Abstract
Objectives
The association between changes in clinician self-efficacy and readiness to change and implementation of an asthma management program (Easy Breathing©) was examined.
Methods
A 36 month randomized, controlled trial was conducted involving 24 pediatric practices (88 clinicians). Randomized clinicians received interventions designed to enhance clinician self-efficacy and readiness to change which were measured at baseline and 3 years. Interventions consisted of an educational toolbox, seminars, teleconferences, mini-fellowships, opinion leader visits, clinician-specific feedback, and pay for performance. The primary outcome was program utilization (number of children enrolled in Easy Breathing/year); secondary outcomes included development of a written treatment plan and severity-appropriate therapy.
Results
At baseline, clinicians enrolled 149 ± 147 (mean ± SD) children/clinician/year; 84% of children had a written treatment plan and 77% of plans used severity-appropriate therapy. At baseline, higher self-efficacy scores were associated with greater program utilization (Relative Rate (RR) 1.34 (95% Confidence Interval 1.04, 1.72), p=0.04) but not treatment plan development (RR 0.63 (0.29, 1.35), p=.23) or anti-inflammatory use (RR 1.76 (0.92, 3.35), p=.09). Intervention clinicians participated in 17 interventions over 36 months. At study end, self-efficacy scores increased in intervention clinicians compared to control clinicians (p=0.01) and more clinicians were in an action stage of change (p=0.001) but these changes were not associated with changes in primary or secondary outcomes.
Conclusions
Self-efficacy scores correlated with program use at baseline and increased in the intervention arm but these increases were not associated with greater program-related activities. Self-efficacy may be necessary but not sufficient for behavior change.
Keywords: Stage of change, social learning theory, contingency management, pay for performance, academic detailing
Introduction
Guidelines for chronic disease management can improve both the process and outcomes of care1–4. Studies of guideline-specific therapies have not demonstrated broad use of evidence-based care in several important areas5–10. Reasons proposed for not adopting guidelines8 include physician-related issues (e.g. lack of awareness, knowledge or agreement)11, guideline-related issues (based on consensus rather than evidence, complexity, adoption complexity)12, organizational issues (e.g. time constraints, job satisfaction, turnover)13–14 and health policy issues (e.g. access to care, reimbursement)15–16.
Two important personal attributes - self-efficacy and readiness to change - have been associated with health behavior change in patients and to a lesser extent to use of guidelines by clinicians17–20. Self-efficacy, (the degree of confidence in one’s capacity for success in implementing a goal-directed behavior21), is a personal attribute that is central to social learning theory (SLT)22. SLT has been applied successfully to many health behaviors and to health-related behavior change and maintenance21, 23. Clinicians with high self-efficacy are thought to be more likely to adopt and adhere to guidelines19. Readiness to change24 recognizes that each individual is at a different stage of behavior change and that interventions must be tailored to each individual’s stage of readiness within the continuum beginning with pre-contemplation, contemplation of a behavior change, the action of a behavior change and the maintenance of that change25. Stages of change recognizes that changing behavior is complex, that one intervention will not work for everyone, that change does not occur quickly or immediately and that increasing self-efficacy may be one of several processes that promote change.
Easy Breathing© is an asthma management program for pediatricians that is based upon the National Asthma Education and Prevention Program Expert Panel Reports (NAEPP-EPR)26–27. The program is currently being used by more than 450 clinicians in Connecticut. In Connecticut, enrollment of Medicaid-insured children in Easy Breathing has resulted in a 34% decrease in hospitalization, a 31% decrease in ED visits and a 29% decrease in outpatient visits28. Privately insured children with persistent asthma in Connecticut have experienced a 56% decrease in outpatient visits and a 91% decrease in ED visits29. The program was designed to overcome guideline- and organizational-related barriers by using an evidence-based approach, by reducing guideline complexity and by reducing the time needed for asthma management. Despite the program’s simplicity and improved efficiency29–31, however, not all pediatricians use the program fully or to the same extent.
A three-arm randomized, controlled trial (The Provider and Organization in Asthma Guidelines, #NCT00345514) was conducted to examine whether interventions directed at changing provider self-efficacy and stages of change or interventions designed to change organizational culture (e.g. teamwork building, role clarity) resulted in greater program utilization. Results from the provider intervention arm compared to the control arm are reported here. We hypothesized that clinicians in the provider-directed intervention arm, as a result of participating in various study-supported interventions, would increase their self-efficacy and move into an action stage of readiness to change and that these changes would be associated with more children being enrolled in the Easy Breathing program as compared to control clinicians.
