Abstract
Purpose
Appendicitis is the most common condition leading to an intra-abdominal operation for a non-obstetric problem in pregnancy. The aim of this study was to examine our experience and to analyze the clinical characteristics and the pregnancy outcomes for appendicitis during pregnancy that was reported in Korea.
Methods
We reported 25 cases of appendicitis during pregnancy that were treated at Good Moonhwa Hospital from January 2004 to March 2010. We also analyzed appendicitis during pregnancy reported in Korea between 1970 and 2008 by a review of journals.
Results
The incidence of acute appendicitis during pregnancy was one per 568 deliveries. The mean age was 27.92 years old, the gestational stage at the onset of symptoms was the first trimester in 10 patients (40%), the second trimester in 14 patients (56%), and the third trimester in 1 patient (4%). Among the 25 cases, 21 were treated with an open appendectomy and 4 with laparoscopic appendectomies. The postoperative complications were 2 wound infections and 1 spontaneous abortion.
Conclusion
Our experience demonstrated that appendectomies on pregnant patients can be successfully performed at secondary hospitals.
Keywords: Appendicitis, Pregnancy, Postoperative complications
INTRODUCTION
Appendicitis is one of the most common conditions requiring laparotomy during pregnancy for a non-obstetric disease and is known to occur once in every 1,500 pregnant women [1]. Because the position of the appendix changes with gestational age and because the physiologic symptoms and signs of pregnancy are varied, the diagnosis of appendicitis during pregnancy is difficult, and delayed diagnosis and treatment results in increased risk of developing a perforation, which can cause harm to mother and fetus. In order to prevent these risks, early diagnosis and early treatment are essential. Most of the Korean literature on appendicitis during pregnancy has been reported by tertiary hospitals such as university hospitals. Thus, we now report, with a literature review, 25 cases of appendicitis during pregnancy treated in our secondary hospitals. Through this report, we will prove that surgery for appendicitis during pregnancy is possible in secondary hospitals with excellent results, and we will reconfirm useful diagnostic knowledge and surgical techniques, as well as provide a literature review, in order to identify possible future developments.
METHODS
A total of 25 pregnant women who underwent an appendectomy by 2 surgeons and who were histologically-confirmed as having appendicitis in Good Moonhwa Hospital between January 2004 and March 2010 were selected for a retrospective study conducted through medical record review and telephone interviews. Korean journals published by academic societies were screened through an internet search: 425 cases of appendicitis during pregnancy were reported in 14 articles published from 1970 to 2008. For the literature review, patient information, including age, number of deliveries, gestational age, time elapsed from onset of symptoms to surgery, clinical manifestations and physical findings, body temperature, number of blood leukocytes, neutrophil ratio, position of the appendix during surgery, hospitalization period, histopathological findings, postoperative complications and postpartum course, was analyzed and categorized. Gestational age was divided into 3 terms: 0 to 14th week (first trimester of pregnancy), 15th to 28th week (second trimester) and 29th week and later (third trimester).
RESULTS
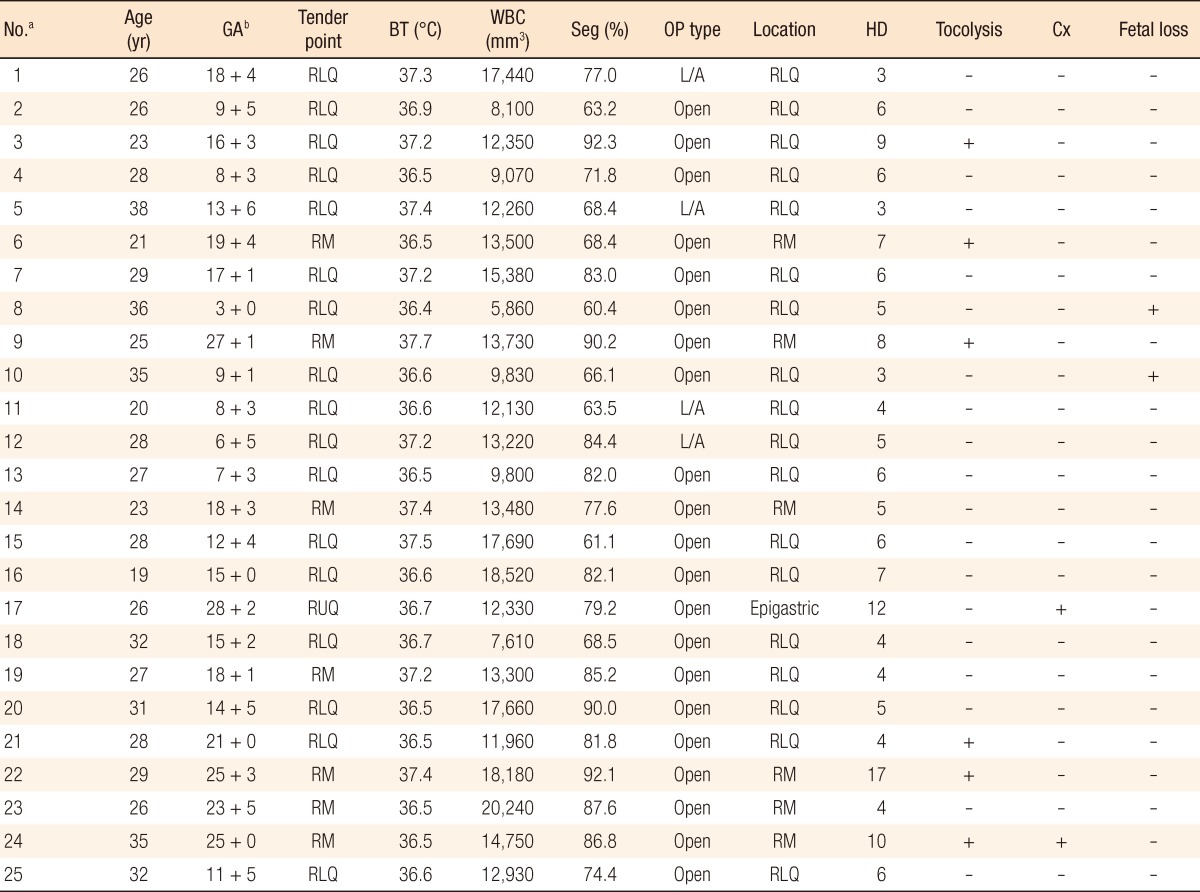
