Abstract
Considerable progress has been made over the last decade in developing candidate preventive vaccines that can protect nonhuman primates against Ebola and Marburg viruses. A vaccine based on recombinant vesicular stomatitis virus (VSV) seems to be particularly robust as it can also confer protection when administered as a postexposure treatment. While filoviruses are not thought to be transmitted by aerosol in nature the inhalation route is among the most likely portals of entry in the setting of a bioterrorist event. At present, all candidate filoviral vaccines have been evaluated against parenteral challenges but none have been tested against an aerosol exposure. Here, we evaluated our recombinant VSV-based Zaire ebolavirus (ZEBOV) and Marburg virus (MARV) vaccines against aerosol challenge in cynomolgus macaques. All monkeys vaccinated with a VSV vector expressing the glycoprotein of ZEBOV were completely protected against an aerosol exposure of ZEBOV. Likewise, all monkeys vaccinated with a VSV vector expressing the glycoprotein of MARV were completely protected against an aerosol exposure of MARV. All control animals challenged by the aerosol route with either ZEBOV or MARV succumbed. Interestingly, disease in control animals appeared to progress slower than previously seen in macaques exposed to comparable doses by intramuscular injection.
Keywords: Ebola virus, Marburg virus, Filovirus, Nonhuman primates, Aerosol, Vaccines
1. Introduction
Members of the family Filoviridae, Ebola virus (EBOV) and Marburg virus (MARV), cause severe hemorrhagic fever (HF) in humans and nonhuman primates. The Marburgvirus genus contains a single species: Lake Victoria marburgvirus (LVMARV). The Ebolavirus genus is subdivided into four distinct species: Ivory Coast ebolavirus (ICEBOV) (also known as Cote d’Ivoire ebolavirus, CIEBOV), Reston ebolavirus (REBOV), Sudan ebolavirus (SEBOV), and Zaire ebolavirus (ZEBOV) [1,2]. MARV, ZEBOV, and SEBOV are important human pathogens with case fatality rates frequently ranging between 70% and nearly 90% for ZEBOV, around 50% for SEBOV, and up to 90% for MARV outbreaks depending on the strain of MARV (reviewed in Ref. [2]). Currently, there are no vaccines or postexposure treatment modalities available for preventing or managing filoviral infections. However, remarkable progress has been made over the last few years in developing candidate preventive vaccines that can completely protect nonhuman primates against EBOV and MARV [3–11]. Among the most promising vaccines is a system based on recombinant vesicular stomatitis virus (VSV) which not only can protect nonhuman primates against EBOV and MARV when used as a single injection preventive vaccine but astonishingly showed 50–100% efficacy when employed as a postexposure treatment [12–14].
Little is known regarding how filoviruses are maintained in nature. All human outbreaks to date have been traced to Central Africa [2]. EBOV has decimated populations of wild apes in this same region [15]; however, apes and other nonhuman primates that have been associated with filoviral outbreaks are reservoir-incompetent species and like humans are accidental hosts [16]. Recent work has shown that bats may serve as a reservoir species for filoviruses [17,18] but it remains unclear whether other species are involved or exactly how transmission to humans and/or apes occurs. Once an individual is exposed to EBOV or MARV person-to-person transmission occurs by direct contact with blood or bodily fluids (saliva, sweat, stool, urine, tears, and breast milk) of an infected patient during the acute phase of illness [2,19]. Care-givers both at home and in hospitals are among populations at greatest risk. While studies have shown that EBOV and MARV can be spread through airborne particles/aerosols under controlled laboratory conditions [20–23], this type of spread rarely occurs among humans in a hospital or household setting during outbreaks.
Despite the relatively low and localized global occurrence of cases and the fact that transmission in nature is primarily by contact exposure, the filoviruses may be exploitable as agents of bioterrorism since they are highly infectious by the aerosol route, produce high morbidity and mortality in primates, and can be readily propagated in vitro. Indeed, the filoviruses have been classified as Category A bioterrorism agents by the Centers for Disease Control and Prevention [24]. When planning defenses against biological warfare agents such as filoviruses, it is important to consider that the inhalation route is the most likely portal of entry for agents disseminated as aerosols [25]. Moreover, it is known that the former Soviet Union experimented with aerosolized EBOV and MARV [26,27]. However, all previous vaccine candidates have been evaluated against peripheral or intraperitoneal filovirus injections while no vaccine has been tested against an aerosol challenge in non-human primates. Here, we used cynomolgus macaque models of filoviral hemorrhagic HF to test the ability of our recombinant VSV-based ZEBOV and MARV vaccines to protect against homologous ZEBOV and MARV aerosol exposures, respectively.
2. Materials and methods
2.1. Vaccine vectors and viruses
The recombinant VSVs expressing either the glycoprotein (GP) of ZEBOV (VSVΔG/ZEBOVGP) or MARV (Musoke strain) (VSVΔG/MARVGP) were generated as described recently using the infectious clone for the VSV, Indiana serotype [28]. ZEBOV (strain Kikwit) was isolated from a patient of the ZEBOV outbreak in Kikwit in Ref. [29] while the Musoke strain of MARV was isolated from a human case in 1980 in Kenya [30].
