Abstract
Background
Hemangioma is a common benign tumor in the liver and usually asymptomatic. Scanty evidence concerning treatment modality of symptomatic hemangioma during pregnancy exists.
Case
A 35 year-old woman with giant hepatic cavernous hemangioma developed consumption coagulopathy due to the enlarged tumor, and underwent danaparoid therapy from 5 weeks of gestation (GW). Magnetic resonance image revealed giant hemangioma with 20 cm in diameter in the right lobe of the liver. A surgical operation of liver resection was successfully performed at 16 GW. Thereafter, the coagulopathy disappeared. She delivered a healthy male infant at 36 GW.
Conclusion
This is the first case report of surgical resection therapy for giant liver hemangioma during pregnancy.
Keywords: liver hemangioma, pregnancy, resection, danaparoid
Introduction
Hemangioma is the most common benign tumor in the liver, and usually asymptomatic. The prevalence of liver hemangioma is found to be 0.4–7.4% in autopsy studies (1). The liver hemangioma with > 5 cm in diameter is rare, and referred to as giant hemangioma. The size of hemangioma can be a decision factor for medical intervention modalities. Yamagata et al. (2) suggest that hemangioma with >5 cm in diameter is considered for surgical operation if hemangioma causes symptoms or shows rapid tumor growth. Spontaneous ruptures of hemangiomas with >4 cm in diameter may occur (3). In case of the tumor rupture, the mortality rate is known to be extremely high as 78% (4). Other medical indications for surgical operation include rapid tumor growth, thrombocytopenia, and intraperitoneal bleeding. On the other hand, non-surgical medical intervention modalities include hepatic artery embolization and radiotherapy. Although arterial embolization is mainly used to control acute bleeding, it is often followed by abscess complication and there is little evidence for a long-term efficacy (5).
We encountered a pregnant woman with giant liver hemangioma and Kasabach-Merrit syndrome (KMS) who successfully underwent liver resection at 16 weeks of gestation (GW). The previous relevant literature on treatment modalities for liver hemangioma during pregnancy was also reviewed.
Case
A 35 year-old Japanese woman with gravida 3, para 0 was first referred to the Kobe University Hospital for the etiology assessment of recurrent pregnancy loss. She was diagnosed as having adult-onset Still’s disease at 32 year-old in a former hospital. The liver hemangioma with 12 x 12 x 9 cm in diameter occupying right liver lobe was detected by abdominal CT scan and magnetic resonance imaging (MRI) when she was examined for Still’s disease. No follow-up for liver hemangioma was performed for the next three years.
When she next visited the University Hospital, she was pregnant. Fibrinogen degradation product (FDP) and D-dimer at 4 GW were found to be remarkably elevated to 29.2 μg/ml (normal <5 μg/ml) and 16.2 μg/ml (normal <1 μg/ml), respectively. Then, she was hospitalized for further examinations at 5 GW. Blood analyses on admission revealed increased levels of FDP (83.6 μg/ml) and D-dimer (47.1μg/ml), and relatively low platelet count (14.3 x 103/mm3). The liver function, renal function and urinalysis results were within the normal ranges. Autoimmune diseases were denied. Venous ultrasound showed no deep venous thrombosis. Abdominal ultrasound showed liver hemangioma with 17 cm x 14 in diameter at 5 GW. The presence of consumption coagulopathy due to the liver hemangioma, namely KMS, was suspected.
