TTP and the accumulation of highly thrombogenic ‘ultra large’ (ULvWF) multimers was first noted in 1982 [77]. ADAMTS13 was identified as the vWF-cleaving protease in 1996 [78, 79], and its deficiency subsequently noted in patients with TTP [80]. ‘Congenital’ TTP (or Upshaw–Schulman syndrome) is due to compound heterozygous or homozygous mutations in the ADAMTS13 gene on chromosome 9q34, first identified using linkage analysis in four kindreds in 2001 [81]. More than 90 mutations have been described, most causing impaired protease secretion from ECs, or impaired catalytic activity (hence ‘functional’ deficiency) [82]. Penetrance is over 90%; however, congenital TTP accounts for a mere 5% of TTP cases. More commonly, ADAMTS13 deficiency due to an inhibitory autoantibody (usually IgG [83]) mediates ‘acquired’ TTP. With the exception of exposure to the antiplatelet agent ticlopidine [84], factors leading to autoantibodies in acquired TTP are unknown.
Clinical diagnosis of TTP is based on thrombocytopenia (often profound) and MAHA where no other cause of TMA is identified. The classic diagnostic ‘pentad’ [85] including also fever, neurological and renal involvement identified more advanced TMA (not specifically TTP) and is no longer relevant. Neurological features at presentation are common in patients later shown to have severe ADAMTS13 deficiency and were reported as being severe in 66 and 48% of the patients in the Oklahoma TTP registry [11] and French TMA Reference Centre cohort [12], respectively. Progression to ESKD is unusual with severe ADAMTS13 deficiency [86], although renal abnormalities including proteinuria, haematuria and mild or transient renal failure occur frequently [11, 12]. Some overlap between TTP and HUS may be attributable to intersecting pathogenic pathways, with both complement activation [87] and shiga toxin [88] able to stimulate vWF secretion from glomerular ECs and/or impair ADAMTS13 activity in vitro. Administration of shiga toxin was also required to trigger TMA in a genetically susceptible mouse strain with homozygous ADAMTS13 deficiency [89]. However, the relevance of the murine model to human TTP is uncertain, given that unprovoked TMA has not been observed in ADAMTS13 knockout mice [89, 90]. Injection of baboons with anti-ADAMTS13 antibodies was associated with immediate TTP [91].
ADAMTS13 assessment in TTP
Severe deficiency of ADAMTS13 appears to be required to cause TTP and is variably defined as <5 or <10% of normal protease activity (with a broad reference range of 40–140%) [92]. The sensitivity of severe ADAMTS13 deficiency for TTP ranged between 18 and 72% in one meta-analysis [92], attributable to differences in the proportion of patients enrolled with coexisting TMA-associated conditions. TMA in the setting of severe sepsis, malignancy, solid-organ transplantation, allogeneic haematopoietic stem cell transplantation (HSCT) and some drug exposures is less likely to involve severe protease deficiency. However, in TMA associated with autoimmune diseases, pregnancy or prior use of ticlopidine (possibly also clopidogrel), severe ADAMTS13 deficiency is commonly found. The specificity of severe ADAMTS13 deficiency for TTP is controversial, with reports of TTP being diagnosed in patients with severe protease deficiency who are subsequently found to have systemic infection [93] or malignancy [11].
ADAMTS13 assays provide prognostic information, with prospective studies suggesting that patients presenting with severe ADAMTS13 deficiency are more likely to remit with TPE and have lower mortality [94, 95]. However, this could be due to fewer life-threatening comorbidities (e.g. metastatic malignancy) in these patients. Inhibitory autoantibodies identified during the acute episode may confer a worse prognosis [96]. Once patients are in remission, a finding of severe protease deficiency or inhibitors is associated with increased risk of relapse, based on retrospective series [97, 98].
Empirical treatment approach
Diagnostic evaluation (Table 4) and treatment (Table 5) of TMA-related disorders are initiated concurrently. As clinical features are often unreliable in determining the cause of TMA, and comprehensive testing takes some time, an empirical treatment strategy is required in most patients presenting with MAHA, thrombocytopenia and renal and/or neurological dysfunction. Guidelines produced in 2009 by the European Paediatric Study Group for HUS recommend ‘urgent and empirical’ TPE with fresh frozen plasma (FFP) or solvent-treated plasma, once STEC (and, if suspected, invasive pneumococcus) have been excluded in children [1]. Evidence for plasma therapy in children with STEC-HUS is lacking, with a 2009 Cochrane systematic review finding none of the additional measures used in children with post-diarrhoeal HUS was superior to supportive care alone [99]. However, this review has been criticized for the inclusion of studies in which the aetiology of TMA was not established, including both the randomized controlled trials (RCTs) in which plasma infusion was not beneficial [100]. In children with aHUS, plasma therapy is recommended [1, 101], based on case reports and registry data, but not prospective trials. TPE is preferred to plasma infusion although evidence is limited to a case report showing differential outcomes in twin 5-year-old girls with a familial CFH mutation [102]. The volume requirements for plasma infusion in small children with renal impairment may necessitate exchange.
Table 4.
Diagnostic tests
| Shiga toxin |
| Stool culture for E. coli plus either toxicology for shiga toxin or PCR for shiga toxin gene |
| Urine culture for E. coli |
| Other bacterial testing as indicated |
| S. pneumoniae |
| T antigen expression on red cells |
| PCR of blood and/or secretions |
| Blood culture |
| Complement dysregulation |
| Plasma/serum protein levels |
| C3 |
| Factor H, factor I, factor B |
| MCP (CD46) expression on PBMCs |
| Factor H autoantibodies |
| Mutations |
| Direct exon sequencing of CFH, MCP, CFI, CFB, C3 |
| Copy number variation across CFH-CFHR locus |
| ADAMTS13 deficiency |
| ADAMTS13 activity |
| ADAMTS13 autoantibodies |
| ADAMTS13 mutations |
| Other associations |
| Pregnancy test |
| Liver and pancreas enzymes |
| Cobalamin (B12), homocysteine assay, methylmalonic acid (plasma and urine) ± mutation analysis of MMACHC gene |
| HIV and other viral serology as indicated |
| ANA, lupus anticoagulant, antiphospholipid antibodies |
| Pharyngeal swab and viral PCR for influenza A (H1N1) |
Table 5.
Treatment
| (i) Supportive measures only |
| Paediatric STEC-HUS and invasive pneumococcal infection (p-HUS) |
| Cobalamin deficiency (children), HSCT- or malignancy-associated TMA, malignant HT |
| (ii) Therapeutic plasma exchange (TPE) |
| First exclude paediatric STEC-HUS and p-HUS |
| Recommended in all other settings |
| Including TTP and aHUS (probably of no benefit in MCP-aHUS) |
| Controversial in adult STEC-HUS |
| Plasma infusion recommended in known congenital TTP |
| (iii) Eculizumab |
| aHUS |
| (iv) Steroids and/or rituximab |
| Possibly in acquired TTP and aHUS with factor H autoantibodies |
| (v) Renal transplantation for ESKD |
| STEC-HUS |
| MCP-aHUS |
| Living-related donation contraindicated |
| (vi) Prophylactic strategies in high-risk transplantation (i.e. non-MCP aHUS) |
| Intensive perioperative TPE |
| Eculizumab |
| Rituximab (for factor H autoantibodies) |
| Combined kidney–liver transplantation |
Mortality in adults with a clinical diagnosis of TTP, prior to the widespread use of plasma therapy, was as high as 90% [85]. In contrast, a 1991 RCT [103] demonstrated mortality of 22% in adults receiving TPE and 37% in those receiving plasma infusion (notwithstanding that the trial population may have had less severe disease at diagnosis). The 2009 Cochrane review concluded that TPE is superior to plasma infusion in the treatment of TTP, with no additional benefit from antiplatelet therapy or the substitution of cryosupernatant for FFP during exchange [99]. As TPE appears to be beneficial irrespective of severe protease deficiency [11], treatment should not be delayed while awaiting results of ADAMTS 13 testing. In patients known to have the congenital form of TTP, isolated infusion of plasma (first described with success over 50 years ago [104]), cryoprecipitate or plasma-derived vWF concentrates is the current recommendation [105].