2.2. Animal studies
Twelve healthy, filovirus-seronegative male cynomolgus macaques (Macaca fascicularis) (5–9 kg) were used for these studies. For the ZEBOV portion of this study, three animals were vaccinated by intramuscular (i.m.) injection with ~2 × 107 pfu of VSVΔG/ZEBOVGP (Subject 1, Subject 2, and Subject 3) and three animals were vaccinated i.m. with ~2 × 107 pfu of VSVΔG/MARVGP (Control 1, Control 2, and Control 3). The six cynomolgus macaques were challenged 28 days after the single dose vaccination by aerosol exposure to a target dose of 1000 pfu of ZEBOV. Before aerosol exposures a body plethysmograph was taken of each animal for 3 min to determine the animal’s respiratory capacity. Each macaque was then inserted into a Class III biological safety cabinet and exposed in a head-only aerosol chamber to a ZEBOV aerosol created by a Collison nebulizer controlled by an automated bioaerosol exposure system for 10 min as previously described [31,32]. For the MARV portion of this study, four animals were immunized i.m. with ~2 × 107 pfu of VSVΔG/MARVGP (Subject 4, Subject 5, Subject 6, and Subject 7) and two animals with ~2 × 107 pfu of VSVΔG/ZEBOVGP (Control 4 and Control 5). These six macaques were challenged 28 days after the single dose vaccination by aerosol exposure to 1000 pfu of MARV (Musoke strain) in the same manner as described above for ZEBOV.
Swab samples (oral, nasal, rectal) and/or blood were taken before vaccination (day –28) and at days 2 (day –26), 14 (day –14), and 27 (day –1) after vaccination and at days 3, 6, 10, 14, and 28 after the ZEBOV or MARV challenges. Animal studies were performed in BSL-4 biocontainment at USAMRIID and were approved by the USAMRIID Laboratory Animal Care and Use Committee. Animal research was conducted in compliance with the Animal Welfare Act and other Federal statutes and regulations relating to animals and experiments involving animals and adheres to the principles stated in the Guide for the Care and Use of Laboratory Animals, National Research Council, 1996. The facility used is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International.
2.3. Hematology and serum biochemistry
Total white blood cell counts, white blood cell differentials, red blood cell counts, platelet counts, hematocrit values, total hemoglobin, mean cell volume, mean corpuscular volume, and mean corpuscular hemoglobin concentration were determined from blood samples collected in tubes containing EDTA, by using a laser-based hematologic Analyzer (Coulter Electronics, Hialeah, FL, USA). The white blood cell differentials were performed manually on Wright-stained blood smears. Serum samples were tested for concentrations of albumin (ALB), amylase (AMY), alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), glucose (GLU), cholesterol (CHOL), total protein (TP), total bilirubin (TBIL), blood urea nitrogen (BUN), and creatinine (CRE) by using a Piccolo Point-Of-Care Blood Analyzer (Abaxis, Sunnyvale, CA, USA).
2.4. Virus detection
RNA was isolated from blood and swabs using appropriate RNA isolation kits (QIAGEN, Mississauga, ON, Canada). For the detection of VSV we used a RT-PCR assay targeting the matrix gene (nt position 2355–2661, NC 001560). ZEBOV and MARV RNA were detected using primer pairs targeting the L genes (ZEBOV (AF 272001): RT-PCR: nt position 13344–13622; nested PCR-nt position 13397–13590; MARV (X 68494): RT-PCR-nt position 1966–2243; nested PCR-nt position 2017–2213). The low detection limit for these ZEBOV and MARV assays is 0.1 pfu/ml of plasma. Virus titration was performed by plaque assay on Vero E6 cells from all blood and selected organ (adrenal, testis, lymph nodes, liver, spleen, kidney, pancreas, lung, brain, and bone marrow) and swab samples. Briefly, increasing 10-fold dilutions of the samples were adsorbed to Vero E6 monolayers in duplicate wells (0.2 ml per well); thus, the limit for detection was 25 pfu/ml.
2.5. Humoral and cellular immune responses
IgG antibodies against ZEBOV and MARV were detected with an enzyme-linked immunosorbent assay (ELISA) using purified virus particles as an antigen source [5,6]. CD4 and CD8 T-cell responses to ZEBOV and MARV were evaluated by assessing the intracellular production of IFN-γ and TNF-α by flow cytometry as previously described [5,6].
3. Results
3.1. Clinical observations
We employed twelve cynomolgus macaques, of which five animals were immunized by i.m. injection with a single dose of VSVΔG/ZEBOVGP (Subjects #1–3 and Controls #4–5) and the remaining seven with a single dose of VSVΔG/MARVGP (Subjects # 4–7 and Controls #1–3). The animals were monitored closely for clinical symptoms and shedding of recombinant VSVs. Following vaccination none of the animals showed any signs of clinical symptoms indicating that the recombinant VSVs are apathogenic for these animals.
