Abstract
The potential benefits of fish oil have been touted for several decades. The authors review evidence from epidemiologic, retrospective, and controlled prospective clinical trials demonstrating the effects of omega-3 fatty acids (fish oil) for the prevention of major cardiovascular events including myocardial infarction and stroke in primary and especially secondary prevention settings. Fish oil's efficacy in reducing total mortality and sudden cardiac death appears particularly promising, probably due to potent antiarrhythmic effects. We believe it is now time to consider fish oil therapy, specifically eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), for most patients with known cardiovascular disease and for patients at increased risk for cardiovascular disease, particularly patients at increased risk of sudden cardiac death.
Omega-3 fatty acids, or fish oil, are increasingly being utilized to provide substantial protection against cardiovascular disease. Multiple epidemiological studies (1–8) and randomized controlled trials in Europe, Japan, India, and the United States (9–12) have shown that moderate fish oil consumption, either by eating fatty fish more than once a week or by taking fish oil supplements, decreases the risk of major cardiovascular events, including myocardial infarction (MI), sudden cardiac death, and stroke (13, 14). The American Heart Association (AHA) has recently recognized the potential importance of various polyunsaturated fatty acids (PUFAs) in the protection against major cardiovascular events (15, 16)
What Is Fish Oil?
The most important components of fish oil are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA); two omega-3 PUFAs. The nomenclature is based on the number of carbon atoms counting from the methyl end before one reaches the first C=C double bond; hence, n-6 and n-3 (also referred to as w-6 and w-3). EPA has 20 carbons with 5 unsaturated bonds, and DHA contains 22 carbons with 6 unsaturated bonds. Both have the first double bond at the site omega-3 from the methyl end of the fatty acid.
DHA and EPA are essential fatty acids, meaning the human body is unable to synthesize them except by an elongation process on alpha linolenic acid (ALA), which is another omega-3 PUFA with shorter carbon sequence of 18 carbons and 3 unsaturated bonds. The structure of the two dietary classes of essential PUFAs containing ALA are documented in Figure 1 (17). The n-6 PUFAs are found primarily in vegetable oils and n-3s primarily in marine animals or plants.
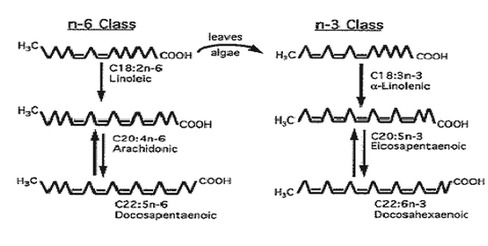
Figure 1: Comparison of the structure of the two dietary classes of essential polyunsaturated fatty acids: n-6 PUFA, found primarily in vegetable oils, and n-3 PUFA, present primarily in fish oils. The nomenclature is based on the number of carbon atoms counting from the methyl end before one reaches the first C=C double bond, hence n-6 and n-3 (also referred to as w-6 and w-3). The figures of the PUFA are drawn to indicate only the number of carbon and the positions of the C=C unsaturated bonds and carry no implication regarding the configuration of each cell within membranes. Reprinted from (17): Kang JX, Leaf A. Circulation 1996; 94: 1774–1780. http://circ.ahajournals.org/content/vol94/issue7/images/large/0005f1.jpeg
Epidemiological Studies and Primary Cardiovascular Prevention
As early as 1944, Sinclair pointed out the rarity of coronary artery disease (CAD) in Greenland Eskimos despite their consumption of a diet known to be high in fat (1). CAD is also less prevalent in Japan, whose population has traditionally consumed more fish than populations in the West. In the Zutphen study from the Netherlands, the 20-year mortality rate was 50% lower among those who ate 30 g of fish per day (approximately one to two fish meals per week) (2). Data from 6250 participants in the Multiple Risk Factor Intervention Trial (MR-FIT) demonstrated decreased 10-year mortality rates with increased consumption of PUFAs but not increased consumption of linoleic acid (18:2n-6), the predominant dietary PUFA (3). The Chicago Western Electric Study examined the relation between fish consumption and 30-year risk of fatal MI in 1822 men free of cardiovascular disease at baseline (6). At the end of the study, there was an inverse relationship between fish consumption and death from CAD but not sudden cardiac death. The US Physician Health Study (5) collected data on the fish intake of 20,551 male physicians ages 40 to 84 who were free of cardiovascular disease or stroke at the beginning of the study. This study indicated that the consumption of fish at least once per week was associated with a 52% reduction in the risk of sudden cardiac death during an 11-year follow-up.
A prospective population study of 1871 middle-aged men in eastern Finland, 42 to 60 years old with no clinical CAD, demonstrated a 44% risk reduction for acute coronary events after an average follow-up of 10 years (4). The same study showed that high mercury content in the hair attenuated the protection conferred by high serum levels of omega-3 fatty acids. This very important finding could potentially explain the lack of efficacy of fish consumption in a few of the epidemiological studies (18–21).
The Nurses Health Study (8) recently examined the dietary habits and the incidence of all kinds of strokes in 79,839 nurses (ages 30 to 55 at the time of enrollment). After 14 years of follow-up, there were significant reductions in both the thrombotic and lacunar strokes among women who consumed fish two or more times per week. This benefit was more obvious among women who had higher risk of stroke and were not taking aspirin. In the Honolulu Heart Program (7), heavy smokers with high fish consumption were at lower risk for CAD mortality than those who smoked heavily and had low fish consumption.
