Abstract
Background
Black men who have sex with men (BMSM) in the United States are at highest risk for HIV infection and are at high risk for limited health service utilization. We describe HIV health center (HHC) affiliation network patterns and their potential determinants among urban BMSM.
Methods
The Men’s Assessment of Social and Risk Network instrument was utilized to elicit HHC utilization as reported by study respondents recruited through respondent driven sampling. 204 BMSM were systematically recruited from diverse venues in Chicago, Illinois in 2010. A 2-mode data set was constructed that included study participants and 9 diverse HHCs. Associations between individual level characteristics and HHC utilization were analyzed using Multiple Regression Quadratic Assignment Procedure (MRQAP). Visualization analyses included computation of HHC centrality and faction membership.
Results
High utilization of HHCs (45.9%-70.3%) was evident among BMSM; 44.4% who were HIV infected. MRQAP revealed that age, social network size and HIV status were associated with HHC affiliation patterns (coef. 0.13-0.27; all p<0.05). With the exception of one HHC, HHCs offering HIV prevention services to HIV-infected participants occupied peripheral positions within the network of health centers. High-risk HIV-uninfected participants affiliated most with an HHC that offers only treatment services.
Conclusions
Sub-categories of BMSM in this sample affiliated with HHCs that may not provide appropriate HIV prevention services. Using 2-mode data, public health authorities may be better able to match prevention services to BMSM need; in particular HIV prevention services for high-risk HIV-uninfected men and HIV “prevention for positives” services for HIV-infected men.
INTRODUCTION
The high rates of HIV infection among black men who have sex with men (BMSM) in large cities across the US suggest the urgent need to evaluate prevention and access to care in this underserved population. According to the CDC, in 2006, 35% of MSM with new HIV infection were black and among MSM ages 1329, the number of new infections in black MSM was nearly twice that of white MSM.1 In Chicago, this disparity is even higher - young black men have 7 times the rate of HIV infection as young white men with similar sexual behavior and substance use patterns.2 The high rates of HIV infection among BMSM and the concomitant lack of HIV status awareness3, 4 motivate the present analysis of utilization of HIV services for this population.
Increased disparities in HIV prevalence rates among BMSM are due to a number of factors including limited utilization of HIV prevention and treatment services.3, 4 While a few studies consider the individual-level factors associated with MSM receiving HIV testing or visiting a healthcare provider5, other studies move beyond the individual-level factors associated with access to care and instead focus on organizational-level factors of healthcare centers in an effort to explain differing levels of access.6, 7 In a study of MSM in Massachusetts, individual factors such as a higher level of social support and having health insurance was associated with access to primary care.5 Individual-level factors associated with BMSM that report no recent history of HIV testing include lower levels of attained education, higher reported sexual risk taking behavior, and not having visited a healthcare provider in the past twelve months.5
Other studies focus on organizational-level aspects of health care centers that enhance or diminish access among minority MSM.6, 7 Some studies stress the need for healthcare settings that are multifaceted and offer not only a medical component but also case management and supportive programs.7 A study of retention of young HIV sero-positive minority MSM suggests that the most important element in linkage and retention in care is whether participants felt respected in the clinic environment.6
Taken together, findings from these strands of research raise concerns about the possibility that different sub-groups of at-risk populations selectively affiliate with different health centers; behavior which may or may not be aligned with HIV prevention services offered at these respective centers. Further, differential affiliation may both give public health authorities a misleading picture of the at-risk population and give clients a skewed understanding of the kinds of services that are available to them. Centers that have different profiles of clients will inevitably receive different information about clients’ needs and may develop different service priorities in response, just as clients’ specific affiliations will shape the information they receive about specific resources and expertise. For example, public health authorities might make assumptions about the population’s needs based upon which clients are selecting into a specific clinic and act according to these assumptions (e.g., shifting resources to substance use counseling). Knowledge of the pattern of HIV health center utilization could also be useful for efficient appropriation of HIV prevention programming at select centers. Without such data, appropriation might be relegated to all centers, or worse yet, to those most able to effectively lobby for their inclusion.
Our objective is to describe specific individual- and organizational-level factors that contribute to utilization patterns of health care centers offering HIV prevention and/or treatment services among BMSM. We use a two-mode8 affiliation network analysis of health center utilization patterns to answer the following questions: (1) Which types of HIV prevention and care centers do BMSM utilize? (2) What individual-level factors are associated with healthcare utilization patterns among BMSM? (3) What individual-level and organizational-level factors are associated with BMSM’s utilization of these same health centers?