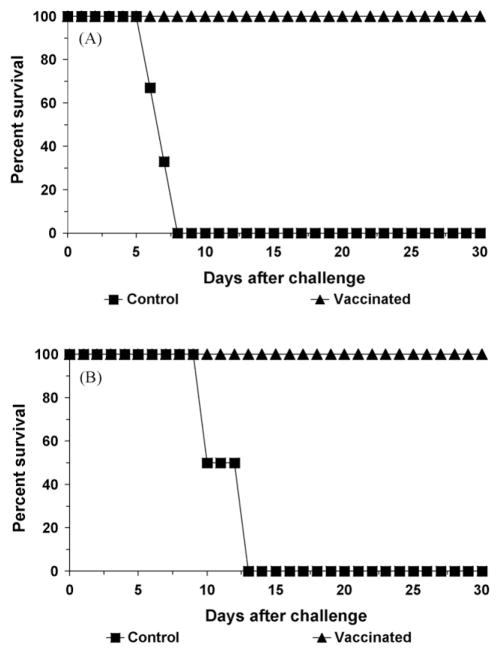
Animals were challenged 28 days after the single dose vaccine by aerosol exposure with either ZEBOV (Subjects #1–3 and Controls #1–3) or MARV (Subjects #4–7 and Controls #4–5). The three VSVΔG/MARVGP-immunized animals (Controls #1–3), which served as controls in the ZEBOV challenge, started to show clinical signs of disease on day 6 after challenge including lymphopenia, thrombocytopenia, elevated levels of serum enzymes associated with liver function, depression, anorexia, and the appearance of macular rashes. The development of the changes in behavior and appearance occurred about one day later than previously reported for cynomolgous macaques challenged with the same ZEBOV seed and dose by i.m. injection [33]. Nonetheless, the animals succumbed to the ZEBOV infection on days 6, 7, and 8, respectively (Fig. 1A). In contrast, none of the three VSVΔG/ZEBOVGP-immunized macaques became sick from the ZEBOV challenge and all three animals were fully protected.
Fig. 1.
Kaplan–Meier survival curves for cynomolgus macaques vaccinated against ZEBOV or MARV and challenged against ZEBOV (A) or MARV (B).
The first sign of disease in the VSVΔG/ZEBOVGP-immunized animals (Controls #4–5), which served as controls for the MARV challenge, occurred on day 6 after MARV challenge when one animal (Control #4) presented with a small macular rash on one arm. Both of these animals showed reduced activity by day 9 and both were depressed and anorexic. By day 10, both animals had macular rashes and other evidence of clinical illness including lymphopenia, thrombocytopenia, and elevated levels of serum enzymes associated with liver function. As was noted with the ZEBOV control animals, the development of the changes in behavior and appearance occurred about 1–2 days later than previously observed for cynomolgous macaques challenged with the same MARV seed and dose by i.m. injection (6, TW Geisbert, unpublished observation). Nevertheless, these animals succumbed to the MARV infection on days 10 and 13, respectively (Fig. 1B). In contrast, none of the four VSVΔG/MARVGP-immunized macaques became sick and all four animals were fully protected against the MARV aerosol challenge. None of the protected animals in either challenge experiment displayed any clinical signs or visual symptoms of EBOV or MARV disease.
3.2. Viremia
To determine whether viremia or shedding of the recombinant VSVs occurred after immunization whole blood and swab samples from all twelve of the vaccinated animals were analyzed by RT-PCR and virus isolation. A transient and low level (≤3.3 log 10 pfu/ml) recombinant VSV viremia was detected by virus isolation only at day 2 after vaccination in plasma from four of the VSVΔG/ZEBOVGP-vaccinated animals (Subjects #1–3 and Control #1). We did not detect recombinant VSV in swab samples of any animal from this study.
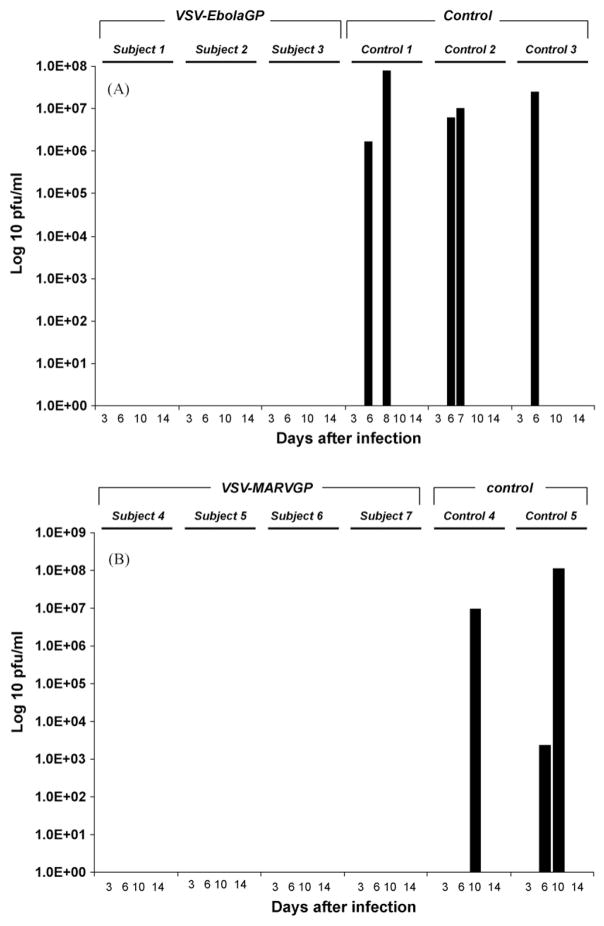
Blood samples were also analyzed after ZEBOV or MARV challenge for evidence of filoviral replication by plaque assay and RT-PCR. By day 6, all three ZEBOV control animals (Control #1–3) developed high ZEBOV titers in plasma as detected by plaque assay (>106 log pfu/ml) (Fig. 2A). In comparison, one of the MARV control animals (Control #5) was viremic at day 6 by plaque assay (~103 log pfu/ml) (Fig. 2B) and high titers of MARV were detected by plaque assay in both animals at day 10 (>107 log pfu/ml). RT-PCR was more sensitive and showed evidence of MARV in plasma of these two control animals by day 3 postinfection. In contrast, no ZEBOV or MARV was detected in plasma or swabs by virus isolation or RT-PCR in any of the animals vaccinated with either VSVΔG/ZEBOVGP or with VSVΔG/MARVGP and challenged with ZEBOV or MARV, respectively.