However, not all epidemiological studies have confirmed the beneficial effects of fish consumption on cardiovascular events. The Physician Health Study (20), a case control evaluation of 14,916 participants, demonstrated similar baseline levels of EPA and DHA in those who had an MI versus those who did not have an MI during 5 years follow-up. Another analysis of a larger group from this same study population, however, showed decreased sudden cardiac death with higher fish consumption (5). The health professional follow-up study (21) found that increasing fish intake from one to two servings per week to five or six did not substantially reduce the risk of CAD among men who were initially free of cardiovascular disease. Three separate analyses on data from respondents to a postal dietary survey in Norway (18) did not show an association between high fish intake and decreased cardiac risk. Another follow-up study on 7615 Japanese men as part of the Honolulu Heart Program (19) did not demonstrate significant association between fish consumption and total and fatal CAD. In light of the more recent results of the large-scale randomized trials (e.g. GISSI trial [10]), we may have different interpretations for the finding of the negative studies. The Physician Health Study and the health professional follow-up study included cohorts with potentially higher baseline intake of omega-3 PUFAs than other cohort studies. These studies involved cohorts at low risk of CAD and included few participants with low fish consumption (less than once per week). A threshold effect in which fish intake is cardioprotective in small amounts may partially explain these discordant results. In addition, the studies from Norway and the follow-up study on Japanese men both included populations with fairly high fish consumption, and the data collected to support conclusions about the effects of fish consumption was far less accurate.
Fish Oil in Cardiovascular Secondary Prevention
There is now mounting evidence that fish oil consumption is very useful in the secondary prevention of cardiovascular events. In the GISSI trial (10), 11,324 patients who had suffered an MI within the previous 3 months were randomized to receive fish oil supplement (1 g daily containing 850 mg of concentrated EPA and DHA) versus no supplement, 300 mg of vitamin E supplement versus no supplement, and both supplements versus no supplements. The primary combined efficacy end point was death, non-fatal MI, and stroke. Patients taking the fish oil supplements had 15% risk reduction in the primary end point, 20% reduction in total mortality, and a 45% reduction in risk of sudden cardiac death. Vitamin E showed no efficacy alone or in combination with fish oil. The beneficial effects of fish oil supplement were noted in patients who had relatively low risk and were generally taking standard post-MI therapy, including aspirin, beta-adrenergic blocker agents, angiotensin converting enzyme inhibitors, and statin therapy. The DART trial (9) (finished long before the GISSI trial), randomized post-MI patients to three kinds of diet advice: a reduction in dietary fat, an increase in cereal fibers, and an increase in fish consumption. Subjects in the fish arm were instructed to eat mackerel two times weekly or to take fish oil supplements. Dietary fat advice and cereal meals advice were not associated with changes in cardiovascular events. After 2 years of follow-up, the fish group showed a 29% mortality reduction, with the difference entirely attributable to reduction in CAD deaths. In fact, the reductions in cardiovascular events were particularly impressive in the subgroup that took the fish oil supplement as opposed to simply increasing dietary fish consumption.
In a randomized placebo-controlled trial, the effects of 1-year treatment with fish oil (EPA, 1.08 g/d, n=122), mustard oil (ALA, 2.9 g/d, n=120), and placebo (n=118) were compared in patients with suspected acute MI (11). At the end of the study, there were significant reductions in total cardiac events and nonfatal MI, and a 50% reduction in sudden cardiac death in the fish oil and mustard groups when compared with the placebo group. The fish oil and mustard oil groups also showed significant reductions in total cardiac arrhythmias, left ventricular enlargement, and angina pectoris compared with the placebo group.
Increased consumption of fish oil was used to slow down or even reverse the progression of the atherosclerotic heart disease in several studies. The Study on Prevention of Coronary Atherosclerosis by Intervention with Marine Omega-3 fatty acids (SCIMO) was a randomized, double blind trial of 225 participants using 6 g/d of fish oil (55% EPA/DHA) for 3 months and then 3 g/d for 21 months versus placebo (22). All participants had a greater than 20% stenosis in at least one coronary artery on angiography, and had revascularization (percutaneous coronary angiography or carotid artery bypass graft) planned or performed in the previous 6 months in no more than one vessel. After the angiograms before and after randomization were compared, coronary segments in the fish oil group showed less progression and more regression than coronary segments in the placebo group. However, in a similar study of patients with angiographically documented CAD, Sacks and colleagues studied, and compared 31 patients on fish oil (6 g/d) with 28 receiving olive oil placebo and failed to show any significant effect of fish oil on CAD patients' angiograms (23).
Fish Oil and Sudden Death
The most impressive and consistent result in these fish oil trials is the reduction in the risk of sudden cardiac death. As shown in Table 1, fish oil had dramatic effects on sudden cardiac death in several major trials (24).
Table 1.
Main results regarding mortality in recent secondary prevention trials. Reprinted with permission from (24): de Logeril M, Salen P. Curr Opin Cardiol 2000; 15:364–370. Copyright 2000, Lippincott, Williams & Wilkins
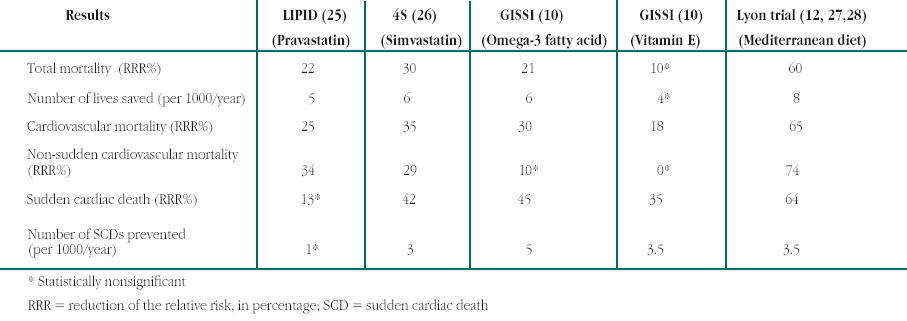
The GISSI trial (10) showed a 45% reduction in sudden cardiac death; the relatively small dose of DHA and EPA used in this trial was associated with a reduction of 5 sudden deaths for each 1000 patients treated. In the DART trial (9), the risk reduction was mainly in all cause deaths and CAD mortality rather than total CAD events.