MATERIALS AND METHODS
In 2010, 204 BMSM were recruited into the study using respondent-driven sampling.9, 10 The protocol was approved by relevant institutional review boards.
Study Participants
Eligibility Criteria
Candidate “seed” participants were eligible for the study if they 1) self-identified as Black, 2) identified as male, 3) were age 18 years or older and 4) reported anal intercourse with a man within the past 12 months. Subsequent recruits were deemed eligible by the same criteria.
Recruitment
Respondent-driven sampling (RDS) has been widely applied to study hard-to-reach populations including MSM.11-14 RDS is an efficient method that uses respondents’ network connections to generate a sample that approximates a probability sample allowing for valid statistical analysis when its assumptions are met.11, 15, 16 Twenty-one seeds were recruited from four diverse venues across the city. Seeds were recruited from the following venues: 1) a Federally Qualified Health Center that provides HIV primary care; 2) a Community Based Organization that provides HIV prevention services; 3) a substance use treatment program; and 4) an LGBT health-care center. Seeds were asked to refer up to 4 recruits who were MSM from their social networks (by definition could include all networks) using vouchers, with each subsequent recruit doing likewise. All study participants were provided with a $50 gift card for participation.
Measures
Dependent Variables
Data on BMSMs’ awareness and utilization of health centers offering HIV services were used to construct the key dependent variables in the study. Prior to recruitment of the main RDS sample, twelve preparatory in-depth qualitative interviews of BMSM from two geographic areas in Chicago were conducted in order to identify health centers associated with either HIV prevention and/or treatment services. There was considerable overlap of center awareness between the participants in this qualitative study, resulting in a list of nine health centers. Centers that were mentioned only once were not included in this final center roster. Health centers were classified by type of center (e.g., CBO, public clinic, or private clinic) and area of the city (e.g., north, south, or west side of Chicago). Services provided in the past two years were determined by discussions with HIV program staff for each of the nine health centers. All centers provided HIV voluntary counseling and testing. Centers that included any of the following services were categorized as providing HIV prevention services: effective behavioral interventions (EBI), pre-exposure or post-exposure prophylaxis (PEP/PrEP), prevention for positives programming. Availability of condoms, education/awareness only, or referral to STI testing were not considered prevention services in the current analysis. Centers that provided antiretroviral based HIV treatment were categorized as providing HIV treatment services. The nine centers included on the final roster reflect a full spectrum of venues along these classifications.
To assess awareness of health centers offering HIV services, participants were presented with the roster of nine Chicago health centers and were asked, “Which of the following centers have you heard of?” To assess utilization, these participants were also asked, “Which of the following centers have you been to?” The result of this measure was an adjacency matrix; each cell in the matrix contains the value (0=no; 1=yes) indicating whether one person (row) is aware of or utilizes a health center (column).8
The dependent variable differs from a count of the number of organizations with which a given participant was affiliated; rather, the dependent variable is a count of the number of health centers that a given pair of participants list in common (204 × 203 = 41,412 potential pairs of participants). For example, if Person 1 listed Centers A, C, and D, and Person 2 listed Centers A, C, and E, then 2 of their affiliations overlap.
The goal of this analysis is to determine which socio-demographic and risk-related factors are associated with the likelihood that two participants share similar profiles of health center affiliation. If we were to find that HIV status is significantly associated with this dependent variable, then it would mean that HIV positive and HIV negative BMSM tend to affiliate with different centers. In other words, the analysis is designed to detect a split or partitioning in the network that signals differential affiliation with certain health centers based on individual attributes.
Independent Variables
Several socio-demographic and risk-related factors could lead to differential health center affiliation within the sample of BMSM. Questions assessing socio-demographic characteristics, substance use, risk behavior and HIV status were adapted from the CDC’s National HIV Behavioral Surveillance System, MSM Cycle17 and the visit 51 Core Behavioral survey of the MACS (available at www.jhsph/epi/MACS.edu). Unprotected anal intercourse (UAI) and sex-drug (SD) use18 were measured as in previous work.19 Group sex (GS) was measured as having sex with two or more individuals at the same time. MSM social network size was measured by asking participants to estimate the number of MSM in their community who they know well and with whom they are likely to have contact in the next two weeks.