Methods
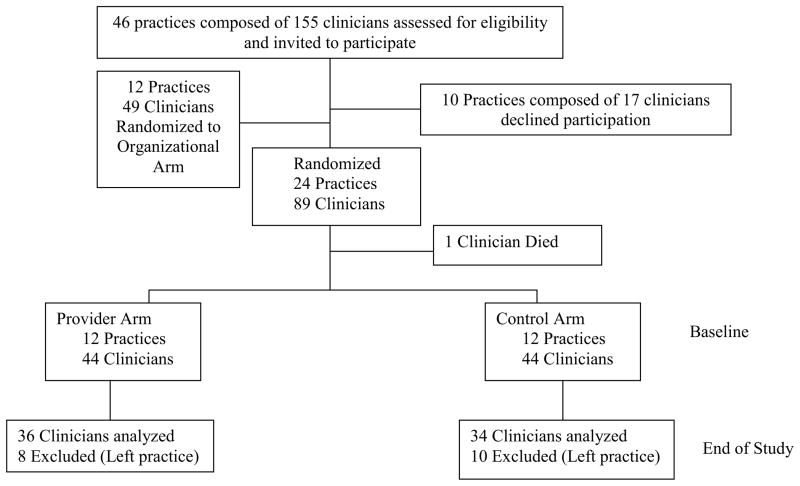
Twenty four pediatric practices (8 urban and 16 private) in central Connecticut completed baseline measures that examined clinician self-efficacy and stages of change related to asthma, in addition to other measures and were randomized into a control or provider intervention arm32, 33 (Figure 1).
Figure 1.
A practice was eligible to participate if the clinicians had been previously trained in the Easy Breathing© program, which has been described34–35. The Easy Breathing program at this time consisted of 4 elements: an Easy Breathing Survey composed of 11 demographic, exposure and family history questions and 4 questions validated for use in making a diagnosis of asthma36; a Provider Assessment with 4 symptom-related questions that guide clinicians in determining asthma severity for children with asthma37; a Treatment Selection Guide of asthma medications and appropriate dosages and insurance coverage by asthma severity for daily, sick and emergency use; and a simple, written Asthma Treatment Plan (in multiple languages) that is given to every parent/child with asthma38. All children greater than 6 months of age, regardless of their asthma status and regardless of the reason for their visit, were eligible to have their parents complete a Survey. A copy of each form was provided to the investigators.
The primary outcome measure was the number of children enrolled in Easy Breathing (i.e. completed an Easy Breathing Survey) per full time equivalent (FTE) clinician per year. This was chosen as the primary outcome measure because children diagnosed with asthma who completed a Survey, experienced significant decreases in medical services utilization28–29. Quality of care measures including severity-appropriate anti-inflammatory therapy prescribing for children with persistent asthma and creation of a written asthma treatment plan were secondary outcomes.
This study was approved by the Institutional Review Boards at Connecticut Children’s Medical Center and the University of Connecticut Health Center and informed consent was obtained from clinicians, staff and parents/guardians.
Study Design
After completion of baseline questionnaires, 12 practices were randomly assigned to the provider arm and 12 were randomized to a control arm. A priori, practice size, the practice patient profile (including the percent of patients receiving state supported assistance) and the duration of participation in Easy Breathing were considered potential modifiers of the interventions. For this reason, the randomization strategy matched practices according to practice type (urban vs. non-urban), practice size and duration of participation in Easy Breathing. Urban clinics were defined as clinics serving primarily a Medicaid (>50%) population who resided in a high density area (>500–1000 people per square mile (www.census.gov/geo/ua)). Urban clinics were in general large (>5 FTE clinicians) and federally funded or subsidized. Both arms received on-going programmatic support from Easy Breathing staff consisting of bi-weekly visits by program coordinators to re-stock forms and program materials, quarterly newsletters, and quarterly clinic/practice summaries. Practices in the intervention arm in addition were offered multiple interventions of a type reported by others to enhance self-efficacy (Table 1). Each intervention practice was given an educational toolbox which consisted of a cart with a VCR and educational tapes, demonstration spacers and inhalers and instruction sheets for each inhaler, medication identification posters, peak flow meters and graphs, educational brochures (risks of corticosteroids, environmental trigger avoidance) and airway models. Luncheon seminars were offered on 7 topics including office management of asthma, spirometry, spacers and peak flow meters. Eight monthly 30 minute teleconferences were offered at 3 different times and discussed cough, indoor airway quality, allergic rhinitis and adolescent adherence to therapy. Mini fellowships consisting of a half day of shadowing an asthma specialist were also offered. Three national experts participated in Grand Rounds and dinner symposia that were open to all clinicians but intervention clinicians received personal invitations. Individual provider feedback on performance including number of children enrolled in Easy Breathing, number of treatment plans submitted and percent of treatment plans that adhered to the national asthma guidelines were distributed quarterly. Since the control arm was not a “do-nothing” arm, the contrast between the two arms represents the impact of interventions over and above that gained from the effect of a successful disease management program. Because the best interventions to change clinician behavior are not known39–43, our goal was not to test one specific intervention but rather to offer clinicians multiple interventions and the opportunity to choose the interventions appropriate to their self-identified needs.
Table 1.
