Abstract
Objectives:
This study was conducted on the estimation of the efficiency of mental health program in primary health care in Chaharmahal and Bakhtyari province, situated in center of the Islamic Republic of Iran, from 1999 to 2009.
Methods:
One of the important objectives of mental health program is screening of mental health disorders and follow up. According to the prescription of mental health program, General Practitioners (GPs) were appointed to screen under-covered individuals, treat patients and also follow-up the patients with mental health disorders who needs referring to psychiatric clinics. Diagnostic criteria of mental disorders were based on American Psychiatry Association (DSM IV1994). Patients were categorized in four groups as follows: 1 - Severe mental disorders, such as major depression, schizophrenia, bipolar disorders, etc., 2 - Mild mental disorders, such as neurosis, anxiety, etc., 3 - Convulsive disorders and 4 - Behavioral disorders. The convulsive disorders and their types were diagnosed by physical examination and electroencephalography. In order to screen mental retardation, intelligence scale (IQ) score < 70 was considered as mental retardation. During the 10 years (1999 to 2009) of conducting program, all new diagnosed cases were confirmed by psychiatrists. All data was recorded in health files by trained GPs and they were assessed and justified by psychiatrists.
Results:
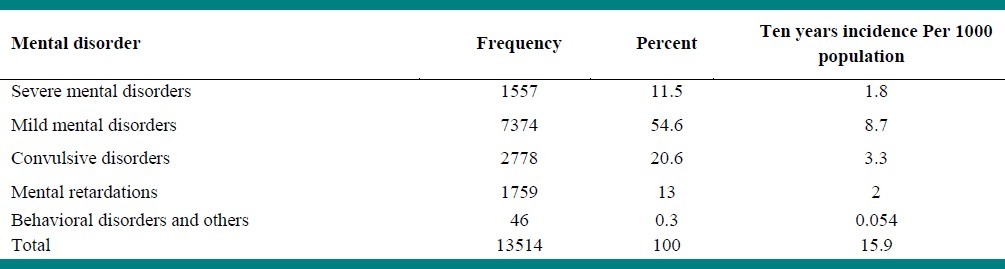
During 10 years after conducting and stabilizing integrated mental health in primary health care, 13514 patients overall were newly detected and followed. Ten years incidence of total psychiatric disorders was estimated in about 15.9 per 1000 populations.
Conclusions:
Integrated mental health care offers the opportunity to increase access and develop efficiency of the mental health cares.
Keywords: Mental health, Integration, Efficiency, Primary health care
INTRODUCTION
Mental disorders have profound, social, cultural and economic effects on communities worldwide.[1]
Burden of mental disorders are increasing markedly in developing countries. According to WHO reports, 12% of the global burden of disease is attributed to mental disorders and it will be increased to 15% of disability-adjusted life years (DALYs) lost to illness by 2020.[2]
Cardiovascular disease and mental disorders (after accidents) ranked second burden of disease which account 14% of DALYs lost.[3]
Integrated mental health services in community creates opportunity for chronic mental patients who require continuous mental health care. These services are highly accessible.[4–6] There are many patients with chronic mental illnesses who are stable, requiring only maintenance medications and could be best managed in the community.[7]
In Islamic Republic of Iran, a mental health policy and program was initially formulated in 1986. The main components are advocacy, promotion, prevention, treatment and follow-up. The main strategy has been to integrate the mental health program within the primary health care system. From 1988 to 1990, successful pilot studies were implemented in ShahreKord and Shahreza in central Islamic Republic of Iran, which showed significant increased knowledge of health workers and improved skill in patient screening compared with the control area. Expansion of the integration of mental health within PHC has resulted in immense improvements in the provision of mental health services.[8]
By achieving desired results, integrated mental healthcare program had been extended to rural areas of 24 provinces and also all regions of community by 1998. To evaluate the efficiency of integrated program in afflicted diagnosed patients, this prospective uncontrolled study was conducted after stabilizing project.
METHODS
This prospective uncontrolled, community-based study was conducted on the average of 85000 urban and rural inhabitants of Chaharmahal and Bakhtyari (C and B) province situated in the center of Islamic Republic of Iran (I.R. Iran) from 1999 to 2009.
According to the prescription of mental health program, General Practitioners (GPs) were appointed to screen under-covered individuals continuously, at least annually and also identify patients who suffer mental disorders and who need to refer to psychiatric clinics.