Data Analysis
Because the observations used to create network variables are not independent, traditional regression techniques are not sufficient. To study the association between individual-level factors and patterns of affiliation with health centers, we used a two-mode network analytic method - Multiple Regression Quadratic Assignment Procedure (MRQAP).20 Like multiple regression analysis, independent variables predict the dependent variable in MRQAP. However, MRQAP is distinguished from traditional multiple regression analysis in that the independent and dependent variables are matrices describing relationships between pairs of participants, which facilitates an analysis in which the dyad (pairs of participants) constitute the unit of analysis. Therefore each MRQAP model related the entire affiliation matrix (containing data on the dependent variable) to each of the matrices of independent variables. Because the observations are not independent of each other, MRQAP generates random permutations of the independent matrix and then computes the regression and saves the resulting r2 values and all coefficients. Low proportions of random permutations, such as less than 0.05, suggest that there is a low likelihood that the relationship between the matrices of interest occurred by chance, and thus a significant relationship is suggested.21, 22 Regression coefficients with 95% confidence intervals (95% CI) were reported for all models with p values less than 0.05 considered statistically significant. UCINET version 6.174 was utilized for all MRQAP analyses.20
In addition, we constructed two-mode affiliation network graphs8 to visualize how health center affiliation is associated with each of the individual-level factors that were associated with utilization patterns in the MRQAP analysis. For instance, because HIV status is significantly associated with patterns of utilization according to the MRQAP analysis, the two-mode networks of health center utilization were stratified by HIV status for comparison of utilization patterns. All two-mode affiliation networks were visualized using NetDraw 2.083.20
At the final stage, we identified health centers that emerge as particularly integral to specific subgroups within the BMSM population. To compare the stratified network graphs, we computed degree centrality and conducted a faction analysis in UCINET. Degree centrality is defined as the number of ties to a person or setting;8 and in this instance the number of participants tied to a particular healthcare setting. This makes it possible to identify the most utilized healthcare setting among participants sharing certain individual-level characteristics, such as HIV status. A faction analysis further divided the network into factions based on the number of links between nodes.23 Nodes (e.g., healthcare centers) with strong indirect connections to each other are placed in the same faction, in which an indicator is used to represent each faction in the network. Health centers that share a significant number of participants are placed in the same faction, while health centers that do not share a significant number of participants are placed in separate factions.
RESULTS
Characteristics of study participants (n=204) are displayed in Table 1. We enrolled 204 BMSM, including 21 seeds, and an average of 23 individuals across 9 RDS waves. 68% of the sample was under 30 years of age, 23% had previously enrolled in an HIV prevention program and 44% self-reported HIV infected status. Characteristics of the nine Chicago health centers offering HIV services are described in Table 2. Three of the centers were classified as public clinics, one as a private clinic and five as community based organizations. Four were located on the South side, three on the North side and two on the West side of the city.
Table 1.
Selected characteristics of Black Men who Have Sex with Men living in Chicago (N=204)
| n(%) | |
|---|---|
| Age | |
| <20 | 26(13.3) |
| 20-24 | 50(25.6) |
| 25-34 | 41(21.0) |
| 35-5 | 47(24.1) |
| 46+ | 31(15.9) |
| Education | |
| Less than high school | 26(12.8) |
| High School or equivalent | 75(36.8) |
| Some College/Post high school certification | 89(43.6) |
| Degree Granted | 14(6.9) |
| Employment status | |
| Currently Employed | 81(39.7) |
| HIV Prevention Program | |
| Ever enrolled | 46(23.4) |
| Self-reported HIV status | |
| HIV positive | 88(44.4) |
| Size of MSM Social Network | |
| <5 | 54(26.5) |
| 5-9 | 43(21.1) |
| 10-20 | 79(38.7) |
| >20 | 28(13.7) |
| Risk Behaviors a | |
| Sex Drug Use | 77(37.8) |
| Unprotected Anal Intercourse | 72(35.8) |
| Group Sex | 45(22.3) |
previous month
Table 2.
Chicago Health Centers, (A-J) by organizational-level characteristics (n=9) and participant report (n=204).
| Health Centers | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Organization-Level Characteristics | A | B | C | D | E | F | G | H | J |
| Center Type a | Public | Public | CBO | CBO | CBO | Public | CBO | CBO | Private |
| Services Offered b | P/T | T | P | P | P/T | T | P | P/T | T |
| Location c | W | W | N | S | N | S | S | N | S |
| Participant has heard of Center (%) | 67.7 | 95.5 | 61.5 | 54.1 | 79.1 | 82.0 | 53.0 | 45.3 | 93.0 |
| Participant has utilized Center (%) | 45.9 | 70.3 | 46.4 | 43,4 | 59.9 | 54.3 | 31.8 | 27.6 | 57.6 |
| Participant ivitli positive immersion (%) | 40.8 | 25.3 | 26 7 | 35.0 | 50.0 | 21 4 | 325 | 33.8 | 61.6 |
Public = Public Clinic; Private = Private Clinic: CBO = Community-Based Organization.