Fig. 2.
(A) Plasma levels of ZEBOV (pfu/ml) from cynomolgus macaques challenged with ZEBOV. (B) Plasma levels of MARV (pfu/ml) from cynomolgus macaques challenged with MARV.
Organ infectivity titration of tissues from the control animals showed ZEBOV or MARV in nearly all tissues examined (Table 1). Interestingly, the tissue tropism in these aerosol-exposed animals appeared to be consistent with results obtained in animals exposed by i.m. injection (33, TW Geisbert, unpublished observation). Notably, viral loads obtained from lungs of aerosol-exposed macaques were no greater than viral loads obtained from lungs of macaques exposed by i.m. injection whereas liver (MARV) and spleen and adrenal gland (ZEBOV and MARV) were primary target organs regardless of route of exposure.
Table 1.
Organ infectivity titers.
| Animal no. | Virus | Day of death | LVR | SPL | LNG | KID | ADR | PAN | AxLN | InLN | MsLN | BRN | TST | BM |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cont 1 | ZEBOV | 8 | 6.31a | 7.41 | 6.84 | 6.47 | 7.95 | 4.08 | 6.84 | 6.68 | 6.97 | 4.68 | 6.22 | 7.03 |
| Cont 2 | ZEBOV | 7 | 6.63 | 5.84 | 6.11 | 5.57 | 5.72 | 3.10 | 6.78 | 6.90 | 6.89 | 3.65 | 4.99 | 4.78 |
| Cont 3 | ZEBOV | 6 | 6.24 | 7.23 | 6.35 | 4.87 | 6.09 | 0.00 | 5.94 | 6.18 | 6.70 | 4.78 | 5.51 | 5.44 |
| Cont 4 | MARV | 13 | 8.27 | 7.14 | 6.08 | 5.83 | 5.92 | 7.40 | 7.38 | 7.65 | 7.26 | 6.76 | 6.60 | 3.90 |
| Cont 5 | MARV | 10 | 9.01 | 7.99 | 6.63 | 6.17 | 7.44 | 5.72 | 7.76 | 7.35 | 7.35 | 5.03 | 6.06 | 7.54 |
LVR, Liver; SPL, Spleen; LNG, Lung; KID, Kidney; ADR, Adrenal gland; PAN, Pancreas; AxLN, Axillary lymph node; InLN, Inguinal lymph node; MsLN, Mesenteric lymph node; BRN, Brain; TST, Testis; BM, Bone marrow.
Log 10 pfu/g of tissue.
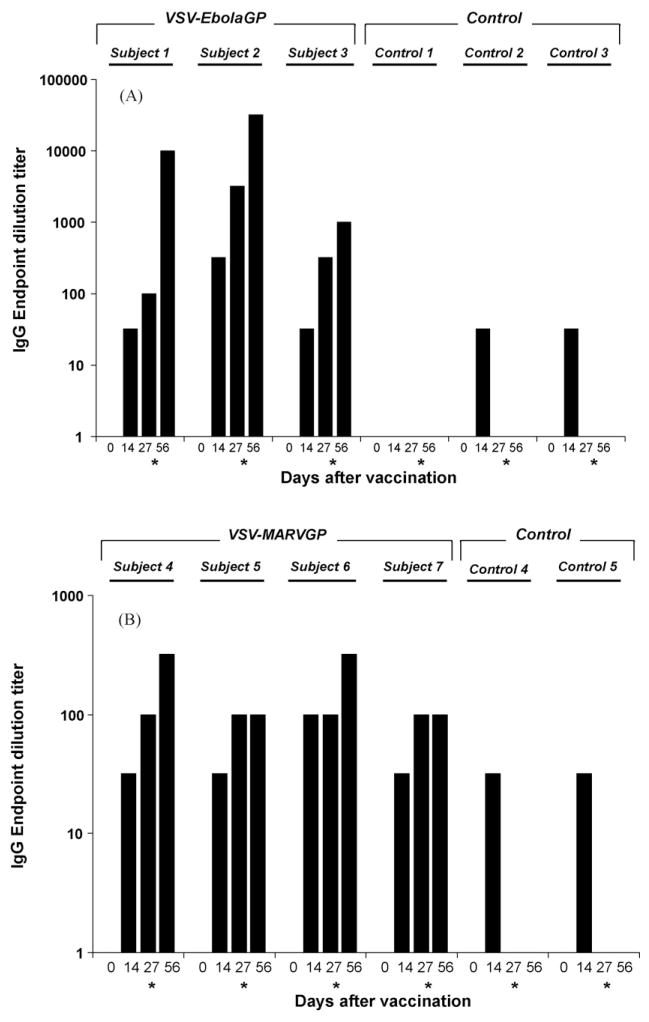
3.3. Evaluation of antibody and cellular immune responses
The antibody responses of the cynomolgus macaques vaccinated with VSVΔG/ZEBOVGP or VSVΔG/MARVGP were evaluated after vaccination (days –14 and 0) and after ZEBOV or MARV challenge (day 28) by IgG ELISA. By the day of ZEBOV challenge (day 0) all VSVΔG/ZEBOVGP-immunized animals had developed modest IgG antibody titers against ZEBOV GP (Fig. 3A). These titers increased after the ZEBOV challenge. By the day of MARV challenge (day 0) all VSVΔG/MARVGP-immunized animals had developed modest IgG antibody titers against MARV GP (Fig. 3B). These titers increased slightly in two of the four animals after the MARV challenge.