A total of 25 patients underwent surgeries after having been diagnosed with acute appendicitis. The total number of deliveries was 14,203 during the study period. Acute appendicitis affected 1 in every 568 deliveries (Table 1). The mean age of the patients was 27.92 years (range, 19 to 38 years), and 1 patient was younger than 20 (4%); the ages of 4 patients were between 20 and 24 (16%), 13 patients were between 25 and 29 (52%), 3 patients were between 30 and 34 (12%), and 4 patients were 35 or older (16%). The number of primipara was 12 (48%), and that of multipara was 13 (52%). By gestational age, 10 patients were in the first trimester of pregnancy (40%), 14 were in the second trimester of pregnancy (56%), and 1 was in the third trimester of pregnancy (4%). Seventeen patients underwent surgery within 24 hours of the onset of symptoms (68%), 4 patients within 48 hours (16%), and 4 patients after 48 hours or later (16%).
Table 1.
Clinical features of 25 pregnant women with an appendectomy
GA, gestational age; BT, body temperature; WBC, white blood cell; Seg, segmented neutrophil; OP, operation; HD, postoperative hospital day; Cx, complication; RLQ, right lower quadrant; RM, right mid-abdomen; RUQ, right upper quadrant; L/A: laparoscopic appendectomy.
aPatient case number. bFor example, "18 + 4" means that GA is 18 weeks and 4 days.
Abdominal pain was reported in all cases. Nausea was reported in 16 cases (64%), and vomiting in 9 cases (36%). In terms of axillary temperature, 19 patients were below 37.3℃ (76%), and 6 patients were 37.3℃ or over (24%). Tenderness and rebound tenderness were reported in all cases. In terms of the location of the maximal tender point, in 17 cases it was observed at McBurney's point (68%), in 7 cases in the right umbilical area (28%), and in 1 case in the right upper abdominal area (4%). Regarding the number of leukocytes, 6 cases (24%) showed less than 10,000 mm3, 12 cases (48%) 10,000 to 15,000 mm3, 6 cases (24%) 15,000 to 20,000 mm3, and 1 case (4%) 20,000 mm3 or more. In terms of neutrophil ratio, 8 cases (32%) showed less than 70%, and 17 cases (68%) showed 70% or more.
For diagnosing appendicitis, ultrasonography was used in all cases. General anesthesia was administered in all cases. A laparotomy was performed in 21 cases (84%) while laparoscopic surgery was performed in 4 cases (16%). Out of the 21 patients who underwent a laparotomy, a McBurney's incision was conducted on 10 patients while a transverse incision was performed on 11 patients. The appendix was positioned in the right lower area of the abdomen in 18 cases, in the right umbilical area in 6 cases, and in the right upper area in 1 case. Histopathological findings showed that 24 cases (96%) were suppurative, and one case (4%) was gangrenous. No maternal death was reported. In the laparotomy group, two cases of wound infection were reported, but no complications were observed in the laparoscopy group. The hospital stay ranged from 3 days to 17 days, with a mean hospital stay of 6.2 days. The mean hospital stay of the laparoscopy group was 3.8 days while that of the laparotomy group was 6.7 days.
Postoperative tocolytic agent was administered to six patients in the laparotomy group while no patients in laparoscopy group were administered the agent. At postoperative two weeks, one spontaneous abortion was reported. Upon request from one patient who was a multipara with three children and was not aware of her pregnancy until a preoperative pregnancy test was conducted, an artificial abortion was performed. Among 23 mothers available for follow-up, no pre-term labor was observed, and a mean of 38 weeks and 4 days passed to delivery.