Interventions in Provider Arm
| Intervention | # times offered | # participating** |
|---|---|---|
| Educational toolbox | 1 | 44 |
| Educational Seminars* | 27 | 42 |
| Teleconferences | 35 | 36 |
| Mini-fellowships | 32 | 21 |
| Opinion Leaders | 3 | N/A |
| Clinician Feedback | 11 | 44 |
| Pay for Performance | 7 | 44 |
Seminars provided CME credits and focused on enhancing education around the diagnosis and management of asthma and asthma-related co-morbidities.
Number of unique individuals who participated in at least one of the specific interventions N/A Information on number participating not available.
Questionnaires
Questionnaires that assessed SLT-derived personal attributes were completed before randomization (baseline, T1) and at the end of the study (T2) and returned in numbered envelopes. Incentives for questionnaire completion included a drawing for a gift card.
The Asthma Practice Survey consisted of 52 items and assessed clinician goals for asthma care, time spent in asthma-related activities, self-efficacy, outcome value and expectancy and barriers to asthma care. The instrument was made specific for asthma from a general pediatric instrument44 and from the recommendations of the NAEPP-EPR26–27. Self-efficacy was assessed by having participants rate their level of confidence on a 7-point Likert scale in being able to carry out activities in 14 areas related to asthma care including making an asthma diagnosis, developing an asthma treatment plan, and teaching patients about asthma. Cronbach’s alpha for self-efficacy for the two time periods was 0.93 and 0.94.
Readiness to change was assessed using a 12-item questionnaire modeled after Rollnick et al45. Clinicians responded to statements regarding the NAEPP Guidelines and their use of the Guidelines using a 5-point Likert scale (strongly disagree to strongly agree). The initial survey was reviewed by 5 experts in the stages of change literature. They determined face and construct validity by examining and assigning each item to pre-contemplative, contemplative, and action stages. A modified Delphi approach was used to come to consensus. Since the goal of the study was to increase enrollment of children in the program, maintenance items were excluded since their inclusion would prevent the emergence of factors corresponding to stages of change46. An exploratory factor analysis demonstrated 3 reliable, well-defined components corresponding to the following stages of change: Pre-contemplative, Contemplative and Action. Re-test reliability was determined over a 3-month period.
Statistical analysis
The primary outcome was the number of Easy Breathing Surveys completed by a clinician and the study was powered to detect an 8% increase in study enrollment (ie Easy Breathing Surveys) at an alpha level of 0.05 and a power of 86%. The Easy Breathing enrollment rate/full time equivalent (FTE) clinician was defined as the total number of children with a completed Easy Breathing Survey per FTE per year. Two secondary outcomes were also tested: submission of a written asthma treatment plan and adherence of that plan to national guidelines for appropriate use of anti-inflammatory therapy for children with persistent asthma. These secondary outcome measures were chosen because clinicians under-prescribe anti-inflammatory therapy and under-use written treatment plans47–48. Asthma treatment plan use for each clinician was defined as the number of children with persistent asthma who had a written treatment plan divided by the number of children with persistent asthma enrolled by that clinician. Adherence to national guidelines for use of anti-inflammatory therapy for each clinician was defined as the number of submitted written treatment plans for children with persistent asthma with a severity-appropriate anti-inflammatory drug (usually an inhaled corticosteroid) divided by the number of written treatment plans for children with persistent asthma since this was the only prescribing information that was available. The investigators received copies of the Survey and the written treatment plan. Analyses were adjusted for FTE and were performed at baseline (T1) and 36 months later at study end (T2). All models were fit using SAS version 9.2 (SAS Institute Inc, Cary, NC).
Changes in self-efficacy and stages of change were tested using the Wilcoxon signed rank test. The Kruskal-Wallis test was used to compare characteristics at baseline across the study arms. Linear mixed models (controlling for the proportion of patients in the practice on public insurance as an indicator of an urban-based clinic) were used to examine differences between mid-level practitioners’ (MLP, e.g., advanced practice nurses, pediatric nurse practitioners and physician assistants) and physicians’ self-efficacy; a random intercept was included in the model to account for the fact that clinicians were clustered within practices.
The nesting of clinicians in a practice was accounted for using linear mixed models with a random intercept to also model the number of Easy Breathing Surveys/FTE clinician as a function of self-efficacy using the square root of the survey number. Covariates included the practice’s insurance profile, the staff-to-clinician ratio, the clinician’s highest degree (MD vs. MLP) and clinician FTE%. The number of submitted written asthma treatment plans and the number of adherent-to-guideline written treatment plans were modeled using the binomial distribution. All random effects were modeled using normal distributions.
Results
Study Participants
Eighty-eight clinicians in 24 practices randomized either into the provider arm (n=44 clinicians, 12 practices) or the control arm (Figure 1, Table 2). Eighteen clinicians (⅔ were MLPs) left their practice before end of study. Their data were used at baseline only. Two thirds of the clinicians were full time physicians and ⅓ were mid-level practitioners. Seventy-five percent of physicians and 40% of mid-level practitioners had received their highest degree more than 10 years previously with a mean tenure of 10 years.
