Abstract
In traditional Chinese medicine (TCM) clinical practice, ZHENG (also known as syndrome) helps to guide design of individualized treatment strategies. In this study, we investigated the clinical use of ZHENG in TCM-treated cancer patients by systematically analyzing data from all relevant reports in the Chinese-language scientific literature. We aimed to determine the clinical ZHENG distributions in six common cancers (lung, liver, gastric, breast, colorectal, and pancreatic) with the expectation of uncovering a theoretical basis for TCM ZHENG as a clinical cancer treatment. In addition, we also reviewed the molecular basis underlying Xue-Yu (blood stasis), Shi-Re (dampness-heat), Yin-Xu (Yin deficiency), and Pi-Xu (spleen deficiency) ZHENG that are commonly found in cancer patients. The results from our summary study provide insights into the potential utility of TCM ZHENG and may contribute to a better understanding of the molecular basis of TCM ZHENG in cancer.
1. Introduction
Traditional Chinese medicine (TCM) has been practiced and recorded in the medical literature for thousands of years. It is considered unique among the world's ancient traditional medicines based upon its integrative use of physiological and holistic theories; for example, a key aim of TCM is to regulate and maintain proper body functions by modulating and exploiting interactions between the patient and their environment. The rich history of TCM has prompted a recent surge in clinical research efforts to evaluate its efficacy as an alternative strategy to the largely pharmaceutical-based approaches used in developed countries to prevent and treat many types of disease, including cancers.
It has been reported that over 90% of modern Chinese cancer patients received some form of TCM during their treatment regimen [1]. The rates of TCM used by health care providers and interest by patients outside of China are continuing or rise annually, especially within the field of oncology [2]. Application of TCM as an adjuvant cancer therapy has been reported to enhance the efficacy of both chemo- and radiotherapy and to help reduce adverse effects of each [3, 4]. Furthermore, the Chinese herbal medicines used in TCM have recently been recognized as an important source for novel drug development, including anticancer drugs [5]. Therefore, western medicine practitioners and researchers are, now more than ever, open to exploring the potential of TCM to enhance conventional treatment of cancer patients [6].
The concept of ZHENG occupies an important position in the TCM system and is key to recognizing a patient's disease state and developing an effective, individualized treatment strategy. ZHENG is a kind of pathology of the disease development of a body in a certain stage, including the disease wherefrom, the cause, the feature, and the conflicts between healthy energy and evils. It reflects the nature of pathological change at a certain stage and reveals the intrinsic quality of disease more completely, profoundly, and accurately than symptoms. Therefore, the diagnosis of TCM ZHENG is to differentiate a disease by analyzing and synthesizing the information, symptoms, and patients' physical status collected through four types of diagnostic methods: inspection, auscultation and olfaction, inquiry, and palpation. According to the combination of diagnostic methods used, different types of ZHENG are possible for a single disease, and all may be equally effective. This feature provides flexibility and ready diversification to the disease-targeting therapy, allowing for the treating clinician to take advantage of the patient's personality and mental and spiritual desires to achieve high rates of compliance and completion. Therefore, TCM ZHENG differentiation must also be applied to the new TCM efforts being used in cancer patients worldwide.
The purpose of this study was to identify the clinical usage of ZHENG TCM in Chinese cancer patients by systematically searching the relevant Chinese-language medical and scientific literature collections. After analyzing the clinical distribution, the molecular basis underlying TCM ZHENG was considered in an attempt to better understand its usefulness in future clinical practice.
2. Literature Search for Publications on TCM ZHENG in Chinese Cancer Patients
We searched the four major electronic databases of Chinese-language medical and scientific literature (China National Knowledge Infrastructure (CNKI), Chinese Scientific Journal Database (VIP), Wanfang Database, and Chinese BioMedical Literature Database (CBM)) for publications between 2000 and 2011 that were related to “Zhong Yi” (traditional Chinese medicine), “ZHENG,” and “Ai” (cancer). More than 20,000 papers on TCM ZHENG in cancer were initially identified and included clinical observations, individual or small-scale case reports, large-scale clinical experiences, and experimental animal studies.
3. Investigation of TCM ZHENG in Cancer Patients by Publication Year and Cancer Type
As shown in Figure 1, there was a dramatic increase in the number of annual publications of TCM ZHENG in cancer patients during the past ten years. Among these articles, 32.2% (700 out of 2175) were related to lung cancer, 22.9% to liver cancer, 19.4% to gastric cancer, 12.1% to breast cancer, 5.9% to colon cancer, 1.7% to pancreatic cancer, and 10.3% to a variety of other types of cancer. This cancer type distribution is consistent with the incidence of cancers in China. It has been reported that the four most frequently diagnosed cancers in Chinese men over the past ten years involved lung, stomach, liver, and colon; Chinese women, however, were most frequently diagnosed with cancers of the breast, lung, stomach, and colon. The incidence of pancreatic cancer in Chinese men and women ranked 8th and 9th, respectively, but produced high mortality (nearly equal to incidence) in both sexes. This result suggests that TCM has been widely applied, as at least one form of treatment, for Chinese cancer patients in modern medical practice. Furthermore, the practice of TCM ZHENG in cancer patients has increased steadily over the past decade.
Figure 1.
