Abstract
Chronic pain is a significant public health problem in the United States. While the understanding that pain is an important biological signal has always been appreciated by health care professionals, management of pain has now come under significant scrutiny following its recognition as the fifth vital sign. Since the measurement of pain is not objective, the answers to questions regarding how to best manage the problem are not always self-evident. Multiple modalities, including interventional procedures and noninvasive techniques, are available for the treatment of pain. Acute pain is usually self-limiting when a reversible element can be identified. If acute pain is undertreated, it may become chronic in nature with the attendant problems of prolonged pain. Chronic pain creates psychological and social problems that are difficult and frustrating for both patient and physician. A multimodal therapeutic program in which the patient is an active participant can satisfactorily manage most pain problems. The use of opioids is considered legitimate medical therapy for chronic nonmalignant pain. If the need for opioid therapy is felt to be indicated, the physician should adhere to recommended guidelines as published by state licensing boards and professional organizations. Successful pain management is a rewarding experience for health care professionals.
“We must all die. But that I can save him from days of torture, that is what I feel as my great and ever new privilege. Pain is a more terrible lord of mankind than even death itself.” (1)
Thus wrote Albert Schweitzer, physician, humanitarian and Nobel Prize Laureate in 1931. His words elegantly describe the nature of pain and the obligation of health care providers to relieve it. Unfortunately, until recently the management of pain has occupied a small if any portion of the curriculum in the training of health care professionals. The historical mindset regarding the use of opiates in the relief of pain is exemplified by Lee (2) who wrote in the Journal of the American Medical Association in 1941:
The use of narcotics in terminal cancer is to be condemned if it can possibly be avoided. Morphine and terminal cancer are in no way synonymous. Morphine usage is an unpleasant experience to the majority of human subjects because of its undesirable side effects. Dominant in the list of these unfortunate effects is addiction.
Even as late as the year 2000, patients with pain were managed so as to provoke the following comments from a health care provider:
I am a 46-year-old registered nurse who specializes in oncology care and education. I am also a patient who suffers from chronic nonmalignant pain, and this malady has been the most frightening, the most humiliating, and the most difficult ordeal of my life. The general tenor of medical advice was this: I would just have to live with the pain…. I found myself begging, as though I were a criminal. Defensive and angry and yet in such great need, I would beg forgiveness for having pain. I became withdrawn, completely disabled by my terrible relentless pain. I was unable to be much of a wife or a mother, a daughter or a friend… Now when I see unnecessary suffering caused by intractable, mismanaged chronic pain I am disgusted. As a health care provider, I am ashamed (3).
Chronic pain is now recognized as a major public health problem and has been described as America's most common and debilitating disorder. It is estimated that 40–50 million people in the United States suffer from chronic pain. The financial cost of pain in the United States is more than $100 billion in lost productivity, lost income, and health care expenditures (4). Many health care providers know little about the etiology of pain and the wide array of treatments that are available today, and the Joint Commission on Accreditation of Health Care Organizations recently released guidelines urging health care facilities to access pain in all patients.
HISTORICAL NOTES AND TERMINOLOGY
Opioids have been the mainstay of pain treatment for thousands of years and remain so today. The first reference to opium is found in the writings of Theophrastus (5), and many of the uses of opium were appreciated during the Middle Ages. In 1680, Sydenham wrote, “Among the remedies it has pleased Almighty God to give to man to relieve his sufferings, none is so universal and so effacious as opium.” During and after the Civil War there was widespread use and abuse of morphine. Hence, in 1904 the Harrison Narcotic Act was passed creating responsibility and documentation of drug usage.
The term opioid refers to all compounds related to opium. Opiates are drugs derived from opium and include morphine, codeine, and thebaine as well as semisynthetic congeners derived from them. Endorphins is the term describing endogenous opioid peptides while also referring to the specific endogenous opioid, beta-endorphin. The word narcotic was derived from the Greek word for stupor. It is commonly used when reference is made to substances with abuse potential. The term opioid has become more inclusive and refers to all agonists—antagonists with morphine-like activity—whether they are naturally occurring or synthetic compounds.
The earliest concepts of pain mechanisms are credited to Descartes (6). For some time, there had been a search for a pain center in the brain. Injury was said to activate pain receptors, which projected afferent impulses to the supposed brain center via the spinal pathway. Pain was held to be proportional to the injury or disease. Psychological contributions such as attention, experience, or the situation were not felt to be significant contributors to the perceived pain. In essence this format of specificity relied primarily on peripheral mechanisms and considered the brain a passive receptor.
