SUMMARY
The severe atrophy of the jaws are a challenging therapeutic problem, since the increase in bone is necessary to allow the placement of a sufficient number of implants. Combining immediate functionalization with the concept of guided surgery they combine the advantages offered by the innovative surgical and prosthetic implant technique (All-on-Four®) with those of computer-assisted planning in cases of severe bone atrophy. The method used in this case report, combines these two concepts in a surgical and prosthetic protocol safe and effective for the immediate function of 4 implants to support a fixed prosthesis in completely edentulous subjects. The integration of technology with immediate function with the concept of computer-guided surgery for implant placement and rehabilitation of completely edentulous jaws is now a predictable treatment modality with implant survival comparable to the traditional protocols.
Keywords: tilted implants, immediate loading, guided surgery
RIASSUNTO
Le gravi atrofie dei mascellari costituiscono un problema terapeutico impegnativo, in quanto l'incremento osseo è necessario per consentire il posizionamento di un numero sufficiente di impianti, secondo le necessità protesiche. Associando la funzionalizzazione immediata con il concetto di chirurgia guidata si uniscono i vantaggi chirurgici e protesici offerti dall’innovativa metodica implantare (All-on-Four®), con quelli della programmazione computer-assistita anche in casi di severa atrofia ossea. La metodica utilizzata in questo caso clinico, unisce questi due concetti in un protocollo chirurgico e protesico sicuro ed efficace per la funzione immediata di 4 impianti (BTLock®) a sostegno di una protesi fissa in soggetti completamente edentuli. L'integrazione della tecnica a funzione immediata con il concetto di chirurgia computer-guidata (SimPlant, Materialise®) per il posizionamen-to dell'impianto e per la riabilitazione delle mascelle completamente edentule è attualmente una modalità di trattamento prevedibile con una sopravvivenza implantare sovrapponibile ai protocolli tradizionali.
Introduction
The implant-prosthetic technique introduced by Malò in 2003 is one of the most modern innovations of recent years in implant-prosthetic rehabilitation of the atrophic maxilla, with very high success rate in the short to medium term follow-up observed to date.
The technique provides for the inclusion of only four pillars within intraforaminal implant in the mandible and in the pre-maxilla, which support a fixed prosthesis type screw, which are under immediate loading. The two systems are orthogonal to the occlusal plane mesial and distal 2 are tilted at 45 ° to the bone.
This technique, despite the low period of follow-up, but thanks to the simplicity of the surgical protocol, the minimal invasiveness and the possibility of applying the implants under immediate load is widespread, with a satisfactory functionally and aesthetically and reduced processing time of biological and economic costs.
By combining the technique All-on-Four with the concept of guided surgery combine the advantages offered by the innovative surgical technique and prosthetic implant with the programming computer-assisted functionalization and immediate offered by guided surgery systems currently present on the market. The severely atrophied maxilla is a challenging therapeutic problem, because bone growth is necessary to allow placement of a sufficient number of plants as needed prostheses. Several surgical procedures have been developed to improve the quality and the volume osseo.1 technique maxillary sinus for bone regeneration is validated as a treatment option, but acceptance of this procedure for patients could be lower, because of their invasive nature associated with an increased risk of morbidity, reducing comfort and increasing costs, 2–4 is also recommended a two-stage procedure with delayed implant placement to get the successo (5, 6).
To overcome these drawbacks, some authors have suggested alternative anatomical regions to place the implant, such as front or rear wall of the womb, the septa of the breast, the curvature of palatal and pterygoid process (7–9).
It has been proposed to tilt the system in bone windows to avoid the use of anatomical innesti (10–12). The technique of inclined lifts has been developed to improve the anchoring and support bone implants, minimizing the overhang and avoiding sinus bone grafting procedures and 8.11. Using plants inclined (> 15 ° angle to the occlusal plane) in one direction or mesiodistale or a buccopalatal angle, you can put plants closer to the front and back walls of the maxillary sinus. The success rate at 5 years for installations angle varies from 95.2 to 98.9% and 91.3 to 93% for plants assiali (13, 14).
The results of biomechanical analysis indicate that the tilt facility has no adverse effect on bone resorption. Following this approach allows the system tilted to extend support prosthetic posterior, thereby reducing the cantilever.
The technique of the most distal tip of the plants can be achieved if the doctor chooses immediate or delayed implant loading. The concept of immediate function, which involves the simultaneous placement of implants, abutments and restorations (temporary or permanent), shows promising results with few complications (15–20).
The technique All-on-Four with immediate function combines these two concepts in a surgical and prosthetic protocol safe and effective for immediate function of 4 implants to support a fixed prosthesis in a completely edentulo (21, 22).