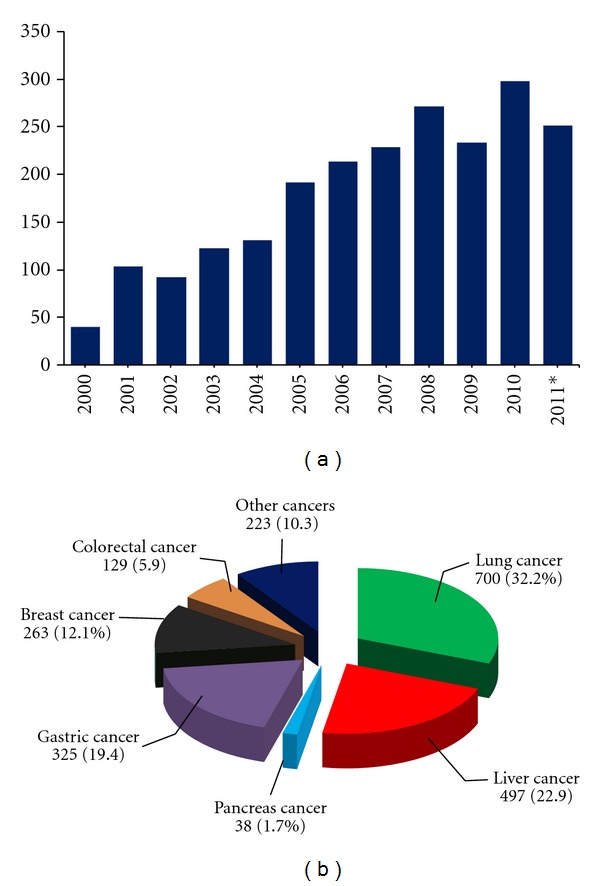
Annual publications on TCM ZHENG in cancer. (a) A total of 2175 papers were retrieved by searching the terms “Zhong Yi” (traditional Chinese medicine), “ZHENG,” and “Ai” (cancer) through the main Chinese electronic databases, including China National Knowledge Infrastructure (CNKI), Chinese Scientific Journal Database (VIP), Wanfang Database, and Chinese BioMedical Literature Database (CBM), and then analyzed by calculating the annual publications from January 1, 2000 to November 13, 2011. (b) The distributions of cancer types among all the publications. *To November 13, 2011.
4. Clinical Distributions of TCM ZHENG in Chinese Patients with Common Cancers
The six most common types of cancer reported in the studies included in this summary analysis were lung, liver, gastric, breast, colorectal, and pancreatic—collectively accounting for 89.7% of all the publications. We attempted to systematically identify and analyze the clinical ZHENG distribution in these six types of cancer. We searched the collection of initially identified relevant studies to identify clinical trials and case series that provided information on ≥10 cases with ZHENG description. A total of 144 articles were selected for clinical distribution analysis. The annual distribution frequencies of TCM ZHENG for each type of cancer were calculated. The cancer types with ZHENG frequency over 10% are presented in Figure 2.
Figure 2.
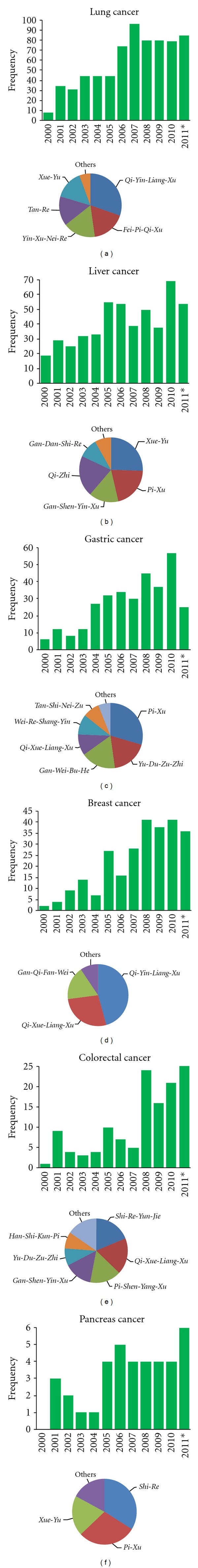
Clinical distributions of TCM ZHENG in common cancers. Annual publications for each common cancer were calculated and presented as a histogram. Publications involved with clinical trials and case series, where information on more than 10 cases with ZHENG description was available, were further selected. Thirty-two articles reported on lung cancer, 26 on liver cancer, 19 on gastric cancer, 21 on breast cancer, 29 on colorectal cancer, and 17 on pancreatic cancer. Finally, for each type of cancer, the distribution frequency of ZHENG was calculated and presented in pie chart. Note: Qi-Yin-Liang-Xu, deficiency of both Qi and Yin; Fei-Pi-Qi-Xu, lung-spleen Qi deficiency; Yin-Xu-Nei-Re, Yin asthenia and internal heat; Tan-Re, phlegm-heat; Xue-Yu, blood stasis; Pi-Xu, spleen deficiency; Gan-Shen-Yin-Xu, liver-kidney Yin deficiency; Qi-Zhi, Qi stagnation; Gan-Dan-Shi-Re, liver-gallbladder dampness-heat; Yu-Du-Zu-Zhi, stagnation of blood stasis and toxin; Gan-Wei-Bu-He, liver-stomach disharmony; Qi-Xue-Liang-Xu, deficiency of both Qi and blood; Yin-Xu-Nei-Re, Yin deficiency due to stomach heat; Tan-Shi-Nei-Zu, stagnation of phlegm-dampness; Gan-Qi-Fan-Wei, liver Qi invading stomach; Shi-Re-Yun-Jie, stagnation of dampness-heat; Pi-Shen-Yang-Xu, asthenic splenonephro-yang; Yu-Du-Nei-Zu, stagnation of blood stasis and toxin; Han-Shi-Kun-Pi, cold-dampness disturbing spleen.