P = Prevention Services; T = Treatment Services; P/T = Prevention and Treatment Servicer. Prevention services include any of the following: effective behavioral interventions (EBI). pre-exposure or post-exposure prophylaxis (PEP/PrEP), prevention for positives programming. Treatment services include health care providers able to prescribe antiretroviral based HIV treatment.
W = west side; N = north side; S = south side
The MRQAP analyses presented in Table 3 identifies individual-level factors associated with differential affiliation with the nine health centers. Individual-level factors significantly associated with the affiliation network of utilization of Chicago health centers included: age (coeff., 0.13; p<0.05), HIV status (coeff., 0.27, p<0.001) and size of MSM social network (coeff., 0.20; p<0.01). In other words, BMSM who are in the same age group, who have the same HIV status (positive or negative), and/or who have similarly sized social networks, are significantly more likely to utilize the same health centers as each other than are BMSM who are from different age groups, who have different HIV statuses, or who have differently sized social networks.
Table 3.
Multiple Regression Quadratic Assignment Procedure for individual-level characteristics on the affiliation networks of awareness and utilization of health centers.
| Awareness Modela | Utilization Modelb | |
|---|---|---|
|
| ||
| Coefficient | Coefficient | |
| Individual-level characteristics | ||
| Demographic Information | ||
| Age | 0.16** | 0.13* |
| Education | 0.16** | 0.10 |
| Employment | 0.01 | 0.02 |
| HIV status | 0.32*** | 0.27*** |
| MSM social network size | 0.25** | 0.20** |
| HIV prevention behavior | ||
| Prevention Program | 0.12* | 0.08 |
| Risk Behavior | ||
| Sex-drug use | 0.04 | 0.08 |
| UAI | −0.04 | −0.01 |
| Group sex | 0.14** | −0.02 |
All individual-level, characteristics are included in each of rhe two models.
Awareness model refers to affilation matrix created from tlie question. “Which of the following nine Chicago health centers have you heard of?”
Utilization model refers to the affiliation matrix created from the question, “Which of the following nine Chicago health centers have you been to?”
P <.05.
P<.01.
P<.001.
HTV - Human Immunodeficiency Virus; MSM - Men who have sex with men; UAI - Unprotected Anal Intercourse
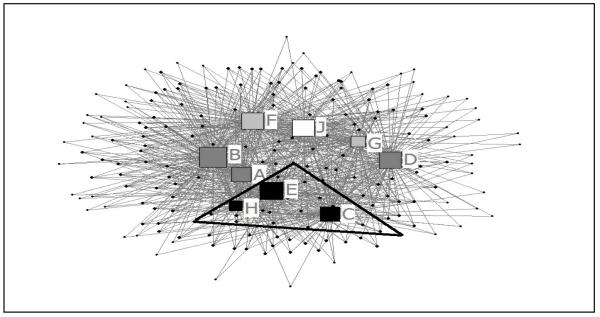
To illustrate the utilization patterns of the overall network, the network of health center affiliations for all 204 participants are graphed in Figure 1. Nodes C, E, and H (in black) represent North Side health centers and are located within the same faction according to the faction analysis. The triangle encompasses these health centers from the same faction. Nodes F, G, and J represent health centers on the South Side and comprise the remaining two factions. This suggests that BMSM affiliate with health centers based upon a geographical distribution (North, South or West).
Figure 1.
Two-mode affiliation network of health center utilization in Chicago Illinois.
Square nodes represent health centers and small circular nodes represent participants. Colors indicate factions (HHCs sharing same participants); and size of nodes reflect degree centrality (number of HHC nominations received). Affiliations are represented by grey edges, which connect participants with utilized health centers. Referring to Table 2, nodes C, E, and H (in black) represent north side health centers and are located within the same faction according to the faction analysis. The triangle encompasses these health centers from the same faction. Meanwhile Nodes A and B represent health centers on the west side and are located within the same faction, in addition to health center on the south side represented by node D. Nodes F, G, and J represent health centers on the south side and comprise the remaining two factions. This suggests that BMSM affiliate with health centers based upon a geographical distribution.