Fig. 3.
Circulating levels of IgG against ZEBOV (A) or MARV (B) from cynomolgus macaques challenged with either ZEBOV (A) or MARV (B). (*) Day of filovirus challenge (28 days after single injection vaccination).
To better understand the cellular responses of T-cell populations found in peripheral blood mononuclear cell fractions of specifically and nonspecifically vaccinated animals in mediating protection against ZEBOV or MARV challenge, flow cytometry was employed during the course of study. There was no evidence of either IFN-γ or TNF-α production in CD4 or CD8 T-cell populations either before or after the ZEBOV or MARV challenges in any of the animals employed in this study (data not shown).
4. Discussion
Few studies have evaluated the pathogenic potential of filoviruses in animals exposed by the aerosol route [20–23]. Infection of nonhuman primates after aerosol exposure to ZEBOV has been reported and was uniformly lethal in both studies [21,23]. With regard to MARV, aerosol exposure was also shown to be lethal [20,22]. However, in one study in African green monkeys there appeared to be a reduced lethality associated with aerosol exposure to MARV [20]. Despite an overall paucity of information on aerosol exposure in animals, the requirements for an EBOV or MARV vaccine suitable for military use include protection against aerosol exposure. In this study we show that our recombinant VSV-based ZEBOV and MARV vaccines completely protect cynomolgus macaques against lethal challenge with either homologous ZEBOV or MARV, respectively. This is the first demonstration of protection against an aerosol challenge with any filovirus vaccine candidate as all previous work in nonhuman primates has been done against either i.m. [3,5–11] or intraperitoneal challenge routes [4].
Consistent with the previous study suggesting that an aerosol exposure to MARV may be less pathogenic than a challenge by i.m. injection [20], our results showed that disease in cynomolgus monkeys appeared to be protracted for aerosol-exposed macaques with animals succumbing on days 10 and 13 after MARV challenge. Our previous studies using the same seed stock and dose of MARV (Musoke strain) administered to cynomolgus macaques by i.m. injection produces a uniformly lethal infection with animals succumbing primarily on day 9 (mean = 9.3, range = 9–10, TW Geis-bert, unpublished observation). While there were only two control animals exposed to MARV by the aerosol route in the current study the animal that died on day 13 was clearly delayed when compared with historical control cynomolgus macaques exposed by i.m. injection. We did not see any clear delay in time to death of the three cynomolgus monkeys exposed to ZEBOV by aerosol when compared to animals exposed by i.m. injection. Animals exposed to ZEBOV by aerosol in this study succumbed on days 6, 7, and 8, respectively compared to a mean time to death of 6.4 days (range 5–8) for animals exposed to the same virus and dose by i.m. injection [2]. Although the animal that succumbed to ZEBOV on day 8 is at the far end of the window for time to death and the disease did appear to progress slower in all three animals when looking at other clinical parameters such development of lymphopenia and thrombocytopenia, elevation in levels of enzymes associated with liver function, and the development of a macular rash.
Clearly, further studies are needed to characterize the pathogenesis of filoviruses in animals exposed by the aerosol route. However, based on our findings in the current study it appears that aerosol exposure to a filovirus may be no more difficult to protect against than a parenteral exposure. This is not surprising as the lung is not a primary target organ for filoviruses in primates [33]. Even in the current study where macaques were exposed to ZEBOV or MARV by aerosol, the lung appeared to be minimally involved compared with other organs such as liver and spleen. These results support the view that monocytes/macrophages and other antigen-presenting cells are initial sites of filovirus infection [33,34] and these cells migrate and rapidly disseminate the virus throughout the host where the virus replicates extensively and uncontrollably in preferred target organs. Thus, it appears that regardless of the portal of entry the overall pathogenesis is similar and the primary difference if any is in the length of the disease course. These results are also consistent with a study where rhesus macaques were exposed to ZEBOV by oral or conjunctival routes yet the disease pathology was indistinguishable from animals exposed by i.m. injection [35]. The fact that i.m. injection appears to produce a very rapid disease course is also consistent with human data obtained from outbreaks. Specifically, the mean incubation period for cases of ZEBOV from the 1976 outbreak known to be due to injection resulting from the reuse of needles was 6.3 days versus 9.5 days for contact exposures [36]. Moreover, the case fatality rate in this outbreak was 100% (85 of 85) in cases associated with injection compared to ~80% (119 of 149) in cases of known contact exposure [36].