Many investigators attempted to develop a new theory, and in 1965 Melzack and colleagues published the gate control theory of pain (6). The emphasis on the central nervous system as an integral component in the mechanism of pain is the most important contribution of the gate control theory. This concept proposed that transmission cells, or T cells, located in the dorsal horn of the spinal cord, project to the brain. Further research has revealed that the dorsal horn is not merely a passive conduit of impulses, but rather is the site of a host of peptide and amino acid neurotransmitters and neuromodulators. Such neurotransmission via the dorsal horn encompasses excitatory transmitters from central terminals of primary afferent nociceptors, excitatory transmitters released between neurons of the spinal cord, and inhibitory transmitters released by interneurons within the spinal cord (7). The dorsal horn of the medulla and spinal cord are, therefore, major termination sites of nearly all sensory afferents irrespective of peripheral origin. Release of a single transmitter does not seem to apply since two or more compounds are commonly released at the same time. Quantities of neurotransmitter release are usually dependent upon stimulus intensity.
Pain transmission is a complex combination of neural transmission and molecular mechanisms as evidenced by the isolation of multiple substances. Stimuli that produce cutaneous pain do so by acting on primary afferent nociceptors. Such nociceptors are widespread in skin, muscle, connective tissue, blood vessels, and thoracic and abdominal viscera. Afferent nociceptors are pseudounipolar neurons with the cell body in the dorsal root ganglion (DRG). The peripheral axon terminal not only transduces mechanical, chemical, and thermal stimuli into a series of action potentials related to the spinal cord, it also releases many peptides in response to injury. Several such peptides that contribute to the peripheral inflammatory process are substance P, calcitonin gene-related peptide (CGRP), and neurokinin A. Additional compounds felt to be related chemically to peripheral injury include hydrogen ions, bradykinin, prostanoids, tumor necrosis factor (TNF), and endogenous vasoactive catecholamines such a norepinephrine (7). Nociceptors may be up- or down-regulated depending on the specific circumstances.
The sympathetic nervous system is a common contributor in pain syndromes, which were previously classified as reflex sympathetic dystrophy or causalgia, depending on the absence or presence of macroscopic nerve injury. Current terminology has classified these entities as complex regional pain syndromes (CRPS) II and I, respectively. Clinical features of CRPS reflect autonomic dysfunction. Vasomotor and sudomotor changes are clinically seen as sensory symptoms of burning pain, hyperalgesia, and allodynia. Associated motor dysfunction is not uncommon. Other compounds that further reflect the molecular mechanisms' aspect of pain are certain amino acids found in high concentrations within the central nervous system. Substances such as gamma aminobutyric acid and glycine may produce inhibition of nociceptive input. Down-regulation or lack of these amino acids may result in neuropathic pain such as allodynia.
The explanation of pain mechanisms with the introduction of the gate theory, combined with multiple molecular mechanisms, has dramatically increased our understanding of neural physiology. Clinically, phantom limb or pain in patients with cord transection does not fit these theories. Painful phantoms point out the need to know more about the brain. Melzack has proposed a theory that purports a large, widespread network of neurons between the thalamus and the cortex and between the cortex and the limbic system (6). He has labeled this entire network as a neuromatrix. Repeated cyclic processing and synthesis of nerve impulses through the neuromatrix imparts a characteristic pattern labeled as the neurosignature (6). This neurosignature creates a neuromodule which remains and produces output in the signature patterns; hence “phantom pain.” Multiple treatment remedies have been attempted, but none are universally effective.
CLINICAL PAIN DEFINITIONS
Pain, as defined by the International Association for the Study of Pain, is an unpleasant sensory and emotional experience that is associated with or described in terms of either potential or actual tissue damage (7). Acute and chronic pain are completely different entities (Tables 1, 2). Pain evaluation is now the so-called fifth vital sign. However, since the assessment of pain is subjective, it is not as easily quantified as pulse, blood pressure, temperature, and respirations. Pain is thereby more difficult to evaluate because it evokes emotional responses that vary even though patients may have comparable injuries. It is important to remember that along with pain there is suffering which further complicates clinical evaluation.