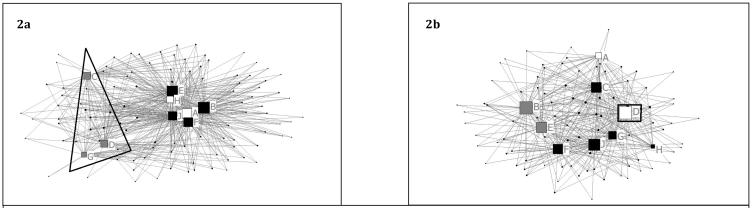
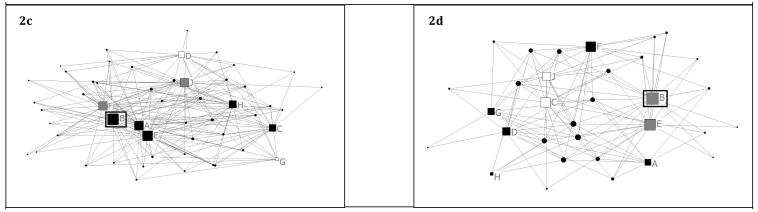
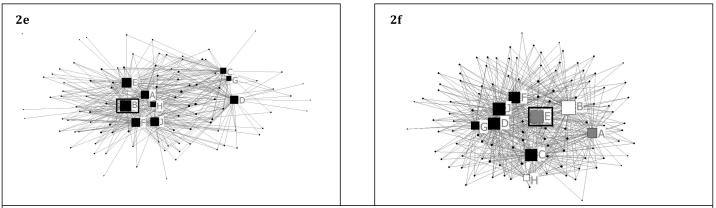
In order to distinguish further between the utilization patterns of BMSM with specific individual-level characteristics, we constructed additional two-mode graphs based on variables that were statistically significant in the MRQAP analysis. We constructed sets of two-mode matrices that were: (1) stratified by HIV status; (2) stratified by HIV status limited to participants practicing UAI within the past 12 months; and 3) stratified by social network size (Figure 2, panels a-f). In the graph of HIV+ participants (Figure 2a), nodes C, D, and G are CBOs offering prevention services only, including prevention for positives, and are located within the same faction on the periphery of the graph (triangle encompasses this faction) and are with lower degree centrality (fewer nominations). The nodes composing the other two factions are located at the core of the network and represent health centers offering treatment services. In the graph of HIV negative participants (Figure 2b), node D (squared), a CBO offering prevention services, is the most popular health center according to the in-degree centrality measure (.63). Patterns of affiliation based upon computation of faction membership (HHCs sharing same participants) and degree centrality (number of HHC nominations received) become apparent; demonstrating that sub-groups of BMSM may not be utilizing centers with prevention services appropriate for their statuses. For example, in Figure 2d, a public clinic that does not offer HIV prevention services has the highest degree centrality (most popular) for HIV negative participants that engage in high-risk behavior. In the graph of participants with a small MSM social network (Figure 2e), a public clinic that provides only treatment services has the highest degree centrality, and faction analysis does not distinguish between health centers. In figure 2f, the graph of participants with a large MSM social network, node E, a CBO has the highest degree centrality within the affiliation network and provides both prevention and treatment services. The faction analysis indicates no specific utilization patterns based on organizational-level characteristics of health centers.
Figure 2.
Two-mode affiliation network of health center utilization stratified by client HIV status (panels a, b), unprotected anal intercourse (panels c, d) and social network size (panels e, f).
Figure 2a,b Two-mode affiliation networks of health center utilization of (2a) HIV+ participants and (2b) HIV-participants. (2a) In the graph of HIV+ participants, nodes C, D, and G are CBOs offering prevention services only, including prevention for positives, and are located within the same faction on the periphery of the graph (triangle encompasses this faction) and are with lower degree centrality (fewer nominations). The nodes composing the other two factions are located at the core of the network and represent health centers offering treatment services. (2b) In the graph of HIV negative participants, node D (squared), a CBO offering prevention services, is the most popular health center according to the in-degree centrality measure (.63).
Figure 2c,d Two-mode affiliation networks of health center utilization of (2c) HIV positive participants that practice UAI and (2d) HIV negative participants that practice UAI. In both networks, node B, a public clinic offering only treatment services has the highest degree centrality (most nominations). Other centers that provide prevention for positives programming are located on the network periphery (e.g. G). A comparison between Figure 2b and Figure 2d demonstrates that the health center utilization patterns of HIV negative participants is distinguished according to high risk behavior. While a CBO has the highest degree centrality for all HIV negative participants, a public clinic has the highest degree centrality for HIV negative participants that engage in high risk behavior. The highest risk HIV uninfected BMSM affiliate most with the health center not offering prevention services.