There is strong evidence from basic research and small intervention trials that fish oil has major antiarrhythmic actions (29–31). In most trials, fish oil was much more effective in decreasing mortality from cardiac disease as opposed to total cardiac events (9, 10). Whereas the Physician's Health Study (20) failed to show efficacy of fish consumption in preventing the incidence of the first acute MI, this same study demonstrated significant reductions in sudden cardiac mortality with increased fish consumption (5).
A study done in Seattle and suburban King County, Washington, examined the fish consumption of 334 victims of primary cardiac arrest and 493 population-based control cases (32). Fish consumption was determined by interviewing the spouses of the victims and the control group; blood specimens from 82 cases and 108 controls were also analyzed to determine membrane fatty acid composition of red blood cells. Compared with no intake of EPA and DHA, an intake of 5.2 g per month (equivalent to one fatty fish meal per week) was associated with a 50% reduction in the risk of primary cardiac arrest (Figure 2). Any amount of fish consumption was associated with significantly reduced risk of sudden cardiac death. The risk reduction continued to be significant after using more objective evidence of omega-3 PUFA consumption from the red blood cell membrane fatty acid composition (Figure 3) (33).
Figure 2.
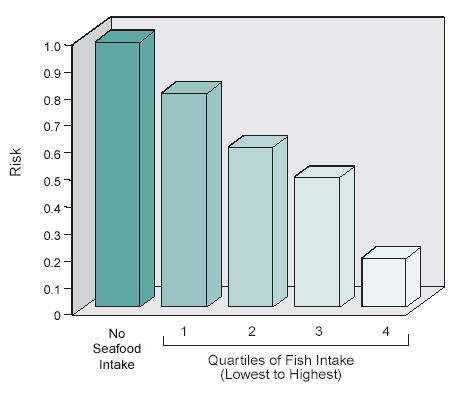
Risk of primary cardiac arrest with dietary intake of long chain 3-polyunsaturated fatty acids. First through fourth quartiles of fish intake from lowest to highest. Data from (32): Siscovick DS, et al. JAMA 1995; 274:1363–1367
Figure 3.
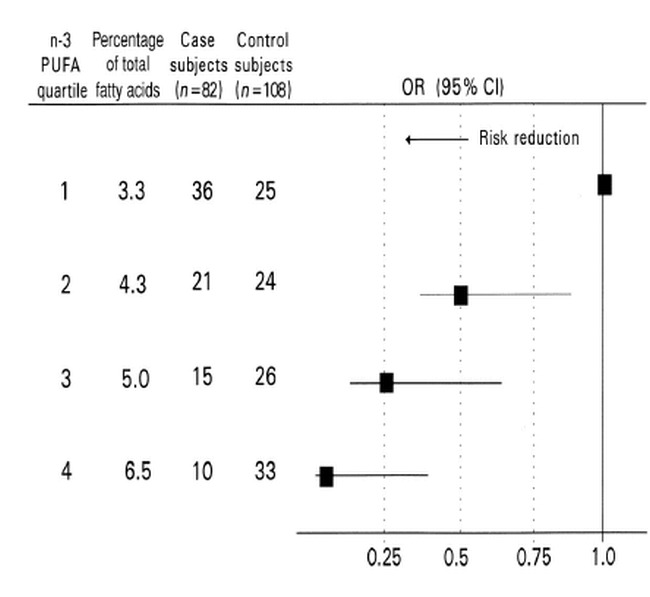
Risk of primary cardiac arrest associated with red blood cell membrane levels of long-chain n-3 polyunsaturated fatty acids (PUFAs). Quartile means are from control subjects. Odds ratios (ORs;) and 95% CIs (bars) were from a conditional logistic model that included the linear term for red blood cell membrane long-chain n-3 PUFAs after adjustment for age, current smoking, former smoking, family history of myocardial infarction or sudden death, fat intake scale, hypertension, diabetes mellitus, physical activity level, weight, height, and education. ORs and 95% CIs were calculated by using the lowest quartile as the reference group and the mean value for each category. Reproduced with permission by the American Journal of Clinical Nutrition. ©Am J Clin Nutr. American Society for Clinical Nutrition. (33) www.ajcn.org/content/vol71/issue1/images/large/020802.jpeg
Prospective data from the US Physician Health Study showed a significant 55% reduction in the risk of sudden cardiac death in subjects who consumed fish meals at least once per week, as compared with subjects who consumed fish less than once per month (5). There seemed to be a threshold effect for fish consumption with the one fish meal per week providing maximum protection. This small dose effect was confirmed by the GISSI trial (10). This same threshold effect noticed at relatively small doses was also noticed with all-cause mortality. The positive effect of fish oil on sudden cardiac death may be attributed to fish oil's suppression of malignant ventricular dysrhythmias.
In a small study, 55 post-MI patients were randomized in a double blind, controlled trial to 5.2 g/d of DHA/EPA or olive oil placebo for 12 weeks; 24-hour Holter monitoring was used to assess heart rate variability (HRV), which is known to be decreased in CAD and post-MI patients and to be associated with decreased ventricular fibrillation threshold and high post-MI mortality. Following fish oil therapy, significant improvements in HRV were noticed, again suggesting a potentially favorable effect on autonomic tone and the risk of malignant ventricular dysrhythmias (31).
The increase in HRV with fish oil was confirmed in a study of 291 patients with suspected CAD referred for coronary angiography. All patients had fish consumption assessed by questionnaires; omega-3 PUFA composition of granulocytes membranes and adipose was also assessed (34). A significant positive correlation was found between HRV and the level of omega-3 PUFA in granulocytes. The balance of autonomic tone is a key indicator of cardiovascular prognosis, and the improvements in risk of sudden cardiac death with omega-3 PUFA intake are probably mediated in part by alterations in autonomic tone (35).