Table 1.
Characterizations of acute pain.
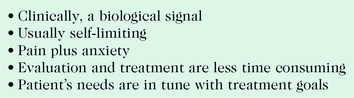
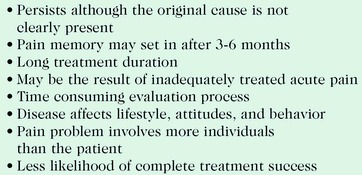
Table 2.
Characterizations of chronic pain.
Clinical pathophysiologic aspects of pain are related to stimuli that produce cutaneous pain by acting on primary afferent nociceptors. As noted previously, these receptors are widespread in their distribution. The cell body of primary afferent nociceptors is located in the DRG.
When the axon terminal releases such peptides as substance P, CGRP, and neurokinin A, clinical findings are those of vasodilation, edema, and hyperalgesia. Common patient complaints describe such pain as aching, throbbing, and gnawing. It is important to note that this type of pain is opioid sensitive. Symptoms associated with visceral nociceptors are usually associated with sympathetically innervated organs. Such symptoms are described as deep, colicky, and paroxysmal in nature.
Neuropathic Pain
Neuropathic pain is associated with injury to peripheral or central nervous system structures. Such pain may also be the result of abnormal pain processing. Such pain is not mediated by nociceptors in the periphery, but may be the result of damage, with resultant pathologic changes in functional relationships causing chronic persistent pain. Examples of such changes are peripheral sensitizations of nociceptors, central sensitization, abnormal sympathetic somatic nervous system interactions, and abnormal activation of N-methyl-D-aspartate (NMDA) receptors (8). Neuropathic pain is frequently described as tingling, burning, and shooting. Physical examination may reveal sensory loss in the affected area. Neuropathic pain may be opioid sensitive or unresponsive.
Psychogenic Pain
Psychogenic pain is highly controversial. It is associated with emotional responses, which clinically present as anxiety, depression, anger, irritability, and frustration. The presence of several of the preceding symptoms or findings will frequently be present in the chronic pain patient. As such, these patients are frequently not managed properly since they may be inappropriately categorized as not having true physical pain.
Pain Management Therapeutic Agents
The use of drugs for pain management remains a highly controversial subject, especially regarding the use of opioids. The presence of an endogenous opioid system was unknown until the early 1970s. Endogenous opioids include enkephalins, endorphins, and dynorphins. Much of our understanding of drug action is related to receptor specificity, and the pharmacological action of opioids is mediated via specific receptor binding. The following actions are noted when such receptors are stimulated:
Delta-enkephalins
Kappa – bradycardia, euphoria, ileus, sedation, miosis
Table 3.
Common mu receptor agonists.
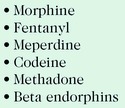
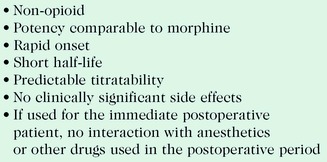
Table 4.
Characteristics of the ideal analgesic.
ACUTE PAIN MANAGEMENT
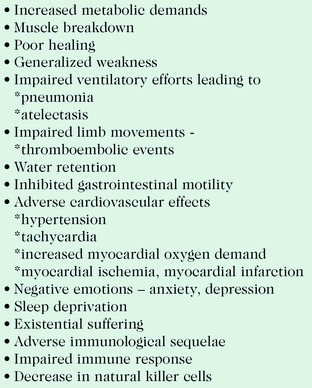
Management of acute pain can be idealized in the postsurgical patient who has need of immediate pain control. It is important to note that under-treatment of acute pain is associated with adverse physiological and psychological effects (Table 5). The following techniques are most commonly utilized in the postsurgical patient but can also be effective for the nonsurgical patient.
Table 5.
Physical and psychological effects of under-treatment of acute pain.
Patient-Controlled Analgesia
Patient-controlled analgesia (PCA) is administered intravenously intermittently with or without a continuous background infusion. Commonly utilized opioids are morphine, dilaudid, and meperdine (Demerol). Dose is limited by the lockout interval. This method allows patients to exert a degree of control, which makes for high patient satisfaction.