The number of publications describing TCM ZHENG in lung cancer increased dramatically from the year 2000 (n = 8, in total) to the end of 2011 (n = 85, in total). Among these publications, 32 reported results from clinical trials or case series with ZHENG-based TCM. Summary analysis indicated that Qi-Yin-Liang-Xu, Fei-Pi-Qi-Xu, Yin-Xu-Nei-Re, Qi-Zhi-Xue-Yu, and Tan-Re were the most common ZHENGs in lung cancer (Figure 2). The number of publications describing TCM ZHENG in other types of cancer (liver, gastric, breast, colorectal, and pancreas) also increased dramatically over the past decade. As shown in Figure 2, by the end of 2011, a total of 26 articles had reported data on TCM ZHENG in liver cancer, 19 on gastric cancer, 21 on breast cancer, 29 on colorectal cancer, and 17 on pancreatic cancer. The frequency distribution of ZHENG for each of these types of cancer was calculated. The results indicated that the main ZHENGs for liver cancer were Xue-Yu, Pi-Xu, Gan-Shen-Yin-Xu, Qi-Zhi, and Gan-Dan-Shi-Re, which accounted for 94.3% of the total. The main ZHENGs for gastric cancer were Pi-Xu, Yu-Du-Zu-Zhi, Gan-Wei-Bu-He, Qi-Xue-Liang-Xu, Tan-Shi, and Wei-Re-Shang-Yin, which accounted for 93.9% of the total. The main ZHENGs for breast cancer were Qi-Yin-Liang-Xu, Qi-Xue-Liang-Xu, and Gan-Qi-Fan-Wei, which accounted for 90.5% of the total. The main ZHENGs for colorectal cancer were Shi-Re-Yun-Jie, Qi-Xue-Liang-Xu, Pi-Shen-Yang-Xu, Yu-Du-Zu-Zhi, Gan-Shen-Yin-Xu, and Han-Shi-Kun-Pi, which accounted for 84.5% of the total. The main ZHENGs for pancreatic cancer were Shi-Re, Pi-Xu, and Xue-Yu, which accounted for 82.8% of the total.
5. The Molecular Basis for Common ZHENGs in Cancer
5.1. Xue-Yu ZHENG (Blood Stasis)
Xue-Yu ZHENG is one of the common syndromes in TCM, characterized by cyanosis (of skin, lips, nails, and/or tongue), ecchymosis and petechia, and irregular pulse (detected by palpation as thin, unsmooth, deep, taut, knotted, slow, or intermittent). In addition, other common clinical signs include blackish complexion, dry skin, and purpura. The Xue-Yu status was recently shown to be related with changes of hemorheological properties, such as high-blood viscosity, increased erythrocyte aggregation, increased blood sedimentation, decreased erythrocyte deformability, and decreased hematocrit [7].
Xue-Yu is associated with many diseases, including cancer. Epidemiological investigation has revealed that Xue-Yu is one of the most prominent ZHENGs in patients with cancer, especially for those with liver, lung, and pancreatic cancer; the results from our summary analysis agreed with this reported pattern (Figure 2). TCM treatment of cancer patients with Xue-Yu using traditional Chinese herbs has shown satisfactory efficacy in clinical practice in China. Since 1990, several retrospective clinical studies have reported strong statistical correlation between tumor metastasis and Xue-Yu ZHENG; treating or controlling tumor metastasis, while Huo-Xue-Hua-Yu (promoting blood circulation and removing blood stasis) has been advocated as a potential therapeutic approach [8, 9]. There are several reasons accounting for this theory. One is that cancer patients usually show Xue-Yu ZHENG. For example, patients with liver cancer usually exhibit bluish tendon on abdomen, scaly skin, a darkened complexion on the face, a hump below the costal region, and a purple-colored tongue and complain of a localized pricking pain in the region corresponding to the liver [10]. These symptoms are indicators of Gan-Xue-Yu (blood stasis in the Gan) and should be treated with the aim of Huo-Xue-Hua-Yu (as described above). Another reason is that cancer patients with Xue-Yu ZHENG usually present with microcirculation disturbance [11]. For example, Liu et al. observed that lung cancer patients with Xue-Yu ZHENG had significantly higher fibrinogen content than their counterparts without Xue-Yu ZHENG; moreover, the increased fibrinogen was found to be correlated with increased metastasis [8]. Another observational study from 105 patients with liver cancer demonstrated that the presence of Xue-Yu ZHENG was associated with a worse prognosis; it was unclear whether treatment for Huo-Xue-Hua-Yu in these patients significantly affected patient survival [12]. The third reason is that a tumor-mediated hypercoagulable state may exist and functionally complicate the disease state. The tumor-mediated hypercoagulable state is known to promote expression of tissue factor (TF) on the surfaces of tumor cells and macrophages, cell surface phospholipids that support coagulation activation, other tumor-mediated factors that trigger platelet activation and support accumulation, and tumor-induced endothelial cell factors that activate coagulation [13]. Furthermore, recently published preclinical data has suggested that activation of coagulation can promote tumor growth and angiogenesis. Since clinical hypercoagulable status is associated with adverse cancer prognosis, treatment with anticoagulation agents may prolong survival in certain types of cancer [14].