Owing to the greater likelihood of TTP in adults, and its potentially fulminant course [106], many centres perform TPE empirically in adults even prior to the exclusion of STEC-HUS [107]. If plasma therapy is commenced empirically, the results of STEC and ADAMTS13 assays guide further management. In those with severe ADAMTS13 deficiency and no evidence of STEC infection, consideration may be given to adjunctive immunosuppressive treatment for TTP (discussed below). The diagnosis remains uncertain if neither STEC infection nor severe protease deficiency is found, although many such patients (especially those with significant renal failure) will have aHUS. This patient group matches the inclusion criteria for aHUS in Phase II trials reporting benefit with eculizumab (discussed below). In adult cases where STEC infection is diagnosed after TPE has been started, consideration may be given to stopping TPE. However, some groups advocate TPE in adults with STEC-HUS, particularly in the presence of severe renal or neurological involvement [108]. This is despite the absence of data from appropriately controlled trials, with published evidence consisting until recently of a single retrospective cohort analysis in elderly patients [109]. TPE was frequently used during the recent German STEC-HUS outbreak [21], mostly in adults with severe disease but also in some children [22]. A Danish subset of five adult patients has been reported with apparent benefit [110], while other outcome data are awaited. Uncontrolled reports of the efficacy of immunoadsorption in patients with severe neurological complications of STEC-HUS during this epidemic [111] and one other [112] have also been published.
In a restricted number of settings, TPE is deferred or ceased. This includes cobalamin (vitamin B12) deficiency in children, for which screening is recommended and treatment with parenteral hydroxycobalamin is effective. In adults with HSCT- or malignancy-associated TMA, plasma therapy is not generally thought beneficial. Blood pressure control is essential for patients with malignant HT as a cause of TMA, although the possibility of underlying aHUS or TTP should be recognized, and consideration also given to starting TPE. Where TPE is indicated but not immediately available, plasma infusion should be commenced pending urgent transfer to a centre offering TPE. If clinical or biochemical response is not attained, or relapse recurs, TPE may be intensified either by increasing the volume of exchange or performing twice-daily TPE. Additional strategies for refractory or relapsing disease are discussed below. In both TTP [113] and aHUS [114], opinion is divided as regards weaning or prompt cessation of TPE following a response to treatment.
Eculizumab in aHUS
Eculizumab is a humanized monoclonal antibody inhibiting C5 activation, a critical effector mechanism in the murine model of aHUS [115]. Recently approved in the USA and Europe as first-line treatment for aHUS, eculizumab was initially reported with efficacy in cases that were refractory to plasma therapy and/or relapsing [116–121], including after renal transplantation (discussed below). Interim data (published in abstract form only) from prospective, uncontrolled Phase II trials show a favourable response in patients with plasma-resistant [122] and plasma-dependent [123] aHUS. Whereas maintenance therapy appears to be effective [124] and was used in the clinical trials, discontinuation has been reported anecdotally with severe relapse [125, 126]. The question of long-term use of eculizumab in aHUS requires further evaluation in clinical trials, especially in view of the very high cost of treatment. Based on reports in pregnant women with paroxysmal nocturnal haemoglobinuria, use of eculizumab in pregnancy may be safe [127]. Inhibition of C5 activation creates vulnerability to meningococcal infections, and immunization with a polyvalent meningococcal vaccine is mandatory prior to initiation of eculizumab. Patients remain susceptible to serotypes not covered by the vaccine. Prompted by a report of its successful use in three children with STEC-HUS [26], eculizumab was extensively used in adults during the STEC-HUS epidemic in Germany, forming the basis for Phase II and III clinical trials (ClinicalTrials.gov NCT01410916). However, eculizumab is not currently approved for this indication.
While many patients with aHUS respond initially to plasma therapy (over two-thirds of those treated in the Italian-based cohort achieving at least a partial response [14]), overall outcomes are poor. Together with the approval of eculizumab, this has prompted a reappraisal of the reliance of empiric treatment protocols on TPE alone. For example in a child in whom STEC-HUS and pneumococcal sepsis have been excluded, a provisional diagnosis of aHUS is arguably sufficient for the commencement of eculizumab. Similar considerations regarding the empirical use of eculizumab may arise in adults with predominant renal manifestations of TMA in whom STEC and ADAMTS13 testing is negative. One suggested strategy in this category of adult patients involves switching to eculizumab if initial response to TPE is poor [128]. Regardless of the initial treatment approach, a provisional diagnosis of aHUS should prompt investigations for complement dysregulation including protein levels, gene sequencing and structural analysis and autoantibody testing (cognisant that complement protein concentrations are altered if TPE is begun).
Immunosuppression
In TTP, the overall response to plasma therapy is ∼80% [129], although one-third of patients entering remission will subsequently relapse [11]. As most TTP is autoimmune, patients who respond poorly or relapse often receive adjunctive immunosuppressive therapy with TPE. Some groups recommend steroids in all patients suspected of having acquired TTP [113], although this has not been assessed in a placebo-controlled trial. One RCT compared intravenous methylprednisolone in a high-dose (10 mg/kg/day for 3 days, then 2.5 mg/kg/day) versus low-dose (1 mg/kg/day) regimen in 60 patients receiving TPE for acute new-onset or relapsing TTP [130]. A significant increase in complete remission rate at 23 days was observed in the group receiving high-dose steroids; however, this group had also received more TPE following a statistically non-significant benefit at 9 days (the primary study outcome). A correlation between steroid responsiveness and the severity of ADAMTS13 deficiency or presence of inhibitors has not been shown although in some studies, immunosuppressive use was restricted to cases of severe protease deficiency [131]. Evidence for steroids in aHUS is lacking (notwithstanding a theoretical benefit in those with factor H autoantibodies).
The anti-CD 20 monoclonal antibody rituximab has been assessed prospectively in small series of adult TTP either refractory to TPE [131–133] or relapsing [131, 133, 134]. While rituximab was safe and appeared to be beneficial in inducing remission (usually in conjunction with TPE and steroids), median follow-up periods were less than 1 year. A recent prospective, non-randomized Phase II trial of adjunctive rituximab involving 34 adults with new-onset TTP, and an additional 6 patients with an acute relapse of TTP, showed a lower relapse rate at a median follow-up of 27 months compared with historical controls [134]. Alternative immunosuppressive therapies for TTP, including vincristine, cyclophosphamide, cyclosporine as well as splenectomy, lack prospective data and are now used infrequently. A number of novel agents designed to block vWF interaction with its platelet receptor are undergoing clinical evaluation [135]. Isolated reports in patients with factor H autoantibody-associated aHUS suggest benefit with immunosuppressive medications [47, 135] and rituximab [47, 136].
Transplantation
In the rare setting of ESKD due to STEC-HUS, transplantation is generally recurrence-free. In contrast, recurrence of aHUS was reported in 60% of transplant recipients in one meta-analysis, with over 90% subsequent graft loss despite plasma therapy [137]. Genetic analysis enables a more refined prediction of recurrence [138] and is an essential component of pre-transplant assessment for patients with aHUS. In those with CFH mutations (the most commonly recognized genetic abnormality), the risk of recurrent disease is in the order of 80% [137], whereas for MCP-aHUS, the recurrence rate is low. This is presumably because wild-type MCP expressed in the vascular endothelium of the donor kidney restores local complement regulation. Recurrent MCP-aHUS has been reported where microchimaerism was observed within graft endothelium [139] and in patients with additional CFH or CFI mutations [140] (despite the earlier suggestion that allograft expression of MCP might be protective [141]). Overall, poor outcomes are reported for all non-MCP mutations [13, 14, 55, 137], factor H autoantibodies [47] and cases where no underlying defect has been demonstrated. Living-related renal transplantation is contraindicated, regardless of the results of genetic screening, because of the risk of familial disease due to unrecognized genetic susceptibility factors. In addition to the risk of recurrence in recipients, there have been reports of aHUS in the previously asymptomatic related kidney donors [142], seemingly triggered by donor nephrectomy.
Treatment of recurrent or de novo aHUS post-transplantation, consisting of TPE (with or without reduction in calcineurin inhibitors), has often been unsuccessful [143]. Response to eculizumab has been reported in plasma-refractory cases [144–149] and in the Phase II trials [122, 123] (notwithstanding additional reports of graft loss in patients who had received a single dose of eculizumab [114, 138]). In recipients at high risk of recurrence due to non-MCP mutations, a perioperative strategy involving intensive TPE has been reported with good long-term results [150–153] (but also with one graft failure following a reduction in frequency of exchanges [150]). Prophylactic administration of eculizumab is reported as effective either alone or in combination with TPE [154–157]. In patients with factor H autoantibodies, successful transplantation has been reported with intensive perioperative TPE [158], coadministration of rituximab [47, 136] or neither [159].