DISCUSSION
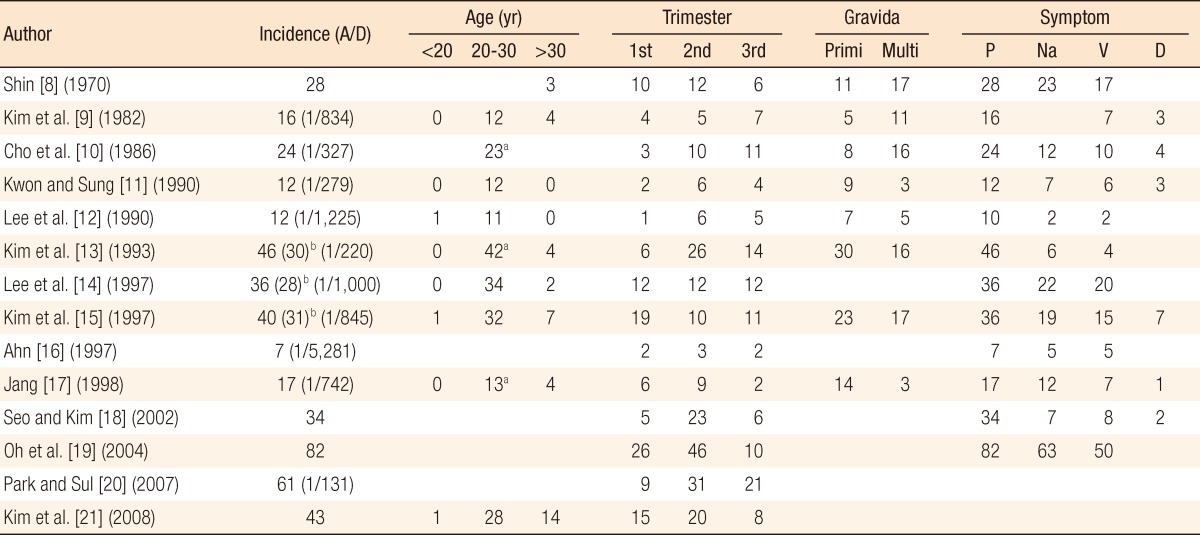
The incidence rate of appendicitis during pregnancy has been reported to range from 1 per 1,000 deliveries to 1 per 5,533 deliveries [1-7]. According to Babaknia et al. [1] who analyzed more than 500,000 deliveries, the rate is 1 to 1,500 deliveries. Overall, the incidence rate is known to be 0.05 to 0.2%. In Korea, 10 studies have reported incidence rates ranging from 1 to 131 deliveries to 1 to 5,281 deliveries, with a mean of 1 to 665 deliveries (246 appendicitis cases in 163,708 deliveries) (Tables 2-4) [8-21]. Including our study results, the mean rate in Korea is 1 to 656 deliveries (271 appendicitis cases in 177,911 deliveries), which is higher than that of Babaknia et al. [1]. It is evident that the incidence rate is at least 1 to 1,000 deliveries.
Table 2.
Literature review of published data for appendicitis during pregnancy in Korea (I)
Blank means no data from reference.
A/D, appendectomy patients/delivery women count; Primi, primigravida; Multi, multigravida; P, abdominal pain; Na, nausea; V, vomiting; D, diarrhea.
aCriteria: 20 to 29. bPreoperative data included negative appendectomies. The numbers in parentheses refer to pathologically-confirmed appendicitis.
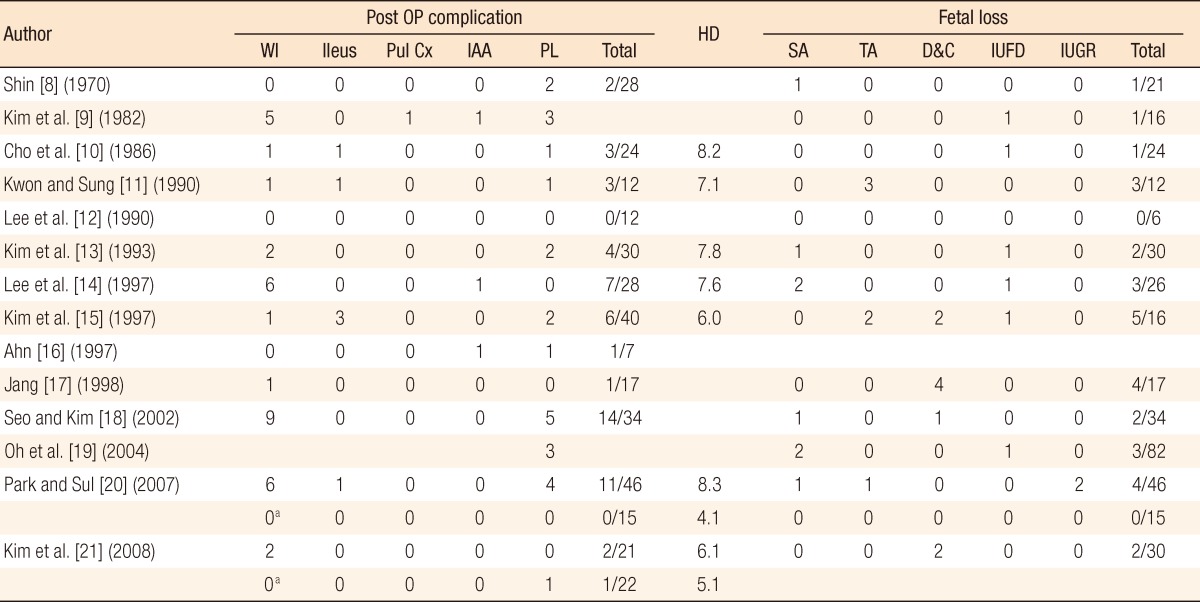
Table 4.
Literature review of published data for appendicitis during pregnancy in Korea (III)
OP, operation; WI, wound infection; Pul Cx, pulmonary complication; IAA, intra-abdominal abscess; PL, preterm labor; HD, hospital day; SA, spontaneous abortion; TA, threatened abortion; D&C, dilatation and curettage; IUFD, intra-uterine fetal death; IUGR, intra-uterine growth retardation.
aThe pregnant women underwent a laparoscopic appendectomy.