Even though a definitive link between cancer and Xue-Yu ZHENG has not yet been identified, some studies have shown evidence that Huo-Xue-Hua-Yu treatment may promote cancer metastasis. A prospective randomized controlled trial in 60 nasopharyngeal carcinoma cases conducted by Han et al. showed that integrated Huo-Xue-Hua-Yu herbs treatment with radiotherapy in nasopharyngeal carcinoma patients was associated with a 2.67-fold increase in distant metastasis, as compared to patients receiving radiotherapy alone [15]. In addition, preclinical studies showed that some Huo-Xue-Hua-Yu medicines, such as Danshen (Red-rooted salvia root), Chishao (Red paeony root), Danggui (Chinese angelica), Honghua (Indian azalea leaf), Jixueteng (Suberect spatholobus stem), Awei (Chinese asafoetida), and Chuanxiong (Szechuan lovage rhizome), could promote lung metastasis in liver cancer xenografted mouse models [16]. Our group previously established a xenograft tumor mouse model with Xue-Yu ZHENG to evaluate the effect of Xue-Yu ZHENG on tumor metastasis. We found that mice with the Xue-Yu ZHENG developed less metastasis than their counterparts without Xue-Yu [17–20]. However, when the tumor-bearing mice with Xue-Yu ZHENG were treated with individual Huo-Xue-Hua-Yu herbs, such as Danshen (Red-rooted salvia root) and Shensanqi (Sanchi), we found that Shensanqi treatment suppressed liver metastasis [19, 20] while Danshen treatment promoted liver metastasis [19]. Therefore, the correlation between ZHENG and cancer cells needs to be further studied in order to gain a more comprehensive understanding of its effects on the complex processes of tumor growth and metastasis.
5.2. Shi-Re ZHENG (Dampness-Heat)
Shi-Re ZHENG is caused by dysfunction of the Pi (“spleen”) and Wei (“stomach”) due to retention of dampness and heat in the body. The occurrence of Shi-Re is usually based on water and wetness. The water and wetness can change into heat if they are stored in the body for long periods, and the combination of water and wetness and heat may cause Shi-Re ZHENG. Shi-Re is characterized by epigastric or abdominal oppression, lack of appetite, heavy body weight, thirst with little/no desire to drink, abdominal pain, loose stools, nausea, vomiting, fever, headache, red tongue body with a yellow sticky coat, and/or slippery rapid pulse.
Shi-Re ZHENG has been associated with many diseases, especially those involving the gastrointestinal (GI) tract. The potential molecular basis of Shi-Re ZHENG has attracted much research attention, although it is far from clear. Recently, Shi-Re ZHENG has been implicated in a broad range of inflammatory conditions, including eczema, psoriasis, cystitis, urethritis, gastroenteritis, vaginitis, cervicitis, meningitis, conjunctivitis, rheumatoid arthritis, and allergic reactions [21–25]. In addition, Shi-Re ZHENG was found to correlate with changes in expression of inflammation cytokines. For example, Liu and Wang showed that the serum levels of tumor necrosis factor-α (TNF-α) and interleukin-13 were significantly higher in rats with ulcerative colitis complicated with Shi-Re ZHENG, as compared with those without Shi-Re [26]. Likewise, Jiang et al. observed that in a total of 63 patients with chronic hepatitis B, 27 cases were diagnosed with Shi-Re ZHENG, and patients with Shi-Re had higher levels of TNF-α and tissue inhibitor of metalloproteinases (TIMP)-1 [27].
It has been reported that symptoms of Shi-Re ZHENG are commonly seen in patients with GI cancer, including cancers of the duodenum, colon, liver, pancreas, and gallbladder. Just as we have shown in Figure 2, Shi-Re has been reported as one of the most common ZHENGs in liver, colorectal, and pancreatic cancers. However, there is still not a clear understanding of the biological validity of Shi-Re and the possible mechanisms of ZHENG in cancer. Our research group has previously established a pancreatic cancer xenograft mouse model with Shi-Re ZHENG [28]. We found that Shi-Re ZHENG mice exhibited altered cancer-associated myofibroblast (CAF) proliferative activities and tumor-associated macrophage (TAM) infiltration, which led to altered levels of CAF- and TAM-derived secreted cytokines (such as, SDF-1, VEGF, TGF-1β, IL-6, CCL3, CCL4, CCL5, TNF-α, IL-8, and bFGF). The presence of Shi-Re ZHENG has also been shown to impact tumor growth. Chinese herbs for Qing-Re-Hua-Shi (removing heat and dampness) were found to inhibit cancer cell proliferation through modification of the components of the tumor microenvironment [28–30]. These findings suggested that Shi-Re is associated with altered tumor microenvironment (Figure 3).
Figure 3.
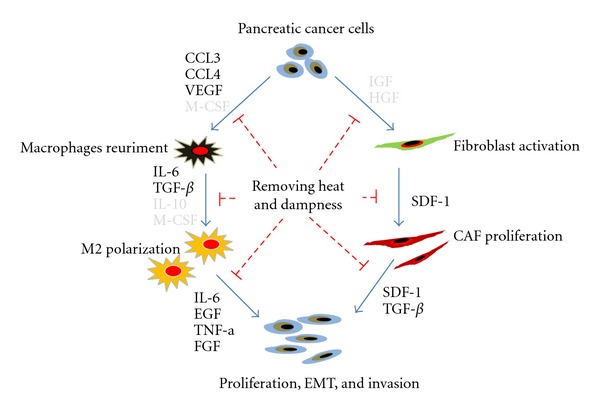
A schematic cartoon portraying the molecular basis of Shi-Re ZHENG in pancreatic cancer, based on our previous studies. It has been proposed that tumors with Shi-Re ZHENG exhibited altered cancer-associated myofibroblast (CAF) proliferative activities and tumor-associated macrophage (TAM) infiltration, which led to altered levels of CAF- and TAM-derived secreted cytokines (such as SDF-1, VEGF, TGF-1β, IL-6, CCL3, CCL4, CCL5, TNF-α, IL-8, and bFGF). The presence of Shi-Re ZHENG has impact on tumor growth. Chinese herbs for Qing-Re-Hua-Shi (removing heat and dampness) inhibited cancer cell proliferation, invasion, and in vivo metastasis through modification of the tumor microenvironment. Cytokines that are marked in bold have been confirmed by our previous studies.