An alternative strategy in ‘high-risk’ patients with non-MCP-aHUS is combined kidney–liver transplantation, with the transplanted liver correcting complement dysregulation through production of wild-type complement proteins [160]. However, this procedure is associated with significant morbidity and mortality, with poor outcomes initially reported in children with CFH mutations and life-threatening disease [161–163]. These have been followed by several successful reports in CFH-aHUS [164–166], and one each in CFB-aHUS [167] and combined CFH/CFI-aHUS [168], using pre- and post-operative TPE, heparin and low-dose aspirin. Guidelines to patient selection for combined liver–kidney transplantation have been published [169]. A single case is reported also of pre-emptive isolated split liver transplant with good graft and native renal function at 2 years [170].
Conclusions
The past decade has seen an extraordinary increase in the understanding of molecular mechanisms mediating TMA, significantly changing approaches to diagnosis and treatment. In accordance with international guidelines, the current mainstay of treatment is the ‘urgent and empirical’ institution of plasma therapy, once paediatric STEC and invasive pneumococcal infection are excluded. Molecular diagnostic techniques are becoming more widely available and are critical to risk stratification for transplantation. Emerging evidence suggests that anti-complement C5 therapy with eculizumab is effective in aHUS. The enrolment of patients with STEC-HUS, aHUS and TTP into registries and clinical trials should further refine empiric treatment and facilitate an evidence-based shift towards more specific and effective therapies. An exciting era beckons where the inexorable progression to ESKD, systemic complications and premature death may be interrupted, with the prospect of renal recovery and long-term avoidance of recurrent disease.
Acknowledgements
T.B. is a Kidney Research UK (KRUK) Clinical Research Fellow (TF12/2011). P.H., S.C. and S.J. have served on advisory boards for Alexion regarding the use of eculizumab in aHUS and/or antibody-mediated renal transplant rejection. P.H. is an investigator on the clinical trial of an anti-von Willebrand factor nanobody (ALX-0081) in TTP sponsored by Ablynx.
Conflict of interest statement. None declared.
References
- 1.Ariceta G, Besbas N, Johnson S, et al. Guideline for the investigation and initial therapy of diarrhea-negative hemolytic uremic syndrome. Pediatr Nephrol. 2009;24:687–696. doi: 10.1007/s00467-008-0964-1. [DOI] [PubMed] [Google Scholar]
- 2.Symmers WS. Thrombotic microangiopathic haemolytic anaemia (thrombotic microangiopathy) Br Med J. 1952;2:897–903. doi: 10.1136/bmj.2.4790.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brain MC, Dacie JV, Hourihane DO. Microangiopathic haemolytic anaemia: the possible role of vascular lesions in pathogenesis. Br J Haematol. 1962;8:358–374. doi: 10.1111/j.1365-2141.1962.tb06541.x. [DOI] [PubMed] [Google Scholar]
- 4.Park YA, Waldrum MR, Marques MB. Platelet count and prothrombin time help distinguish thrombotic thrombocytopenic purpura-hemolytic uremic syndrome from disseminated intravascular coagulation in adults. Am J Clin Pathol. 2010;133:460–465. doi: 10.1309/AJCPPNF63FLIORCI. [DOI] [PubMed] [Google Scholar]
- 5.Moschcowitz E. An acute febrile pleiochromic anemia with hyaline thrombosis of the terminal arterioles and capillaries: an undescribed disease. Arch Intern Med. 1925;36:89–93. [PubMed] [Google Scholar]
- 6.Gasser C, Gautier E, Steck A, et al. Hämolytisch-urämische Syndrome: bilaterale Nierenrindennekrosen bei akuten erworbenen hämolytischen Anämien. Schweiz Med Wochenschr. 1955;85:905–909. [PubMed] [Google Scholar]
- 7.Hosler GA, Cusumano AM, Hutchins GM. Thrombotic thrombocytopenic purpura and hemolytic uremic syndrome are distinct pathological entities. Arch Pathol Lab Med. 2003;127:834–839. doi: 10.5858/2003-127-834-TTPAHU. [DOI] [PubMed] [Google Scholar]
- 8.Besbas N, Karpman D, Landau D, et al. A classification of hemolytic uremic syndrome and thrombotic thrombocytopenic purpura and related disorders. Kidney Int. 2006;70:423–431. doi: 10.1038/sj.ki.5001581. [DOI] [PubMed] [Google Scholar]
- 9.Nathanson S, Kwon T, Elmaleh M, et al. Acute neurological involvement in diarrhea-associated hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2010;5:1218–1228. doi: 10.2215/CJN.08921209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koehl B, Boyer O, Biebuyck-Gougé N, et al. Neurological involvement in a child with atypical hemolytic uremic syndrome. Pediatr Nephrol. 2010;25:2539–2542. doi: 10.1007/s00467-010-1606-y. [DOI] [PubMed] [Google Scholar]
- 11.Kremer Hovinga JA, Vesely SK, Terrell DR, et al. Survival and relapse in patients with thrombotic thrombocytopenic purpura. Blood. 2010;115:1500–1511. doi: 10.1182/blood-2009-09-243790. [DOI] [PubMed] [Google Scholar]
- 12.Coppo P, Schwarzinger M, Buffet M, et al. Predictive features of severe acquired ADAMTS13 deficiency in idiopathic thrombotic microangiopathies: the French TMA reference center experience. PLoS One. 2010;5:e10208. doi: 10.1371/journal.pone.0010208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sellier-Leclerc A-L, Frémeaux-Bacchi V, Dragon-Durey M-A, et al. Differential impact of complement mutations on clinical characteristics in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2007;18:2392–2400. doi: 10.1681/ASN.2006080811. [DOI] [PubMed] [Google Scholar]
- 14.Noris M, Caprioli J, Bresin E, et al. Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol. 2010;5:1844–1859. doi: 10.2215/CJN.02210310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geerdink LM, Westra D, van Wijk JA, et al. Atypical hemolytic uremic syndrome in children: complement mutations and clinical characteristics. Pediatr Nephrol. 2012 doi: 10.1007/s00467-012-2131-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karmali MA, Steele BT, Petric M, et al. Sporadic cases of haemolytic-uraemic syndrome associated with faecal cytotoxin and cytotoxin-producing Escherichia coli in stools. Lancet. 1983;1:619–620. doi: 10.1016/s0140-6736(83)91795-6. [DOI] [PubMed] [Google Scholar]
- 17.Karpman D, Sartz L, Johnson S. Pathophysiology of typical hemolytic uremic syndrome. Semin Thromb Hemost. 2010;36:575–585. doi: 10.1055/s-0030-1262879. [DOI] [PubMed] [Google Scholar]
- 18.Noris M, Remuzzi G. Hemolytic uremic syndrome. J Am Soc Nephrol. 2005;16:1035–1050. doi: 10.1681/ASN.2004100861. [DOI] [PubMed] [Google Scholar]
- 19.Brandt J, Wong C, Mihm S, et al. Invasive pneumococcal disease and hemolytic uremic syndrome. Pediatrics. 2002;110(2 Pt 1):371–376. doi: 10.1542/peds.110.2.371. [DOI] [PubMed] [Google Scholar]
- 20.Frank C, Werber D, Cramer JP, et al. Epidemic profile of Shiga-toxin-producing Escherichia coli O104:H4 outbreak in Germany. N Engl J Med. 2011;365:1771–1780. doi: 10.1056/NEJMoa1106483. [DOI] [PubMed] [Google Scholar]
- 21.The German EHEC-HUS Registry. The German 2011 epidemic of Shiga toxin-producing E. coli—the nephrological view. Nephrol Dial Transplant. 2011;26:2723–2726. doi: 10.1093/ndt/gfr462. [DOI] [PubMed] [Google Scholar]
- 22.Kemper MJ. Outbreak of hemolytic uremic syndrome caused by E. coli O104:H4 in Germany: a pediatric perspective. Pediatr Nephrol. 2012;27:161–164. doi: 10.1007/s00467-011-2067-7. [DOI] [PubMed] [Google Scholar]
- 23.Goldwater PN, Bettelheim KA. An outbreak of hemolytic uremic syndrome due to Escherichia coli O157:H7: or was it? Emerg Infect Dis. 1996;2:153–154. doi: 10.3201/eid0202.960218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buchholz U, Bernard H, Werber D, et al. German outbreak of Escherichia coli O104:H4 associated with sprouts. N Engl J Med. 2011;365:1763–1770. doi: 10.1056/NEJMoa1106482. [DOI] [PubMed] [Google Scholar]