The antiarrhythmic effect of fish oil was tested in several animal trials. Fish oil infusion prevented ventricular fibrillation in a dog model of sudden cardiac death (30). Canine models were prepared with anterior MI by surgically ligating the left anterior descending coronary artery. During the operation, a hydraulic cuff was placed around the left circumflex coronary artery. After recovery from MI, the dogs were trained to run on the treadmill. In 3–4 weeks, another ischemic event was produced during stress exercise by inflating the hydraulic cuff, and only the dogs with ischemia-induced ventricular fibrillation who responded to resuscitation were chosen to complete the study (n=17). The exercise and ischemic events were reproduced 1 week later, after intravenous treatment with one of the following purified omega-3 fatty acids: EPA, DHA, or ALA. One week after the completion of each EPA, DHA or ALA study, a second control exercise plus ischemia test was repeated after either an infusion of lipid emulsion of soybean oil or an infusion of saline. The infusion of fish oil concentrate, EPA, DHA or ALA prevented fatal ventricular arrhythmias in 10 out of 13, 5 out of 7, 6 out of 8, and 6 out of 8 dogs tested, respectively, while the control treatment did not protect any dog from the malignant ventricular arrhythmia. In another study, rats fed fish oil for 1 month showed a significant reduction in ischemia-induced ventricular arrhythmia (36).
At the present time, these major antiarrhythmic actions of fish oil, confirmed in animal and human studies, have not been equaled by any other therapy, including the beta-adrenergic blocking agents or amiodarone, the most powerful anti-arrhythmic drug in use.
Potential Mechanisms of Action
Large doses (3–5 g/d) of fish oil (generally using 6–10 fish oil pills per day) have been shown to produce 30% to 50% reduction in triglycerides (37), whereas most studies using low dose therapy (e.g. 1 g/d) have not been associated with any lipid improvements, although the GISSI trial using 850 mg/d did show very small (3.4%), but statistically significant, reductions in triglycerides (10). Therefore, other mechanisms must play a major role in the clinical effects of fish oil, particularly in the antiarrhythmic effects and the reduction in sudden cardiac death.
Fish oil reduces ventricular arrhythmias, slows the heart rate, and increases HRV (31, 34, 36). Moreover, high doses of fish oil have been shown to lower blood pressure (38, 39). Fish oil therapy resulted in a significant 25% reduction in mean arterial pressure and systemic vascular resistance, modest reduction in LVH, and modest improvements in left ventricular diastolic filling in cardiac transplant patients with cyclosporine-induced hypertension (40, 41). Fish oil may also reduce expression of cell adhesion molecules and decrease secretion of platelet-derived growth factor (42, 43). By reducing transcription of inflammatory cytokines and other mechanisms, fish oil has been shown to have significant anti-inflammatory actions (44), which may make it efficacious in several other chronic inflammatory diseases like ulcerative colitis and rheumatoid arthritis, as well as play a role in plaque stabilization (45).
Omega-3 fatty acids alter the pattern of synthesis of thromboxanes and prostacyclins (46). EPA competes with arachidonic acid for the cyclo-oxygenase, which leads to decreased synthesis of thromboxane A2 and increased levels of thromboxane A3. Thromboxane A2 is a strong platelet agonist while thromboxane A3 is relatively inactive, so the net effect of high doses of fish oil is platelet inhibition.
In a double blind trial of 53 male patients with CAD, 35 were randomized to receive fish oil (four capsules three times daily) and 18 to receive rapeseed (12 g/d) (47). At the end of the study, there was a significant reduction in lipoprotein (a), or Lp(a), in the fish oil group. High levels of Lp(a) are known to be a significant and independent risk factor for CAD, and only two therapies (niacin and estrogen) are generally available to reduce Lp(a) levels (48).
In a randomized, double blind, placebo-controlled trial, Goodle and colleagues isolated small arteries from skin biopsy of 16 hypercholesterolemic patients and 12 age- and sex-matched controls with normal levels of plasma cholesterol (49). Patients and controls were randomized to receive fish oil or placebo for 3 months, and a second biopsy was taken at the end of the study. The small arteries were mounted on a wire myography for isometric tension experiments. In hypercholesterolemic patients, fish oil was shown to significantly improve endothelial function in peripheral small arteries.
In a rat study by Anderson et al, the researchers tried to establish the mechanisms by which omega-3 fatty acids produce antiarrhythmic action (29). They found that dietary supplement with omega-3 fatty acids inhibited the reperfusion rise in Inositole triphosphate (Ins P3). The rapid release of Ins P3 during postischemic reperfusion has been implicated in reperfusion arrhythmias.
Safety of Fish Oil
The FDA recently reviewed the safety of fish oil and concluded that dietary intakes up to 3 g/d of EPA and DHA are “generally recognized as safe” (50). Fish oil consumption may increase the levels of low-density lipoprotein cholesterol (LDL-C) (51). The increase in LDL-C with fish oil consumption is usually less than 5%, but may be as high as 30% in patients with severe hypertriglyceridemia. Combining statin therapy, which is generally needed anyway for patients with atherosclerosis, with fish oil can easily treat this problem. However, no increases in LDL-C have been noticed in large-scale clinical trials using doses less than 1 g/d of fish oil (5).
Although increased bleeding time has been noted with very high doses of PUFA (20 g/d) (51, 52), no bleeding complications have been noticed with the 7 g/d dose of PUFA in a large restenosis study (53), and no increased bleeding when the fish oil was combined with aspirin or warfarin (54).
Some studies have shown some worsening glycemic control in patients with type II diabetes mellitus with consumption of large amounts of fish oil (55). However, studies using moderate doses (2–3 g/d) have not reported any adverse effects on glycemic control (56–59).
