Abstract
Purpose. Evaluation of the short implant (8 mm in height) long-term prognosis and of the implant site influence on the prognosis. Methods. A longitudinal study was carried out on 121 patients (57 males and 64 females) consecutively treated with 257 implants. 108 implants were short. Results. Four (3.6%) short implants supporting fixed partial prostheses failed. Similarly, three standard implants supporting fixed partial prostheses and one supporting single-crown prosthesis failed. Mean marginal bone loss (MBL) and probing depth (PD) of short and standard implants were statistically comparable (P > .05). The 20-year cumulative survival rates of short and standard implants were 92.3 and 95.9%, respectively. The cumulative success rates were 78.3 and 81.4%. The survival rates of short implants in posterior and anterior regions were comparable: 95 and 96.4%, respectively. The difference between survival rates was not significant (P > .05). Conclusions. The high reliability of short implants in supporting fixed prostheses was confirmed. Short and standard implants long-term prognoses were not significantly different. The prognosis of short implants in posterior regions was comparable to that of in anterior regions. Nevertheless, a larger sample is required to confirm this trend.
1. Introduction
Actual patient's expectations for prosthetic rehabilitation are increasingly high, especially with regard to quality of life and functionality. The introduction of dental implants has led to a turning point in the rehabilitation of partially or totally edentulous patients [1]. However, not always, the placement of dental standard length implants is possible or feasible in the first instance. Several anatomical conditions affect the rehabilitation treatment and have an impact on costs and morbidity for the patient. An example is the rehabilitation of the maxillary posterior regions. Excessive pneumatization of the maxillary sinus or marked resorption of the edentulous alveolar ridge are factors that may lead to look for different solutions. Thus, techniques such as the elevation of the maxillary sinus or the use of length-reduced implants have been introduced to allow an implant rehabilitation even though these anatomical peculiarities [2].
The risk of morbidity, the cost, and time for the treatment of sinus elevation should be taken into account when an implant rehabilitation in the maxilla is necessary.
So the use of short implants can be an alternative in these cases although, historically, they were associated with low success rates. Recent studies in fact show that short implants can reach satisfactory clinical levels of reliability and survival [3–8]. These results were also due to the introduction of rough-surface implants that permit the decrease of implant length while ensuring an adequate contact between bone and fixture.
Therefore, the use of short implants allows an implant rehabilitation for the patient without the surgical involvement of delicate structures such as the maxillary sinus.
The aim of the present longitudinal study was to evaluate the survival of short implants when compared to that of standard implants in a long-period follow-up. A secondary aim was to compare the prognosis of short implants placed in posterior regions (molars and second premolar) to that of short implants placed in anterior regions (incisors, canine, and first premolar).
2. Materials and Methods
2.1. Patients
Between April 1990 and June 2010, 121 patients (57 males and 64 females) with a mean age of 54 years (range 22 to 69 years) were consecutively treated in the Dental Clinic, Department of Medicine, Surgery and Dentistry, University of Milan, Italy. The follow-up after prosthesis installation ranged from 10 to 21 years (mean 13.2 years).
Criteria for implant placement included: good general health at the time of surgical procedure, favourable intermaxillary relationship, and adequate bone volume on implant site (at least for 8 mm in length) radiographically evaluated.
Exclusion criteria were: alcohol or tobacco abuse; sever renal or liver disease; history of radiotherapy in the head and neck region; chemotherapy for malignant tumors at the time of surgical procedure; uncontrolled diabetes; periodontal disease involving the residual dentition; mucosal disease, such as lichen planus in the area to be treated; poor oral hygiene; noncompliant patients; patients with a need for prostheses supported by combined short and standard implants used in combination; narrow-diameter implants (i.e., 3.3 mm).
Patients received no more than 1 implant-supported prosthesis each.
Calibrated plastic probe and juxtagingival radiographs taken before treatment were used to evaluate crown-to-implant ratio. Implant distribution according to opposing teeth or prostheses was considered: short and standard implants opposing mobile partial or total prostheses were excluded from the study.
The routine treatment of patients was documented as follows.
Panoramic radiographs taken before treatment.
Periapical radiographs taken before treatment, at the time of implant placement at the time of prosthetic rehabilitation, and every year thereafter.
Computed tomography (CT) scans whenever radiographs were not sufficient to plan the implant treatment (27 patients showing severe atrophic ridges).