Table 2.
Baseline Demographics of Participants
| Personal Characteristics* | Control Arm (n=44) | Provider Arm (n=44) | P Value |
|---|---|---|---|
|
| |||
| Age (yrs) | 45 ± 9 (range: 27–62) | 43 ± 12 (range: 26–80) | 0.48 |
|
| |||
| Gender | M: 9 (20%) | M: 18 (41%) | 0.04 |
|
| |||
| Ethnicity | 0.61 | ||
| Caucasian | 37 (84%) | 40 (91%) | |
| African-American | 3 (7%) | 2 (5%) | |
| Other/Unknown | 4 (9%) | 2 (5%) | |
|
| |||
| Employment Status | 0.12 | ||
| Full Time | 25 (57%) | 32 (73%) | |
| Part Time | 19 (43%) | 12 (27%) | |
|
| |||
| Tenure (yrs) | 9 ± 8 (range: 1–30) | 9 ± 9 (range: 1–30) | 0.84 |
|
| |||
| Clinician Demographics | |||
| Provider Type | 0.82 | ||
| Physician | 28 (64%) | 29 (66%) | |
| Mid-Level Practitioner | 16 (36%) | 15 (34%) | |
|
| |||
| Yrs Since Highest Degree | 0.32 | ||
| <5 Yrs | 4 (9%) | 7 (16%) | |
| 5 – 10 Yrs | 17 (40%) | 11 (26%) | |
| >10 Yrs | 22 (51%) | 25 (58%) | |
|
| |||
| No. Hours Seeing Patients/week: | |||
| Physicians | 33 ± 12 (5–60) | 36 ± 11 (8–60) | 0.39 |
| Mid-level practitioner | 31 ± 10 (10–40) | 31 ± 10 (8–40) | 0.86 |
Mean ± SD (Range) or Frequency (Percent)
Baseline Program Use and Quality, Self-efficacy and Relationship to Easy Breathing Surveys
At baseline, clinicians completed 149 ± 147 surveys/FTE/yr (mean ± SD); 84% of children had a written treatment plan and 77% of those plans adhered to national asthma guidelines. Baseline self-efficacy scores for all clinicians in both study arms were high (Table 3). There was no difference in baseline survey number, use of a treatment plan, anti-inflammatory therapy use or self-efficacy scores between clinicians in either study arm or between physicians as compared to mid-level practitioners.
Table 3.
Self Efficacy Scores*
| Baseline (T1); n** | End of Study (T2); n | P value | |
|---|---|---|---|
|
| |||
| Overall | |||
|
| |||
| All Clinicians | 5.91 ± 0.62; n=88 | 6.10 ± 0.69; n=68 | 0.0001 |
| Physicians Only | 5.86 ± 0.70; n=57 | 6.08 ± 0.65; n=49 | 0.0002 |
| Mid-levels Only | 6.01 ± 0.65; n=31 | 6.16 ± 0.79; n=19 | 0.20 |
|
| |||
| By Intervention Arm | |||
|
| |||
| Provider Arm | |||
| All Clinicians | 5.95 ± 0.58; n=44 | 6.18 ± 0.54; n=34 | 0.0008 |
|
| |||
| Control Arm | |||
| All Clinicians | 5.88 ± 0.66; n=44 | 6.02 ± 0.81; n=34 | 0.23 |
Mean ±SD
n= number completing self-efficacy measurement; two clinicians in the provider arm did not complete self efficacy measures at study end
Higher baseline clinician self-efficacy scores were associated with a greater number of surveys (Relative Rate (RR) 1.34 (95% Confidence Interval 1.04, 1.72), p=0.04) but were not associated with anti-inflammatory therapy use or creation of a written asthma treatment plan (RR = 1.76 (0.92, 3.35), p=0.09, RR =0.63 (0.29, 1.35), p=0.23 respectively).
Effect of Interventions on Self-efficacy in Clinicians in the Provider Arm
All clinicians in practices in the provider arm participated in at least one of the 8 categories of provider interventions which were offered a total of 115 times over the 3 years (Table 1). On average, provider arm clinicians participated in 17 interventions (range 1 to 30) over the 3 years.
In the intervention arm, clinician self-efficacy scores increased between baseline and end of study (p=.0008) (Table 3). Clinicians with the lowest self-efficacy scores (below 50th percentile, i.e. less than 5.92) at baseline had larger increases in self-efficacy scores from baseline to end of study as compared to clinicians with higher self-efficacy scores at baseline (change = +0.70 ± 0.55 vs. +0.09 ± 0.55, p=0.02) but self-efficacy increased for all clinicians regardless of their baseline self-efficacy scores In contrast, for clinicians in the control arm, there was no change in self-efficacy scores between baseline and end of study (change = +0.17 ± 0.55, p=0.23 respectively).