- 25.Fang CJ, Frémeaux-Bacchi V, Liszewski MK, et al. Membrane cofactor protein mutations in atypical hemolytic uremic syndrome (aHUS), fatal Stx-HUS, C3 glomerulonephritis, and the HELLP syndrome. Blood. 2008;111:624–632. doi: 10.1182/blood-2007-04-084533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lapeyraque AL, Malina M, Frémeaux-Bacchi V, et al. Eculizumab in severe Shiga-toxin-associated HUS. N Engl J Med. 2011;364:2561–2563. doi: 10.1056/NEJMc1100859. [DOI] [PubMed] [Google Scholar]
- 27.Noris M, Remuzzi G. Atypical hemolytic-uremic syndrome. N Engl J Med. 2009;361:1676–1687. doi: 10.1056/NEJMra0902814. [DOI] [PubMed] [Google Scholar]
- 28.Sallée M, Daniel L, Piercecchi MD, et al. Myocardial infarction is a complication of factor H-associated atypical HUS. Nephrol Dial Transplant. 2010;25:2028–2032. doi: 10.1093/ndt/gfq160. [DOI] [PubMed] [Google Scholar]
- 29.Edey MM, Mead PA, Saunders RE, et al. Association of a factor H mutation with hemolytic uremic syndrome following a diarrheal illness. Am J Kidney Dis. 2008;51:487–490. doi: 10.1053/j.ajkd.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 30.Kerr H, Richards A. Complement-mediated injury and protection of endothelium: lessons from atypical haemolytic uraemic syndrome. Immunobiology. 2012;217:195–203. doi: 10.1016/j.imbio.2011.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cameron JS, Vick R. Plasma-C3 in hæmolytic-uræmic syndrome and thrombotic thrombocytopenic purpura. Lancet. 1973;302:975. doi: 10.1016/s0140-6736(73)92645-7. [DOI] [PubMed] [Google Scholar]
- 32.Campbell S, Carre IJ. Fatal haemolytic uraemic syndrome and idiopathic hyperlipaemia in monozygotic twins. Arch Dis Child. 1965;40:654–658. doi: 10.1136/adc.40.214.654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warwicker P, Goodship THJ, Donne RL, et al. Genetic studies into inherited and sporadic hemolytic uremic syndrome. Kidney Int. 1998;53:836–844. doi: 10.1111/j.1523-1755.1998.00824.x. [DOI] [PubMed] [Google Scholar]
- 34.Thompson RA, Winterborn MH. Hypocomplementaemia due to a genetic deficiency of beta 1H globulin. Clin Exp Immunol. 1981;46:110–119. [PMC free article] [PubMed] [Google Scholar]
- 35.Manuelian T, Hellwage J, Meri S, et al. Mutations in factor H reduce binding affinity to C3b and heparin and surface attachment to endothelial cells in hemolytic uremic syndrome. J Clin Invest. 2003;111:1181–1190. doi: 10.1172/JCI16651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pickering MC, Goicoechea de Jorge E, Martínez-Barricarte R, et al. Spontaneous hemolytic uremic syndrome triggered by complement factor H lacking surface recognition domains. J Exp Med. 2007;204:1249–1256. doi: 10.1084/jem.20070301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pechtl IC, Kavanagh D, McIntosh N, et al. Disease-associated N-terminal complement factor H mutations perturb cofactor and decay-accelerating activities. J Biol Chem. 2011;286:11082–11090. doi: 10.1074/jbc.M110.211839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pickering MC, Cook HT. Translational mini-review series on complement factor H: renal diseases associated with complement factor H: novel insights from humans and animals. Clin Exp Immunol. 2008;151:210–230. doi: 10.1111/j.1365-2249.2007.03574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dragon-Durey MA, Loirat C, Cloarec S, et al. Anti-Factor H autoantibodies associated with atypical hemolytic uremic syndrome. J?Am Soc Nephrol. 2005;16:555–563. doi: 10.1681/ASN.2004050380. [DOI] [PubMed] [Google Scholar]
- 40.Józsi M, Strobel S, Dahse HM, et al. Anti factor H autoantibodies block C-terminal recognition function of factor H in hemolytic uremic syndrome. Blood. 2007;110:1516–1518. doi: 10.1182/blood-2007-02-071472. [DOI] [PubMed] [Google Scholar]
- 41.Józsi M, Licht C, Strobel S, et al. Factor H autoantibodies in atypical hemolytic uremic syndrome correlate with CFHR1/CFHR3 deficiency. Blood. 2008;111:1512–1514. doi: 10.1182/blood-2007-09-109876. [DOI] [PubMed] [Google Scholar]
- 42.Zipfel PF, Edey M, Heinen S, et al. Deletion of complement factor H-related genes CFHR1 and CFHR3 is associated with atypical hemolytic uremic syndrome. PLoS Genet. 2007;3:e41. doi: 10.1371/journal.pgen.0030041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abarrategui-Garrido C, Martínez-Barricarte R, López-Trascasa M, et al. Characterization of complement factor H-related (CFHR) proteins in plasma reveals novel genetic variations of CFHR1 associated with atypical hemolytic uremic syndrome. Blood. 2009;114:4261–4271. doi: 10.1182/blood-2009-05-223834. [DOI] [PubMed] [Google Scholar]
- 44.Moore I, Strain L, Pappworth I, et al. Association of factor H autoantibodies with deletions of CFHR1, CFHR3, CFHR4, and with mutations in CFH, CFI, CD46, and C3 in patients with atypical hemolytic uremic syndrome. Blood. 2010;115:379–387. doi: 10.1182/blood-2009-05-221549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Venables JP, Strain L, Routledge D, et al. Atypical haemolytic uraemic syndrome associated with a hybrid complement gene. PLoS Med. 2006;3:e431. doi: 10.1371/journal.pmed.0030431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Francis NJ, McNicholas B, Awan A, et al. A novel hybrid CFH/CFHR3 gene generated by a microhomology-mediated deletion in familial atypical hemolytic uremic syndrome. Blood. 2012;119:591–601. doi: 10.1182/blood-2011-03-339903. [DOI] [PubMed] [Google Scholar]
- 47.Dragon-Durey MA, Sethi SK, Bagga A, et al. Clinical features of anti-factor h autoantibody-associated hemolytic uremic syndrome. J Am Soc Nephrol. 2010;21:2180–2187. doi: 10.1681/ASN.2010030315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Noris M, Brioschi S, Caprioli J, et al. Familial haemolytic uraemic?syndrome and an MCP mutation. Lancet. 2003;362:1542–1547. doi: 10.1016/S0140-6736(03)14742-3. [DOI] [PubMed] [Google Scholar]
- 49.Richards A, Kemp EJ, Liszewski MK, et al. Mutations in human complement regulator, membrane cofactor protein (CD46), predispose to development of familial hemolytic uremic syndrome. Proc Natl Acad Sci USA. 2003;100:12966–12971. doi: 10.1073/pnas.2135497100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Frémeaux-Bacchi V, Dragon-Durey MA, Blouin J, et al. Complement factor I: a susceptibility gene for atypical haemolytic uraemic syndrome. J Med Genet. 2004;41:e84. doi: 10.1136/jmg.2004.019083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bienaimé F, Dragon-Durey MA, Regnier CH, et al. Mutations in components of complement influence the outcome of Factor I-associated atypical hemolytic uremic syndrome. Kidney Int. 2010;77:339–349. doi: 10.1038/ki.2009.472. [DOI] [PubMed] [Google Scholar]