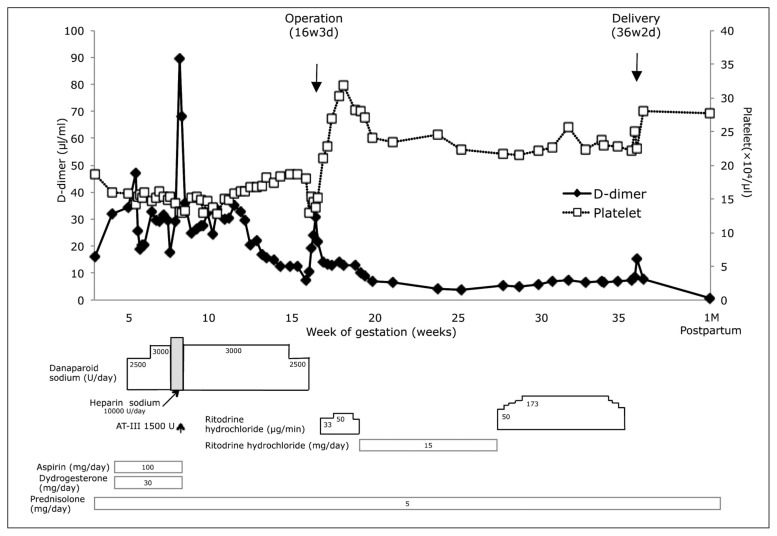
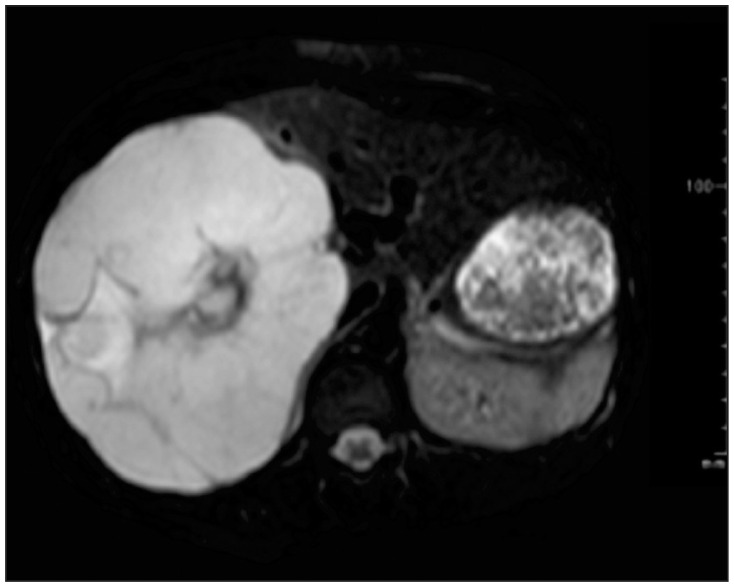
Consequently, anticoagulant therapy with intravenous infusion of danaparoid sodium was commenced. Danaparoid infusion (2500–3000 units/day) was maintained to achieve adequate anticoagulation effect by serial monitoring of D-dimer and bleeding time. Heparin sodium (10000 IU/day) was once substituted for danaparoid at 8 GW. However, coagulopathy became worse, so that we thereafter used danaparoid infusion. AT-III concentrate was also administered once. Low-dose aspirin and dydrogesterone were administered until 9 GW (Figure 1). Abdominal MRI was performed at 12 GW. Liver hemangioma occupied the right lobule and increased in the size (20 cm x 15 cm x 12 cm diameters) as compared with that of 3 years before (Figure 2). We informed the patient and family that the coagulopathy deteriorated after she became pregnant due to the enlarged liver hemangioma, and that risks of tumor rupture and serious bleeding along with use of anticoagulation therapy during pregnancy were present, and that in case of the rupture maternal and fetal mortality risks were high. The patient and family selected surgical resection option rather than conservative therapies. At 16 GW, the patient underwent tumor resection under general anesthesia. Laparotomy was performed in inverted T-shape, and the liver was remarkably enlarged. Chorecystectomy was first done, and right lobe of the liver was resected. The 7 hours 9 minutes operation was successfully completed with blood loss of 1380 mL. The patient received 4 IU of red blood cell and 4 IU of fresh frozen plasma transfusions during the operation. Resected liver including hemangioma weighed 1500 g. Pathological examination of the surgical specimen confirmed the presence of hepatic cavernous hemangioma. Coagulation abnormalities disappeared immediately after the surgery, and danaparoid infusion was not necessary thereafter. Postoperative course was uneventful and the patient was discharged at 20 GW.
Figure 1.
Clinical course and treatment.
Figure 2.
Coronal section of MRI T2-weighted image at 12 GW revealed a giant hemangioma, 20 cm in diameter, in the enlarged right lobe of the liver. Right hepatic vein and anterior segmental branch of the portal vein were compressed by the tumor.
Due to threatened premature labor, the patient was rehospitalized at 27 GW. She was treated with ritodorine hydrochloride until 35 GW. The patient delivered a male weighing 2214 g with Apgar score of 8 (1′) and 9 (5′) at 36w GW. The puerperal course of the mother and newborn were uneventful, and they were discharged on day 5.