Patient-Controlled Epidural Analgesia
With patient-controlled epidural analgesia, a catheter is placed in the lumbar or thoracic vertebral interspace, depending on the location of the pain problem. Usual combinations include a local anesthetic, which may be combined with an opioid. Usually, a continuous background rate is maintained with intermittent patient-controlled bolus dose. This is a highly effective method for relief of severe acute pain.
Interventional Techniques
Other techniques include nerve, regional, or plexus blocks using local anesthetics. A catheter may be introduced to the affected area or surgical wound site that is connected to a mobile reservoir containing local anesthetic which releases a predetermined amount for a specified period of time. The catheter is easily removed by the patient if used in the outpatient setting and, therefore, may be used as an in- or outpatient modality. In the surgical patient, administration of certain drugs or local anesthetics applied to the surgical field prior to the incision may decrease the need for opioids in the postoperative period. The idea in this setting is that it is easier to manage prevention of afferent, evoked facilitation than to deal with the sequelae (8).
NSAIDs and COX Inhibition
Many agents are available for the treatment of acute and chronic pain. The nonsteriodal anti-inflammatory drugs (NSAIDs) provide an additional, unique, and valuable pharmacotherapy that can be effective in patients with such pain. The mode of action NSAIDs has been defined to a greater extent in recent years: inhibition of cyclooxygenase (COX), the enzyme responsible for prostaglandin production, is thought to be the mechanism of action. Prostaglandins are present in almost all body tissues and fluids. It is now appreciated that there are two forms of cyclooxygenase: Cox 1 and Cox 2. Cox 1 is found in most normal cells and is known to have protective action in the gastric mucosa and maintenance of renal function. Cox 2 is said to be inducible, and thereby responds to inflammatory mediators. The recent introduction of Cox 2-specific inhibitors has promise in a variety of clinical settings (9). The combination of NSAIDs and opioids can be a highly effective mode of therapy in the acute pain setting while sparing the use of opioids.
CHRONIC PAIN MANAGEMENT
Chronic pain is a difficult and frustrating experience for both the patient and the physician. Cancer pain management is not quite as formidable since a clear relationship between the disease and the patient's pain can be identified. Use of multidrug therapy including opioids administered by enteral, systemic, or intrathecal routes are viable options.One would think that pain management in the terminal patient would be well recognized in modern day medical practice. Several years ago, Bill Moyers hosted a program on PBS entitled The Way We Die. Each person interviewed was in the throes of a disease soon to be fatal. Several of the individuals were physicians. All were questioned as to what was their greatest concern. Each responded without hesitation that they might not receive adequate pain relief. The goal in the chronic pain patient is improvement in the patient's quality of life. If the patient is made to feel that they are not going to be abandoned and accepts an active role in the treatment program, success is likely.
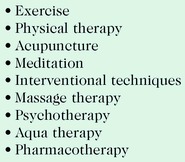
Evaluation of the chronic pain patient must initially include a complete history and appropriate physical examination. Review of circumstances that create or aggravate pain, activities of daily living, and sleep habits is critical since these elements must be explored. It is of utmost importance to understand that the interpersonal relationships of such patients are not infrequently strained and must be addressed. It is a common finding in many patients that depression plays a significant role and, if indicated, a psychiatric consultation should be considered. Prior diagnostic studies should be reviewed in order to determine if any further testing is required to clarify the problem: what therapies have been previously utilized and which have been helpful? A treatment plan with goals should be formulated with the patient made to understand that they are an active participant in their treatment program. Good health habits must be encouraged such as weight reduction, smoking cessation, and—at the minimum—a cardiovascular exercise program. Chronic pain management success is most often achieved using a multimodal approach (Table 6).
Table 6.
Useful modalities for the treatment of chronic pain.
Chronic Pain Conditions
Chronic pain conditions deserve mention. Osteoarthritis (OA) is probably present to some degree in all patients 65 years or older. Myofasical pain syndrome (MPS) is characterized by complaints of regional pain that may frequently be reproduced by palpation of specific areas which are noted to be tender, i.e. trigger points. Injection of such areas with local anesthetics, with or without steroids, is frequently beneficial. Fibromyalgia (FM) is soft tissue chronic pain syndrome, whose existence is doubted by many physicians (9). Generalized aching and diffuse musculoskeletal pain is present along with fatigue, which is related to non-restful sleep in patients with FM. Treatment is usually a combination of the previously mentioned modalities.