- 52.Kavanagh D, Pappworth IY, Anderson H, et al. Factor I autoantibodies in patients with atypical hemolytic uremic syndrome: disease-associated or an epiphenomenon? Clin J Am Soc Nephrol. 2012;7:417–426. doi: 10.2215/CJN.05750611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ståhl AL, Kristoffersson A, Olin AI, et al. A novel mutation in the complement regulator clusterin in recurrent hemolytic uremic syndrome. Mol Immunol. 2009;46:2236–2243. doi: 10.1016/j.molimm.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 54.Fremeaux-Bacchi V, Miller EC, Liszewski MK, et al. Mutations in complement C3 predispose to development of atypical hemolytic uremic syndrome. Blood. 2008;112:4948–4952. doi: 10.1182/blood-2008-01-133702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Goicoechea de Jorge E, Harris CL, Esparza-Gordillo J, et al. Gain-of-function mutations in complement factor B are associated with atypical hemolytic uremic syndrome. Proc Natl Acad Sci USA. 2007;104:240–245. doi: 10.1073/pnas.0603420103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Delvaeye M, Noris M, De Vriese A, et al. Thrombomodulin mutations in atypical hemolytic-uremic syndrome. N Engl J Med. 2009;361:345–357. doi: 10.1056/NEJMoa0810739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Conway EM. Thrombomodulin and its role in inflammation. Semin Immunopathol. 2012;34:107–125. doi: 10.1007/s00281-011-0282-8. [DOI] [PubMed] [Google Scholar]
- 58.Amara U, Flierl MA, Rittirsch D, et al. Molecular intercommunication between the complement and coagulation systems. J Immunol. 2010;185:5628–5636. doi: 10.4049/jimmunol.0903678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kavanagh D, Goodship T. Genetics and complement in atypical HUS. Pediatr Nephrol. 2010;25:2431–2442. doi: 10.1007/s00467-010-1555-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Caprioli J, Castelletti F, Bucchioni S, et al. Complement factor H mutations and gene polymorphisms in haemolytic uraemic syndrome: the C-257T, the A2089G and the G2881T polymorphisms are strongly associated with the disease. Hum Mol Genet. 2003;12:3385–3395. doi: 10.1093/hmg/ddg363. [DOI] [PubMed] [Google Scholar]
- 61.Frémeaux-Bacchi V, Kemp EJ, Goodship JA, et al. The development of atypical haemolytic-uraemic syndrome is influenced by susceptibility factors in factor H and membrane cofactor protein: evidence from two independent cohorts. J Med Genet. 2005;42:852–856. doi: 10.1136/jmg.2005.030783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Blom AM, Bergström F, Edey M, et al. A novel non-synonymous polymorphism (p.Arg240His) in C4b-binding protein is associated with atypical hemolytic uremic syndrome and leads to impaired alternative pathway cofactor activity. J Immunol. 2008;180:6385–6391. doi: 10.4049/jimmunol.180.9.6385. [DOI] [PubMed] [Google Scholar]
- 63.Esparza-Gordillo J, Goicoechea de Jorge E, Buil A, et al. Predisposition to atypical hemolytic uremic syndrome involves the concurrence of different susceptibility alleles in the regulators of complement activation gene cluster in 1q32. Hum Mol Genet. 2005;14:703–712. doi: 10.1093/hmg/ddi066. [DOI] [PubMed] [Google Scholar]
- 64.Ermini L, Goodship TH, Strain L, et al. Common genetic variants in complement genes other than CFH, CD46 and the CFHRs are not associated with aHUS. Mol Immunol. 2012;49:640–648. doi: 10.1016/j.molimm.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fakhouri F, Roumenina L, Provot F, et al. Pregnancy-associated hemolytic uremic syndrome revisited in the era of complement gene mutations. J Am Soc Nephrol. 2010;21:859–867. doi: 10.1681/ASN.2009070706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Salmon JE, Heuser C, Triebwasser M, et al. Mutations in complement regulatory proteins predispose to preeclampsia: a genetic analysis of the PROMISSE cohort. PLoS Med. 2011;8:e1001013. doi: 10.1371/journal.pmed.1001013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fakhouri F, Jablonski M, Lepercq J, et al. Factor H, membrane cofactor protein, and factor I mutations in patients with hemolysis, elevated liver enzymes, and low platelet count syndrome. Blood. 2008;112:4542–4545. doi: 10.1182/blood-2008-03-144691. [DOI] [PubMed] [Google Scholar]
- 68.Roumenina LT, Loirat C, Dragon-Durey MA, et al. Alternative complement pathway assessment in patients with atypical HUS. J Immunol Methods. 2011;365:8–26. doi: 10.1016/j.jim.2010.12.020. [DOI] [PubMed] [Google Scholar]
- 69.Tortajada A, Pinto S, Martínez-Ara J, et al. Complement factor H variants I890 and L1007 while commonly associated with atypical hemolytic uremic syndrome are polymorphisms with no functional significance. Kidney Int. 2012;81:56–63. doi: 10.1038/ki.2011.291. [DOI] [PubMed] [Google Scholar]
- 70.Sullivan M, Erlic Z, Hoffmann MM, et al. Epidemiological approach to identifying genetic predispositions for atypical hemolytic uremic syndrome. Ann Hum Genet. 2010;74:17–26. doi: 10.1111/j.1469-1809.2009.00554.x. [DOI] [PubMed] [Google Scholar]
- 71.Esparza-Gordillo J, Jorge EG, Garrido CA, et al. Insights into hemolytic uremic syndrome: segregation of three independent predisposition factors in a large, multiple affected pedigree. Mol Immunol. 2006;43:1769–1775. doi: 10.1016/j.molimm.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 72.Johnson SA, Williams JM, Hakobyan S, et al. Impact of compound heterozygous complement factor H mutations on development of atypical hemolytic uremic syndrome-A pedigree revisited. Mol Immunol. 2010;47:1585–1591. doi: 10.1016/j.molimm.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 73.Eremina V, Jefferson JA, Kowalewska J, et al. VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med. 2008;358:1129–1136. doi: 10.1056/NEJMoa0707330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Goldberg RJ, Nakagawa T, Johnson RJ, et al. The role of endothelial cell injury in thrombotic microangiopathy. Am J Kidney Dis. 2010;56:1168–1174. doi: 10.1053/j.ajkd.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.George JN. Thrombotic thrombocytopenic purpura. N Engl J Med. 2006;354:1927–1935. doi: 10.1056/NEJMcp053024. [DOI] [PubMed] [Google Scholar]
- 76.Frawley N, Ng AP, Nicholls K, et al. Thrombotic thrombocytopenic purpura is associated with a high relapse rate after plasma exchange: a single-centre experience. Intern Med J. 2009;39:19–24. doi: 10.1111/j.1445-5994.2008.01637.x. [DOI] [PubMed] [Google Scholar]
- 77.Moake JL, Rudy CK, Troll JH, et al. Unusually large plasma factor VIII: von Willebrand factor multimers in chronic relapsing thrombotic thrombocytopenic purpura. N Engl J Med. 1982;307:1432–1435. doi: 10.1056/NEJM198212023072306. [DOI] [PubMed] [Google Scholar]
- 78.Furlan M, Robles R, Lämmle B. Partial purification and characterization of a protease from human plasma cleaving von Willebrand factor to fragments produced by in vivo proteolysis. Blood. 1996;87:4223–4234. [PubMed] [Google Scholar]
- 79.Tsai HM. Physiologic cleavage of von Willebrand factor by a plasma protease is dependent on its conformation and requires calcium ion. Blood. 1996;87:4235–4244. [PubMed] [Google Scholar]
- 80.Furlan M, Robles R, Solenthaler M, et al. Deficient activity of von Willebrand factor-cleaving protease in chronic relapsing thrombotic thrombocytopenic purpura. Blood. 1997;89:3097–3103. [PubMed] [Google Scholar]
- 81.Levy GG, Nichols WC, Lian EC, et al. Mutations in a member of the ADAMTS gene family cause thrombotic thrombocytopenic purpura. Nature. 2001;413:488–494. doi: 10.1038/35097008. [DOI] [PubMed] [Google Scholar]
- 82.Tsai HM. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010;91:1–19. doi: 10.1007/s12185-009-0476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ferrari S, Scheiflinger F, Rieger M, et al. Prognostic value of anti-ADAMTS 13 antibody features (Ig isotype, titer, and inhibitory effect) in a cohort of 35 adult French patients undergoing a first episode of thrombotic microangiopathy with undetectable ADAMTS 13 activity. Blood. 2007;109:2815–2822. doi: 10.1182/blood-2006-02-006064. [DOI] [PubMed] [Google Scholar]