Recommendations
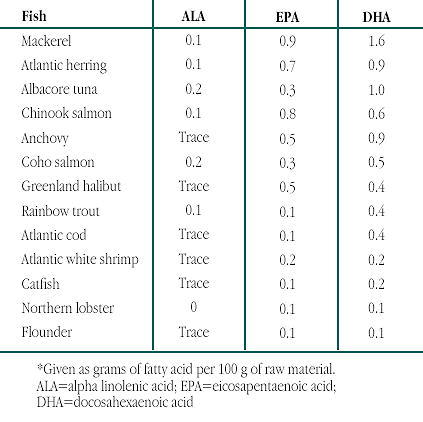
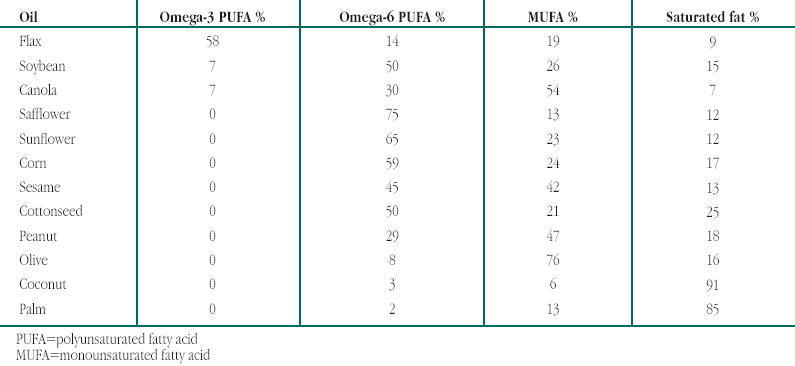
Based on the considerable evidence, most patients should increase their consumption of omega-3 fatty acids, and specifically EPA/DHA. Although the data for primary prevention are not yet as convincing as for secondary prevention, there is evidence that higher intake of fish may be associated with significant reductions in cardiac arrest in patients without known heart disease. Certainly the data appear quite impressive for the secondary prevention of cardiac events and particularly cardiac death and sudden cardiac death. Based on these data, we are routinely recommending therapy with fish oil for most of our patients with established heart disease or high CAD risk based on either multiple risk factors, a high Framingham risk score (greater than 10%–20% 10 year risk of major cardiac event) (60, 61), or by assessing risk on our (RVM, CJL) web site, www.myheartrisk.com. Generally, we recommend a dose of about 1000 mg of EPA and DHA daily. In patients who eat a considerable amount of fish, especially if they eat fatty fish or fish containing relatively large amounts of omega-3 fatty acids, this can be obtained from dietary sources. Tables 2–4 provide some information about the fish and plant dietary sources of PUFA and the fatty acids composition of common oils (62).
Table 2.
Omega-3 polyunsaturated fatty acid content of selected fish.* Reprinted with permission from (62): Arch Int Med 2001; 161:2185–2192. Copyrighted 2001, American Medical Association
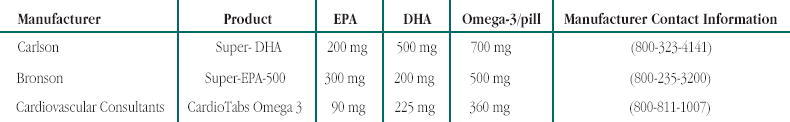
However, for most of our patients who either do not eat fish or who consume relatively small doses of EPA/DHA from dietary sources, we recommend fish oil supplements. We prefer to use supplements that are relatively inexpensive, potent (meaning less pills per day, such as 1 or 2, are needed to obtain the recommended dose), purified (low content of mercury and cholesterol), and contain a relatively high concentration of DHA (some fish oil supplements contain as little as 12% DHA, and there is considerable evidence suggesting that DHA may provide even more protection against CAD than does EPA). Table 5 provides information on three supplements (which can be purchased by phone) that meet these criteria. Generally we are supplementing our patients with approximately 1 gram of PUFA per day, either as one to two capsules of the Carlson Super-DHA, two capsules of the Bronson Super EPA-500, or two capsules of CardioTabs Omega-3.
Table 5.
Recommended brands of fish oil supplements
Conclusions
There is considerable evidence from both epidemiological studies and controlled clinical trials demonstrating the positive effects of fish oil in the secondary prevention of major cardiovascular events and stroke. The efficacy in preventing sudden cardiac death seems to be particularly powerful. The results of the controlled trials suggest that fish oil has antiarrhythmic action and survival benefits that are unequaled by any other agent. Most of the data on fish oil efficacy are derived from controlled, but not blinded trials. However, these unblinded trials were large enough to have significant validity, especially when we take into account the mounting epidemiological data. Although the evidence for fish oil in primary prevention is still in its early stages, the epidemiological findings in populations without known CAD makes a strong argument for the efficacy of fish oil in the primary prevention of cardiovascular events. Additionally, increased omega-3 PUFA intake has been associated with a myriad of other health benefits, including decreased risk of prostate cancer, depression, inflammatory bowel disease, and others. This pattern of multisystem benefits is a typical response to supplementation of a deficient nutrient to bring levels of the essential compound back into optimal range. Studies indicate that the typical American omega-6 to omega-3 dietary ratio is about 20:1 compared with a Paleolithic ratio of 2:1 (13, 63).
After 25 years of research and re-examination of fish oil therapy, we believe it is now time to consider fish oil therapy for most patients with known cardiovascular disease and for patients at increased risk for cardiovascular disease, and particularly for patients at relatively high risk of sudden cardiac death.

Dr. Alaswad is a fellow of the Ochsner Heart and Vascular Institute
Table 3.