5.3. Yin-Xu ZHENG (Yin Deficiency)
Yin-Xu represents insufficiency of body fluid. It is characterized by dryness in the throat and/or mouth, perspiration during sleep, tinnitus, dizziness, fatigue, insomnia, red tongue body with no coating on, and pulse that is thin, fine, or floating and empty. Yin-Xu may occur in many organs, including the stomach, lung, liver, kidney, or heart. Symptoms of Yin-Xu ZHENG are commonly seen in cancers of the liver, lung, breast, stomach, and colon (Figure 2). However, only a few publications in the literature have studied the molecular basis of Yin-Xu. Shen et al. observed that in patiens with lung cancer, Yin-Xu was correlated with changes in the cytokine expression profile [31–34]. They also showed that lung cancer tissue with Yin-Xu ZHENG exhibited dysregulated expression of TNF-α, IL-lα, IFN, IL-2, IL-8, and IL-1Rα, as compared with that without Yin-Xu ZHENG. Thus, the molecular basis of Yin-Xu ZHENG is believed to involve components of the inflammatory cytokines network.
5.4. Pi-Xu (Spleen Deficiency)
For this ZHENG, the word “spleen” does not refer to the organ, as in western medicine. It is a term used to describe an entire group of physiological functions. Based on the so-called Pi-Wei theory (also called spleen-stomach theory), the Pi (“spleen”) governs molecular transport and transformation since the Pi transforms food into nutrients, which are the sources of Qi and blood, and distributes the nutrients to the limbs and other organs. Hence, the theory of “Pi being acquired foundation” has emerged. This theory postulates that when there is Pi-Xu, the digestion process is perturbed, causing abdominal discomfort and making the person feel tired.Since the Pi would normally keep the body fluids flowing in their respective pathways, signs of Pi-Xu ZHENG are hemorrhage, swelling, and bruising.
Pi-Xu has been shown to be involved with dysfunction of the vegetative nervous system of the GI tract, immune pathways, and endocrine processes. It can also mediate the distribution and content of fecal bacteria flora and gut-associated microbiota, including ulcer- and inflammation-causing Helicobacter pylori, as well as trace elements involved in blood and muscle metabolism [35]. Patients with different cancer types, in addition to the GI type, may present with Pi-Xu at various stages of the disease. Because many if not all cancers share at least some pathophysiological features, it is possible that they may be treated by an intervention approach based on a single principle but with flexibility to allow emphasis on different aspects of the disease in different patients.
Extensive research has been carried out to determine the molecular basis of Pi-Xu in cancer. Since the 1960s, a group led by Yu Erxin has performed a series of investigations in liver cancer patients to investigate the potential molecular components of Pi-Xu [36, 37]. These efforts have identified a correlation between Pi-Xu and immunological dysfunction [38]. Liver cancer xenograft mice with Pi-Xu were shown to have significantly less total T cells and T helper (Th) cell lymphocytes, but more inhibitory T cells, than their counterparts without Pi-Xu. Furthermore, when these Pi-Xu mice were treated with Dangshen (Pilose asiabell root) and Huangqi (Pilose asiabell root) combination therapy, the level of Th cell-expressed CD4 was elevated significantly. Thus, it is believed that Pi-fortifying prescriptions may enhance proliferation of splenic cells and significantly increase auto-antibody secretory cell number, thereby enhancing the cytotoxic action of lymphocytes. Indeed, it has been shown that administration of Pi-fortifying therapy to ConA-stimulated mice promotes splenic cells to secrete cytokines, such as IL-2 [38]. Likewise, clinical observation in patents with liver cancer showed that patients with Pi-Xu were treated with Pi-fortifying therapy the activities of both natural killer cells and lymphokine-activated killer cells were restored [39].
Pi-Xu has been correlated with the abnormal energy metabolism that occurs in tumor cells. Observational study from 40 cased with liver cancer showed that liver cancer patients with Pi-Xu exhibited decreased serum levels of cyclic adenosine monophosphate (cAMP), while those patients with Shi-Re or Xue-Yu showed no significant changes in cAMP level [40]. Liver cancer xenograft mice with Pi-Xu also showed decreased serum and splenic cAMP levels, and increased cGMP and cAMP/cGMP ratio; intriguingly, the condition was not improved or resolved by treatment with the Pi-fortifying prescriptions [41]. These findings were also observed in patients with gastric cancer [42]. In addition to its effects on immune-related mechanisms and energic metabolism, the Pi-fortifying prescriptions was also shown to mediate the patterns of trace elements [43, 44]. Patients with various chronic diseases and Pi-Xu present with altered expression and distribution patterns of trace elements, including Cu, Zn, and Fe [45]. In gastric cancer patients with Pi-Xu, the levels of Cu and Zn are significantly changed, in particular [46]. Therefore, Pi-Xu is a now considered as a multisystem functional impairment.