2.2. Examinations
Two hundred fifty-seven straight, 2-part, grade IV, pure titanium, solid screw, ITI (Institute Straumann, Waldenburg/BL, Switzerland) plasma-spayed dental implants were placed. One hundred and eight of them were short (8 mm in length), while 149 were standard (10 mm). Implant distribution by diameter and length is reported in Table 1.
Table 1.
Implant distribution by diameter, length, and type.
| Length | Diameter | No. |
|---|---|---|
| 8 mm | 3.75 mm | 21 |
| 4.1 mm | 66 | |
| 4.8 mm | 21 | |
|
| ||
| 108 | ||
|
| ||
| 10 mm | 3.75 mm | 33 |
| 4.1 mm | 89 | |
| 4.8 mm | 37 | |
|
| ||
| 149 | ||
Fourty-two and 66 short implants were placed in the maxilla and mandible, respectively. On the hand, 63 and 86 standard implants were placed in the maxilla and mandible, respectively. The following regions were considered: anterior and posterior maxilla, anterior and posterior mandible. Anterior region included the canine and incisive districts; posterior region included premolars and molars (Table 2).
Table 2.
Implant lengths and locations.
| Implant length | District | Implants |
|---|---|---|
| 8 mm | maxillary anterior | 18 |
| maxillary posterior | 24 | |
| mandibular anterior | 10 | |
| mandibular posterior | 56 | |
|
| ||
| 10 mm | maxillary anterior | 16 |
| maxillary posterior | 47 | |
| mandibular anterior | 17 | |
| mandibular posterior | 69 | |
Overall, 44 and 77 prostheses were positioned in the maxilla and mandible, respectively. The following prostheses were used (Table 3): 52 fixed single-tooth prostheses (ST), 58 fixed partial prostheses (FPD), and 11 fixed complete dentures (FCD).
Table 3.
Implant distribution by prosthesis type.
| Prostheses type | Implants | |
|---|---|---|
| (8 mm) | (10 mm) | |
| FPD | 56 (24)∗ | 38 (16)∗ |
| FCD | 26 (4)∗ | 22 (4)∗ |
| ST | 26 (26)∗ | 11 (11)∗ |
|
| ||
| Total | 108 (54)∗ | 71 (67)∗ |
∗Number of prostheses supported by the implants are in brackets.
ST: single tooth prosthesis.
FCD: fixed complete dentures.
PFD: partial fixed dentures.
If a patient could not be followed at consecutive annual examination, the corresponding implants were classified as “drop-out implants.” The reasons for dropouts were lack of interest in attending the examinations (n = 9) and moving out of the area (n = 7). Moreover, 14 patients could not be reached. Thus, a total of 30 patients with 50 implants were excluded from the follow-up protocol. The prostheses included 11 FPDs and 19 STs.
2.3. Prosthetic Treatment
Following a healing period of 3 to 4 months in the mandible and 4 to 6 months in the maxilla, patients were recalled for a preprosthetic evaluation; healing duration was based on bone quality [9]. After healing abutments removal (three to six months from implant placement), the prosthetic abutments were connected as recommended by the manufacturers.
Prosthesis frameworks and aesthetic veneer were fabricated in gold alloy and porcelain, respectively. No welding was performed. Cemented prostheses were fixed with zinc oxyphosphate cement (32 FPD, 44 ST, and 3 FCD prostheses) or zinc-oxide eugenol cement (14 FPD prostheses), while screw-retained prostheses (8 FCD, 12 FPD, and 8 ST prostheses) were secured to the abutments by means of abutment-framework screws using a manual torque driver. Twenty-one temporary prostheses were used to restore anterior teeth. Opposite dentition was natural teeth and fixed prostheses for 185 and 72 implants, respectively.
2.4. Assessments
Implants were followed with Annual clinical examinations and juxta-gingival radiographs were carried out. The following parameters were evaluated.
Radiographic assessment of peri-implant bone resorption (MBL) mesial and distal to each implant. MBL was determined by comparing juxta-gingival radiographs taken at the time of prosthetic loading, and every year thereafter. The distance between the apex of the implant and the most coronal level of direct bone-to-implant contact was measured mesially and distally to each implant by means of computerized analysis (Canoscan radiograph scanner and Image-J software) [10]. Intraoral radiographs (Kodak Ekta-speed EP-22, Eastman Kodak Co., Rochester, NY, USA) were taken with parallel technique to control projection geometry: the following exposure parameters (65–90 kV, 7.5–10 mA, and 0.22–0.25 s) were used. Dimensional distortion related to the juxta-gingival radiographs was corrected comparing the actual dimensions of the loaded implants to the image on film.