In terms of age, most of the literature reports the highest incidence rate in the 20 to 30 age group, with some differences according to classification criteria. In our study, 17 patients (68%) were in the 20 to 29 age group, which formed the largest portion, followed by 7 patients (28%) in their 30s or older. According to the study of Kim et al. [21], the 20 to 30 age group showed the largest share with 28 patients (65.1%), followed by 14 patients (32.6%) in their 30s or older, which is a comparatively high ratio. This is thought to be due to late marriage, which is expected to increase further in the future as a part of the social phenomenon in Korea these days. In summary, appendicitis during pregnancy shows the highest incidence for women in their 20's [14, 21], but the rate is also very high for women in their 30's in accordance with increasing number of pregnancies among older women [21].
Acute appendicitis can develop at any time during pregnancy. According to Gomez and Wood [2], Babaknia et al. [1], Popkin et al. [7] and Korean literature, it occurs in the second trimester of pregnancy most often, and these results correspond to that of the present study [8, 11-13, 16-21]. Kim et al. [15] reported that the highest incidence rate was shown during the first trimester of pregnancy while Kim et al. [9] and Cho et al. [10] reported the third trimester of pregnancy as having the highest rate. In the case of Lee et al. [14], no difference was reported among trimesters (Table 2).
Making a diagnosis of appendicitis during pregnancy simply with history taking and physical exams is difficult due to physiologic factors such as the various symptoms appearing during normal pregnancy (anorexia, nausea, and vomiting) and to other factors including changes in the position of the appendix in accordance with uterine enlargement and relaxation in abdominal muscles. Moreover, restriction in the use of radiologic methods due to the fetus may delay making a diagnosis. Delay in diagnosis results in delay in treatment, which can cause perforation, increasing the death rate for the fetus and the mother, and the development of serious complications. In general, a point system including clinical manifestations, physical findings and blood tests is used for the diagnosis of appendicitis, and ultrasonography or computed tomography (CT) is additionally conducted. The Alvarado score is the most frequently used point system and gives scores such as 1 mark to migrating pain, 1 mark to loss of appetite, 1 mark to nausea or vomiting, 2 marks to tenderness in the right lower abdominal area, 1 mark to rebound tenderness, 1 mark to fever, 2 marks to leukocytosis, and 1 mark to an increase in the number of neutrophils, comprising 10 marks in total. According to Oh et al. [22], an Alvarado score of 7 or more marks may be most appropriate to evaluate appendicitis as positive in cases of adults. However, pregnant women show nausea, vomiting, pyrexia and increased number of leukocytes and neutrophils as physiologic clinical findings; accordingly, the point system is not ideal for diagnosis. According to the study of Brown et al. [23] on clinical manifestations and physical findings of 7 reports and 450 patients, 345 patients (76.7%) showed nausea, 228 patients (50.7%) showed vomiting, 295 patients (65.6%) showed pyrexia, 450 patients (100%) showed right lower abdominal pain, 412 patients (91.6%) showed right upper abdominal pain, 327 patients (72.7%) showed peritoneal irritation, and 309 patients (68.7%) showed uterine contraction. They obtained positive and negative predictive values and odds ratio, but they reported that there was no useful clinical indicator for predicting appendicitis during pregnancy. According to the Korean literature, abdominal pain was reported in almost all cases, but nausea was reported in 13 to 82.1% of the total cases, vomiting in 8.7 to 71.4%, pyrexia in 3.6 to 50%, and right lower abdominal tenderness in 26.7 to 100% [8-21]. In our study, abdominal pain was reported in all cases, nausea in 16 patients (64%), vomiting in 9 patients (36%), pyrexia in 6 patients (24%), and right lower abdominal tenderness in 17 patients (68%) (Table 2).
The appendix is positioned in the right lower abdominal area at the early stage of pregnancy, but transpositions to the right umbilical area or the right upper abdominal area with the progression of pregnancy due to uterine enlargement; consequently, the area of pain also changes. Some recent studies reported developments of right lower abdominal pain caused by appendicitis during pregnancy regardless of gestational age. Even though right lower abdominal pain is very common in pregnant women without appendicitis, right lower abdominal pain is thought to be the most reliable finding of appendicitis during pregnancy. It is sometimes difficult to confirm tenderness in patients with appendicitis during pregnancy because the appendix is transpositioned due to uterine enlargement, the peritoneal wall is apart from the appendix, and symptoms of stimulating the peritoneum are reduced due to relaxation in muscles. According to some reports, the Rovsing sign and the Psoas sign were not found in 2/3 of pregnant women. The Alder's sign is known to be useful, but a study reported it not to be helpful [23]. Abdominal pain developed in all cases without exception; accordingly, abdominal pain is the only definite clinical indicator for appendicitis during the pregnancy.