In developing vaccines against any virus, there are always concerns about broad protection and the ability to protect against different species, strains, or isolates of the same virus. Here, we demonstrated that our VSV-based vaccines protected nonhuman primates against homologous aerosol challenges with either ZEBOV or the Musoke strain of MARV, respectively. We have previously shown that our VSVΔG/MARVGP preventive vaccine expressing the Musoke strain GP can completely protect nonhuman primates against heterologous peripheral challenge with either the seemingly more pathogenic Angola strain or the more distantly related Ravn strain of MARV [7]. We have also shown that a vaccine that can protect against different species of EBOV will require inclusion of antigens specific for each distinct species [6]. While most EBOV vaccine studies have focused on ZEBOV, we recently showed that a VSVΔG/SEBOVGP vaccine completely protected macaques against a homologous SEBOV peripheral challenge when administered as a postexposure treatment [14]. While aerosol challenge studies will be needed to confirm the results of these peripheral challenge studies, the results from the current aerosol studies suggest that the VSVΔG/MARVGP vaccine based on the Musoke strain of MARV will be able to protect against aerosol challenge with other MARV strains and that any EBOV vaccine will likely require inclusion of species-specific antigens.
Regarding the mechanism by which the VSVΔG/ZEBOVGP and VSVΔG/MARVGP vaccines confer protection, as in our previous studies both vaccines appeared to be associated with a strong humoral immune response [6,7]. However, for EBOV it is likely that a robust humoral immune response while possibly necessary is insufficient to confer protection. Specifically, passive antibody studies in nonhuman primates using a variety of anti-ZEBOV immune reagents including polyclonal equine immune globulin [29], a recombinant human monoclonal antibody [37], and convalescent monkey blood [38] have uniformly failed to provide protection and more importantly have failed to provide any beneficial effect. In this study and in previous studies [6,7] we failed to detect a cellular immune response against MARV. In a previous study we observed a cellular immune response against ZEBOV [6] whereas in this study we did not observe a cellular response against ZEBOV. However, as has been reported by others our findings illustrate the limitation of the evaluation of cellular immune responses using small numbers of functional measurements (such as interferon-gamma) [39]. It is evident that the T cell cytokine profile generated in response to an immunogen can be rather complex. In addition, even with successful cellular responses, the frequency of antigen-specific T cells can still be quite low (typically less than 0.1% of lymphocytes) [40,41]. It is likely that the intracellular cytokine assay that we have employed in the current study is not sensitive or thorough enough to detect a cellular immune response against ZEBOV or MARV. Future studies will need to develop a more sensitive and systematic evaluation of antigen-specific T cells which will require the coordinate measurement of several cytokines across different populations of T cells which is now possible using multicolor flow cytometry assays (e.g., 18-color flow cytometry).
The primary objective of the current study was to determine whether our VSV-based ZEBOV and MARV vaccines could completely protect nonhuman primates against an aerosol challenge. Our results unequivocally show that both of these VSV-based vaccines can confer complete protection against either i.m. [6,7] or aerosol challenges (this study) of high doses of infectious filoviruses. It is likely that these results will have importance for other vaccine systems. However, because the host immune response elicited by different vaccine platforms could be different it is not possible to say with absolute certainty that the results shown here for the VSV-based filovirus vaccine system will hold true for all filovirus vaccine candidates and each will therefore need to be evaluated independently.
Acknowledgments
From USAMRIID, the authors thank John Crampton and Carlton Rice for animal care and Matthew Lackemeyer and Adam Hedge for assistance with aerosol exposures. From the National Microbiology Laboratory (NML) of the Public Health Agency of Canada (PHAC), the authors thank Jason Gren and Anders Leung for technical assistance in biocontainment. We are grateful to John Rose (Yale University) for kindly providing us with the vesicular stomatitis virus reverse genetics system. Work on filoviruses at USAMRIID was funded by the Defense Threat Reduction Agency (project number 04-4-7J-012). Work on filoviruses at the National Microbiology Laboratory was supported by Public Health Agency of Canada, a grant awarded to HF from the Canadian Institutes of Health Research (MOP-39321), and a grant awarded to SMJ from Chemical, Biological, Radiological, and Nuclear (CBRN) Research and Technology Initiative (CRTI). Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by Boston University, the U.S. Army, or the Public Health Agency of Canada.