6. Prospects and Challenges
In TCM, the medicines are prescribed according to ZHENG, and ZHENG remains the essence of TCM treatment. However, there are some important issues that deserve mentioning. First, as TCM ZHENG differentiation is usually based upon the treating physician's intuition and personal experience, results differ from physician to physician and from clinic to clinic. Thus, ZHENG differentiation has a low reproducibility. To date, no unified criteria have been published for ZHENG differentiation, and it remains one of the main obstacles to widespread application of TCM in the clinical and research settings. Second, in this summary analysis, we emphasized the important position of ZHENG since it helps to guide the design of an individual's treatment regimen. We believe that the results of this study may help provide a theoretical basis for clinical diagnosis and treatment. However, we also recognize that when used as the sole treatment for cancer, TCM ZHENG does not consistently produce satisfactory therapeutic efficacy. Recently, there has been much interest in the potential clinical utility of “analogous ZHENG existing in the same disease” for improving TCM in clinical practice [47], especially for cancer patients. Thus, a strategy combining ZHENG differentiation and disease diagnosis is considered promising for future cancer treatment.
While much research has attempted to elucidate the molecular basis of the cancer-associated ZHENGs, the available data are subject to several limitations that must be considered when contemplating the utility of TCM ZHENG as a cancer therapy. First, TCM is focused on alleviating a particular disease or condition, while the ZHENG is based on systemic and holistic concepts. Therefore, a system's biology approach may be the optimal way to research the clinical utility and therapeutic efficacy of TCM ZHENG. Second, TCM is practiced with respect to the rules of “treating the same disease with different methods” and “treating different diseases with the same methods”. In our summary analysis, we found the same molecular basis underlying the same ZHENG in different diseases. However, we should also emphasize that molecular differences that are disease- or diagnosis-specific, while sharing a ZHENG, may prove particularly important in designing effective individualized treatment regimens. This notion is consistent with the current understanding that combination of ZHENG differentiation and disease diagnosis yields improved treatment efficacy. Third, we point out that a comprehensive profile of ZHENG-specific molecules has yet to be identified, and the correlation between ZHENG and molecules has yet to be firmly established. Finally, it is important to remember that ZHENG is now considered as a multisystem and multiorgan functional impairment. Although modern technologies have been applied to ZHENG research, we are far from obtaining a clear understanding of the exact molecular basis of ZHENG. We are hopeful that future integration of modern technologies and continued research may eventually promote ZHENG research.
7. Conclusions
In this study, we systematically identified the collected body of research on TCM ZHENG in cancer patients. The sources of these data were the publically available Chinese language scientific and medical literature databases. We first summarized the clinical ZHENG distribution among six common cancer types, including lung, liver, gastric, breast, colorectal, and pancreatic, which may help to provide a theoretical basis for TCM as a clinical cancer treatment. We then considered the molecular basis of Xue-Yu, Shi-Re, Yin-Xu, and Pi-Xu ZHENGs that are commonly present in different types of cancer, which may contribute to a better understanding of the potential of TCM ZHENG for supplementing modern therapeutic strategies for cancer.
Acknowledgments
This study was supported by National Science Foundation of China (81001061); Shanghai Nature Science Fund, Shanghai, China (09ZR1406800); Doctoral Programs Foundation of Ministry of Education of China (20090071120076); Shanghai Science and Technology Committee Rising-Star Program (11QA1401300); Medical Talents Training Program of Health Bureau of Shanghai (XYQ2011008); Shanghai Municipal Health Bureau Grant (KY148).
References
- 1.Chen Z, Gu K, Zheng Y, Zheng W, Lu W, Shu XO. The use of complementary and alternative medicine among Chinese women with breast cancer. Journal of Alternative and Complementary Medicine. 2008;14(8):1049–1055. doi: 10.1089/acm.2008.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang KH, Brodie R, Choong MA, Sweeney KJ, Kerin MJ. Complementary and alternative medicine use in oncology: a questionnaire survey of patients and health care professionals. BMC Cancer. 2011;11, article 196 doi: 10.1186/1471-2407-11-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCulloch M, See C, Shu XJ, et al. Astragalus-based Chinese herbs and platinum-based chemotherapy for advanced non-small-cell lung cancer: meta-analysis of randomized trials. Journal of Clinical Oncology. 2006;24(3):419–430. doi: 10.1200/JCO.2005.03.6392. [DOI] [PubMed] [Google Scholar]