The integration of technology at All-on-Four immediate function with the concept of computer-guided surgery for implant placement and rehabilitation of completely edentulous jaws is a predictable treatment modality with a very high implant survival (23).
Tilt systems, parallel to the front and back walls of the breast, in a correct biomechanical position with good primary stability of 19–23 seems to be easier, indeed requires a high level of surgical skill and can be invasive breast procedures such as transplantation. Angle of the front wall of the breast has been viewed through a hole in the side of the breast and the implant was placed in parallel and close to it. Thus, this system has been tilted distally about 30–35 degrees. This technique provides the following three advantages: (1) support system is moved posteriorly, (2) implant length increased, and (3) the system follows a dense bone structure, the anterior wall of the womb, thus increasing the stability primary. If a patient has a number of sufficient bone in the tuberosity, a similar procedure was performed for placement of a plant before sloping back wall near the breast 8. The advent of 3-dimensional computer-guided optimizes treatment planning, allowing the doctor to put plants in an angle based on anatomical and prosthetic needs with high accuracy and low invasiveness (24–26).
The prosthetic restoration on implants slope is challenging for both the dentist and technician. After implantation, the angle can be easily compensated using angled abutments. CAD-CAM allows production of custom columns by changing the angle of inclination of implants according to prosthetic emergence profile. The prosthetic rehabilitation can be delivered using an approach delayed loading or immediate loading approach. To minimize mechanical complications and provide rigid support for plants, especially in the case of immediate loading, it is always recommended to strengthen the superstructure with a metal frame (21, 22).
Materials and methods
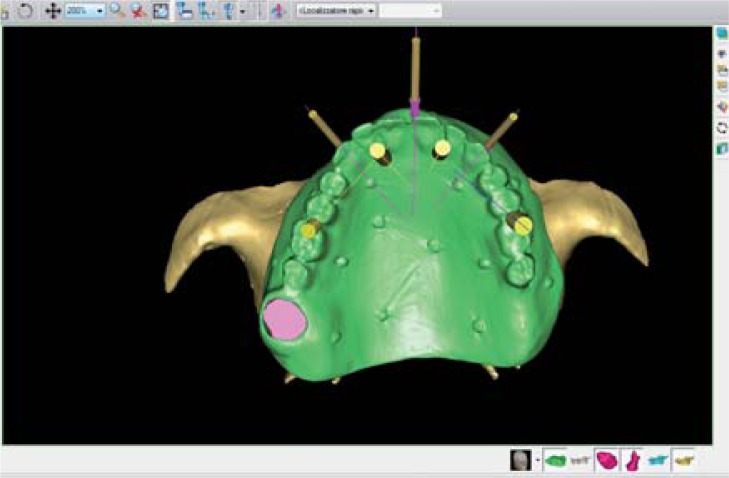
The computer-assisted planning system used in this study is the SimPlant® (materiality, Technologielaan 15, 3001 Leuven, Belgium) and was the first virtual planning system introduced on the market. The software interacts with most X-ray computed tomography systems commercially available 23. The data obtained from CT are introduced in the software that displays both axial cross sections, 3D front and interactively with each other (Fig. 1). The placement of virtual systems can therefore be controlled simultaneously in different projections. The image can be rotated in different planes, allowing a complete spatial vision real anatomy (Figs. 2,3,4,5). The software allows a good approximation to evaluate the bone quality of the 24 sites surveyed. The program is applicable to most implant systems. It is equipped with a library which is stored almost all the plants more widespread. These are represented by their real shape, so the clinician can make a realistic virtual surgery through the overlap of the silhouette of the plant on the corresponding section of bone. You can control the input from various angles simultaneously, it is immediate verification of any fenestration, collisions with respect to anatomical structures or other installations that were included (Figs. 6,7). You can simulate also possible reconstructive measures to correct existing volumes if insufficient bone for implant placement. The program can calculate a good approximation of the volumetric extent of the increase necessary, which allows the clinical guidelines on the levy or the amount of material for use homologous or heterologous. The software has a monitoring system that informs in the case of interference between the trajectories chosen implant and anatomical areas at risk (alveolar nerve, maxillary sinus, etc.) (Figs. 8, 9). Also highlights, with a color change, the occurrence of dehiscence, fenestration, and any success from FUO-bone morphology.
Figure 1.
Axial image sections, transverse, frontal and 3D.
Figure 2.
3D image Front.
Figure 3.
3D image occlusal.
Figure 4.
Left lateral 3D image.
Figure 5.
3D image right side.