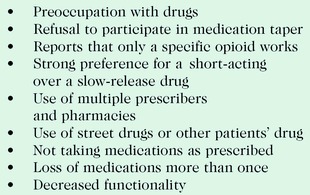
Dependence, Abuse, and Addiction
It is important in the management of the chronic pain patient that the physician believes that the patient's complaints are genuine. This does not imply that there are not individuals who are involved in drug-seeking. Hence, a physician is obligated to attempt an evaluation regarding the legitimacy of the patient's complaints. The question as to whether the patient is involved in illegal activities places another burden upon the physician. In essence, is the patient a drug abuser or a drug diverter (Table 7)? It is important to recall the phenomena of tolerance, i.e., requiring increasing drug to achieve pain relief. Dependence develops as a result of adaptation in response to repeated drug use. The only evidence of physical dependence occurs upon termination of the drug, which clinically presents as central nervous system hyperarousal (10). Neither of these conditions is necessarily equated to addiction. Addiction is said to be present when an individual continues use of the substance despite a decreased quality of life. Addiction is rare with prescribed drugs in the treatment of chronic pain. Slow-release forms of opioids are generally said to have less potential of addiction.
Table 7.
Common warning signs that a pain patient may be a drug abuser or a drug diverter.
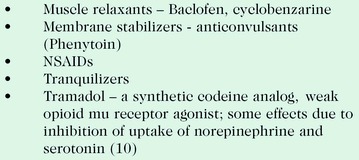
Drug Combinations
Drug combinations are frequently useful in the treatment of acute and chronic pain. Classes of commonly effective drugs are described in Table 8. The following are common questions and concerns regarding safe and effective use of multidrug therapy.
Table 8.
Classes of drugs commonly and effectively used in the combination treatment of acute and chronic pain.
Use only one analgesic for pain control?
The use of one from each group is often more effective.
Use only one NSAID and, when possible, only one opioid.
Combining analgesics
The use of acetaminophen and any other analgesic is acceptable, common practice.
Combining acetaminophen and an NSAID is an acceptable, common practice.
NSAID combinations are unacceptable: additional pain relief is minimal.
Is it acceptable to administer an opioid, NSAID, and adjuvants (antidepressants and/or anticonvulsant) for pain control?
It is acceptable to administer several drugs when they each work by different mechanisms.
What are some acceptable combinations of analgesics?
Adjuvant opioid, acetaminophen, and an NSAID are appropriate for chronic pain and can be used for acute pain in certain circumstances.
What adjuvant combinations are useful in chronic pain?
Antidepressants and anticonvulsants
Is it dangerous to administer opioids and NSAIDs at the same time?
If each is safe for the patient, it is more convenient to give them together, and it is unnecessary to administer them at different times.
If a non-opioid does not relieve pain, discontinue and give an opioid?
When pain is severe enough to require opioid, non-opioid may be continued.
Use of mu-agonist and agonist-antagonist?
Rarely appropriate
Mu-agonist combinations: usually not necessary, but can combine a shorter-acting with slow-release for breakthrough pain.
Steroid use?
Corticosteriod and NSAID: use cautiously, as prolonged administration increases side effects such as GI bleeding.
Acute pain combination
Combination of opioid, non-opioid, and acetaminophen is highly recommended.
Many physicians have concerns regarding the use of opioids in the management of chronic noncancerous pain. They may feel that their medical licensure is at risk in such circumstances. Most state medical licensing boards have addressed this particular issue and have published rules regarding the use of such drugs in the treatment of noncancerous pain. It behooves all physicians to become familiar with their particular state board rules in this matter. The goal of both federal and state rules is to insure that a therapeutic drug is available when needed. I have been involved in the construction of the rules of the Louisiana State Board of Medical Examiners regarding the use of opioids in the treatment of nonmalignant pain (11). Most states have followed guidelines developed by the Federation of State Medical Boards.
The following guidelines will be helpful regarding opioid use in chronic nonmalignant pain.
Complete history and appropriate physical examination at initial evaluation.
Review all pertinent diagnostic work-up.
Establish a working diagnosis.
-
Fully disclose potential side effects and complications of opioids, with ample opportunity for discussion with the patient.
a. Document that this information and discussion have been made available to the patient.