Peri-implant soft tissue parameter such as Probing Depth (PD) was measured with a calibrated plastic probe (TPS probe, Vivadent, Schaan, Liechtenstein) at the time of prosthetic loading and every year thereafter. Probing depth scores were recorded at 4 sites for each implant (mesial, distal, buccal, and lingual).
2.5. Prognostic Criteria
Implant stability, peri-implant conditions, marginal bone loss, and other treatment-related complications, as well as success and survival criteria were evaluated according to Albrektsson et al. [11] and Roos et al. [12].
Implant success was calculated on the following parameters: absence of mobility, painful symptoms, or paresthesia; absence of radiolucency during radiographic evaluation and progressive marginal bone loss (Bone resorption in measurement areas not greater than 1 mm. during the first year of implant positioning, and 0.2 mm per year in subsequent years); peri-implant probing depth ≤3 mm on each peri-implant site (mesial, distal, buccal, and oral).
Implant Survivals Included —
Therapeutic implant successes; functional and asymptomatic in situ implants thought showing a peri-implant probing MBL rate that exceed the maximum limits established by the present study; functional and asymptomatic in situ implants after peri-implantitis treatment [13, 14].
Clinical mobility (due to implant overloading, implant fracture, or peri-implantitis not successfully treated) was mandatory for implant removal. Implants showing mobility were regarded as “failures.”
2.6. Statistical Analysis
The statistical life analysis was performed as described by Kalbleish and Prentice and Colton at end of June 2010 [15, 16]. Life tables were calculated on short implants supporting different types of prostheses.
All restored implants completed at least 10 years clinical examination. Cumulative survival and success rates were calculated for the entire group of 265 implants according to the criteria fixed by Albrektsson et al. [11], van Steenberghe et al. [9]. Internal survival rate for each time interval and the entire 20 years period was considered.
Life tables included the following parameters: time period (observation time); number of implants at interval start; number of early failed implants (not loaded implants); number of loaded implants; number of implants lost to follow-up as a result of patients dropout; number at risk (it represented the “harmonic mean” of the implants at the beginning of an interval and the ones remaining at the end of the same interval); number of failed implants during the interval; annual survival and success rates; cumulative survival and success rates [16, 17].
Chi-square test was performed to compare the survival and success rates of short and standard implants, respectively. Also the prognosis of implants placed in posterior segments was compared to those in anterior segments. A 95% significance level was fixed.
3. Results
No early failures were observed, thus all the positioned implants were loaded (Figures 1 and 2).
Figure 1.
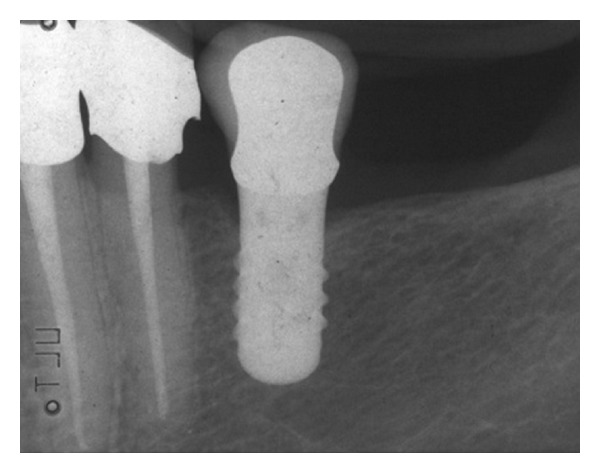
Single-tooth fixed prosthesis supported by a short implant (4.1 × 8 mm), 0 years loading. Periapical radiograph.
Figure 2.
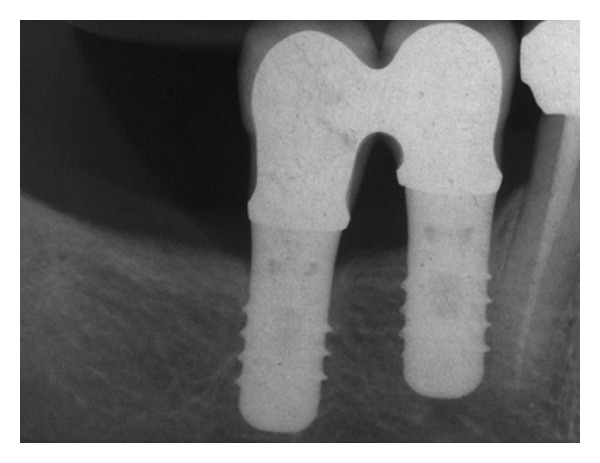
Partial fixed prosthesis supported by short implants (4.1 × 8 mm), 0 years loading. Periapical radiograph.