Diagnostic criteria of mental disorders were based on American Psychiatry Association (DSM IV). Patients were categorized in four groups as follows: 1 - Severe mental disorders, such as: major depression, schizophrenia, bipolar disorders, etc., 2 - Mild mental disorders, such as: neurosis, anxiety, somatization, etc., 3 -Convulsive disorders and 4 - Behavioral disorders.[8]
The convulsive disorders were diagnosed by physical examination and were confirmed by electroencephalography. In order to screen mental retardation, IQ test by using the intelligence scale was administered. IQ score <70 was considered as mental retardation.[9]
In this study, the behavioral disorders were discussed as other diseases, and no attempt have been carried out on addiction.
The process of patients’ screening, treatment, follow-up and data collection in health centers were supervised by psychiatrists (one psychiatrist in every district). Sometimes lack of psychiatrists in some districts were compensated by trained concerned GPs in many psychiatric skills and mental disorders management for better supervision of patients, undergoing better access to higher grade mental health services and development of program. There was one psychologist besides the trained GP to consult families of patients presenting with mental disorders. By this strategy, there was no district without psychiatrist or trained GP in this interval.
Executive committee of Shahrekord University of Medical Sciences (SKUMS) in the C and B province supported programs financially and allocated one psychiatrist professor as the scientific focal point to supervise the program by presenting in field every 3 month. Study was conducted according to ethical standards and protocols approved by Shahrekord University of Medical Sciences.
There were attempted to pay attention to cities’ councils and well-known trustworthy persons in each region, that would be amended the misinterpretation of people about patients were afflicted with mental disorders gradually. All mental health outpatients at least received one psychotropic medicine of each therapeutic class. Besides them, majority of patients received one or more psychosocial treatments.[8] Due to low socio-economical situation in this region (C and B Province), all medical expenditures (such as visits and drugs costs) were paid by medical insurance institutions and SKUMS. This policy also attracted lots of people including rich citizen in urban areas to benefit from these facilities.
Patients’ treatments were under the order of doctors’ prescription without any compulsion or specific limitation.
By deviating more than 10% 0f 1500 governmental hospitals’ beds in C and B province to mental disorders, the numbers of patients referred to other provinces were reduced significantly.
In health centers, all data were recorded in health files by GPs, while in hospitals, nurses were compelled to enter all data, according to patients’ files confidentially. Psychiatrists assessed and justified all documents ultimately.
Data Collection
During 10 years (1999 to 2009) of conducting program in C and B province, all new diagnosed cases confirmed by psychiatrists were entered in this study. The data of the diagnosed patients from the first 8 years of initial phase of mental health program (before 1998) were excluded.
Data Analysis
The data were examined for significant associations using SPSS version 11.0 for windows. The chi-square was used for comparison of categorical variables. P < 0.05 was considered to indicate statistically significant.
RESULTS
During the 10 years (1999 to 2009) of conducting integrated primary care program in C and B province, 13514 patients overall were newly detected and entered to study and followed. In this province, around between 800000 and 880000 persons stayed in such interval. From this it could be summarized that the ten years incidence of psychiatric disorders was estimated about 15.9 in every 1000 populations.
The frequency of total mental disorders were as follows: 1557 cases of severe mental disorders, 7374 cases of mild mental disorders, 2778 cases with convulsive disorders and 1759 cases of mental retardation [Table 1].
Table 1.