Increases in self-efficacy over the intervention period among clinicians in the intervention arm did not predict increases in survey number when controlling for % FTE, non-clinician to clinician ratio, public insurance, and clinician type (p=0.45). For these clinicians in the intervention arm, there was no relationship between the increase in self-efficacy scores from baseline to study end and the number of interventions in which they participated (R2 = 0.007, p=0.70). Furthermore, increases in self-efficacy after the interventions in clinicians with the lowest self-efficacy scores at baseline were not associated with increases in survey number. Increases in self-efficacy scores at study end were associated with neither greater use of anti-inflammatory therapy for children with persistent disease (RR=0.94 (0.51, 1.75), p=0.85 respectively) nor an increase in the number of children with a written asthma treatment plan (RR=1.82 (0.65, 5.05), p=0.24).
At study end, there was no difference in program utilization, in anti-inflammatory use or in creation of a written treatment plan between the intervention and control arms of the study.
Stages of Change at Baseline and After Interventions in the Provider Arm
Most clinicians at baseline were in the action stage of change (66% action, 34% contemplative). Self-efficacy scores at baseline were higher among clinicians in the action stage than among those in the contemplative stage (6.09 ± 0.49 vs. 5.68 ± 0.67, p=0.05). At study end, all clinicians in the intervention arm except one were in the action stage of change (p=0.001). In contrast, there was no change in stage of change for clinicians in the control arm (88% action at study start; 86% action at end of study, p=0.72). The increase in the number of clinicians in the action stage of change in the intervention arm at study end was not associated with an increase in the number of children enrolled in Easy Breathing (p=.13), with adherence to use of anti-inflammatory therapy for children with persistent disease (p=0.11) or with use of a written asthma treatment plan (p=0.36).
Discussion
For all participants in this study, higher asthma-related self-efficacy scores at baseline were associated with greater asthma program-related activity (i.e., enrollment in Easy Breathing). Self-efficacy scores and readiness to change increased in clinicians in the intervention arm but these increases were not associated with an increase in program enrollment, in increased development of a written asthma treatment plan or with greater use of anti-inflammatory therapy for persistent asthma.
The gap between asthma guidelines and their implementation in primary care practice settings is considerable. The reasons for this gap are multi-factorial and include patient, payer25 and provider-related issues11. We implemented a set of interventions designed to increase clinician self-efficacy and examined the effectiveness of these interventions at changing behavior as measured by enrollment of children in a disease management program, creation of a written asthma treatment plan and use of anti-inflammatory therapy. The interventions were consistent with social learning theory and were designed to motivate clinicians to increase enrollment through use of live, interactive CME programs to enhance their knowledge, and change their attitudes and beliefs; other strategies known to change behavior including performance feedback, opinion leaders, flow sheets and an educational toolbox were also used. The variable of time was then added using the transtheoretical (readiness to change) model and tailored interventions to assure a full range of stage-appropriate interventions and the interventions were offered multiple times over a 3 year period. The interventions increased clinician self-efficacy and moved clinicians to an action stage of change but did not change any of the targeted behaviors.
Most of the clinicians were in the action stage of change at the beginning of this study. This is not surprising since all of them had modified their practice behavior by participating in Easy Breathing and in this study. Knowledge provided through the various Continuing Medical Education (CME) activities could have created the precondition for change but other interventions including quarterly newsletters, pay for performance and clinician-specific feedback might also have moved clinicians in the intervention arm from the contemplative to the action stage of change. This did not, however, result in an increase in enrollment in children in Easy Breathing. Often behavior change is equated with action but action is only one of the many stages of change in the transtheoretical model and not all modifications of behavior count as action in this model49 which could explain why the transtheoretical model has recently been criticized50.
Self-efficacy is a perception of one’s own capacity for success in organizing and implementing a goal-directed behavior21. Resilient self-efficacy enables individuals to do extraordinary things by productive use of the skills they possess in the face of overwhelming obstacles22–23. Clinicians on average participated in 17 interventions over the 3 year study period and the rates of participation remained constant even after 3 years. Although self-efficacy scores were high at the start of the study, they increased further among intervention participants suggesting a lack of a ceiling effect even though those with lower self-efficacy showed greater improvement over time. These increases in self-efficacy, however, did not result in an increase in enrollment even though an association between baseline self-efficacy and enrollment in Easy Breathing was observed. The minimum effective change in measures such as self-efficacy that result in behavior change is not known and so it is possible that the increase in self-efficacy that we observed was statistically significant but not clinically significant. Alternatively, it is possible that self-efficacy demonstrates a threshold for its association with behavior and clinicians in the study were above this threshold. Thus, changes in self-efficacy might translate into changes in a goal-directed behavior in individuals starting with lower self-efficacy levels even though this was not observed in the subset of clinicians with the lowest self-efficacy scores in this study.
This study has several additional limitations. The large clinician drop out (primarily mid-level practitioners) secondary to leaving the practice was unexpected and could have resulted in a decrease in power but the number of participants was sufficient to demonstrate a change in both self-efficacy and in stages of change. The number of children enrolled did not increase over time in either study arm and this potentially could be due to a fatigue factor51, or to a decrease in the number of eligible children for enrollment over time; these could also have limited the benefits of our interventions. Other measures such as ease of use or efficiency of asthma management may have increased over time but were not measured.