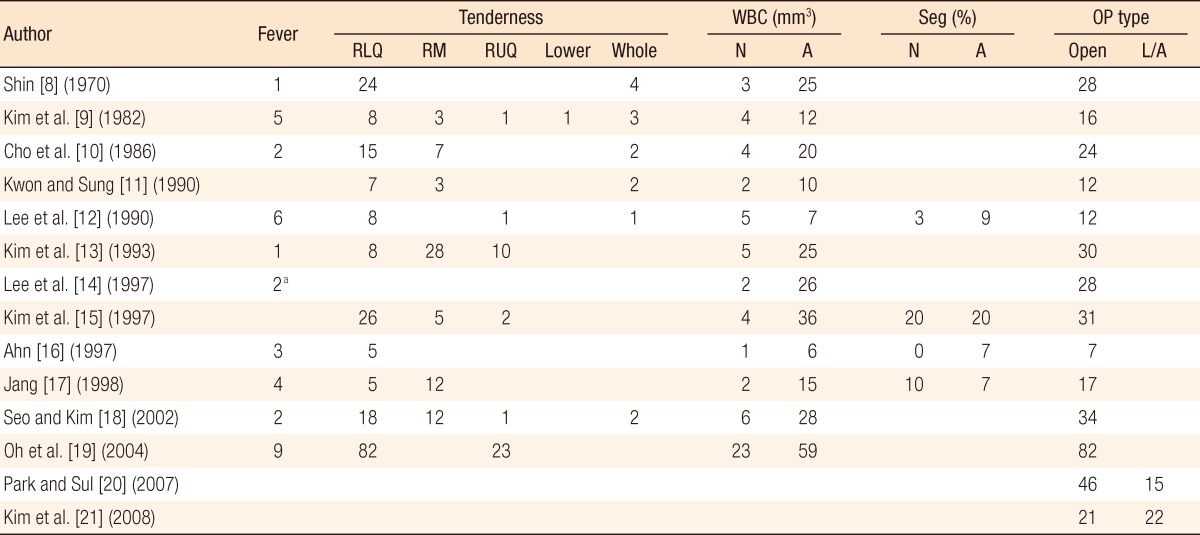
Close attention should be paid to the interpretation of diagnostic test results for appendicitis during pregnancy. In a normal pregnancy, the number of leukocytes increases up to 12,000 mm3, and during delivery, the number increases up to 18,000 to 30,000 mm3. According to Hee and Viktrup [5] to Seo and Kim [18], the number of leukocytes in appendicitis patients during pregnancy significantly increased compared with pregnant women with a normal appendix. Kim et al. [21] reported that perforated appendicitis is suspected for leukocytes levels of 16,000 mm3 or more. However, according to other Korean studies, normal leukocyte and neutrophil levels were found in 7.1 to 41.7% and 0 to 58.8% of pregnant women with appendicitis, respectively. Therefore, patients with normal levels of leukocytes and neutrophils cannot be free from the suspicion of appendicitis (Table 3). In our case, 7 patients (28%) had a normal number of leukocytes and 8 (32%) had a normal range of neutrophils when the normal value of leukocytes was set as 12,000 mm3. Six patients (24%) showed leukocyte levels at 16,000 mm3 or over, and one of them was diagnosed with gangrenous appendicitis while the remaining patients were diagnosed with suppurative appendicitis. Therefore, interpretations of the levels of leukocytes and neutrophils in patients who are suspected with appendicitis during pregnancy should be made carefully because as mentioned above, no increase in the levels does not necessarily mean no appendicitis and increases in the levels does not necessarily mean appendicitis. Increases in the levels of neutrophils accompanied by the prodromal symptom of appendicitis may help with the diagnosis of appendicitis, and if the level of leukocytes is very high, the possibility of a perforation should be considered, and an urgent operation should be performed.
Table 3.
Literature review of published data for appendicitis during pregnancy in Korea (II)
Blank means no data from reference.
RLQ, right lower quadrant; RM, right mid-abdomen; RUQ, right upper quadrant; WBC, white blood cell; N, normal; A, abnormal; Seg, segmented neutrophil; OP, operation; L/A, laparoscopic appendectomy.
aAbove 38℃.
In articles on surgery for appendicitis during pregnancy, the negative appendectomy rate varied from 15 to 50%. The ratio was 15 to 35% when general surgeons performed the surgery while the ratio was 25 to 50% when a gynecologist performed the surgery [23, 24]. According to Korean literature, the ratio was in the range of 15 to 36.4% [8, 13-17]. Radiologic examination is necessary in order to reduce the negative appendectomy rate, but due to radiation hazards to the fetus, ultrasonography is frequently used instead. According to Lim et al. [25], tests were conducted for 45 pregnant women suspected of having appendicitis, but 3 patients in the third trimester of pregnancy were not diagnosed while the remaining 42 patients were diagnosed. Out of the 42 diagnosed patients, 16 patients were diagnosed with appendicitis while the remaining 26 were confirmed to have normal appendices, with 100% sensitivity, 96% specificity and 98% accuracy. Zhang et al. [26] reported that out of 65 patients, 26 patients (40%) were diagnosed using ultrasonography. Due to multilateral results of ultrasonography [27], studies on diagnoses using CT or magnetic resonance imaging are in progress these days. According to Freeland et al. [24], ultrasonography was conducted on 43 pregnant women, but only 5 patients (11.6%) were diagnosed with appendicitis, and definitive diagnosis as appendicitis was made through histopathologic examinations. The remaining 38 patients (88.4%) were not detected by ultrasonography, and 9 patients (23.7%) out of the undetected 38 were diagnosed with appendicitis through histopathologic examinations. CT was conducted on 13 patients who were not diagnosed with appendicitis through ultrasonography. In order to avoid the risk of a deformity developing in the fetus, the radiation dose was kept below the threshold of 0.05 to 0.15 Gy: at the first trimester of pregnancy, 0.024 Gy (2.4 rad), and at the third trimester of pregnancy, 0.046 Gy (4.6 rad). Regarding the onset of cancer in infants, exposure to 5 rad results in a probability of 1/2,000 to 1/1,000, but this was not experienced, but follow-up was required. Freeland et al. [24] suggested an algorithm on diagnostic imaging for patients with appendicitis during pregnancy, but the safest diagnostic imaging method known to now is ultrasonography. We performed ultrasonography for this study, and we used the outcomes as criteria for preoperative diagnostic imaging.