Frequency of new mental disorders cases in ten years study in Chaharmahal and Bakhtyari province in I.R. Iran
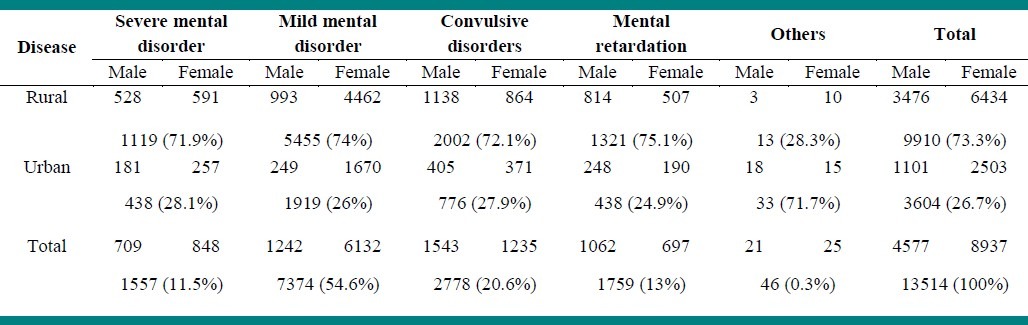
The mean populations who stayed in rural areas were 398000 persons, in whom 9910 newly psychiatric and convulsive disorders were diagnosed and followed. The mean populations who stayed in urban areas were 465000 persons, in whom 3604 new cases were detected. Ten years cumulative incidence of psychiatric disorder and convulsive disorders in rural and urban areas were estimated about 24.9 and 7.75 per 1000 population, respectively [Table 2]. The psychiatric disorders and seizure incidence are significantly higher in rural areas. (Chi square = 56.136, df = 4, P Value < 0.000). Overall 4577 (33.9%) patients were males and 8937 (66.1%) were females. Frequencies of mental disorders were significantly higher in females than males. (Chi square = 2.1, df = 4, P Value < 0.000).
Table 2.
Frequency of new mental disorder cases in ten years study in Chaharmahal and Bakhtyari Province (in I.R. Iran), per patients residences
During the survey, 590 (4.37%) new patients or 70 per 100000 populations have been hospitalized for inpatient mental care services. More than 70% of inpatients were from rural areas.
In the 10 years follow-up of patients who were screened as positive cases for mental disorders, 5551 (66.2%) cases were excluded from the study because of some reasons such as migration or were not attended in the study.
2474 cases were exempted from follow-up after their recoveries who were justified by their doctors and 359 (2.66%) cases died during the study [Table 3]. The death rate was significantly higher in rural areas (Chi square = 3.54, df = 8, P Value < 0.000). The death rate were significantly higher in patients with convulsive disorders than other mental disorders (Chi square = 1.41, df = 32, P Value < 0.000).
Table 3.
Causes of follow-up interruption in patients with mental disorders in ten years follow up in Chaharmahal and Bakhtyari Province in I.R. Iran

By extension of mental health integrations such as health promotion programs, targeting empowerment high risk population, the rate of completed suicides were reduced from 60 cases yearly (approximately 6 per 100000) in the first two years of conducting program to 27 – 30 cases yearly (2.97 – 3 per 100000 population).
DISCUSSION
Integration of mental health care program in general practice and involvement of GPs as providers raised patients’ satisfaction and improve their adherence to medication. The broad range of patients with different illnesses and co-morbidities received new highly accessible, acceptable and adoptable services that raised patients’ outcomes and cost effectiveness.[6,10,11] It was found no that there were no similar studies on the incidence rate of psychiatric disease in I.R. Iran, so comparing the results of this study with other researches would not be eligible.
The 12-month prevalence of mental disorders varies between countries, from 6.0% in Nigeria to 27.0% in the United States of America.[12] Based on many surveys, the prevalence of psychiatric disorders in Islamic Republic of Iran prior to 2004 was reported at least as 25.9% in women and 14.9% in men,[13] while in recent years, this was decreased to 14.3% and 7.34% in women and men, respectively.[14]
The incidence of mood disorders and cognitive disorders in present survey are lower in comparison with results of the epidemiological catchment area study where it was 1.59 per 100 person-years of risk (SE) or in Swedish Lundby study, where annual first incidence of depression was 0.76% for women and 0.43% for men (SE) or yearly incidence of cognitive disorders has been reported as 1.2 (SE).[15]
Low incidence of psychiatric diseases in this study (in comparison with western published researches) may be explained, firstly because I.R. Iran is located in Asia and incidence of mood disorders in eastern countries is lower than the western countries.[15] Secondly, the effect of mental health interventions in this long time (10 years length of study), particularly after integration of mental health in primary health care and reduction in the side effects of Iraq-Iran war situations, has improved the mental health status of the population.
It was possible that during this study, some patients were missed out especially since they went to private clinics in spite of mental health centers in urban areas. Fortunately, the mental health services being free of charge for visits and drugs costs in public centers, they have motivated patients especially severe ones to just refer to public mental health care services. However besides all these, patients with mild mental disorders may have had lower consultation with integrated mental health services in urban regions.