- 84.Tsai HM, Rice L, Sarode R, et al. Antibody inhibitors to von Willebrand factor metalloproteinase and increased binding of von Willebrand factor to platelets in ticlopidine-associated thrombotic thrombocytopenic purpura. Ann Intern Med. 2000;132:794–799. doi: 10.7326/0003-4819-132-10-200005160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Amorosi EL, Ultmann JE. Thrombotic thromocytopenic purpura: report of 16 cases and review of the literature. Medicine (Baltimore) 1966;45:139–159. [Google Scholar]
- 86.Tsai HM. The kidney in thrombotic thrombocytopenic purpura. Minerva Med. 2007;98:731–747. [PMC free article] [PubMed] [Google Scholar]
- 87.Hattori R, Hamilton KK, McEver RP, et al. Complement proteins C5b-9 induce secretion of high molecular weight multimers of endothelial von Willebrand factor and translocation of granule membrane protein GMP-140 to the cell surface. J Biol Chem. 1989;264:9053–9060. [PubMed] [Google Scholar]
- 88.Nolasco LH, Turner NA, Bernardo A, et al. Hemolytic uremic syndrome-associated Shiga toxins promote endothelial-cell secretion and impair ADAMTS13 cleavage of unusually large von Willebrand factor multimers. Blood. 2005;106:4199–4209. doi: 10.1182/blood-2005-05-2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Motto DG, Chauhan AK, Zhu G, et al. Shigatoxin triggers thrombotic thrombocytopenic purpura in genetically susceptible ADAMTS13-deficient mice. J Clin Invest. 2005;115:2752–2761. doi: 10.1172/JCI26007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Banno F, Kokame K, Okuda T, et al. Complete deficiency in ADAMTS13 is prothrombotic, but it alone is not sufficient to cause thrombotic thrombocytopenic purpura. Blood. 2006;107:3161–3166. doi: 10.1182/blood-2005-07-2765. [DOI] [PubMed] [Google Scholar]
- 91.Feys HB, Roodt J, Vandeputte N, et al. Thrombotic thrombocytopenic purpura directly linked with ADAMTS13 inhibition in the baboon (Papio ursinus) Blood. 2010;116:2005–2010. doi: 10.1182/blood-2010-04-280479. [DOI] [PubMed] [Google Scholar]
- 92.Mannucci PM, Peyvandi F. TTP and ADAMTS13: when is testing appropriate? Hematology Am Soc Hematol Educ Program. 2007;1:121–126. doi: 10.1182/asheducation-2007.1.121. [DOI] [PubMed] [Google Scholar]
- 93.Booth KK, Terrell DR, Vesely SK, et al. Systemic infections mimicking thrombotic thrombocytopenic purpura. Am J Hematol. 2011;86:743–751. doi: 10.1002/ajh.22091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vesely SK, George JN, Lämmle B, et al. ADAMTS13 activity in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: relation to presenting features and clinical outcomes in a prospective cohort of 142 patients. Blood. 2003;102:60–68. doi: 10.1182/blood-2003-01-0193. [DOI] [PubMed] [Google Scholar]
- 95.Zheng XL, Kaufman RM, Goodnough LT, et al. Effect of plasma exchange on plasma ADAMTS13 metalloprotease activity, inhibitor level, and clinical outcome in patients with idiopathic and nonidiopathic thrombotic thrombocytopenic purpura. Blood. 2004;103:4043–4049. doi: 10.1182/blood-2003-11-4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mannucci PM, Franchini M. Advantages and limits of ADAMTS13 testing in the prognostic assessment of thrombotic thrombocytopenic purpura. Presse Med. 2012;41(3 Pt 2):e157–162. doi: 10.1016/j.lpm.2011.10.025. [DOI] [PubMed] [Google Scholar]
- 97.Peyvandi F, Lavoretano S, Palla R, et al. ADAMTS13 and anti-ADAMTS13 antibodies as markers for recurrence of acquired thrombotic thrombocytopenic purpura during remission. Haematologica. 2008;93:232–239. doi: 10.3324/haematol.11739. [DOI] [PubMed] [Google Scholar]
- 98.Jin M, Casper TC, Cataland SR, et al. Relationship between ADAMTS13 activity in clinical remission and the risk of TTP relapse. Br J Haematol. 2008;141:651–658. doi: 10.1111/j.1365-2141.2008.07107.x. [DOI] [PubMed] [Google Scholar]
- 99.Michael M, Elliott EJ, Craig JC, et al. Interventions for haemolytic uraemic syndrome and thrombotic thrombocytopenic purpura. Am?J Kidney Dis. 2009;53:259–272. doi: 10.1053/j.ajkd.2008.07.038. [DOI] [PubMed] [Google Scholar]
- 100.Noris M, Remuzzi G. Thrombotic microangiopathy: what not to learn from a meta-analysis. Nat Rev Nephrol. 2009;5:186–188. doi: 10.1038/nrneph.2009.28. [DOI] [PubMed] [Google Scholar]
- 101.Taylor CM, Machin S, Wigmore SJ, et al. Clinical practice guidelines for the management of atypical haemolytic uraemic syndrome in the United Kingdom. Br J Haematol. 2010;148:37–47. doi: 10.1111/j.1365-2141.2009.07916.x. [DOI] [PubMed] [Google Scholar]
- 102.Davin JC, Olie KH, Verlaak R, et al. Complement factor H-associated atypical hemolytic uremic syndrome in monozygotic twins: concordant presentation, discordant response to treatment. Am J Kidney Dis. 2006;47:e27–e30. doi: 10.1053/j.ajkd.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 103.Rock GA, Shumak KH, Buskard NA, et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian Apheresis Study Group. N Engl J Med. 1991;325:393–397. doi: 10.1056/NEJM199108083250604. [DOI] [PubMed] [Google Scholar]
- 104.Schulman I, Pierce M, Lukens A, et al. Studies on thrombopoiesis.?I.?A factor in normal human plasma required for platelet production; chronic thrombocytopenia due to its deficiency. Blood. 1960;16:943–957. [PubMed] [Google Scholar]
- 105.Szczepiorkowski ZM, Winters JL, Bandarenko N, et al. Guidelines on the use of therapeutic apheresis in clinical practice—evidence-based approach from the Apheresis Applications Committee of the American Society for Apheresis. J Clin Apher. 2010;25:83–177. doi: 10.1002/jca.20240. [DOI] [PubMed] [Google Scholar]
- 106.Bell WR, Braine HG, Ness PM, et al. Improved survival in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Clinical experience in 108 patients. N Engl J Med. 1991;325:398–403. doi: 10.1056/NEJM199108083250605. [DOI] [PubMed] [Google Scholar]
- 107.Clark WF, Hildebrand A. Attending rounds: microangiopathic hemolytic anemia with renal insufficiency. Clin J Am Soc Nephrol. 2012;7:342–347. doi: 10.2215/CJN.07230711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ruggenenti P, Remuzzi G. A German outbreak of haemolytic uraemic syndrome. Lancet. 2011;378:1057–1058. doi: 10.1016/S0140-6736(11)61217-8. [DOI] [PubMed] [Google Scholar]
- 109.Dundas S, Murphy J, Soutar RL, et al. Effectiveness of therapeutic plasma exchange in the 1996 Lanarkshire Escherichia coli O157: H7 outbreak. Lancet. 1999;354:1327–1330. doi: 10.1016/s0140-6736(99)01251-9. [DOI] [PubMed] [Google Scholar]
- 110.Colic E, Dieperink H, Titlestad K, et al. Management of an acute outbreak of diarrhoea-associated haemolytic uraemic syndrome with early plasma exchange in adults from southern Denmark: an observational study. Lancet. 2011;378:1089–1093. doi: 10.1016/S0140-6736(11)61145-8. [DOI] [PubMed] [Google Scholar]
- 111.Greinacher A, Friesecke S, Abel P, et al. Treatment of severe neurological deficits with IgG depletion through immunoadsorption in patients with Escherichia coli O104: H4-associated haemolytic uraemic syndrome: a prospective trial. Lancet. 2011;378:1166–1173. doi: 10.1016/S0140-6736(11)61253-1. [DOI] [PubMed] [Google Scholar]
- 112.Combe C, Bui HN, de Precigout V, et al. Immunoadsorption in patients with haemolytic uraemic syndrome. Lancet. 2012;379:517–518. doi: 10.1016/S0140-6736(12)60228-1. author reply 8–9. [DOI] [PubMed] [Google Scholar]
- 113.George JN. How I treat patients with thrombotic thrombocytopenic purpura: 2010. Blood. 2010;116:4060–4069. doi: 10.1182/blood-2010-07-271445. [DOI] [PubMed] [Google Scholar]
- 114.Loirat C, Saland J, Bitzan M. Management of hemolytic uremic syndrome. Presse Med. 2012;41(3 Pt 2):e115–135. doi: 10.1016/j.lpm.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 115.Goicoechea de Jorge E, Macor O, Paixão-Cavalcante D, et al. The development of atypical hemolytic uremic syndrome depends on complement C5. J Am Soc Nephrol. 2011;22:137–145. doi: 10.1681/ASN.2010050451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gruppo RA, Rother RP. Eculizumab for congenital atypical hemolytic-uremic syndrome. N Engl J Med. 2009;360:544–546. doi: 10.1056/NEJMc0809959. [DOI] [PubMed] [Google Scholar]