When the diagnosis is made with appendicitis, immediate surgery can reduce the risk to the mother and the fetus. Surgery can be either a traditional open appendectomy or a laparoscopic appendectomy, which was recently introduced. Prior to 1990, a laparotomy was preferred because laparoscopic surgery was understood as a contraindication of pregnancy. However, laparoscopic surgery was performed for adnexal torsion and ovarian cysts during pregnancy by obstetricians at the end of the 1980s, and surgeons performed laparoscopic cholecystectomies and appendectomies. As a result, the outcome of laparoscopic surgery was confirmed to be not worse than that of a laparotomy in terms of safety; consequently, laparoscopic surgery has also been performed quite often recently for appendicitis during pregnancy. In the study through literature screening, Nezhat et al. [27] analyzed 93 patients who underwent laparoscopic surgery during pregnancy and confirmed that laparoscopic surgery during pregnancy was not dangerous. They also analyzed the types of risks that might be involved in laparoscopic surgery during pregnancy. The first risk is the risk of uterine damage due to the trocar caused by uterine enlargement with increased gestational age or to insertion of the Veress needle. In order to prevent this risk, Nezhat et al. [27] suggested an open technique using Hasson cannula. The second risk is the risk of acid-base imbalance, which can occur due to the CO2 gas used during laparoscopic surgery and the risk of fetal acidosis due to hypercarbia. In order to minimize the risk of developing hypercarbia and acidosis, the intra-abdominal pressure should be kept at 20 mmHg or below, and the operation time should be shortened. The preferred times for laparoscopic surgery during pregnancy are known to be in the first and the second trimesters of pregnancy, with the third trimester of pregnancy being understood to be contraindicated. However, cases of laparoscopic surgery in the third trimester of pregnancy have been reported recently. A journal screening on laparoscopic surgeries performed for appendicitis during pregnancy showed that Machado and Grant [28] suggested restricting the intra-abdominal pressure to 10 to 12 mmHg and the operative time within 60 minutes for good outcomes in the fetus and the mother. However, long-term follow-up on children after delivery was not conducted. According to their only one report on 11 children who were born after a laparoscopic appendectomy during pregnancy, no growth or developmental retardation was found in a postoperative 1- to 8-year follow-up. In addition, out of 637 patients who underwent a laparoscopic appendectomy, 155 patients had records on gestational age, and 26 patients were in the third trimester of pregnancy. According to the study, performing laparoscopic surgery in the third trimester of pregnancy makes it difficult both to secure a clear view due to uterine enlargement and to do instrumentation. Therefore, laparoscopic surgery should be performed by experienced surgeons. In a study on 61 patients with appendicitis during pregnancy, Park and Sul [20] compared 46 patients who underwent an open appendectomy to 15 patients who underwent a laparoscopic appendectomy. According to the study, the mean hospital stay of the laparotomy group was 8.3 days while that of the laparoscopy group was 4.1 days, showing a statistically significant difference. In terms of postoperative complications, the laparotomy group reported 6 cases of wound infection, 1 case of intestinal ileus, 1 case of abortion, and 4 cases of pre-term delivery while the laparoscopy group did not report any complications. In a study on 43 patients with appendicitis during pregnancy, Kim et al. [21] compared 21 patients of the laparotomy group with 22 patients of the laparoscopy group. The mean hospital stay of the laparotomy group was 6.7 days while that of the laparoscopy group was 5.1 days, showing a statistically significant difference. In terms of postoperative complications, the laparotomy group reported 2 cases of wound infection. According to the present study, laparoscopic surgery was performed on 4 patients since December 2009. The sample size of the laparoscopy group was too small to compare it with laparotomy group, but the laparoscopy group showed a shorter hospital stay than the laparotomy group, and no complications such as wound infections, abortions, or pre-term deliveries were observed. In the present study, patients in whom the gestational age of the fetus was less than 20 weeks underwent laparoscopic surgery because patients in whom the gestational age of the fetus was 20 weeks or more were not recommended to undergo due to the fear of uterine damage caused by uterine enlargement and due to the difficulty securing a clear view. In addition, because our hospital was under the bundle of services system, health insurance claims for laparoscopic surgery have been available since July 2009; accordingly, the first laparoscopic surgery was performed in December 2009. Even though laparoscopic surgery for appendicitis during pregnancy can reduce wound infection and can contribute to quick recovery by virtue of decreased pain level, which reduces development of postoperative ileus, and diagnosis and treatment can be conducted simultaneously, it has been contraindicated based on studies reporting increased fetal death rate as a result of laparoscopic surgery. However, according to recent studies on laparoscopic surgery during pregnancy, the fetal death rate in laparoscopic surgery is rather lower than or similar to that of a laparotomy. Park and Sul [20], Kim et al. [21], Nezhat et al. [27] and Machado and Grant [28] reported fetal death rates lower than 1%. In the present study, four cases of laparoscopic surgery were performed, and no abortions, stillbirths or pre-term labor were reported. Based on the above results, if the intra-abdominal pressure and the operation time can be properly controlled, avoiding uterine damage through the open technique, laparoscopic surgery can be used for appendicitis during pregnancy; moreover, it is advantageous in terms of mean hospital stay and postoperative complications. However, the laparoscopic appendectomy is to be established as a standard treatment for appendicitis during pregnancy, a long-term follow-up on children born after the surgery is necessary. When no cases of growth or developmental retardation are found during a long-term follow-up of over 10 years or more, laparoscopic surgery may significantly replace the conventional laparotomy for the treatment of appendicitis during pregnancy.