Thus, the interventions in the provider arm increased self-efficacy and moved individuals to an action stage of change. Nevertheless, these changes were not sufficient to increase patient enrollment or to increase the number of submitted written asthma treatment plans or use of anti-inflammatory therapy. Both high self-efficacy and an action stage of change may be required to change behavior but neither may be sufficient to change behavior. Environmental factors or organizational attributes could also influence behavior and either support a clinician’s personal attributes or inhibit their capacity for productivity.
What’s New.
This study demonstrates that interventions can increase clinician self-efficacy and move clinicians to an action stage of change but neither may be sufficient to effect behavior change related to guideline implementation.
Acknowledgments
We are grateful to Ms Pamela Higgins for programmatic support, Ms Trudy Lerer and Ms Autherene Grant for data analysis and entry, and Ms Michelle Morse for administrative support and to the practices, clinicians and staff who participated in this project.
This work was supported by the National Heart Lung and Blood Institute of the National Institutes of Health (RO1 HL 70785-01) (Michelle M. Cloutier P.I.).
Footnotes
Authors confirm there are no conflicts of interest related to this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rodbard HW, Blonde L, Braithwaite SS, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Endocr Pract. 2007;13(Suppl 1):1–68. doi: 10.4158/EP.13.S1.1. [DOI] [PubMed] [Google Scholar]
- 2.Khan NA, McAlister FA, Rabkin SW, et al. The 2006 Canadian Hypertension Education Program recommendations for the management of hypertension: Part II - Therapy. Can J Cardiol. 2006;22(7):583–593. doi: 10.1016/s0828-282x(06)70280-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green LA, Dickinson WP, Nease DEJ, et al. AAFP guideline for the detection and management of post-myocardial infarction depression. Ann Fam Med. 2009;7(1):71–79. doi: 10.1370/afm.918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Cholesterol Education Program (NCEP) Expert Panel on Detection. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 5.Schiele F, Meneveau N, Seronde MF, et al. Compliance with guidelines and 1-year mortality in patients with acute myocardial infarction: a prospective study. Eur Heart J. 2005;26(9):873–880. doi: 10.1093/eurheartj/ehi107. [DOI] [PubMed] [Google Scholar]
- 6.Al-Omran M, Mamdani MM, Lindsay TF, et al. Suboptimal use of statin therapy in elderly patients with atherosclerosis: a population-based study. J Vasc Surg. 2008;48(3):607–612. doi: 10.1016/j.jvs.2008.04.057. [DOI] [PubMed] [Google Scholar]
- 7.Boulet LP, McIvor RA, Marciniuk D Committee CTSRG. Respiratory guidelines implementation in Canada. Can Respir J. 2007;14(6):329–330. doi: 10.1155/2007/592534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collini P, Beadsworth M, Anson J, et al. Community-acquired pneumonia: doctors do not follow national guidelines. Postgrad Med. 2007;83(982):552–555. doi: 10.1136/pgmj.2006.056556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raum E, Lietzau S, Stegmaier C, Brenner H, Rothenbacher D. For the majority of patients with diabetes, blood pressure and lipid management is not in line with recommendations. Results from a large population-based cohort in Germany. Pharmacoepidemiol Drug Saf. 2008;17(5):485–494. doi: 10.1002/pds.1589. [DOI] [PubMed] [Google Scholar]
- 10.Navaratnam P, Jayawant SS, Pedersen CA, Balkrishnan R. Asthma pharmacotherapy prescribing in the ambulatory population of the United States: evidence of nonadherence to national guidelines and implications for elderly people. Journal of the American Geriatrics Society. 2008;56(7):1312–1317. doi: 10.1111/j.1532-5415.2008.01767.x. [DOI] [PubMed] [Google Scholar]
- 11.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? JAMA. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 12.Picken HA, Greenfield S, Teres D, Hirway PS, Landis JN. Effect of local standards on the implementation of national guidelines for asthma: primary care agreement with national asthma guidelines. J Gen Intern Med. 1998;13(10):659–663. doi: 10.1046/j.1525-1497.1998.00200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsai CL, Sullivan AF, Gordon JA, et al. Quality of care for acute asthma in 63 US emergency departments. J Allergy Clin Immunol. 2009;123(2):354–361. doi: 10.1016/j.jaci.2008.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elovainio M, Makela M, Sinervo T, Kivimaki T, Eccles M, Kahan J. Effects of job characteristics, team climate, and attitudes towards clinical guidelines. Scand J Public Health. 2000;28(2):117–122. doi: 10.1177/140349480002800207. [DOI] [PubMed] [Google Scholar]