- 117.Prescott HC, Wu HM, Cataland SR, et al. Eculizumab therapy in an adult with plasma exchange-refractory atypical hemolytic uremic syndrome. Am J Hematol. 2010;85:976–977. doi: 10.1002/ajh.21862. [DOI] [PubMed] [Google Scholar]
- 118.Lapeyraque AL, Frémeaux-Bacchi V, Robitaille P. Efficacy of eculizumab in a patient with factor-H-associated atypical hemolytic uremic syndrome. Pediatr Nephrol. 2011;26:621–624. doi: 10.1007/s00467-010-1719-3. [DOI] [PubMed] [Google Scholar]
- 119.Tschumi S, Gugger M, Bucher BS, et al. Eculizumab in atypical hemolytic uremic syndrome: long-term clinical course and histological findings. Pediatr Nephrol. 2011;26:2085–2088. doi: 10.1007/s00467-011-1989-4. [DOI] [PubMed] [Google Scholar]
- 120.Ariceta G, Arrizabalaga B, Aguirre M, et al. Eculizumab in the treatment of atypical hemolytic uremic syndrome in infants. Am J Kidney Dis. 2012;59:707–710. doi: 10.1053/j.ajkd.2011.11.027. [DOI] [PubMed] [Google Scholar]
- 121.Dorresteijn EM, van de Kar NC, Cransberg K. Eculizumab as rescue therapy for atypical hemolytic uremic syndrome with normal platelet count. Pediatr Nephrol. 2012;27:1193–1195. doi: 10.1007/s00467-012-2130-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Legendre CM, Babu S, Furman RR, et al. Safety and efficacy of eculizumab in aHUS patients resistant to plasma therapy: interim analysis form a Phase II trial. 43rd Annual Meeting of the American Society of Nephrology; 2010. Abstracts: SA-FC406. [Google Scholar]
- 123.Muus P, Legendre CM, Douglas K, et al. Safety and efficacy of eculizumab in ahus patients on chronic plasma therapy: interim analysis of a Phase II trial. 43rd Annual Meeting of the American Society of Nephrology; 2010. Abstracts: F-PO1274. [Google Scholar]
- 124.Ohanian M, Cable C, Halka K. Reduced dose maintenance eculizumab in atypical hemolytic uremic syndrome (aHUS): an update on a previous case report. Clin Pharmacol. 2011;3:45–50. doi: 10.2147/CPAA.S23687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mache CJ, Acham-Roschitz B, Frémeaux-Bacchi V, et al. Complement inhibitor eculizumab in atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2009;4:1312–1316. doi: 10.2215/CJN.01090209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Köse O, Zimmerhackl LB, Jungraithmayr T, et al. New treatment options for atypical hemolytic uremic syndrome with the complement inhibitor eculizumab. Semin Thromb Hemost. 2010;36:669–672. doi: 10.1055/s-0030-1262889. [DOI] [PubMed] [Google Scholar]
- 127.Kelly R, Arnold L, Richards S, et al. The management of pregnancy in paroxysmal nocturnal haemoglobinuria on long term eculizumab. Br J Haematol. 2010;149:446–450. doi: 10.1111/j.1365-2141.2010.08099.x. [DOI] [PubMed] [Google Scholar]
- 128.Cataland SR, Yang S, Wu HM. The use of ADAMTS13 activity, platelet count, and serum creatinine to differentiate acquired thrombotic thrombocytopenic purpura from other thrombotic microangiopathies. Br J Haematol. 2012;157:501–503. doi: 10.1111/j.1365-2141.2012.09032.x. [DOI] [PubMed] [Google Scholar]
- 129.Sadler JE. Von Willebrand factor, ADAMTS13, and thrombotic thrombocytopenic purpura. Blood. 2008;112:11–18. doi: 10.1182/blood-2008-02-078170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Balduini CL, Gugliotta L, Luppi M, et al. High versus standard dose methylprednisolone in the acute phase of idiopathic thrombotic thrombocytopenic purpura: a randomized study. Ann Hematol. 2010;89:591–596. doi: 10.1007/s00277-009-0877-5. [DOI] [PubMed] [Google Scholar]
- 131.Froissart A, Buffet M, Veyradier A, et al. Efficacy and safety of first-line rituximab in severe, acquired thrombotic thrombocytopenic purpura with a suboptimal response to plasma exchange. Experience of the French Thrombotic Microangiopathies Reference Center. Crit Care Med. 2012;40:104–111. doi: 10.1097/CCM.0b013e31822e9d66. [DOI] [PubMed] [Google Scholar]
- 132.Fakhouri F, Vernant JP, Veyradier A, et al. Efficiency of curative and prophylactic treatment with rituximab in ADAMTS13-deficient thrombotic thrombocytopenic purpura: a study of 11 cases. Blood. 2005;106:1932–1937. doi: 10.1182/blood-2005-03-0848. [DOI] [PubMed] [Google Scholar]
- 133.Scully M, Cohen H, Cavenagh J, et al. Remission in acute refractory and relapsing thrombotic thrombocytopenic purpura following rituximab is associated with a reduction in IgG antibodies to ADAMTS-13. Br J Haematol. 2007;136:451–461. doi: 10.1111/j.1365-2141.2006.06448.x. [DOI] [PubMed] [Google Scholar]
- 134.Scully M, McDonald V, Cavenagh J, et al. A phase 2 study of the safety and efficacy of rituximab with plasma exchange in acute acquired thrombotic thrombocytopenic purpura. Blood. 2011;118:1746–1753. doi: 10.1182/blood-2011-03-341131. [DOI] [PubMed] [Google Scholar]
- 135.Boyer O, Balzamo E, Charbit M, et al. Pulse cyclophosphamide therapy and clinical remission in atypical hemolytic uremic syndrome with anti-complement factor H autoantibodies. Am J Kidney Dis. 2010;55:923–927. doi: 10.1053/j.ajkd.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 136.Kwon T, Dragon-Durey MA, Macher MA, et al. Successful pre-transplant management of a patient with anti-factor H autoantibodies-associated haemolytic uraemic syndrome. Nephrol Dial Transplant. 2008;23:2088–2090. doi: 10.1093/ndt/gfn063. [DOI] [PubMed] [Google Scholar]
- 137.Bresin E, Daina E, Noris M, et al. Outcome of renal transplantation in patients with non-Shiga toxin-associated hemolytic uremic syndrome: prognostic significance of genetic background. Clin J Am Soc Nephrol. 2006;1:88–99. doi: 10.2215/CJN.00050505. [DOI] [PubMed] [Google Scholar]
- 138.Zuber J, Le Quintrec M, Sberro-Soussan R, et al. New insights into postrenal transplant hemolytic uremic syndrome. Nat Rev Nephrol. 2010;7:23–35. doi: 10.1038/nrneph.2010.155. [DOI] [PubMed] [Google Scholar]
- 139.Frémeaux-Bacchi V, Arzouk N, Ferlicot S, et al. Recurrence of HUS due to CD46/MCP mutation after renal transplantation: a role for endothelial microchimerism. Am J Transplant. 2007;7:2047–2051. doi: 10.1111/j.1600-6143.2007.01888.x. [DOI] [PubMed] [Google Scholar]
- 140.Seitz B, Albano L, Vocila F, et al. Recurrence of hemolytic uremic syndrome after renal transplantation. Transplant Proc. 2007;39:2583–2585. doi: 10.1016/j.transproceed.2007.08.021. [DOI] [PubMed] [Google Scholar]
- 141.Cruzado JM, Rodríguez de Córdoba S, Melilli E, et al. Successful renal transplantation in a patient with atypical hemolytic uremic syndrome carrying mutations in both factor I and MCP. Am J Transplant. 2009;9:1477–1483. doi: 10.1111/j.1600-6143.2009.02647.x. [DOI] [PubMed] [Google Scholar]
- 142.Donne RL, Abbs I, Barany P, et al. Recurrence of hemolytic uremic syndrome after live related renal transplantation associated with subsequent de novo disease in the donor. Am J Kidney Dis. 2002;40:E22. doi: 10.1053/ajkd.2002.36938. [DOI] [PubMed] [Google Scholar]
- 143.Karthikeyan V, Parasuraman R, Shah V, et al. Outcome of plasma exchange therapy in thrombotic microangiopathy after renal transplantation. Am J Transplant. 2003;3:1289–1294. doi: 10.1046/j.1600-6143.2003.00222.x. [DOI] [PubMed] [Google Scholar]
- 144.Nürnberger J, Philipp T, Witzke O, et al. Eculizumab for atypical hemolytic–uremic syndrome. N Engl J Med. 2009;360:542–544. doi: 10.1056/NEJMc0808527. [DOI] [PubMed] [Google Scholar]