Appendicitis during pregnancy has risks to the mother or the fetus even after the surgery. The postoperative complications can be classified for the mother and the fetus. In terms of mother-side complications, the maternal death rate was 24% in early studies, but recently, no maternal deaths have been reported by virtue of performing early operations, development of antibiotics, and developments in anesthetic and surgical techniques. Complications other than maternal death include wound infection, postoperative ileus, intestinal obstruction, respiratory complications, intra-abdominal abscess and pre-term labor. Among the 315 patients who were confirmed to have complications in the open appendectomy group in Korea, 34 patients (10.8%) had wound infections, 6 patients (1.9%) had postoperative ileus, 1 patient (0.3%) had respiratory complications, 3 patients (1%) had intra-abdominal abscesses, and 22 patients (7%) had pre-term labor (Table 4). In our study, out of the 21 patients in the open appendectomy group, only 2 cases (9.5%) of wound infections were reported, and no other complications were found. According to Lee et al. [14], a 16.7% wound-infection development rate was reported in pregnant women, and once perforation occurred, wound infections developed in all perforation cases. According to Seo and Kim [18], the wound-infection development ratio in non-pregnant women was 14.7%, and in pregnant women, the ratio was 26.5%, showing more wound infections in pregnant women. The reasons for the higher wound-infection development rate in pregnant women may be delay in diagnosis and subsequent delay in surgery, and an increase in development of perforation. Yilmaz et al. [29] reported that the incidence rate of perforated appendicitis during pregnancy was 40% and that the rate was associated with the time from the onset of symptoms to surgery. The risk of developing perforation is high when the time from the onset of symptoms to surgery exceeds 20 hours. According to Yilmaz et al. [29], an increase in gestational age is not associated with perforation, which is different from other study results. In addition, Yilmaz et al. [29] reported that the increase in pre-term labor is affected by increases in perforation and gestational age. Zhang et al. [26] reported a 1.6% pre-term labor rate in cases of non-perforated appendicitis, but a 25% pre-term labor rate was observed in cases of perforated appendicitis.
Complications for the fetus include abortion, stillbirth, congenital anomaly, and intrauterine growth retardation. In early studies, the fetal death rate was reported at 40 to 50%, but the rate has decreased by virtue of early operations and developments in antibiotics, anesthetic and surgical techniques, fetal monitoring systems, and neonatal intensive care. Recently, the fetal death rate in noncomplicated appendicitis has been reported at 1.5 to 4%, but in cases of perforated appendicitis, the rate is still high at 21 to 35% [23]. Zhang et al. [26] reported a 1.6% fetal death rate in cases of non-perforated appendicitis, but the rate increased to 25% in cases of perforated appendicitis. Mazze and Kallen [30] reported that out of 778 infants, 41 infants (5.3%) were observed to have congenital deformations. In the case of Korea, out of 375 identified patients, there were 8 cases (2.1%) of spontaneous abortion, 6 cases (1.6%) of threatened abortion, 9 cases (2.4%) of artificial abortion, 7 cases (1.9%) of stillbirth, and 2 cases (0.5%) of intrauterine growth retardation (Table 4). In the present study, 1 case (4%) of spontaneous abortion and 1 case (4%) of artificial abortion were observed. Based on these results, since the probability of complications in appendicitis during the pregnancy will be higher in cases of perforated appendicitis, early urgent surgery is essential.
In conclusion, reports on appendicitis during pregnancy have mostly been reported by university hospitals or tertiary hospitals in Korea. In the present study, 25 surgery cases of appendicitis during pregnancy performed in a secondary hospital were reported, and the outcomes were not worse than those of tertiary hospitals. Considering study results confirming increases in postoperative complications in mothers and fetuses with the progression of perforated appendicitis, the most important point of treating appendicitis in pregnancy is making an early diagnosis and deciding on subsequent urgent surgery. In case of pregnant women with abdominal pain, detailed physical examinations, diagnostic tests and ultrasonography should be conducted regardless of gestational age before performing early surgery. In addition, in case of symptoms lasting over an extended period of time or of leukocytosis, the risk of perforation is high, and appendicitis should be suspected. If abdominal pain is lasting, even normal test results should not be considered as normal. In terms of method of surgery, an open appendectomy is not the only choice; rather, a laparoscopic appendectomy is rather advantageous in terms of hospital stay and wound infection. However, principles in surgery on organ damage, intraabdominal pressure and operative time should also be kept in laparoscopic surgery. Upon completion of accumulating long-term data through follow-up, laparoscopic surgery may be established as a standard treatment for appendicitis in pregnancy.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Babaknia A, Parsa H, Woodruff JD. Appendicitis during pregnancy. Obstet Gynecol. 1977;50:40–44. [PubMed] [Google Scholar]