Discussion
KMS is a consumptive coagulopathy that was originally described in association with cutaneous hemangiomas in children. The incidence of liver hemangioma in KMS is reported to be about 2.0–3.8% (6, 7). Local activation of coagulation commonly results in disseminated intravascular coagulation. Heparin is commonly used in patients with KMS. On the other hand, danaparoid is heparinoid that has a longer half life of 20 hours and has a high anti-Xa/anti-IIa ratio. There were only two case reports of danaparoid administration for treatment of chronic DIC associated with KMS (8, 9). In the present case, coagulopathy deteriorated during pregnancy due to the enlarged liver hemangioma. Danaparoid administration was found to be partially effective. Risks of tumor rupture and serious bleeding along with continuous use of anticoagulation therapy during pregnancy were present. In case of the rupture risks of maternal/fetal mortality and morbidity seemed to be high. With informed consent, liver resection was performed at 16 GW. Thereafter, anticoagulant therapy was not necessary. The patient vaginally delivered a healthy baby at 36 GW.
To the best of our knowledge, this was the first case report on successful surgical resection therapy for giant liver hemangioma in a pregnant woman. The databases MEDLINE were searched using the following MeSH terms and/or as free text: ‘liver hemangioma’, ‘liver cavernous hemangioma’ and ‘pregnancy’. In addition, reviews and reference lists were searched for further references. In the English literature, another 15 pregnant cases complicated with liver hemangiomas were found (10–22) (Table 1). Tumor sizes determined in pregnancy ranged from 2 to 61 cm in diameter. Hormonal influence on liver hemangioma growth is suggested (15, 16, 23). In Table 1, six out of eight cases showed enlargement during pregnancy. Other than asymptomatic liver hemangioma, symptoms of liver hemangioma included vomiting, epigastric pain, right upper quadrant pain, awareness of a mass and abnormality in fetal heart rate pattern. Two cases with spontaneous rupture during labor had signs of non-reassuring fetal status (19) and late deceralation on cardiotocogram (21). Gungor et al. described that the pain caused by rupture felt in the right hypochondriac region was not differed from regular labor pain (21). Sewell et al. reported a case with spontaneous rupture of 10-cm hemangioma and hemorrhagic shock in 4 months of gestation (11). Schwartz et al. reported a case treated with trisegmentectomy, but no pregnancy course after surgery was addressed (14). Graham et al. reported the use of arteriography and embolization to treat a liver hemangioma with intra-tumor hemorrhage at 19 GW. The 9-cm mass was located in the caudate lobe of the liver. The tumor regressed to about 50% of its original size (15). In pregnancy, enlargement of the uterus, intense diaphragmatic and abdominal muscular contractions or labor cause high intraabdominal pressure and increase a risk of tumor rupture. Hemangioma with 2-cm diameter ruptured during labor (21). A high pressure in the abdomen caused by fundal pressure may lead to tumor rupture and bleeding. Therefore, most authors selected cesarean section.
Table 1.
Reported cases of pregnancies with liver hemangioma.
| Author (publication year) | Age (years) | G | P | Location | Diameter (cm) | Growth during pregnancy | Symptom/Finding | Complications during pregnancy | Treatment | Delivery | Fetal outcome | Maternal outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rubin IC10(1918) | 33 | 9 | 9 | Rt | 61 | NS | Abdominal distension | NS | Resection after artificial abortion | (Termination) | - | Good |
| Sewell JH et al.11 (1961) | 21 | 0 | 0 | Rt | 10 | NS | Abdominal pain, shock in 4 months | Rupture, intraabdominal hemorrhage | Packing of the bleeding site | - | NS | Died 5 hours after surgery |