- 4.Pan CX, Morrison RS, Ness J, Fugh-Berman A, Leipzig RM. Complementary and alternative medicine in the management of pain, dyspnea, and nausea and vomiting near the end of life: a systematic review. Journal of Pain and Symptom Management. 2000;20(5):374–387. doi: 10.1016/s0885-3924(00)00190-1. [DOI] [PubMed] [Google Scholar]
- 5.Efferth T, Li PC, Konkimalla VS, Kaina B. From traditional Chinese medicine to rational cancer therapy. Trends in Molecular Medicine. 2007;13(8):353–361. doi: 10.1016/j.molmed.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Liu J, Li X, Ma L, Fonnebo V. Traditional Chinese medicine in cancer care: a review of case reports published in Chinese literature. Forsch Komplementmed. 2011;18(5):257–263. doi: 10.1159/000333065. [DOI] [PubMed] [Google Scholar]
- 7.Zhang CF. Exploring of blood viscosity in cancer patients. China Joumal of ModelTI Medicine. 2004;14(7):73–75. [Google Scholar]
- 8.Liu YH, Zhang YW, Liang GG, Yang KQ. Experimental and clinical study on tumor metastasis and microscopic blood stasis. Xian Dai Zhong Yi. 1996;4(33):224–228. [Google Scholar]
- 9.Chen YF, Zhang SH. Promoting blood circulation and Removing blood stasis in cancer treatment. Journal of Shanxi College of Traditional Chinese Medicine. 2006;29(2):62–63. [Google Scholar]
- 10.Wu YF. Correlation factors analysis on hepatic blood stagnation type of primary liver cancer. Shanxi Journal of Traditional Chinese Medicine. 2007;23(1):63–65. [Google Scholar]
- 11.Yang WH, Liu LM, Zhao HS, Wu LC. Microcirculation analysis in liver cancer with blood stasis. Chinese Journal of Integrated Traditional and Western Medicine on Liver Diseases. 1999;9(6):10–11. [Google Scholar]
- 12.Chen XZ, Tian HQ, Huang XQ, Liang GW, Huang ZQ. Effect of Ganji formula on blood stasis in patients with advanced liver cancer. Shan Xi Zhong Yi. 2005;26(9):891–893. [Google Scholar]
- 13.Mousa SA. Anticoagulants in thrombosis and cancer: the missing link. Expert Review of Anticancer Therapy. 2002;2(2):227–233. doi: 10.1586/14737140.2.2.227. [DOI] [PubMed] [Google Scholar]
- 14.Ahmad S, Ansari AA. Therapeutic roles of heparin anticoagulants in cancer and related disorders. Medicinal Chemistry. 2011;7(5):504–517. doi: 10.2174/157340611796799104. [DOI] [PubMed] [Google Scholar]
- 15.Han JQ, Chen YT, Man YY. Clinical study on effect of combined treatment of fuchunpian with radiotherapy on nasopharyngeal carcinoma. Zhongguo Zhong Xi Yi Jie He Za Zhi. 1995;15(12):710–712. [PubMed] [Google Scholar]
- 16.Li XT, Wang YQ, Fu NW. Effects of herbs for promoting blood circulation and removing blood stasis on lung metastasis in liver cancer xenografted mice. Journal of Traditional Chinese Medicine. 1980;21(8):p. 75. [Google Scholar]
- 17.Chen Z, Liu LM, He YB. Correlation between TXB2, 6-Keto-PGF1alpha and liver metastasis in rats model with blood stasis. Zhong Xi Yi Jie He Xue Bao. 2003;1(3):199–201. doi: 10.3736/jcim20030316. [DOI] [PubMed] [Google Scholar]
- 18.Chen Z, Liu LM, He YB. Effects of blood stasis on W256 tumor growth and liver metastasis. Chinese Archives of Traditonal Chinese Medicine. 2003;21(6):866–872. [Google Scholar]
- 19.Chen PF, Liu LM, Chen Z, Xu YF, Xie CS. Study on blood stasis of liver metastasis of cancer and the intervention of shen sanqi and danshen. Journal of Zhejiang Chinese Medical University. 2007;31(5):552–553. [Google Scholar]
- 20.Chen PF, Liu LM, Chen Z, Lin SY, Song WX, Xu YF. Effects of ethanol extracts of Panax notoginseng on liver metastasis of B16 melanoma grafted in mice. Zhong Xi Yi Jie He Xue Bao. 2006;4(5):500–503. doi: 10.3736/jcim20060512. [DOI] [PubMed] [Google Scholar]
- 21.Zheng XB, Liu HB, Feng YL, Dai SX. Huangqin decoction lowers the number of mast cells in ulcerative colitis in rats with dampness and heat syndrome. Nan Fang Yi Ke Da Xue Xue Bao. 2011;31(2):252–255. [PubMed] [Google Scholar]
- 22.Yuan JL, Zhang H, Wang L, et al. Biochemical characteristics of traditional Chinese medicine syndromes and their elements in patients with hepatitis B cirrhosis. Zhong Xi Yi Jie He Xue Bao. 2011;9(4):374–381. doi: 10.3736/jcim20110405. [DOI] [PubMed] [Google Scholar]
- 23.Zheng XB, Feng YL, Liu HB, Dai SX. Effect of huangqin decoction on CD4+T Cell and its co-stimulator factors for unlcerative colitis rat with damp-and-heat syndrome. Chinese Journal of Experimental Traditional Medical Formulae. 2011;17(1):169–172. [Google Scholar]
- 24.Cui NJ, Hu L, Lao SX. Relationship between Pi-Wei damp-heat syndrome with expressions of nuclear factor-kappaBmRNA and heat shock protein 70 mRNA in patients with chronic gastritis. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2010;30(1):18–21. [PubMed] [Google Scholar]