- 2.Gomez A, Wood M. Acute appendicitis during pregnancy. Am J Surg. 1979;137:180–183. doi: 10.1016/0002-9610(79)90140-5. [DOI] [PubMed] [Google Scholar]
- 3.Easton AL. Acute appendicitis in pregnancy: from the department of obstetrics and gynecology the Middlesex Hospital. Postgrad Med J. 1957;33:272–277. 286. doi: 10.1136/pgmj.33.380.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.King RM, Anderson GV. Appendicitis and pregnancy. Calif Med. 1962;97:158–162. [PMC free article] [PubMed] [Google Scholar]
- 5.Hee P, Viktrup L. The diagnosis of appendicitis during pregnancy and maternal and fetal outcome after appendectomy. Int J Gynaecol Obstet. 1999;65:129–135. doi: 10.1016/s0020-7292(99)00013-2. [DOI] [PubMed] [Google Scholar]
- 6.Guttman R, Goldman RD, Koren G. Appendicitis during pregnancy. Can Fam Physician. 2004;50:355–357. [PMC free article] [PubMed] [Google Scholar]
- 7.Popkin CA, Lopez PP, Cohn SM, Brown M, Lynn M. The incision of choice for pregnant women with appendicitis is through McBurney's point. Am J Surg. 2002;183:20–22. doi: 10.1016/s0002-9610(01)00842-x. [DOI] [PubMed] [Google Scholar]
- 8.Shin TS. Clinical observation appendectomy during pregnancy. J Korean Surg Soc. 1970;12:13–16. [Google Scholar]
- 9.Kim DJ, Cho HW, Kang JS. A clinical study on acute appendicitis in pregnancy. J Korean Surg Soc. 1982;24:83–88. [Google Scholar]
- 10.Cho H, Han DJ, Yoon DW. Clinical analysis of acute appendicitis in pregnancy. J Korean Surg Soc. 1986;31:363–372. [Google Scholar]
- 11.Kwon DH, Sung KH. A clinical analysis of acute appendicitis in pregnancy. J Korean Surg Soc. 1990;38:510–516. [Google Scholar]
- 12.Lee KW, Koo BG, Han HD, Kim DH. Appendicitis during pregnancy. Korean J Obstet Gynecol. 1990;33:1544–1548. [Google Scholar]
- 13.Kim LS, Lee YC, Kim DK, Kim S, Choi WJ, Lee JM, et al. A clinical study of acute appendicitis in pregnancy. J Korean Surg Soc. 1993;44:847–856. [Google Scholar]
- 14.Lee CS, Joo DH, Lee HI, Park SH, Yoo YO, Kim YI, et al. Clinical analysis of 36 appendectomies in pregnant women. J Korean Surg Soc. 1997;53:408–414. [Google Scholar]
- 15.Kim EC, Kang TW, Chang TS. Acute appendicitis during pregnancy. J Korean Surg Soc. 1997;52:128–136. [Google Scholar]
- 16.Ahn DH. Acute appendicitis during pregnancy. J Korean Soc Coloproctol. 1997;13:509–516. [Google Scholar]
- 17.Jang YS. A clinical study of acute appendicitis in pregnancy. J Korean Soc Coloproctol. 1998;14:767–774. [Google Scholar]
- 18.Seo SW, Kim SK. Acute appendicitis in pregnant patients and non-pregnant patients: recent clinical experience of the tertiary hospital. J Korean Surg Soc. 2002;62:486–490. [Google Scholar]
- 19.Oh SJ, Lee SH, Kim SY, Kim MJ, Kwon I, Heo SY, et al. Acute appendicitis in pregnancy. Korean J Obstet Gynecol. 2004;47:2104–2108. [Google Scholar]
- 20.Park CW, Sul JY. A comparison of laparoscopic versus open appendectomy during pregnancy. J Korean Soc Endosc Laparosc Surg. 2007;10:100–104. [Google Scholar]
- 21.Kim DH, Lee IK, Choi SB, Lee YS, Lee SK, Oh ST, et al. Laparoscopic vs. conventional appendectomy in pregnancy. J Korean Soc Coloproctol. 2008;24:161–165. [Google Scholar]
- 22.Oh BY, Kim KH, Lee RA, Chung SS. Diagnostic efficacy of the alvarado score according to age in acute appendicitis. J Korean Surg Soc. 2010;78:100–105. [Google Scholar]
- 23.Brown JJ, Wilson C, Coleman S, Joypaul BV. Appendicitis in pregnancy: an ongoing diagnostic dilemma. Colorectal Dis. 2009;11:116–122. doi: 10.1111/j.1463-1318.2008.01594.x. [DOI] [PubMed] [Google Scholar]
- 24.Freeland M, King E, Safcsak K, Durham R. Diagnosis of appendicitis in pregnancy. Am J Surg. 2009;198:753–758. doi: 10.1016/j.amjsurg.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 25.Lim HK, Bae SH, Seo GS. Diagnosis of acute appendicitis in pregnant women: value of sonography. AJR Am J Roentgenol. 1992;159:539–542. doi: 10.2214/ajr.159.3.1503019. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y, Zhao YY, Qiao J, Ye RH. Diagnosis of appendicitis during pregnancy and perinatal outcome in the late pregnancy. Chin Med J (Engl) 2009;122:521–524. [PubMed] [Google Scholar]
- 27.Nezhat FR, Tazuke S, Nezhat CH, Seidman DS, Phillips DR, Nezhat CR. Laparoscopy during pregnancy: a literature review. JSLS. 1997;1:17–27. [PMC free article] [PubMed] [Google Scholar]
- 28.Machado NO, Grant CS. Laparoscopic appendicectomy in all trimesters of pregnancy. JSLS. 2009;13:384–390. [PMC free article] [PubMed] [Google Scholar]
- 29.Yilmaz HG, Akgun Y, Bac B, Celik Y. Acute appendicitis in pregnancy: risk factors associated with principal outcomes: a case control study. Int J Surg. 2007;5:192–197. doi: 10.1016/j.ijsu.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 30.Mazze RI, Kallen B. Appendectomy during pregnancy: a Swedish registry study of 778 cases. Obstet Gynecol. 1991;77:835–840. [PubMed] [Google Scholar]