| Okazaki N et al.12 (1977) | 31 | 4 | 2 | Rt/Lt | (Diffuse) | NS | Palpable mass in 3 months | NS | Irradiation after artificial abortion | (Termination) | - | Good |
| Creasy G W et al.13 (1985) | 29 | 2 | 2 | Rt | 4 | + | Incidental finding on US in 2nd trimester | NS | Observation | NS | NS | NS |
| Schwartz SI et al.14 (1987) | 31 | 1 | 1 | Rt | 32 | + | Appearance and rapid enlargement in 1st trimester | NS | Trisegmentectomy | NS | NS | Good |
| Graham E et al.15 (1993) | 29 | 1 | 0 | Caudate | 12 | NS | Vomiting and epigastric pain at 18 weeks | Vomiting and epigastric pain | Embolization | Elective C/S (to avoid possible rupture) | Good | Good |
| Saegusa T et al.16 (1995) | 34 | 3 | 1 | Rt/Lt | 5 | NS | Palpable mass prior to pregnancy | None | Observation (partial resection at 6M postpartum) | Elective C/S (due to previous C/S) | Good | Good |
| Marques R et al.17 (1997) | 29 | 3 | 1 | Rt | 30 | - | Hepatomegaly at 19 weeks | None | Observation | Vacuum extraction (to shorten expulsive period) | Good | Good |
| Spitzer D et al.18 (1997) | 31 | 0 | 0 | Rt | 14 | + | Incidental finding on US prior to pregnancy | None | Observation | Elective C/S (to avoid possible rupture) | Good | Good |
| Krasuski P et al.19 (2001) | 28 | 2 | 1 | Rt | (Large) | NS | Right upper quadrant pain at 35 weeks. Meconium stain, non-reassuring fetal heart rate. Emergent C/S | Rupture, intraabdominal hemorrhage at 35 weeks | Packing of the bleeding site | Emergent C/S | Good | Good |
| Cobey HC et al.20 (2004) | 36 | 3 | 2 | NS | 8 | + | Incidental finding on US prior to pregnancy | None | Observation | Vaginal | Good | Good |
| Cobey HC et al.20 (2004) | 39 | 5 | 4 | NS | 10 | + | Incidental finding on US at 17 weeks | None | Observation (enucleation at ly postpartum) | C/S | Good | Good |
| Cobey HC et al.20 (2004) | 31 | 5 | 4 | NS | 3 | - | Right upper quadrant pain at 36 weeks | None | Observation | C/S | Good | Good |
| Gungor T et al.21 (2004) | 27 | 0 | 0 | Rt | 2 | NS | Late deceleration during labor at 36 weeks. Emergent C/S | Rupture, intraabdominal hemorrhage at 36 weeks | Resection shortly after C/S | Emergent C/S | Good | Good |
| Au WY et al.22 (2005) | 33 | 2 | 2 | Rt | 3 | NS | Incidental finding on US at 16 weeks | None | Observation | Elective C/S (due to triplet pregnancy) | Good | Good |
| Present case | 35 | 3 | 0 | Rt | 20 | + | Incidental finding on US prior to pregnancy | Consumptive coagulopathy | Danaparoid infusion/Resection at 16 weeks | Vacuum extraction (due to fetal distress) | Good | Good |
G: Gravida; P: Para; NS: Not stated; US: Ultrasound.
We demonstrated that symptomatic and coagulopathy-complicated liver hemangioma could be successfully treated by surgical resection at 16 GW. Although natural history of hemangiomas is not fully understood, a giant hemangioma as shown in the present case should be treated prior conception to avoid possible complications in pregnancy.
References
- 1.Ishak KG, Rabin L. Benign tumors of the liver. Med Clin North Am. 1975;59:995–1013. doi: 10.1016/s0025-7125(16)31998-8. [DOI] [PubMed] [Google Scholar]
- 2.Yamagata M, Kanematsu T, Matsumata T, Utsunomiya T, Ikeda Y, Sugimachi K. Management of haemangioma of the liver: comparison of results between surgery and observation. Br J Surg. 1991;78:1223–1225. doi: 10.1002/bjs.1800781025. [DOI] [PubMed] [Google Scholar]
- 3.Yamamoto T, Kawarada Y, Yano T, Noguchi T, Mizumoto R. Spontaneous rupture of hemangioma of the liver: treatment with transcatheter hepatic arterial embolization. Am J Gastroenterol. 1991;86:1645–1649. [PubMed] [Google Scholar]
- 4.Gilon D, Slater PE, Benbassat J. Can decision analysis help in the management of giant hemangioma of the liver? J Clin Gastroenterol. 1991;13:255–258. [PubMed] [Google Scholar]
- 5.Reading NG, Forbes A, Nunnerley HB, Williams R. Hepatic haemangioma: a critical review of diagnosis and management. Q J Med. 1988;67:431–445. [PubMed] [Google Scholar]