- 15.Rapezzi C, Biagini E, Bellis P, et al. Exploring the gap between National Cholesterol Education Program guidelines and clinical practice in secondary care: results of a cross-sectional study involving over 10,000 patients followed in different specialty settings across Italy. J Cardiovasc Med. 2008;9(9):878–887. doi: 10.2459/JCM.0b013e3282f56513. [DOI] [PubMed] [Google Scholar]
- 16.Weinberger M. Seventeen years of asthma guidelines: Why hasn’t the outcome improved for children? J Pediatr. 2009;154:786–788. doi: 10.1016/j.jpeds.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Vogt F, Hall S, Hankins M, Marteau TM. Evaluating three theory-based interventions to increase physicians’ recommendations of smoking cessation services. Health Psychology. 2009;28(2):174–182. doi: 10.1037/a0013783. [DOI] [PubMed] [Google Scholar]
- 18.Zhu DQ, Norman IJ, While AE. The relationship between doctors’ and nurses’ own weight status and their weight managment practices: a systematic review. Obesity Reviews. 2011;12(6):459–469. doi: 10.1111/j.1467-789X.2010.00821.x. [DOI] [PubMed] [Google Scholar]
- 19.Salinas GD, Williamson JC, Kalhan R, et al. Barriers to adherence to chronic obstructive pulmonary disease guidelines by primary care physicians. International Journal of Copd. 2011;6:171–179. doi: 10.2147/COPD.S16396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shirazi M, Zeinaloo AA, Parikh SV, et al. Effects on readiness to change of an educational intervention on depressive disorders for general physicians in primary care based on a modified Prochaska model - a randomized controlled study. Fam Pract. 2008;25(2):98–104. doi: 10.1093/fampra/cmn008. [DOI] [PubMed] [Google Scholar]
- 21.Bandura A. Self-efficacy: The Exercise of Control. New York: WH Freeman; 1996. The Nature and Structure of Self-efficacy; pp. 36–78. [Google Scholar]
- 22.Bandura A. A Social Cognitive Theory. Englewood Cliffs: NJ Prentice-Hall; 1986. Social Foundation of Thought and Action. [Google Scholar]
- 23.Maddux JE, Norton LW, Stoltenberg CD. Self-efficacy expectancy, outcome expectancy, and outcome value: Relative effects on behavioral intentions. J Personality Soc Psych. 1986;51:783–789. [Google Scholar]
- 24.Prochaska JO, Velicer WF, DiClemente CC, Fava J. Measuring processes of change: applications to the cessation of smoking. J Consult Clin Psychol. 1988;56:520–528. doi: 10.1037//0022-006x.56.4.520. [DOI] [PubMed] [Google Scholar]
- 25.Cohen SJ, Halvorson HW, Gosselink CA. Changing physician behavior to improve disease prevention. Prev Med. 1994;23:284–291. doi: 10.1006/pmed.1994.1040. [DOI] [PubMed] [Google Scholar]
- 26.National Institutes of Health, National Heart Lung, and Blood Institute. Guidelines for the diagnosis and management of asthma. Bethesda, MD: NIH Publication; 1997. pp. 97–4051. [Google Scholar]
- 27.National Institutes of Health. National Heart Lung, and Blood Institute. Guidelines for the diagnosis and management of asthma Expert Panel Report 2 - update on selected topics 2002. Bethesda, MD: NIH Publication 02-5074; 2003. [Google Scholar]
- 28.Cloutier MM, Wakefield DB. Translation of a pediatric asthma management program into the community in Connecticut. Pediatrics. 2011;127(1):11–18. doi: 10.1542/peds.2010-1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cloutier MM, Wakefield DB, Sangeloty-Higgins P, Delaronde S, Hall CB. Asthma guideline use by pediatricians in private practices and asthma morbidity. Pediatrics. 2006;118(5):1880–1887. doi: 10.1542/peds.2006-1019. [DOI] [PubMed] [Google Scholar]
- 30.Cloutier MM, Grosse SD, Wakefield DB, Nurmagambetov TA, Brown CM. The economic impact of an urban asthma management program. Am J Managed Care. 2009;15(6):345–351. [PubMed] [Google Scholar]
- 31.Brazil K, Cloutier MM, Tennen H, Bailit H, Higgins PS. A qualitative study of the relationship between clinician attributes, organization, and patient characteristics on implementation of a disease management program. Dis Manage. 2008;11(2):129–137. doi: 10.1089/dis.2008.1120008. [DOI] [PubMed] [Google Scholar]
- 32.Tennen H, Cloutier MM, Wakefield DB, Hall CB, Brazil K. The buffering effect of hope on clinicians’ behavior: A test in pediatric primary care. J Soc Clin Psychol. 2009;28(5):554–576. doi: 10.1521/jscp.2009.28.5.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hall CB, Tennen H, Wakefield DB, Brazil K, Cloutier MM. Organizational assessment in pediatric primary care: development and initial validation of the primary care organizational questionnaire. Health Serv Manage Res. 2006;19(4):207–214. doi: 10.1258/095148406778951457. [DOI] [PubMed] [Google Scholar]