Plant sources of α-linolenic acid. Reprinted with permission from (62): Arch Int Med 2001; 161:2185–2192. Copyrighted 2001, American Medical Association
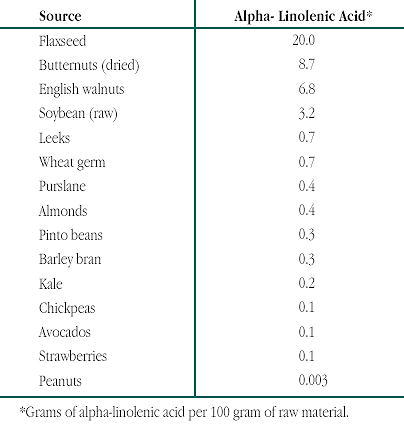
Table 4.
Fatty acid composition of common oils. Reprinted from (62): Arch Int Med 2001; 161:2185–2192. Copyrighted 2001, American Medical Association
References
- Sinclair H. M. The diet of Canadian Indians and Eskimos. Proc Nutr Soc. 1953;12:69–82. [Google Scholar]
- Kromhout D., Bosschieter E. B., de Lezenne Coulander C. The inverse relation between fish consumption and 20-year mortality from coronary heart disease. N Engl J Med. 1985;312:1205–1209. doi: 10.1056/NEJM198505093121901. [DOI] [PubMed] [Google Scholar]
- Dolecek T. A. Epidemiological evidence of relationships between dietary polyunsaturated fatty acids and mortality in the multiple risk factor intervention trial. Proc Soc Exp Biol Med. 1992;200:177–182. doi: 10.3181/00379727-200-43413. [DOI] [PubMed] [Google Scholar]
- Rissanen T., Voutilainen S., Nyyssonen K. Fish oil-derived fatty acids, docosahexaenoic acid and docosapentaenoic acid, and the risk of acute coronary events: the Kuopio ischaemic heart disease risk factor study. Circulation. 2000;102:2677–2679. doi: 10.1161/01.cir.102.22.2677. [DOI] [PubMed] [Google Scholar]
- Albert C. M., Hennekens C. H., O'Donnell C. J. Fish consumption and risk of sudden cardiac death. JAMA. 1998;279:23–28. doi: 10.1001/jama.279.1.23. [DOI] [PubMed] [Google Scholar]
- Daviglus M. L., Stamler J., Orencia A. J. Fish consumption and the 30-year risk of fatal myocardial infarction. N Engl J Med. 1997;336:1046–1053. doi: 10.1056/NEJM199704103361502. [DOI] [PubMed] [Google Scholar]
- Rodriguez B. L., Sharp D. S., Abbott R. D. Fish intake may limit the increase in risk of coronary heart disease morbidity and mortality among heavy smokers. The Honolulu Heart Program. Circulation. 1996;94:952–956. doi: 10.1161/01.cir.94.5.952. [DOI] [PubMed] [Google Scholar]
- Iso H., Rexrode K. M., Stampfer M. J. Intake of fish and omega-3 fatty acids and risk of stroke in women. JAMA. 2001;285:304–312. doi: 10.1001/jama.285.3.304. [DOI] [PubMed] [Google Scholar]
- Burr M. L., Fehily A. M., Gilbert J. F. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART) Lancet. 1989;2:757–761. doi: 10.1016/s0140-6736(89)90828-3. [DOI] [PubMed] [Google Scholar]
- Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto miocardico. Lancet. 1999;354:447–455. [PubMed] [Google Scholar]
- Singh R. B., Niaz M. A., Sharma J. P. Randomized, double-blind, placebo-controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: the Indian experiment of infarct survival–4. Cardiovasc Drugs Ther. 1997;11:485–491. doi: 10.1023/a:1007757724505. [DOI] [PubMed] [Google Scholar]
- de Lorgeril M., Salen P., Martin J. L. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99:779–785. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]
- O'Keefe J. H., Jr, Harris W. S. From Inuit to implementation: Omega-3 fatty acids come of age. Mayo Clin Proc. 2000;75:607–614. doi: 10.4065/75.6.607. [DOI] [PubMed] [Google Scholar]
- O'Keefe J. H., Harris W. S. Omega-3 fatty acids: Time for clinical implementation? Am J Cardiol. 2000;85:1239–1241. doi: 10.1016/s0002-9149(00)00735-9. [DOI] [PubMed] [Google Scholar]
- Kris-Etherton P., Daniels S. R., Eckel R. H. Summary of the scientific conference on dietary fatty acids and cardiovascular health. Conference summary from the nutrition committee of the American Heart Association. Circulation. 2001;103:1034–1039. doi: 10.1161/01.cir.103.7.1034. [DOI] [PubMed] [Google Scholar]
- Kris-Etherton P., Eckel R. H., Howard B. V. AHA Science Advisory Lyon Diet Heart Study: Benefits of a Mediterranean-style, National Cholesterol Education Program/American Heart Association Step I Dietary Pattern on Cardiovascular Disease. Circulation. 2001;103:1823–1825. doi: 10.1161/01.cir.103.13.1823. [DOI] [PubMed] [Google Scholar]
- Kang J. X., Leaf A. Antiarrhythmic effects of polyunsaturated fatty acids. Recent studies. Circulation. 1996;94:1774–1780. doi: 10.1161/01.cir.94.7.1774. [DOI] [PubMed] [Google Scholar]
- Vollset S. E., Heugh I., Bjelke E. Fish consumption and mortality from coronary heart disease. New Engl J Med. 1985;313:820–824. doi: 10.1056/NEJM198509263131311. (letter) [DOI] [PubMed] [Google Scholar]
- Yano K., Reed D. M., Curb J. D. Biological and dietary correlates of plasma lipids and lipoproteins among elderly Japanese men in Hawaii. Arteriosclerosis. 1986;34:422–433. doi: 10.1161/01.atv.6.4.422. [DOI] [PubMed] [Google Scholar]
- Guallar E., Hennekens C. H., Sacks F. M. A prospective study of plasma fish oil levels and incidence of myocardial infarction in U.S. male physicians. J Am Coll Cardiol. 1995;25:387–394. doi: 10.1016/0735-1097(94)00370-6. [DOI] [PubMed] [Google Scholar]