-
A contract is recommended stating that the patient agrees minimally to the following:
a. They will obtain opioids only through the physician so-named.
b. They will not call after hours for medication.
c. They will not obtain weekend medications unless the designated physician is contacted.
d. They will agree to drug testing at the discretion of the prescribing physician.
e. They will understand that the use of only one pharmacy is recommended.
f. They understand that they may be discharged from the program if violation of the agreement occurs.
g. They should be seen every 3 months to assess the efficacy of treatment, evaluate progress toward treatment goals, and note any adverse drug reactions. Indications of drug abuse or diversion must be evaluated.
h. They understand that treatment goals will be stated in the medical record, viz., an increase in physical activity and potential decrease in opioid use.
i. They will agree to reevaluation and consideration of consultation with a pain specialist or other physician as indicated.
j. They understand that any telephone conversations, especially those regarding medication response or symptom change, will be documented in their medical record.
CONCLUSIONS AND SUMMARY
Pain has historically been under-treated. Acute pain can be managed by multiple treatment regimens ranging from oral medications to interventional procedures. Acute pain can become chronic if not relieved appropriately. Chronic pain can be frustrating to both physicians and patients alike. A multimodal approach will have the greatest degree of success in chronic pain patients. Opioid therapy by multiple routes of administration is legitimate medical therapy for the treatment of the chronic pain patient. The use of opioids for long-term pain control should be made available to chronic pain patients with adherence to recommended guidelines.
Footnotes
Following suggested as concise clinical reference: Principles of Analgesic Use in the Treatment of Acute Pain and Cancer Pain 4th ed: Glenview, IL, American Pain Society.
Dr. Mack Thomas is on staff in Ochsner's Department of Anesthesiology. He served as the Director of the Acute and Chronic Pain Program at the New Orleans Veterans Administration Hospital 1980–2001, established and served as the Medical Director for the Acute and Chronic Pain Programs at Kenner Regional Medical Center in Kenner, LA 1985–1999, and was the Chairman for the State of Louisiana Pain Management Committee responsible for developing State guidelines for pain management.
REFERENCES
- Bonica J. J. History of pain concepts and therapies. 1990:2–13. In: Bonica JJ, et al. Editors. The Management of Pain. 2nd Edition. Malvern, PA: Lea & Febiger. [Google Scholar]
- Lee L. E. Medication in the control of pain in terminal cancer with reference to study of newer synthetic analgesics. JAMA. 1941;116:216–220. [Google Scholar]
- Aronoff G. M. Opioids in chronic pain management: is there a significant risk of addiction? Curr Rev Pain. 2000;4:112–121. doi: 10.1007/s11916-000-0044-0. [DOI] [PubMed] [Google Scholar]
- Romano T. J. Essentials of Chronic Pain Management. Anesthesia Today. 2001;12:1–23. New Providence, NJ: Baxter Healthcare Corp. [Google Scholar]
- Gutstein H. B., Akil H. Opioid analgesics and antagonists. 2001:569–620. In: Hardman JG, Limbird LE, editors. Goodman & Gilman's Pharmacological Basis of Therapeutics. 10th Edition. New York: McGraw-Hill. [Google Scholar]
- Melzack R. Toward a new concept of pain for the new millennium. 2001:1–10. In: Waldman SD, editor. Interventional Pain Management, 2nd edition. Philadelphia: Saunders. [Google Scholar]
- Siddall P. J., Hudspith M. J., Munglani R. Sensory systems and pain. 2000:213–232. In: Hemmings HC Jr, Hopkins PM, editors. Foundations of Anesthesia: Basic and Clinical Science. Philadelphia: Mosby. [Google Scholar]
- Salgo P. L. The pain management challenge. Medical Crossfire-Conference proceedings. 2002;4:30–42. In: Pinho N, managing editor. [Google Scholar]
- Yaksh T. L. Pharmacology of the pain-processing system. 2001:21–34. In: Waldman SD, editor. Interventional Pain Management. Philadelphia: Mosby. [Google Scholar]
- Roberts J. L., II, Morrow J. D. Analgesic-antipyretic and antiiflammatory agents and drugs employed in the treatment of gout. 2001:687–691. In: Hardman JG, Limbird LE, editors, Goodman & Gilman's Pharmacological Basis of Therapeutics 10th Edition. New York: McGraw-Hill. [Google Scholar]
- Louisiana State Board of Examiners. Use of controlled substances, limitations. Louisiana Register. April 20;2000:26–4. [Google Scholar]