References
- 1.Feldmann H, Geisbert TW, Jahrling PB, Klenk HD, Netesov SV, Peters CJ, et al. Filoviridae. In: Fauquet C, Mayo MA, Maniloff J, Desselberger U, Ball LA, editors. Virus taxonomy: VIIIth report of the international committee on taxonomy of viruses. London: Elsevier/Academic Press; 2004. pp. 645–53. [Google Scholar]
- 2.Sanchez A, Geisbert TW, Feldmann H. Filoviridae: Marburg and Ebola viruses. In: Knipe DM, Howley PM, Griffin DE, editors. Fields virology. 5. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 1409–48. [Google Scholar]
- 3.Hevey M, Negley D, Pushko P, Smith J, Schmaljohn A. Marburg virus vaccines based upon alphavirus replicons protect guinea pigs and nonhuman primates. Virology. 1998;251:28–37. doi: 10.1006/viro.1998.9367. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan NJ, Sanchez A, Rollin PE, Yang ZY, Nabel GJ. Development of a preventive vaccine for Ebola virus infection in primates. Nature. 2000;408:605–9. doi: 10.1038/35046108. [DOI] [PubMed] [Google Scholar]
- 5.Sullivan NJ, Geisbert TW, Geisbert JB, Xu L, Yang Z-Y, Roederer M, et al. Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates. Nature. 2003;424:681–4. doi: 10.1038/nature01876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones SM, Feldmann H, Ströher U, Geisbert JB, Fernando L, Grolla A, et al. Live attenuated recombinant vaccine platform protects non-human primates against lethal challenge with either Ebola virus or Marburg virus. Nat Med. 2005;11:786–90. doi: 10.1038/nm1258. [DOI] [PubMed] [Google Scholar]
- 7.Daddario-DiCaprio KM, Geisbert TW, Geisbert JB, Stroher U, Hensley LE, Grolla A, et al. Cross-protection against Marburg virus strains using a live, attenuated recombinant vaccine. J Virol. 2006;80:9659–66. doi: 10.1128/JVI.00959-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sullivan NJ, Geisbert TW, Geisbert JB, Shedlock DJ, Xu L, Lamoreaux L, et al. Immune protection of nonhuman primates against Ebola virus with single low-dose adenovirus vectors encoding modified GPs. PLoS Med. 2006;3:e177. doi: 10.1371/journal.pmed.0030177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bukreyev A, Rollin PE, Tate MK, Yang L, Zaki SR, Shieh WJ, et al. Successful topical respiratory tract immunization of primates against Ebola virus. J Virol. 2007;81:6379–88. doi: 10.1128/JVI.00105-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warfield KL, Swenson DL, Olinger GG, Kalina WV, Aman MJ, Bavari S. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J Infect Dis. 2007;196(Suppl 2):S430–7. doi: 10.1086/520583. [DOI] [PubMed] [Google Scholar]
- 11.Swenson DL, Wang D, Luo M, Warfield KL, Woraratanadharm J, Holman DH, et al. Complete protection of nonhuman primates against multi-strain Ebola and Marburg virus infections. Clin Vaccine Immunol. 2008 Jan 23; doi: 10.1128/CVI.00431-07. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daddario-DiCaprio KM, Geisbert TW, Stroher U, Geisbert JB, Grolla A, Fritz EA, et al. Postexposure protection against Marburg haemorrhagic fever with recombinant vesicular stomatitis virus vectors in non-human primates: an efficacy assessment. Lancet. 2006;367:1399–404. doi: 10.1016/S0140-6736(06)68546-2. [DOI] [PubMed] [Google Scholar]
- 13.Feldmann H, Jones SM, Daddario-Dicaprio KM, Geisbert JB, Stroher U, Grolla A, et al. Effective post-exposure treatment of Ebola infection. PLoS Pathog. 2007;3:e2. doi: 10.1371/journal.ppat.0030002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geisbert TW, Daddario-Dicaprio KM, Williams K, Geisbert JB, Leung A, Feldmann F, et al. Recombinant vesicular stomatitis virus vector mediates pos-texposure protection against Sudan Ebola hemorrhagic fever in nonhuman primates. J Virol. 2008;82:5664–8. doi: 10.1128/JVI.00456-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walsh PD, Abernethy KA, Bermejo M, Beyers R, De Wachter P, Akou ME, et al. Catastrophic ape decline in western equatorial Africa. Nature. 2003;422:611–4. doi: 10.1038/nature01566. [DOI] [PubMed] [Google Scholar]
- 16.Groseth A, Feldmann H, Strong JE. The ecology of Ebola virus. Trends Microbiol. 2007;15:408–16. doi: 10.1016/j.tim.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Leroy EM, Kumulungui B, Pourrut X, Rouquet P, Hassanin A, Yaba P, et al. Fruit bats as reservoirs of Ebola virus. Nature. 2005;438:575–6. doi: 10.1038/438575a. [DOI] [PubMed] [Google Scholar]
- 18.Towner JS, Pourrut X, Albariño CG, Nkogue CN, Bird BH, Grard G, et al. Marburg virus infection detected in a common African bat. PLoS ONE. 2007;2:e764. doi: 10.1371/journal.pone.0000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bausch DG, Feldmann H, Geisbert TW, Bray M, Sprecher AG, Boumandouki P, et al. Outbreaks of filovirus hemorrhagic fever: time to refocus on the patient. J Infect Dis. 2007;196(Suppl 2):S136–41. doi: 10.1086/520542. [DOI] [PubMed] [Google Scholar]
- 20.Bazhutin NB, Belanov EF, Spiridonov VA, Voitenko AV, Krivenchik NA, Krotov SA, et al. The influence of the methods of experimental infection with Marburg virus on the course of illness in green monkeys. Vopr Virusol. 1992;3:153–6. [PubMed] [Google Scholar]
- 21.Johnson E, Jaax N, White J, Jahrling P. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int J Exp Pathol. 1995;76:227–36. [PMC free article] [PubMed] [Google Scholar]
- 22.Lub MIu, Sergeev AN, P’iankov OV, P’iankova OG, Petrishchenko VA, Kotliarov LA. Certain pathogenetic characteristics of a disease in monkeys in infected with the Marburg virus by an airborne route. Vopr Virusol. 1995;40:158–61. [PubMed] [Google Scholar]
- 23.P’yankov OV, Sergeev AN, P’yankova OG, Chepurnov AA. Experimental Ebola fever in Macaca rhesus. Vopr Virusol. 1995;3:113–5. [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. [Accessed July 29, 2008];Category A Agents. Available at: http://www.bt.cdc.gov/agent/agentlist-category.asp#a.