- 25.Li XH, Xie GQ. The correlation study between damp-heat syndrome and pro-inflammatory cytokines in primary nephrotic syndrome. Liaoning Journal of Traditional Chinese Medicine. 2011;38(6):1096–1098. [Google Scholar]
- 26.Liu W, Wang YZ. Effects of Reyusan on serum levels of tumor necrosis factor-a and Interleukin-13 in rats with ulcerative colitis complicated with damp-heat syndrome of stomach and intestine. Journal of Anhui TCM college. 2010;29(6):56–58. [Google Scholar]
- 27.Jiang KP, Tao Y, Hu HT, et al. A clinical study on the serum levels of TGF-b1 and TIMP-1 in patients with chronic B hepatitis in TCM types damp-heat. Chinese Journal of Integrated Traditional and Western Medicine on Liver Diseases. 2007;17(5):264–265. [Google Scholar]
- 28.Dai HY, Wang P, Feng LY, et al. The molecular mechanisms of traditional Chinese medicine ZHENG syndromes on pancreatic tumor growth. Integrative Cancer Therapies. 2010;9(3):291–297. doi: 10.1177/1534735410373922. [DOI] [PubMed] [Google Scholar]
- 29.Ouyang HQ, Liu LM, Chen Z, Luo JM, Yu EX. Effects of Qingyi Huaji decoction on serum levels of interleukin-6, interleukin-8 and tumor necrosis factor-α in nude mice bearing pancreatic tumors. Zhong Xi Yi Jie He Xue Bao. 2010;8(7):655–661. doi: 10.3736/jcim20100709. [DOI] [PubMed] [Google Scholar]
- 30.Yin JH, Shi WD, Zhu XY, Chen Z, Liu LM. Qingyihuaji formula inhibits progress of liver metastases from advanced pancreatic cancer xenograft by targeting to decrease expression of Cyr61 and VEGF. Integrative Cancer Therapies. 2012;11(1):37–47. doi: 10.1177/1534735411400315. [DOI] [PubMed] [Google Scholar]
- 31.Shen WX, Sun Y, Zhang SR. Study on relation between IL-1a, Il-1b, IL-1Ra gene mRNA expression and Yin-deficiency syndrome in lung cancer. Bulletin of Medical Research. 2000;29(8):5–7. [Google Scholar]
- 32.Zheng H, Shen WX, Liu XY, et al. An experimental study of the gene expression profile of cytokines in Yin deficiency syndrome of different diseases. Journal of Basic and Clinical Oncology. 2006;19(6):448–450. [Google Scholar]
- 33.Liu XY, Shen WX, Liu YM, et al. Inflammatory cytokines profile in lung cancer with Yin-deficiency syndrome. Yi Xue Yan Jiu Za Zhi. 2006;35(3):75–76. [Google Scholar]
- 34.Shen WX, Sun Y, Zhang SR. Correlation between IL-8, Il-10 and Yin-deficiency syndrome. Bulletin of Medical Research. 2003;32(5):62–64. [Google Scholar]
- 35.Wu XN. Current concept of Spleen-Stomach theory and Spleen deficiency syndrome in TCM. World Journal of Gastroenterology. 1998;4(1):2–6. doi: 10.3748/wjg.v4.i1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yu EX, Lv LN. clinical and molecular mechanism of Spleen-nourishing and Qi-regulating therapy for liver cancer. Journal of Traditional Chinese Medicine. 1987;43(7):28–30. [Google Scholar]
- 37.Wang P, Huang WX, Liu LM. Overview of clinical and experimental study on Spleen-nourishing and Qi-regulating therapy for liver cancer. Shanghai Journal of Traditional Chinese Medicine. 2005;39(5):60–62. [Google Scholar]
- 38.Yu EX, Lv LN, Wang QD. Effects of Spleen-nourish ing and Qi-regulating herbs on immunofunction of liver tumor xenografted mice with Spleen-deficiency. Tumor. 1983;3(4):168–170. [Google Scholar]
- 39.Huang HY, Yu EX. Effect of Spleen-nourish ing herbs on NK and LAK cells and IL-2 activities. Zhongguo Zhong Xi Yi Jie He Za Zhi. 1993;13(4):253–255. [PubMed] [Google Scholar]
- 40.Song MZ, Yu EX. Serum cAMP levels in liver cancer with different TCM syndromes. Shanghai Journal of Traditional Chinese Medicine. 1981;23(4):40–43. [Google Scholar]
- 41.Zhang SL, Yin GS, Wang GX, Li E. Effects of Spleen-nourishing decoction on plasma and spleenic cAMP levels in rats. Zhong Xi Yi Jie He Za Zhi. 1990;10(11):672–674. [PubMed] [Google Scholar]
- 42.Yin GY. A study of the relation of intestinal metaplasia, gastric carcinoma and the Spleen deficiency syndrome using histochemical staining of the gastric mucosa and determination of cAMP and cGMP. Zhong Xi Yi Jie He Za Zhi. 1986;6(7):395–397. [PubMed] [Google Scholar]
- 43.Wang J, Zhang ML, Qiu XF. The efect of Spleen-reinforcing therapy on the transporting and distribution Of 59Fe metablism of Spleen-deficiency-sufering mice in the organs. Journal of Hubei College of TCM. 2007;9(3):20–22. [Google Scholar]
- 44.Ma JW, Hao G, Li J. Serum level of Zn, Cu and Mg in patients with Spleen deficiency. Zhejiang Journal of Traditional Chinese Medicine. 1990;25(10):p. 471. [Google Scholar]
- 45.Dong GM. Changes of trace elements in gastric juice in peptic ulcer patients with Spleen deficiency syndrome. Shi Yong Zhong Xi Yi Jie He Za Zhi. 1995;8(2):68–69. [Google Scholar]
- 46.Yin GZ, Xu XZ. Correlation between gastric mucosa Zn, cAMP, DNA and 3H-TdRLCT in gastric carcinoma with Spleen deficiency. Jiang Su Yi Yao. 1989;16(8):408–412. [Google Scholar]
- 47.Wang WJ. Pay more attention to ‘Analogous syndrome complex in the same disease and treating the same disease with analogous methods ’. Zhong Xi Yi Jie He Xue Bao. 2008;6(5):441–445. doi: 10.3736/jcim20080501. [DOI] [PubMed] [Google Scholar]