During the 20 years follow-up period, 4 short and 4 standard implants were found mobile due to severe peri-implantitis and therefore removed. No implant fractures occurred. Failed short and standard implants are reported in Table 4. Five of these were positioned in the maxilla and 3 in the mandible (Table 4).
Table 4.
Short and standard implants distribution: compliances and failures.
| Site | Implant size (mm) | Type of prosthesis | Cause of compliance | Cause of failure |
|---|---|---|---|---|
| 24 | 3.75 × 8 | FCD | — | Mobility due to severe peri-implantitis |
| 36 | 4.1 × 8 | FPD | — | Mobility due to severe peri-implantitis |
| 16 | 4.1 × 8 | FPD | — | Mobility due to severe peri-implantitis |
| 15 | 4.1 × 8 | FPD | — | Mobility due to severe peri-implantitis |
| 46 | 4.8 × 8 | ST | Pathologic periimplant bone resorption | — |
| 35 | 4.1 × 8 | FPD | Successfully treated periimplantitis | — |
| 24 | 4.1 × 8 | ST | Successfully treated periimplantitis | — |
| 15 | 4.1 × 8 | FPD | Successfully treated periimplantitis | — |
| 25 | 4.1 × 8 | ST | Successfully treated periimplantitis | — |
| 24 | 4.1 × 8 | FCD | Pathologic periimplant bone resorption | |
| 16 | 4.1 × 8 | ST | Pathologic periimplant bone resorption | — |
| 24 | 4.1 × 8 | FPD | Successfully treated periimplantitis | — |
| 45 | 4.1 × 8 | FPD | Pathologic periimplant bone resorption | |
| 16 | 4.8 × 10 | ST | — | Mobility due to severe peri-implantitis |
| 24 | 4.1 × 10 | FCD | — | Mobility due to severe peri-implantitis |
| 25 | 3.75 × 10 | FPD | — | Mobility due to severe peri-implantitis |
| 36 | 4.1 × 10 | FPD | — | Mobility due to severe bone resorption |
| 37 | 4.1 × 10 | FPD | Successfully treated periimplantitis | — |
| 14 | 4.1 × 10 | FPD | Pathologic periimplant bone resorption | — |
| 25 | 4.8 × 10 | FPD | Successfully treated periimplantitis | — |
| 16 | 4.1 × 10 | ST | Successfully treated periimplantitis | — |
| 46 | 4.1 × 10 | FPD | Successfully treated periimplantitis | — |
| 25 | 4.1 × 10 | FPD | Successfully treated periimplantitis | — |
| 35 | 4.1 × 10 | ST | Pathologic periimplant bone resorption | — |
| 25 | 4.1 × 10 | ST | Pathologic periimplant bone resorption | — |
| 34 | 4.1 × 10 | FPD | Pathologic periimplant bone resorption | — |
| 16 | 4.8 × 10 | FPD | Pathologic periimplant bone resorption | — |
| 44 | 4.1 × 10 | FPD | Successfully treated periimplantitis | — |
Tooth numbers: 14: maxillary right first premolar, 15: maxillary right second premolar, 16: maxillary right first molar, 24: maxillary left first premolar, 25: maxillary left second premolar, 35: mandibular right second premolar, 36: mandibular left first molar, 37: mandibular left second molar, 44: mandibular right first premolar, and 46: mandibular right first molar. ST: single tooth prosthesis, FCD: fixed complete dentures, PFD: partial fixed dentures.
Life table analyses recorded as “complications” 9 short and 11 standard implants on the whole. Peri-implant probing depth (PD) was recorded: for 4 short and 5 standard implants, respectively, it was greater than 3 mm on each peri-implant site (measurements were performed with a calibrated plastic probe). Ten peri-implantitis, respectively, for five short and 6 standard implants, were observed and successfully treated [14, 18, 19].
Mean MBL and PD values were recorded for short and standard implants at the beginning of prosthetic load and at time of last control (Table 5): at time of the last evaluation MBL mean values were 1.8 and 1.9 mm for short and standard implants, respectively. So, the authors recorded small changes of MBL and PD scores as compared to those recorded at last evaluation: this trend was noted both for short and standard implants (Figures 3 and 4). No statistically significant differences in MBL and PD values were observed between short and standard implants (P > .05) and no relationship between implant length and these parameters was observed.