- 25.Christopher GW, Cieslak TJ, Pavlin JA, Eitzen EM., Jr Biological warfare. A historical perspective. JAMA. 1997;278:412–7. [PubMed] [Google Scholar]
- 26.Alibek K. Testimony before the Joint Economic Committee, United States Congress; Wednesday, May 20, 1998; [Accessed July 29, 2008]. Available at: http://www.house.gov/jec/hearings/intell/alibek.htm. [Google Scholar]
- 27.Alibek K, Handelman S. Told from the inside by the man who ran it. New York: Random House; 1999. Biohazard: the chilling true story of the largest covert biological weapons program in the world. [Google Scholar]
- 28.Garbutt M, Liebscher R, Wahl-Jensen V, Jones S, Moller P, Wagner R, et al. Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J Virol. 2004;78:5458–65. doi: 10.1128/JVI.78.10.5458-5465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jahrling PB, Geisbert TW, Geisbert JB, Swearengen JR, Bray M, Jaax NK, et al. Evaluation of immune globulin and recombinant interferon α-2b for treatment of experimental Ebola virus infections. J Infect Dis. 1999;179(Suppl 1):S224–34. doi: 10.1086/514310. [DOI] [PubMed] [Google Scholar]
- 30.Smith DH, Johnson BK, Isaacson M, Swanepoel R, Johnson KM, Kiley M, et al. Marburg-virus disease in Kenya. Lancet. 1982;1:816–20. doi: 10.1016/s0140-6736(82)91871-2. [DOI] [PubMed] [Google Scholar]
- 31.Reed DS, Lind CM, Sullivan LJ, Pratt WD, Parker MD. Aerosol infection of cynomolgus macaques with enzootic strains of Venezuelan equine encephalitis viruses. J Infect Dis. 2004;189:1013–7. doi: 10.1086/382281. [DOI] [PubMed] [Google Scholar]
- 32.Reed DS, Lind CM, Lackemeyer MG, Sullivan LJ, Pratt WD, Parker MD. Genetically engineered, live, attenuated vaccines protect nonhuman primates against aerosol challenge with a virulent IE strain of Venezuelan equine encephalitis virus. Vaccine. 2005;23:3139–47. doi: 10.1016/j.vaccine.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 33.Geisbert TW, Hensley LE, Larsen T, Young HA, Reed DS, Geisbert JB, et al. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am J Pathol. 2003;163:2347–70. doi: 10.1016/S0002-9440(10)63591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Geisbert TW, Jahrling PB, Hanes MA, Zack PM. Association of Ebola-related Reston virus particles and antigen with tissue lesions of monkeys imported to the United States. J Comp Pathol. 1992;106:137–52. doi: 10.1016/0021-9975(92)90043-t. [DOI] [PubMed] [Google Scholar]
- 35.Jaax NK, Davis KJ, Geisbert TW, Vogel P, Jaax GP, Topper M, et al. Lethal experimental infection of rhesus monkeys with Ebola-Zaire (Mayinga) virus by the oral and conjunctival route of exposure. Arch Pathol Lab Med. 1996;120:140–55. [PubMed] [Google Scholar]
- 36.Breman JG, Piot P, Johnson KM, White MK, Mbuyi M, Sureauet P, et al. The epidemiology of Ebola haemorrhagic fever in Zaire 1976. In: Pattyn S, editor. Ebola virus haemorrhagic fever. Amsterdam: Elsevier/North Holland; 1978. pp. 103–24. [Google Scholar]
- 37.Oswald WB, Geisbert TW, Davis KJ, Geisbert JB, Sullivan NJ, Jahrling PB, et al. Neutralizing antibody fails to impact the course of Ebola virus infection in monkeys. PLoS Pathog. 2007;3:e9. doi: 10.1371/journal.ppat.0030009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jahrling PB, Geisbert JB, Swearengen JR, Larsen T, Geisbert TW. Ebola hemorrhagic fever: evaluation of passive immunotherapy in nonhuman primates. J Infect Dis. 2007;196(Suppl 2):S400–3. doi: 10.1086/520587. [DOI] [PubMed] [Google Scholar]
- 39.De Rosa SC, Lu FX, Yu J, Perfetto SP, Falloon J, Moser S, et al. Vaccination in humans generates broad T cell cytokine responses. J Immunol. 2004;173:5372–80. doi: 10.4049/jimmunol.173.9.5372. [DOI] [PubMed] [Google Scholar]
- 40.Caulfield MJ, Wang S, Smith JG, Tobery TW, Liu X, Davies M-E. Sustained peptide-specific gamma interferon T-cell response in rhesus macaques immunized with human immunodeficiency virus gag DNA vaccines. J Virol. 2002;76:10038–43. doi: 10.1128/JVI.76.19.10038-10043.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roederer M, Brenchley JM, Betts MR, De Rosa SC. Flow cytometric analysis of vaccine responses: how many colors are enough? Clin Immunol. 2004;110:199–205. doi: 10.1016/j.clim.2003.11.015. [DOI] [PubMed] [Google Scholar]