Higher diagnosed mental disorders in rural area than urban areas in this study may be due to the higher frequency of mental disorders in rural areas,[11] which was not mentioned in other studies basically.[15] Otherwise, this may be referred to screening pattern, in which, patient screening in rural areas was performed actively, in spite of urban areas where patients were screened passively. Also information system was more accurate in rural areas.[16]
There was a lack of clarity over the incidence of mental retardation (MR) in scientific resources and they were focused more on the prevalence of mental retardation approximately as 1% in population.[17] In our study, the previous mental retardation cases were excluded and only new diagnosed patients over 10 years of study entered, so ten years (MR) incidence will be as 2 per 1000 populations.
During this study, 2778 new convulsive disorders were diagnosed. Thus 10 years incidence of convulsive disorders would be about 0.33% in comparison with yearly incidence of 0.05% in scientific resources.[18]
The frequencies of mental disorders were present approximately two times more in women than in men, which was consistent with many other surveys.[8,13] In the survey that was done by Kessler et al., the mood disorder and anxiety were more prevalent in women while addiction and bipolarity disorders were common in men.[12]
Upon the Iranian National reports, major depressive disorders, phobia and epilepsy were the top three common psychiatric disorders.[13]
The depression and anxiety were the most common disease by the prevalence of 12.7% and 7% in Gubash survey in United Arabica.[19]
Despite the results of mentioned researches, in present study, mild mental disorders especially anxiety were the most frequent disorders and they constituted 54.6% of the total cases.
The most common causes of referred patients to specialized centers during this survey were epilepsy and seizure attacks and severe mental disorders. These findings would indicate the attention of health staffs on psychiatric emergencies, which is consistent with other study.[5,20]
The rate of admission to psychiatric services in South Africa was 150 per 100000 populations, which is much more than the rate in this study. These findings suggest that adequate service provision, accessible services, and accurate and continuous care following integrated mental health in our province reduced the mean bed occupancy ratio for inpatient treatment.[21] Integration of mental health services in primary care services significantly reduced (38% to 14%) the rate of referred patients from team to especially mental health services and psychiatrists and also increased the rate of access to mental health services in emergency needs.[20,22]
By deviating at least 10% of hospitals’ beds to mental disorder patients, there have been increased access to mental health inpatient cares. Following integration mental health into primary health care system, outpatient treatments and in otherwise access to specialized services particularly were developed. According to the WHO assessments, the number of referrals and admissions of under-covered patients in I.R. Iran is suitable.[16]
The best example of this success is decreasing the incidence of completed suicide to half after first two years and it was stabilized on approximately 3 per 100,000 populations yearly. In recent years, incidence rate of completed suicide in our study in all age was lower than this index in U.S.A.[23] While the inpatient treatments in this study ever is lower than other countries.[20] So the quality and duration of inpatient cares and the etiologies of patients’ death in addition to suicide should be evaluated in further studies.
CONCLUSION
Development of a system-wide approach to the provision of mental health as integrated care program offers the opportunity to increase the proportion of people with mental health problems who receive pleasant, fairly and more efficient treatments.
ACKNOWLEDGMENTS
We wish to thank the health staff of health networks in Chaharmahal and Bakhtyari province (administrators, psychiatrists, general physicians, experts and axillaries workers particularly behvarzes). Also we would like to thank the psychiatrists in either provincial or national level.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ronald Kessler C, Bedirhan Ustun T. The WHO World Mental Health Surveys. USA: Cambridge University Press; 2008. p. 144. [Google Scholar]