- Ascherio A., Rimm E. B., Stampfer M. J. Dietary intake of marine n-3 fatty acids, fish intake, and the risk of coronary disease among men. N Engl J Med. 1995;332:977–982. doi: 10.1056/NEJM199504133321501. [DOI] [PubMed] [Google Scholar]
- von Schacky C., Angerer P., Kothny W. The effect of dietary omega-3 fatty acids on coronary atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1999;130:554–562. doi: 10.7326/0003-4819-130-7-199904060-00003. [DOI] [PubMed] [Google Scholar]
- Sacks F. M., Stone P. H., Gibson C. M. Controlled trial of fish oil for regression of human coronary atherosclerosis. HARP Research Group. J Am Coll Cardiol. 1995;25:1492–1498. doi: 10.1016/0735-1097(95)00095-l. [DOI] [PubMed] [Google Scholar]
- de Lorgeril M., Salen P. Diet as preventive medicine in cardiology. Curr Opin Cardiol. 2000;15:364–370. doi: 10.1097/00001573-200009000-00009. [DOI] [PubMed] [Google Scholar]
- The Long-term Intervention with Prevastatin in Ischemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with prevastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastin Survival Study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- de Longeril M., Renaud S., Mamelle N. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronar heart disease. Lancet. 1994;343:1454–1459. doi: 10.1016/s0140-6736(94)92580-1. [DOI] [PubMed] [Google Scholar]
- de Longeril M., Salen P., Martin J. L. Effect of a Mediterranean type of diet on the rate of cardiovascular complications in patients with coronary artery disease. Insights into the cardioprotective effect of certain nutriments. J Am Coll Cardiol. 1996;28:1103–1108. doi: 10.1016/S0735-1097(96)00280-X. [DOI] [PubMed] [Google Scholar]
- Anderson K. E., Du X. J., Sinclair A. J. Dietary fish oil prevents reperfusion Ins(1,4,5)P3 release in rat heart: possible antiarrhythmic mechanism. Am J Physiol. 1996;271:H1483–H1490. doi: 10.1152/ajpheart.1996.271.4.H1483. (4 Pt 2) [DOI] [PubMed] [Google Scholar]
- Billman G. E., Kang J. X., Leaf A. Prevention of sudden cardiac death by dietary pure omega-3 polyunsaturated fatty acids in dogs. Circulation. 1999;99:2452–2457. doi: 10.1161/01.cir.99.18.2452. [DOI] [PubMed] [Google Scholar]
- Christensen J. H., Gustenhoff P., Korup E. Effect of fish oil on heart rate variability in survivors of myocardial infarction: a double blind randomised controlled trial. BMJ. 1996;312:677–678. doi: 10.1136/bmj.312.7032.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siscovick D. S., Raghunathan T. E., King I. Dietary intake and cell membrane levels of long-chain n-3 polyunsaturated fatty acids and the risk of primary cardiac arrest. JAMA. 1995;274:1363–1367. doi: 10.1001/jama.1995.03530170043030. [DOI] [PubMed] [Google Scholar]
- Siscovick D. S., Raghunathan T. E., King I. Dietary intake and cell membrane levels of long-chain n-3 polyunsaturated fatty acids and the risk of primary cardiac arrest. Am J Clin Nutr. 2000;71:208–212. doi: 10.1093/ajcn/71.1.208S. [DOI] [PubMed] [Google Scholar]
- Christensen J. H., Skou H. A., Fog L. Marine n-3 fatty acids, wine intake, and heart rate variability in patients referred for coronary angiography. Circulation. 2001;103:651–657. doi: 10.1161/01.cir.103.5.651. [DOI] [PubMed] [Google Scholar]
- Curtis B. M., O'Keefe J. H., Jr Autonomic tone as a cardiovascular risk factor: the dangers of chronic fight or flight. Mayo Clin Proc. 2002;77:45–54. doi: 10.4065/77.1.45. [DOI] [PubMed] [Google Scholar]
- McLennan P. L., Abeywardena M. Y., Charnock J. S. Influence of dietary lipids on arrhythmias and infarction after coronary artery ligation in rats. Can J Physiol Pharmacol. 1985;63:1411–1417. doi: 10.1139/y85-232. [DOI] [PubMed] [Google Scholar]
- Harris W. S. Fish oils and plasma lipid and lipoprotein metabolism in humans: a critical review. J Lipid Res. 1989;30:785–807. [PubMed] [Google Scholar]
- Gray D. R., Gozzip C. G., Eastham J. H. Fish oil as an adjuvant in the treatment of hypertension. Pharmacotherapy. 1996;16:295–300. [PubMed] [Google Scholar]
- Schmidt E. B., Lervang H. H., Varming K. Long-term supplementation with n-3 fatty acids, I: Effect on blood lipids, haemostasis and blood pressure. Scand J Clin Lab Invest. 1992;52:221–228. doi: 10.3109/00365519209088789. [DOI] [PubMed] [Google Scholar]
- Ventura H. O., Lavie C. J., Messerli F. H. Cardiovascular adaptation to cyclosporine-induced hypertension. J Hum Hypertens. 1994;8:233–237. [PubMed] [Google Scholar]
- Ventura H. O., Milani R. V., Lavie C. J. Cyclosporineinduced hypertension. Efficacy of omega-3 fatty acids in patients after cardiac transplantation. Circulation. 1993;88:II281–II285. (5 Pt 2) [PubMed] [Google Scholar]
- Knapp H. R., Reilly I. A., Alessandrini P. In vivo indexes of platelet and vascular function during fish-oil administration in patients with atherosclerosis. N Engl J Med. 1986;314:937–942. doi: 10.1056/NEJM198604103141501. [DOI] [PubMed] [Google Scholar]