Figure 2 e,f Two-mode affiliation networks of health center utilization of (2e) participants with a small MSM social network (less than 10 MSM) and (2f) participants with a larger MSM social network (10 or more MSM). (2e) In the graph of participants with a small MSM social network, a public clinic that provides only treatment services has the highest degree centrality, and faction analysis does not distinguish between health centers. (2f) In the graph of participants with a large MSM social network, node E, a CBO has the highest degree centrality within the affiliation network and provides both prevention and treatment services. The faction analysis indicates no specific utilization patterns based on organizational-level characteristics of health centers.
DISCUSSION
In response to the number of studies that underscore the contribution of limited health care access to the HIV disparity among Black MSM24-26, we aimed to take a new approach to clarify multiple competing individual and organizational-level factors of utilization of health centers in a large urban setting. While a few researchers have applied an affiliation network approach to describe the role that venues play in disease transmission27, or tobacco control28, no published studies that we are aware of have employed affiliation network analysis to identify factors associated with patterns of health service utilization. Using this approach, we were able to identify several important individual- and organization-level factors that shape patterns of contact of BMSM with a range of health centers offering HIV services. We found that, in aggregate, BMSM depict a pattern of HHC affiliation based upon their age, HIV status and social network size. Analysis of health center grouping, however, demonstrates that a sub-group of high-risk uninfected men affiliate less with centers providing HIV prevention services. Similarly, BMSM who are HIV positive, and who have smaller social networks utilize public or private health clinics only offering treatment services. HIV prevention centers that provide specialized HIV prevention for positive programming, however, were not affiliated with these HIV infected participants.
HIV Status and Utilization
In contrast to the utilization patterns of HIV uninfected participants, HIV infected BMSM in our study reported limited engagement with health centers offering HIV prevention programs, including prevention for positives. In the affiliation network of HIV uninfected participants, a CBO offering prevention services has the highest degree centrality and is thus the most utilized center in this subset of participants. Notably, health centers offering prevention services comprise the periphery of the affiliation network of HIV infected participants, while health centers offering treatment services compose the core of the affiliation network. This finding is consistent with previous literature documenting that HIV infected BMSM are less likely to participate in behavioral interventions.29
Role of social support in health center utilization
Our analysis suggests that CBOs play a significant role in health center seeking behaviors of participants with larger MSM social networks. The central location of a CBO in the affiliation network of participants with large MSM social networks suggests that this group of participants utilize CBOs in addition to more traditional health care settings. In contrast, the peripheral position of three CBOs in the affiliation network of participants with smaller MSM social networks suggests that men with smaller networks of social support rely on public and private clinics. Study participants reporting a larger social network of MSM were more likely to have utilized more health centers than study participants with a smaller social network of MSM. This finding is consistent with previous work documenting that individuals with higher levels of social support are more likely to access health care services.30 Social network effects (e.g., friend influence) on health care utilization also occurs across a broad range of non-HIV related settings and clients including participation in influenza vaccine clinics, use of herbal preparations among clients of antenatal clinics, tuberculosis care seeking, and intrauterine device acceptors in a gynecological clinic.
It remains an open question whether individual characteristics lead to selective affiliating (e.g., friends who are similar to each other lead each other to the same centers, or people simply select into centers that seem to cater to their own “type” or their specific needs/problems) or whether the very fact that two people attend the same centers increases the likelihood that they will form a social connection to each other which then somehow influence each other such that they become similar to each other. The fact that from MRQAP analysis risky behavior profiles are not related to persons’ health center affiliation profiles, whereas HIV status is, is very interesting. It might suggest, for example, that health centers that are more associated with HIV infected BMSM are just as useful targets for interventions aimed at reducing risk behavior as are health centers that are more associated with HIV negative BMSM, because risk behavior is not associated with health center affiliation in the same way that HIV status is.