- 2.Mental Health Policy and Service Guidance Package. Geneva: World Health Organization; 2003. The Mental Health Content; pp. 12–20. [Google Scholar]
- 3.Yasamy MT, Gudarzi SS, Esmaeeli MA, Mahdavi N, Ebrahimpour A, Bageri Yazdi SA, et al. Practical Mental Health for General and Family Practitioner. Teheran: Aramesh Publisher; 2005. p. 12. [Google Scholar]
- 4.Mental Health Policy and Service Guidance Package. Geneva: World Health Organization; 2003. Organization of services for Mental Health; p. 16. [Google Scholar]
- 5.Pomerantz A, Brady H, Cole MA, Watts BV, Weeks WB. Improving efficiency and access to mental health care: Combining integrated care and advanced access. Gen Hosp Psychiatry. 2008;30:546–51. doi: 10.1016/j.genhosppsych.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Giel Hutschemaekers JM, Bea Tiemens G, de Winter M. Effects and side-effects of integrating care: The case of mental health care in the Netherlands. Int J Integr Care. 2007;7:e31. doi: 10.5334/ijic.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lum AM, Kwok KW, Chong SA. Providing integrated mental health services in the Singapore primary care setting – the general practitioner psychiatric programme experience. Ann Acad Med Singapore. 2008;37:128–31. [PubMed] [Google Scholar]
- 8.WHO-Aims Report on Mental Health system in the Islamic Republic of Iran. Teheran: World Health Organization; 2006. pp. 8–12. [Google Scholar]
- 9.Bregman JD, Harris JC. Mental retardation. In: Harold Kaplan I, Benjamin J, Sadock J., editors. Comprehensive textbook of Psychiatry. 6th ed. Vol. 3. USA: Williams & Wilkins; 1995. p. 2208. [Google Scholar]
- 10.Harmon K, Carr VJ, Lewin TJ. Comparison of integrated and consultation-liaison models for providing mental health care in general practice in New South Wales, Australia. J Adv Nurs. 2000;32:1459–66. doi: 10.1046/j.1365-2648.2000.01616.x. [DOI] [PubMed] [Google Scholar]
- 11.England E, Lester H. Integrated mental health services in England: A policy paradox. Int J Integr Care. 2005;5:e24. doi: 10.5334/ijic.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Ustun TB. The WHO World Mental Health Surveys. USA: Cambridge University Press; 2008. pp. 534–5. [Google Scholar]
- 13.Noorbala AA, Baghei SA, Yasamy SA, Mohammad K. Mental health survey of the adult population in Iran. Br J Psychiatry. 2004;184:70–3. doi: 10.1192/bjp.184.1.70. [DOI] [PubMed] [Google Scholar]
- 14.Mohammadi MR, Davidian H, Noorbala AA, Malekafzali H, Naghavi HR, Pouretemad HR, et al. An epidemiological survey of psychiatric disorders in Iran. Clin Pract Epidemiol Ment Health. 2005;1:16. doi: 10.1186/1745-0179-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rihmer Z, Angst J. Comprehensive textbook of psychiatry. 9th ed. Vol. 2. Philadelphia USA: Lippincott Williams & Wilkins; 2009. Mood disorder epidemiology: Kaplan & Sadock's; pp. 1577–647. [Google Scholar]
- 16.WHO-Aims Report on Mental Health system in the Islamic Republic of Iran. Teheran: World Health Organization; 2006. p. 26. [Google Scholar]
- 17.Bryan KH, Hodapp RM, Dykens EM. Comprehensive textbook of psychiatry. 9th ed. Vol. 4. Philadelphia: Lippincott Williams & Wilkins; 2009. Intellectual Disability Kaplan & Sadock's; p. 3453. [Google Scholar]
- 18.Mendez MF. Kaplan & Sadock's; Comprehensive textbook of psychiatry. 9th ed. Philadelphia: Lippincott Williams & Wilkins; 2009. Neuropsychiatric aspect of Epilepsy; p. 452. [Google Scholar]
- 19.Ghubash R, Hamidi E, Belbington P. The Dubu: Community psychiatvic Survey. Soc Psychiatry Psychiatr Epidemiol. 1992;27:53–61. doi: 10.1007/BF00788506. [DOI] [PubMed] [Google Scholar]
- 20.Felker BL, Barnes RF, Greenberg DM, Chaney EF, Shores MM, Gillespie-Gateley L, et al. Preliminary outcomes from an integrated mental health primary care team. Psychiatr Serv. 2004;55:442–4. doi: 10.1176/appi.ps.55.4.442. [DOI] [PubMed] [Google Scholar]
- 21.Lund C, Flisher AJ. South African mental health process indicators. J Ment Health Policy Econ. 2001;4:9–16. [PubMed] [Google Scholar]
- 22.Van Rijswijk E, Borghuis M, Van de Lisdonk E, Zitman F, Van Weel C. Treatment of mental health problems in general practice: A survey of psychotropics prescribed and other treatments provided. Int J Clin Pharmacol Ther. 2007;45:23–9. doi: 10.5414/cpp45023. [DOI] [PubMed] [Google Scholar]
- 23.Wagner KD, Brent DA. Kaplan & Sadock's; Comprehensive textbook of psychiatry. 9th ed. Vol. 4. Philadelphia: Lippincott Williams & Wilkins; 2009. Depression disorders and suicide; p. 3658. [Google Scholar]