Figure 6.
Image Section Front.
Figure 7.
Cross-sectional image.
Figure 8.
Axial image.
Figure 9.
Axial image.
The operator has all the information needed to perform a volumetric virtual surgery by inserting the implants in a more congenial bone anatomy. After the virtual planning you can collect the files in a project developed and require the company to build a surgical guide that will allow the operator corresponding to faithfully follow the virtual design.
The workflow of this system is as follows:
The first step is the duplication of complete dentures if the patient is functionally correct, or inserting into it some radiographic secure retrieval.
The patient performs the test with this mask X-ray tomography, stabilized by an arch rival index silicone previously realized.
And have performed a CT scan technique with double images were acquired with a conventional CT scanner (Tomoscan SR-6000, Philips) using a standard dental CT protocol (1.5 mm slice thickness, 1.0 mm of play table, 120 kV, 75 mA, 2 - s scan time, 100 – 120 mm field of view) (25). The first scan was of the maxilla and the design of the model in situ, the second single model of planning. Using the software for treatment planning (SimPlant) we acquired scans we obtained overlapping union of two sets of three-dimensional scans on which sites are designed for positioning equipment. The planning data are transferred to the processing center and production Materialise, which has produced a template surgical precision resin cylindrical guides with titanium. The planned deep osteotomies were determined precisely by cross-sectional images of the site. The planned drilling depth was calculated by adding 10 mm to this value (9 mm distance between the top edge of planned installation and the top tube of titanium, plus 1 mm height of drill guide).
Surgical procedure
One hour before surgery, antibiotic prophylaxis was done with 2 g of amoxicillin and clavulanate (Augmentin, GlaxoSmithKline). It’s been prescribed three days before surgery, based mouthwash chlorhexidine digluconate 0.2% (Corsodyl, GlaxoSmithKline). Before surgery was given local anesthesia with articaine hydrochloride 4% (40 mg / mL) and epinephrine 1:100,000 (Septodont Inc). The surgery was performed by placing 4 implants BTLock (2 rear inclined with Ø4, 5mm x 13mm in length and O3, 75mm x 13mm and 2 front axial both Ø3, 75mm x 13mm) provided anatomical sites with a free flap approach. The protocol drilling is customized based on bone density of the implant site to achieve stability prior to placement with the couple more than 40 Ncm using foam-compactors (BTLock).
Postoperatively, the patient received amoxicillin and clavulanic acid 1 g twice daily for 4 days, then b 0.5 g daily for 3 days. B chlorhexidine daily for 10 days. The pillars prefabricated CAD / CAM have been established for facilities with dedicated prosthetic titanium screws tightened with a torque of 30 Ncm. The reinforced acrylic resin provisional restoration with cast metal substructure was immediately delivered to the patient. The installation of the temporary restoration allowed to offset any loss of precision positioning system. The marginal accuracy, retention and stability were improved by a rebasement with a self-curing polyurethane resin (Voco, GmbH). The temporary prosthesis was fixed with a cement phosfate zinc mixed with 30% petroleum jelly.
All centric and lateral contacts were evaluated with articulating paper 40 microns (Bausch) and adjusted to obtain a correct occlusal contact.
Conclusions
The case suggests that immediate loading associated with tilted implants prosthesis can be considered a viable treatment modality for the atrophic maxilla.
These results indicate that if the prerequisites for immediate loading as high primary stability (30Ncm or more), splinting of the implants through a temporary prosthesis and the use of an osteoconductive surface are satisfied, the tilt of the plant may not affect results of the final result.
Analysis of the case shows that the use of guided surgery system for positioning and axial tilt and predictable, while reducing surgical invasiveness. This treatment option is an effective and biologically useful alternative to the procedures for increasing the sinus floor. Thanks to recent computer-assisted methods is now possible to place implants in an “anatomically optimized”, using all the available bone in accordance with the noble vascular and nerve structures and the maxillary sinus, while taking into account the needs prosthetic. Finally, we must emphasize that the use of computer-assisted methods and surgery without flap, despite represents an obvious simplification of surgical and prosthetic procedures, requires some experience in the planning and execution of the case.
Figure 10.
Kit BTLock-Guide.
Figure 11.
Drill-guide color code BTLock.
Figure 12.
Expanding-condensing osteotomes BTlock.
Figure 13.