- Endres S., Ghorbani R., Kelley V. E. The effect of dietary supplementation with n-3 polyunsaturated fatty acids on the synthesis of interleukin-1 and tumor necrosis factor by mononuclear cells. N Engl J Med. 1989;320:265–271. doi: 10.1056/NEJM198902023200501. [DOI] [PubMed] [Google Scholar]
- Belluzzi A., Brignola C., Campieri M. Effect of an entericcoated fish-oil preparation on relapses in Crohn's disease. N Engl J Med. 1996;334:1557–1560. doi: 10.1056/NEJM199606133342401. [DOI] [PubMed] [Google Scholar]
- Stenson W. F., Cort D., Rodgers J. Dietary supplementation with fish oil in ulcerative colitis. Ann Intern Med. 1992;116:609–614. doi: 10.7326/0003-4819-116-8-609. [DOI] [PubMed] [Google Scholar]
- Mori T. A., Beilin L. J., Burke V. Interactions between dietary fat, fish, and fish oils and their effects on platelet function in men at risk of cardiovascular disease. Arterioscler Thromb Vasc Biol. 1997;17:279–286. doi: 10.1161/01.atv.17.2.279. [DOI] [PubMed] [Google Scholar]
- Herrmann W., Biermann J., Kostner G. M. Comparison of effects of N-3 to N-6 fatty acids on serum level of lipoprotein (a) in patients with coronary artery disease. Am J Cardiol. 1995;76:459–462. doi: 10.1016/s0002-9149(99)80130-1. [DOI] [PubMed] [Google Scholar]
- Danesh J., Collins R., Peto R. Lipoprotein(a) and coronary heart disease. Meta-analysis of prospective studies. Circulation. 2000;102:1082–1085. doi: 10.1161/01.cir.102.10.1082. [DOI] [PubMed] [Google Scholar]
- Goode G. K., Garcia S., Heagerty A. M. Dietary supplementation with marine fish oil improves in vitro small artery endothelial function in hypercholesterolemic patients: a double-blind placebo-controlled study. Circulation. 1997;96:2802–2807. doi: 10.1161/01.cir.96.9.2802. [DOI] [PubMed] [Google Scholar]
- Substances affirmed as generally recognized as safe: menhaden oil. Federal Register. June 5, 1997;62:30751–30757. [Google Scholar]
- Alaswad K., Pogson G. W., Harris W. S. Effect of phenytoin, niacin, gemfibrozil, and omega-3 fatty acids on high density lipoproteins in patients with hypoalphalipoproteinemia. Preventive Cardiology. 1999;2:141–150. [Google Scholar]
- Goodnight S. H., Jr, Harris W. S., Connor W. E. The effects of dietary omega 3 fatty acids on platelet composition and function in man: a prospective, controlled study. Blood. 1981;58:880–885. [PubMed] [Google Scholar]
- Leaf A., Jorgensen M. B., Jacobs A. K. Do fish oils prevent restenosis after coronary angioplasty? Circulation. 1994;90:2248–2257. doi: 10.1161/01.cir.90.5.2248. [DOI] [PubMed] [Google Scholar]
- Eritsland J., Arnesen H., Gronseth K. Effect of dietary supplementation with n-3 fatty acids on coronary artery bypass graft patency. Am J Cardiol. 1996;77:31–36. doi: 10.1016/s0002-9149(97)89130-8. [DOI] [PubMed] [Google Scholar]
- Glauber H., Wallace P., Griver K. Adverse metabolic effect of omega-3 fatty acids in non-insulin-dependent diabetes mellitus. Ann Intern Med. 1988;108:663–668. doi: 10.7326/0003-4819-108-5-663. [DOI] [PubMed] [Google Scholar]
- Axelrod L., Camuso J., Williams E. Effects of a small quantity of omega-3 fatty acids on cardiovascular risk factors in NIDDM. A randomized, prospective, double-blind, controlled study. Diabetes Care. 1994;17:37–44. doi: 10.2337/diacare.17.1.37. [DOI] [PubMed] [Google Scholar]
- Rivellese A. A., Maffettone A., Iovine C. Long-term effects of fish oil on insulin resistance and plasma lipoproteins in NIDDM patients with hypertriglyceridemia. Diabetes Care. 1996;19:1207–1213. doi: 10.2337/diacare.19.11.1207. [DOI] [PubMed] [Google Scholar]
- Sirtori C. R., Paoletti R., Mancini M. N-3 fatty acids do not lead to an increased diabetic risk in patients with hyperlipidemia and abnormal glucose tolerance. Italian Fish Oil Multicenter Study. Am J Clin Nutr. 1997;65:1874–1881. doi: 10.1093/ajcn/65.6.1874. [DOI] [PubMed] [Google Scholar]
- Friedberg C. E., Janssen M. J., Heine R. J. Fish oil and glycemic control in diabetes. A meta-analysis. Diabetes Care. 1998;21:494–500. doi: 10.2337/diacare.21.4.494. [DOI] [PubMed] [Google Scholar]
- Grundy S. M., Balady G. J., Criqui M. H. Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the AHA Task Force on Risk Reduction. Circulation. 1998;97:1876–1887. doi: 10.1161/01.cir.97.18.1876. [DOI] [PubMed] [Google Scholar]
- Grundy S. M., Pasternak R., Greenland P. Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. Circulation. 1999;100:1481–1492. doi: 10.1161/01.cir.100.13.1481. [DOI] [PubMed] [Google Scholar]
- Harper C. R., Jacobson T. A. The fats of life: the role of omega-3 fatty acids in the prevention of coronary heart disease. Arch Intern Med. 2001;161:2185–2192. doi: 10.1001/archinte.161.18.2185. [DOI] [PubMed] [Google Scholar]
- Terry P., Lichtenstein P., Feychting M. Fatty fish consumption and risk of prostate cancer. Lancet. 2001;357:1764–1766. doi: 10.1016/S0140-6736(00)04889-3. [DOI] [PubMed] [Google Scholar]