- 34.Cloutier MM, Wakefield DB, Carlisle PS, Bailit HL, Hall CB. The effect of Easy Breathing on asthma management and knowledge. Arch Pediatr Adolesc Med. 2002;156(10):1045–1051. doi: 10.1001/archpedi.156.10.1045. [DOI] [PubMed] [Google Scholar]
- 35.Cloutier MM, Wakefield DB, Hall CB, Bailit HL. Childhood asthma in an urban community: prevalence, care system, and treatment. Chest. 2002;122(5):1571–1579. doi: 10.1378/chest.122.5.1571. [DOI] [PubMed] [Google Scholar]
- 36.Hall CB, Wakefield D, Rowe TM, Carlisle PS, Cloutier MM. Diagnosing pediatric asthma: validating the Easy Breathing Survey. J Pediatr. 2001;139(2):267–272. doi: 10.1067/mpd.2001.116697. [DOI] [PubMed] [Google Scholar]
- 37.Cowen MK, Wakefield DB, Cloutier MM. Classifying asthma severity: objective versus subjective measures. Journal of Asthma. 2007;44(9):711–715. doi: 10.1080/02770900701595576. [DOI] [PubMed] [Google Scholar]
- 38.Marder D, Cloutier MM. Asthma education: Are inner city families getting the message? J Resp Dis. 1999;20(9):630–635. [Google Scholar]
- 39.Smeele IJ, Grol RP, van Schayck CP, van den Bosch WJ, van den Hoogen HJ, Muris JW. Can small group education and peer review improve care for patients with asthma/chronic obstructive pulmonary disease? Qual Health Care. 1999;8(2):92–98. doi: 10.1136/qshc.8.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cortoos PJ, Simoens S, Peetermans W, Willems L, Laekeman G. Implementing a hospital guideline on pneumonia: a semi-quantitative review. Int J Qual Health Care. 2007;19(6):358–367. doi: 10.1093/intqhc/mzm045. [DOI] [PubMed] [Google Scholar]
- 41.Lu CY, Ross-Degnan D, Soumerai SB, Pearson SA. Interventions designed to improve the quality and efficiency of medication use in managed care: a critical review of the literature - 2001–2007. BMC Health Serv Res. 2008;8:75. doi: 10.1186/1472-6963-8-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crawford PB, Gosliner W, Strode P, et al. Walking the talk: fit WIC wellness programs improve self-efficacy in pediatric obesity prevention counseling. Am J Public Health. 2004;94(9):1480–1485. doi: 10.2105/ajph.94.9.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Colombet I, Sabatier B, Gillaizeau F, Prognon P, Begue D, Durieux P. Long-term effects of a multifaceted intervention to encourage the choice of the oral route for proton pump inhibitors: an interrupted time-series analysis. Qual Saf Health Care. 2009;18(3):232–235. doi: 10.1136/qshc.2007.023887. [DOI] [PubMed] [Google Scholar]
- 44.Cheng TL, DeWitt TG, Savageau JA, O’Connor KG. Determinants of counseling in primary care pediatric practices: Physician attitudes about time, money and health issues. Arch Pediatr Adolesc Med. 1999;153:629–635. doi: 10.1001/archpedi.153.6.629. [DOI] [PubMed] [Google Scholar]
- 45.Rollnick S, Healther N, Gold R, Hall W. Development of a short “readiness to change” questionnaire for use in brief, opportunistic interventions among excessive drinkers. Br J Addict. 1992;87:743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- 46.Rollnick S, Mason P, et al. Health behavior change: A guide for practitioners. London, United Kingdom: Churchill Livingston; 1999. [Google Scholar]
- 47.Piecoro LT, Potoski M, Talbert JC, Doherty DE. Asthma prevalence, cost, and adherence with expert guidelines on the utilization of health care services and costs in a state Medicaid population. Health Serv Res. 2001;36:357–371. [PMC free article] [PubMed] [Google Scholar]
- 48.Lieu TA, Quesenberry P, Capra AM, Sorel ME, Martin KE, Mendoza GR. Outpatient management practices associated with reduced risk of pediatric asthma hospitalization and emergency department visits. Pediatrics. 1997;100:334–341. doi: 10.1542/peds.100.3.334. [DOI] [PubMed] [Google Scholar]
- 49.Snyder CR, Forsyth DR. Handbook of Social and Clinical Psychology: The Health Perspective. New York: Pergamon Press; 1990. Self-efficacy; pp. 57–78. [Google Scholar]
- 50.West R. Time for a change: Putting the transtheoretical (stages of change) model to rest. Addiction. 2005;100(8):1036–1039. doi: 10.1111/j.1360-0443.2005.01139.x. [DOI] [PubMed] [Google Scholar]
- 51.Smith WR. Evidence for the effectiveness of techniques to change physician behavior. Chest. 2000;118(2):8S–17S. doi: 10.1378/chest.118.2_suppl.8s. [DOI] [PubMed] [Google Scholar]