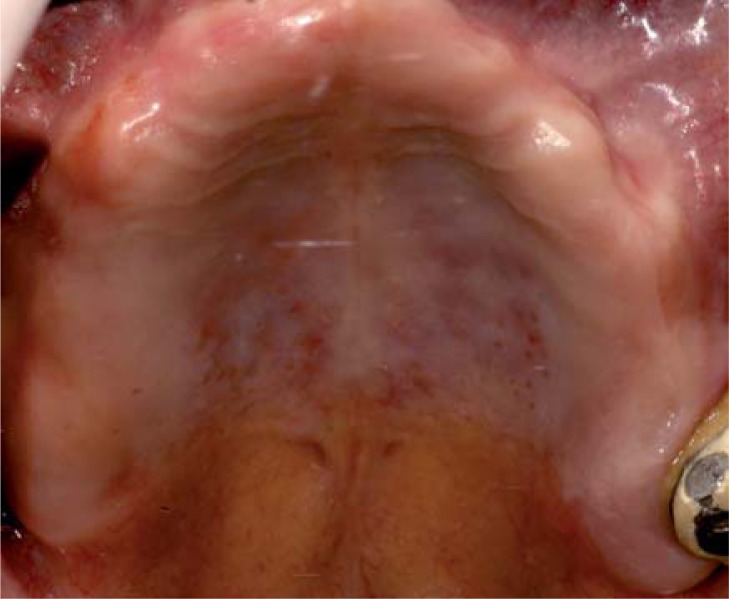
Intraoral view.
Figure 14.
Preoperative intraoral view.
Figure 15.
Preoperative occlusal view.
Figure 16.
Surgical Template.
Figure 17.
Preparation of anchor pins.
Figure 18.
Positioning anchor pins.
Figure 19.
Mechanical circular blade.
Figure 20.
Implant site preparation through pilot drill and drill-guides.
Figure 21.
Implant site preparation through drill ø 3.3 mm.
Figure 22.
Implant site preparation using drill ø 3.75 mm.
Figure 23.
Implant site preparation using expanding-condensing osteotomes.
Figure 24.
The manual installation of implants.
Figure 25.
Implant inserted with reference mounter.
Figure 26.
Removing anchor pins after placement of implants.
Figure 27.
Post-surgery intraoral view.
Figure 28.
Titanium abutments in situ.
Figure 29.
Post-surgery rx control.
Figure 30.
Final aesthetics result.
References
- 1.Esposito M, Hirsch JM, Lekholm U, Thomsen P. Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur J Oral Sci. 1998;106:527–551. doi: 10.1046/j.0909-8836..t01-2-.x. [DOI] [PubMed] [Google Scholar]
- 2.Cricchio G, Lundgren S. Donor site morbidity in two different approaches to anterior iliac crest bone harvesting. Clin Implant Dent Relat Res. 2003;5:161–169. doi: 10.1111/j.1708-8208.2003.tb00198.x. [DOI] [PubMed] [Google Scholar]
- 3.Nkenke E, Schultze-Mosgau S, Radespiel-Troger M, Kloss F, Neukam FW. Morbidity of harvesting of chin grafts: a prospective study. Clin Oral Implants Res. 2001;12:495–502. doi: 10.1034/j.1600-0501.2001.120510.x. [DOI] [PubMed] [Google Scholar]
- 4.Clavero J, Lundgren S. Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: comparison of donor site morbidity and complications. Clin Implant Dent Relat Res. 2003;5:154–160. doi: 10.1111/j.1708-8208.2003.tb00197.x. [DOI] [PubMed] [Google Scholar]
- 5.Lundgren S, Nystrom E, Nilson H, Gunne J, Lindhagen O. Bone grafting to the maxillary sinuses, nasal floor and anterior maxilla in the atrophic edentulous maxilla. A two-stage technique. Int J Oral Maxillofac Surg. 1997;26:428–434. doi: 10.1016/s0901-5027(97)80007-0. [DOI] [PubMed] [Google Scholar]
- 6.Lundgren S, Rasmusson L, Sjostrom M, Sennerby L. Simultaneous or delayed placement of titanium implants in free autogenous iliac bone grafts. Histological analysis of the bone graft-titanium interface in 10 consecutive patients. Int J Oral Maxillofac Surg. 1999;28:31–37. [PubMed] [Google Scholar]
- 7.Fortin Y, Sullivan RM, Rangert BR. The Marius implant bridge: surgical and prosthetic rehabilitation for the completely edentulous upper jaw with moderate to severe resorption: a 5-year retrospective clinical study. Clin Implant Dent Relat Res. 2002;4:69–77. doi: 10.1111/j.1708-8208.2002.tb00155.x. [DOI] [PubMed] [Google Scholar]
- 8.Krekmanov L. Placement of posterior mandibular and maxillary implants in patients with severe bone deficiency: A clinical report of procedure. Int J Oral Maxillofac Implants. 2000;15:722–730. [PubMed] [Google Scholar]
- 9.Calandriello R, Tomatis M. Simplified treatment of the atrophicposterior maxilla via immediate/early function and tilted implants: A prospective 1-year clinical study. Clin Implant Dent Relat Res. 2005;7(supp1):S1–S12. doi: 10.1111/j.1708-8208.2005.tb00069.x. [DOI] [PubMed] [Google Scholar]
- 10.Mattsson T, Köndell P-A, Gynther GW, Fredholm U, Bolin A. Implant treatment without bone grafting in severely resorbed edentulous maxillae. J Oral Maxillofac Surg. 1999;57:281–287. doi: 10.1016/s0278-2391(99)90673-0. [DOI] [PubMed] [Google Scholar]