- 6.Iqbal N, Saleem A. Hepatic hemangioma: a review. Tex Med. 1997;93:48–50. [PubMed] [Google Scholar]
- 7.Moreno Egea A, Del Pozo Rodriguez M, Vicente Cantero M, Abellan Atenza J. Indications for surgery in the treatment of hepatic hemangioma. Hepatogastroenterology. 1996;43:422–426. [PubMed] [Google Scholar]
- 8.Ontachi Y, Asakura H, Omote M, Yoshida T, Matsui O, Nakao S. Kasabach-Merritt syndrome associated with giant liver hemangioma: the effect of combined therapy with danaparoid sodium and tranexamic acid. Haematologica. 2005;90(Suppl):ECR29. [PubMed] [Google Scholar]
- 9.Moriguchi A, Iwahashi K, Onishi Y, Kita H, Nishio A, Kanno T, et al. An operated case of retroperitoneal venous hemangioma complicated with Kasabach-Merritt syndrome which was well controlled by danaparoid sodium. Nippon Shokakibyo Gakkai Zasshi. 2009;106:1660–1668. [PubMed] [Google Scholar]
- 10.Rubin I. Larger pedunculated cavenous angioma of the liver reaching down into the pelvis and causing obstetric difficulty. Am J Obste Dis Women Children. 1918;77:273–276. [Google Scholar]
- 11.Sewell JH, Weiss K. Spontaneous rupture of hemangioma of the liver. A review of the literature and presentation of illustrative case. Arch Surg. 1961;83:729–733. doi: 10.1001/archsurg.1961.01300170085016. [DOI] [PubMed] [Google Scholar]
- 12.Okazaki N, Yoshino M, Yoshida T, Ohno T, Kitagawa T. Radiotherapy of hemangioma cavernosum of the liver. Gastroenterology. 1977;73:353–356. [PubMed] [Google Scholar]
- 13.Creasy GW, Flickinger F, Kraus RE. Maternal liver hemangioma in pregnancy as an incidental finding. Obstet Gynecol. 1985;66:10S–13S. [PubMed] [Google Scholar]
- 14.Schwartz SI, Husser WC. Cavernous hemangioma of the liver. A single institution report of 16 resections. Ann Surg. 1987;205:456–465. doi: 10.1097/00000658-198705000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Graham E, Cohen AW, Soulen M, Faye R. Symptomatic liver hemangioma with intra-tumor hemorrhage treated by angiography and embolization during pregnancy. Obstet Gynecol. 1993;81:813–816. [PubMed] [Google Scholar]
- 16.Saegusa T, Ito K, Oba N, Matsuda M, Kojima K, Tohyama K, et al. Enlargement of multiple cavernous hemangioma of the liver in association with pregnancy. Intern Med. 1995;34:207–211. doi: 10.2169/internalmedicine.34.207. [DOI] [PubMed] [Google Scholar]
- 17.Marques R, Taborda F, Jorge CS, Areias J, Rodrigues AM. Successful outcome in a pregnancy complicated by large hepatic hemangioma. Acta Obstet Gynecol Scand. 1997;76:606–607. doi: 10.3109/00016349709024595. [DOI] [PubMed] [Google Scholar]
- 18.Spitzer D, Krainz R, Graf AH, Menzel C, Staudach A. Pregnancy after ovarian stimulation and intrauterine insemination in a woman with cavernous macrohemangioma of the liver. A case report. J Reprod Med. 1997;42:809–812. [PubMed] [Google Scholar]
- 19.Krasuski P, Poniecka A, Gal E, Wali A. Intrapartum spontaneous rupture of liver hemangioma. J Matern Fetal Med. 2001;10:290–292. doi: 10.1080/714052747. [DOI] [PubMed] [Google Scholar]
- 20.Cobey FC, Salem RR. A review of liver masses in pregnancy and a proposed algorithm for their diagnosis and management. Am J Surg. 2004;187:181–191. doi: 10.1016/j.amjsurg.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 21.Gungor T, Aytan H, Tapisiz OL, Zergeroglu S. An unusual case of incidental rupture of liver hemangioma during labor. Chin Med J (Engl) 2004;117:311–313. [PubMed] [Google Scholar]
- 22.Au WY, Liu CL. Growth of giant hepatic hemangioma after triplet pregnancy. J Hepatol. 2005;42:781. doi: 10.1016/j.jhep.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 23.Glinkova V, Shevah O, Boaz M, Levine A, Shirin H. Hepatic haemangiomas: possible association with female sex hormones. Gut. 2004;53:1352–1355. doi: 10.1136/gut.2003.038646. [DOI] [PMC free article] [PubMed] [Google Scholar]