- 145.Larrea CF, Cofan F, Oppenheimer F, et al. Efficacy of eculizumab in the treatment of recurrent atypical hemolytic-uremic syndrome after renal transplantation. Transplantation. 2010;89:903–904. doi: 10.1097/TP.0b013e3181ccd80d. [DOI] [PubMed] [Google Scholar]
- 146.Davin JC, Gracchi V, Bouts A, et al. Maintenance of kidney function following treatment with eculizumab and discontinuation of plasma exchange after a third kidney transplant for atypical hemolytic uremic syndrome associated with a CFH mutation. Am J Kidney Dis. 2010;55:708–711. doi: 10.1053/j.ajkd.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 147.Chatelet V, Frémeaux-Bacchi V, Lobbedez T, et al. Safety and long-term efficacy of eculizumab in a renal transplant patient with recurrent atypical hemolytic-uremic syndrome. Am J Transplant. 2009;9:2644–2645. doi: 10.1111/j.1600-6143.2009.02817.x. [DOI] [PubMed] [Google Scholar]
- 148.Al-Akash SI, Almond PS, Savell VH, Jr., et al. Eculizumab induces long-term remission in recurrent post-transplant HUS associated with C3 gene mutation. Pediatr Nephrol. 2011;26:613–619. doi: 10.1007/s00467-010-1708-6. [DOI] [PubMed] [Google Scholar]
- 149.Wilson CH, Brown AL, White SA, et al. Successful treatment of de novo posttransplant thrombotic microangiopathy with eculizumab. Transplantation. 2011;92:e42–e43. doi: 10.1097/TP.0b013e318230c0bd. [DOI] [PubMed] [Google Scholar]
- 150.Davin JC, Strain L, Goodship TH. Plasma therapy in atypical haemolytic uremic syndrome: lessons from a family with a factor H mutation. Pediatr Nephrol. 2008;23:1517–1521. doi: 10.1007/s00467-008-0833-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Hirt-Minkowski P, Schaub S, Mayr M, et al. Haemolytic uraemic syndrome caused by factor H mutation: is single kidney transplantation under intensive plasmatherapy an option? Nephrol Dial Transplant. 2009;24:3548–3551. doi: 10.1093/ndt/gfp377. [DOI] [PubMed] [Google Scholar]
- 152.Rosales A, Riedl M, Zimmerhackl LB. Thrombotic microangiopathy: atypical HUS: current diagnostic and therapeutic approaches. Nat Rev Nephrol. 2010;6:504–506. doi: 10.1038/nrneph.2010.98. [DOI] [PubMed] [Google Scholar]
- 153.Albertazzi V, Bonucchi D, De Amicis S, et al. A favorable 3-year outcome of kidney transplantation in atypical hemolytic uremic syndrome associated with a factor H mutation: case report. Transplant Proc. 2010;42:1352–1354. doi: 10.1016/j.transproceed.2010.03.048. [DOI] [PubMed] [Google Scholar]
- 154.Zimmerhackl LB, Hofer J, Cortina G, et al. Prophylactic eculizumab after renal transplantation in atypical hemolytic-uremic syndrome. N Engl J Med. 2010;362:1746–1748. doi: 10.1056/NEJMc1001060. [DOI] [PubMed] [Google Scholar]
- 155.Nester C, Stewart Z, Myers D, et al. Pre-emptive eculizumab and plasmapheresis for renal transplant in atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2011;6:1488–1494. doi: 10.2215/CJN.10181110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Weitz M, Amon O, Bassler D, et al. Prophylactic eculizumab prior to kidney transplantation for atypical hemolytic uremic syndrome. Pediatr Nephrol. 2011;26:1325–1329. doi: 10.1007/s00467-011-1879-9. [DOI] [PubMed] [Google Scholar]
- 157.Zlamy M, Hofer J, Elias J, et al. Immunogenicity of meningococcus C vaccination in a patient with atypical hemolytic uremic ?syndrome (aHUS) on eculizumab therapy. Pediatr Transplant. 2011 doi: 10.1111/j.1399-3046.2011.01585.x. [DOI] [PubMed] [Google Scholar]
- 158.Le Quintrec M, Zuber J, Noël LH, et al. Anti-Factor H autoantibodies in a fifth renal transplant recipient with atypical hemolytic and uremic syndrome. Am J Transplant. 2009;9:1223–1229. doi: 10.1111/j.1600-6143.2009.02586.x. [DOI] [PubMed] [Google Scholar]
- 159.Waters AM, Pappworth I, Marchbank K, et al. Successful renal transplantation in factor H autoantibody associated HUS with CFHR1 and 3 deficiency and CFH variant G2850T. Am J Transplant. 2010;10:168–172. doi: 10.1111/j.1600-6143.2009.02870.x. [DOI] [PubMed] [Google Scholar]
- 160.Waters AM, Licht C. aHUS caused by complement dysregulation: new therapies on the horizon. Pediatr Nephrol. 2011;26:41–57. doi: 10.1007/s00467-010-1556-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Remuzzi G, Ruggenenti P, Codazzi D, et al. Combined kidney and liver transplantation for familial haemolytic uraemic syndrome. Lancet. 2002;359:1671–1672. doi: 10.1016/S0140-6736(02)08560-4. [DOI] [PubMed] [Google Scholar]
- 162.Remuzzi G, Ruggenenti P, Colledan M, et al. Hemolytic uremic syndrome: a fatal outcome after kidney and liver transplantation performed to correct factor h gene mutation. Am J Transplant. 2005;5:1146–1150. doi: 10.1111/j.1600-6143.2005.00783.x. [DOI] [PubMed] [Google Scholar]
- 163.Cheong HI, Lee BS, Kang HG, et al. Attempted treatment of factor H deficiency by liver transplantation. Pediatr Nephrol. 2004;19:454–458. doi: 10.1007/s00467-003-1371-2. [DOI] [PubMed] [Google Scholar]
- 164.Wilson C, Torpey N, Jaques B, et al. Successful simultaneous liver-kidney transplant in an adult with atypical hemolytic uremic ?syndrome associated with a mutation in complement factor H. Am J Kidney Dis. 2011;58:109–112. doi: 10.1053/j.ajkd.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 165.Jalanko H, Peltonen S, Koskinen A, et al. Successful liver-kidney transplantation in two children with aHUS caused by a mutation in complement factor H. Am J Transplant. 2008;8:216–221. doi: 10.1111/j.1600-6143.2007.02029.x. [DOI] [PubMed] [Google Scholar]
- 166.Saland JM, Shneider BL, Bromberg JS, et al. Successful split liver-kidney transplant for factor H associated hemolytic uremic syndrome. Clin J Am Soc Nephrol. 2009;4:201–206. doi: 10.2215/CJN.02170508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Sánchez-Corral P, Melgosa M. Advances in understanding the aetiology of atypical haemolytic uraemic syndrome. Br J Haematol. 2010;150:529–542. doi: 10.1111/j.1365-2141.2010.08295.x. [DOI] [PubMed] [Google Scholar]
- 168.Noris M, Remuzzi G. Thrombotic microangiopathy after kidney transplantation. Am J Transplant. 2010;10:1517–1523. doi: 10.1111/j.1600-6143.2010.03156.x. [DOI] [PubMed] [Google Scholar]
- 169.Saland JM, Ruggenenti P, Remuzzi G. Liver–kidney transplantation to cure atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2009;20:940–949. doi: 10.1681/ASN.2008080906. [DOI] [PubMed] [Google Scholar]
- 170.Haller W, Milford DV, Goodship TH, et al. Successful isolated liver transplantation in a child with atypical hemolytic uremic syndrome and a mutation in complement factor H. Am J Transplant. 2010;10:2142–2147. doi: 10.1111/j.1600-6143.2010.03228.x. [DOI] [PubMed] [Google Scholar]
- 171.Goicoechea de Jorge E, Martínez-Barricarte R, Tortajada A, et al. The Spanish atypical haemolytic uraemic syndrome registry: a genetic update. Mol Immunol. 2007;44:3923. [Google Scholar]
- 172.Dragon-Durey MA, Blanc C, Marliot F, et al. The high frequency of complement factor H related CFHR1 gene deletion is restricted to specific subgroups of patients with atypical haemolytic uraemic syndrome. J Med Genet. 2009;46:447–450. doi: 10.1136/jmg.2008.064766. [DOI] [PubMed] [Google Scholar]
- 173.Westra D, Volokhina E, van der Heijden E, et al. Genetic disorders in complement (regulating) genes in patients with atypical haemolytic uraemic syndrome (aHUS) Nephrol Dial Transplant. 2010;25:2195–2202. doi: 10.1093/ndt/gfq010. [DOI] [PubMed] [Google Scholar]
- 174.Maga TK, Nishimura CJ, Weaver AE, et al. Mutations in alternative pathway complement proteins in American patients with atypical hemolytic uremic syndrome. Hum Mutat. 2010;31:E1445–E1460. doi: 10.1002/humu.21256. [DOI] [PubMed] [Google Scholar]