Limitations
There are several limitations. The data are cross-sectional and we cannot determine the impact that exposure to particular health centers may have had on the behavior of study participants. Study participants reported their awareness and utilization of a pre-determined list of health centers offering HIV care which may have excluded other HHCs. However, we selected centers based on discussions with BMSM during focus groups. Additionally, while we describe utilization patterns of health centers and prevention services utilized by participants, we do not explore the quality, timing, or frequency of visits to health centers. However, the results provide critical insight into contact that BMSM have with a range of health centers. Our narrow definition of HIV prevention might have limited some centers inclusion as prevention centers even if they provided standard of care risk-reduction counseling for HIV infected clients. Finally, the study took place in one city potentially limiting its generalizability. However, health care centers described in this analysis were categorized by typology, and are similar to those in other urban settings.
Our findings suggest that patterns of health care utilization among BMSM in Chicago are structured by several individual-level characteristics. Sub-categories of BMSM in this sample affiliated with HIV health centers that may not provide appropriate HIV prevention services. Given the strong affiliation of HIV infected BMSM with public and private clinics offering treatment services, future studies should consider the degree to which HIV infected BMSM receive behavioral interventions in public and private clinic settings (prevention for positives); and whether CBOs should shift focus to provide such programming to target specific clients with for example, smaller social networks. Public health authorities could better match prevention services to both HIV infected and uninfected BMSM need. Lack of knowledge of the networked pattern of HIV health center utilization could allow resource allocation to all HCCs, and matching of appropriate HHC services to specific clients is critical in an environment of constrained resources.
ACKNOWLEDGEMENTS
This work was funded by grants from the National Institutes of Health (U54 RR023560 and R03 DA026089).
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Prejean J, Ruiguang S, Hernandez A, et al. Estimated HIV Incidence in the United States, 2006-2009. PLoS ONE. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. doi:10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDPH . HIV Prevalence and Unrecognized Infection among Men Who Have Sex with Men – Chicago. Chicago Department of Public Health; Chicago: 2008. [Google Scholar]
- 3.Millett GA, Ding H, Marks G, et al. Mistaken Assumptions and Missed Opportunities: Correlates of Undiagnosed HIV Infection among Black and Latino Men who have Sex with Men. J Acquir Immune Defic Syndr. 2011 Jun 7; doi: 10.1097/QAI.0b013e31822542ad. [DOI] [PubMed] [Google Scholar]
- 4.Oster AM, Wiegand RE, Sionean C, et al. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS. 2011 May 15;25(8):1103–1112. doi: 10.1097/QAD.0b013e3283471efa. [DOI] [PubMed] [Google Scholar]
- 5.Mimiaga MJ, Reisner SL, Cranson K, et al. Sexual mixing patterns and partner characteristics of black MSM in Massachusetts at increased risk for HIV infection and transmission. Journal of Urban Health. 2009;68(4):602–623. doi: 10.1007/s11524-009-9363-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magnus M, Jones K, Phillips G, 2nd, et al. Characteristics associated with retention among African American and Latino adolescent HIV-positive men: results from the outreach, care, and prevention to engage HIV-seropositive young MSM of color special project of national significance initiative. Journal of Acquired Immune Deficiency Syndromes. 2010 Apr 1;53(4):529–536. doi: 10.1097/QAI.0b013e3181b56404. [DOI] [PubMed] [Google Scholar]
- 7.Johnson RL, Botwinick G, Sell RL, et al. The utilization of treatment and case management services by HIV-infected youth. Journal of Adolescent Health. 2003 Aug;33(2 Suppl):31–38. doi: 10.1016/s1054-139x(03)00158-7. [DOI] [PubMed] [Google Scholar]
- 8.Wasserman S, Faust K. Social Network Analysis: Methods and Applications. First ed Cambridge University Press; Cambridge,UK: 1994. [Google Scholar]
- 9.Heckathorn D. Respondent-Driven Sampling: A New Approach to the Study of Hidden Populations. Social Problems. 1997;44(2) [Google Scholar]
- 10.Heckathorn DD. Respondent-driven sampling II: deriving valid population estimates from chain-referral samples of hidden populations. Social Problems. 2002;49(1):11–34. [Google Scholar]