- 11.Aparicio C, Perales P, Rangert B. Tilted implants as an alternative to maxillary sinus grafting. J Clin Implant Dent Relat Res. 2001;3(1):39–49. doi: 10.1111/j.1708-8208.2001.tb00127.x. [DOI] [PubMed] [Google Scholar]
- 12.Aparicio C, Arévalo JX, Ouazzani W, Granados C. Retrospective clinical and radiographic evaluation of tilted implants used in the treatment of the severely resorbed edentulous maxilla. Applied Osseo Res. 2002;3:17–21. [Google Scholar]
- 13.Zampelis A, Rangert B, Heijl L. Tilting of splinted implants for improved prosthodontic support: a two-dimensional finite element analysis. J Prosthet Dent. 2007;97(suppl 6):S35–S43. doi: 10.1016/S0022-3913(07)60006-7. [DOI] [PubMed] [Google Scholar]
- 14.Krekmanov L, Kahn M, Rangert B, Lindström H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000;15:405–414. [PubMed] [Google Scholar]
- 15.van Steenberghe D, Glauser R, Blomback U, et al. A computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae: a prospective multicenter study. Clin Implant Dent Relat Res. 2005;7(suppl 1):S111–S120. doi: 10.1111/j.1708-8208.2005.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 16.Becker W, Doerr J. Three-dimensional software for fabrication of a surgical template and final implant-supported restoration for a fully edentulous maxilla: a case report. Compend Contin Educ Dent. 2005;26:802, 804–807. [PubMed] [Google Scholar]
- 17.Balshi SF, Wolfinger GJ, Balshi TJ. Surgical planning and prosthesis construction using computer technology and medical imaging for immediate loading of implants in the pterygomaxillary region. Int J Periodontics Restorative Dent. 2006;26:239–247. [PubMed] [Google Scholar]
- 18.Kan JY, Rungcharassaeng K, Oyama K, et al. Computer-guided immediate provisionalization of anterior multiple adjacent implants: surgical and prosthodontic rationale. Pract Proced Aesthet Dent. 2006;18:617–623. [PubMed] [Google Scholar]
- 19.Kupeyan HK, Shaffner M, Armstrong J. Definitive CAD/CAM-guided prosthesis for immediate loading of bone-grafted maxilla: a case report. Clin Implant Dent Relat Res. 2006;8:161–167. doi: 10.1111/j.1708-8208.2006.00018.x. [DOI] [PubMed] [Google Scholar]
- 20.Marchack CB, Moy PK. The use of a custom template for immediate loading with the definitive prosthesis: a clinical report. J Calif Dent Assoc. 2003;31:925–929. [PubMed] [Google Scholar]
- 21.Malo P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Branemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(suppl 1):2–9. doi: 10.1111/j.1708-8208.2003.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 22.Malo P, Rangert B, Nobre M. All-on-4 immediate-function concept with Branemark System implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;7(suppl 1):S88–S94. doi: 10.1111/j.1708-8208.2005.tb00080.x. [DOI] [PubMed] [Google Scholar]
- 23.Mupparapu M, Singer SR. Implant imaging for the dentist. J Can Dent Assoc. 2004 Jan;70(1):32. [PubMed] [Google Scholar]
- 24.Norton MR, Gamble C. Bone classification: an objective scale of bone density using the computerized tomography scan. Clin Oral Implants Res. 2001 Feb;12(1):79–84. doi: 10.1034/j.1600-0501.2001.012001079.x. [DOI] [PubMed] [Google Scholar]
- 25.Gahleitner A, Watzek G, Imhof H. Dental CT: Imaging technique, anatomy, and pathologic conditions of the jaws. Eur Radiol. 2003;13:366–376. doi: 10.1007/s00330-002-1373-7. [DOI] [PubMed] [Google Scholar]