- 11.Iguchi MY, Ober AJ, Berry SH, et al. Simultaneous recruitment of drug users and men who have sex with men in the United States and Russia using respondent-driven sampling: sampling methods and implications. Journal of Urban Health. 2009;86(1):S5–S31. doi: 10.1007/s11524-009-9365-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnston LG, Khanam R, Reza M, et al. The effectiveness of respondent driven sampling for recruiting males who have sex with males in Dhaka, Bangladesh. AIDS and Behavior. 2008;12(2):294–304. doi: 10.1007/s10461-007-9300-1. [DOI] [PubMed] [Google Scholar]
- 13.Ramirez-Valles J, Heckathorn DD, Vázquez R, Diaz RM, Campbell RT. From networks to populations: the development and application of respondent-driven sampling among IDUs and Latino gay men. AIDS and Behavior. 2005;9(4):387–402. doi: 10.1007/s10461-005-9012-3. [DOI] [PubMed] [Google Scholar]
- 14.Mimiaga MJ, Goldhammer H, Belanoff C, Tetu AM, Mayer KH. Men who have sex with men: perceptions about sexual risk, HIV and sexually transmitted disease testing, and provider communication. Sexually Transmitted Diseases. 2007;34(2):113–119. doi: 10.1097/01.olq.0000225327.13214.bf. [DOI] [PubMed] [Google Scholar]
- 15.Gile KJ, Handcock KS. Respondent-driven sampling: an assessment of current methodology. Sociological Methodology. 2010;40(1):285–327. doi: 10.1111/j.1467-9531.2010.01223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goel S, Salganik MJ. Respondent-driven sampling as Markov chain Monte Carlo. Statistics in Medicine. 2009;28(17):2202–2229. doi: 10.1002/sim.3613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanchez T, Finlayson T, Drak A, et al. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors--United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003-April 2005. MMWR Surveill Summ. 2006;55(6):1–16. [PubMed] [Google Scholar]
- 18.Ostrow DG, Stall RC. Alcohol, tobacco, and drug use among gay and bisexual men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal Opportunity: Health Disparities Affecting Gay and Bisexual Men in the United States. Oxford University Press; Oxford,UK: 2008. pp. 121–158. [Google Scholar]
- 19.Ostrow DG, Plankey MW, Cox C, et al. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. Journal of Acquired Immune Deficiency Syndromes (1999) 2009;51(3):349–355. doi: 10.1097/QAI.0b013e3181a24b20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borgatti SP, Everett MG, Freeman LC. UCINET for Windows: Software for social network analysis. Harvard Analytic Technologies. 2002;2006 [Google Scholar]
- 21.Borgatti SP, Everett MG, Freeman LC. UCINET VI for Windows: Software for social network analysis. Harvard Analytic Technologies. 1999 [Google Scholar]
- 22.Labianca G, Brass DJ, Gray B. Social networks and perceptions of inter-group conflict: The role of negative relationships and third parties. Academy of Management Journal. 1998;41:55–67. [Google Scholar]
- 23.Borgatti SP, Everett MG. Network analysis of 2-mode data. Social Networks. 1997;19:243–269. [Google Scholar]
- 24.Malebranche DJ. Black men who have sex with men and the HIV epidemic: next steps for public health. Americal Journal of Public Health. 2003 Jun;93(6):862–865. doi: 10.2105/ajph.93.6.862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crosby R, Holtgrave DR, Stall R, Peterson JL, Shouse L. Differences in HIV risk behaviors among black and white men who have sex with men. Sex Transm Dis. 2007 Oct;34(10):744–748. doi: 10.1097/OLQ.0b013e31804f81de. [DOI] [PubMed] [Google Scholar]
- 26.Hall HI, Byers RH, Ling Q, Espinoza L. Racial/ethnic and age disparities in HIV prevalence and disease progression among men who have sex with men in the United States. American Journal of Public Health. 2007 Jun;97(6):1060–1066. doi: 10.2105/AJPH.2006.087551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frost SDW. Using sexual affiliation networks to describe the sexual structure of a population. Sex Transm Infect. 2007 Aug 1;83:I37–I42. doi: 10.1136/sti.2006.023580. [DOI] [PubMed] [Google Scholar]
- 28.Wipfli HL, Fujimoto K, Valente TW. Global tobacco control diffusion: the case of the framework convention on tobacco control. American Journal of Public Health. 2010 Jul;100(7):1260–1266. doi: 10.2105/AJPH.2009.167833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hatfield LA, Ghiselli ME, Jacoby SM, et al. Methods for Recruiting Men of Color Who Have Sex with Men in Prevention-for-Positives Interventions. Prev Sci. 2010 Mar;11(1):56–66. doi: 10.1007/s11121-009-0149-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Merighi JR, Chassler D, Lundgren L, Inniss HW. Substance use, sexual identity, and health care provider use in men who have sex with men. Subst Use Misuse. 2011;46(4):452–459. doi: 10.3109/10826084.2010.502208. [DOI] [PubMed] [Google Scholar]