Table 5.
Radiographic and clinical assessments at time of prosthetic loading and at last evaluation.
| Implants | MBL (marginal bone loss)∗ | PD (probing depth)∗ | ||||
|---|---|---|---|---|---|---|
| Loading | Last evaluation | Loading | Last evaluation | |||
| X σ | X σ | X σ | X σ | |||
| Mesial | 0.5 ± 0.4 | 1.7 ± 1.4 | Mesial | 1.8 ± 1.4 | 2.4 ± 1.1 | |
| Distal | 0.4 ± 0.6 | 1.9 ± 1.5 | Distal | 1.7 ± 1.2 | 2.4 ± 1.6 | |
| Short n = 108 |
Mean | 0.5 ± 0.5 | 1.8 ± 1.5 | Buccal | 2.1 ± 1.3 | 2.1 ± 1.5 |
| Lingual | 1.6 ± 1.3 | 2.0 ± 1.5 | ||||
| Mean | 1.8 ± 1.4 | 2.3 ± 1.4 | ||||
|
| ||||||
| Mesial | 0.2 ± 0.4 | 1.7 ± 1.5 | Mesial | 1.5 ± 1.1 | 1.8 ± 1.7 | |
| Distal | 0.3 ± 0.5 | 2.0 ± 1.1 | Distal | 1.5 ± 1.2 | 2.4 ± 1.5 | |
| Standard n = 149 | Mean | 0.3 ± 0.5 | 1.9 ± 1.6 | Buccal | 1.9 ± 1.2 | 1.6 ± 1.5 |
| Lingual | 1.3 ± 1.4 | 2.3 ± 1.4 | ||||
| Mean | 1.5 ± 1.3 | 2.1 ± 1.5 | ||||
∗Marginal bone loss and probing depth were measured in millimetres.
n: implants, X: mean, σ: standard deviation.
Figure 3.

Single-tooth fixed prosthesis supported by a short implant (4.1 × 8 mm): 12 years after loading. Periapical radiograph.
Figure 4.
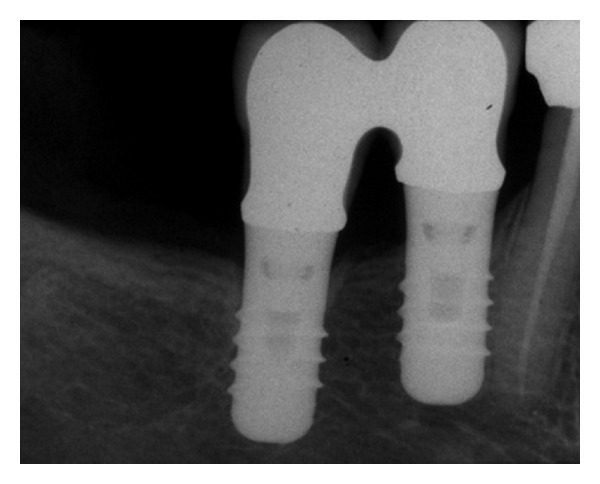
Partial fixed prosthesis supported by short implants (4.1 × 8 mm): 14 years loading. Periapical radiograph.
Moreover, no statistically different mean MBL values (P > .05) were measured for short implants placed in posterior regions (1.9 ± 1.4 mm) when compared to those of short implants placed in anterior regions (1.7 ± 1.5 mm).
Short and standard implants showed 20-years implant cumulative survival rates of 92.3% and 95.9%, respectively. Besides, the 20 years implant cumulative success rates were 78.3% and 81.4%, respectively, for short and standard implants. The difference between these rates were not significant (P > .05).
Only one short implant placed in anterior region failed after 20-years of function (Table 4), while complications were recorded for 3 and 6 short implants placed in anterior and posterior regions, respectively. Instead, the survival rate for short implants in posterior regions was comparable to that in anterior regions: 95 and 96.4%, respectively. The difference between these survival rates was not significant (P > .05).
4. Discussion
Factors involved in the survival rates seem to be independent of the implant length. These rates, for both standard and short implants, were similar. Despite the limited sample of short implants that followed similar conclusion could be drawn when short implants in posterior regions were compared to those in anterior region. Nevertheless, more researches are needed to confirm this trend since the low number of short implants followed, particularly when short implants placed in posterior region were compared to those in anterior region [20].
Jaffin and Berman [21], and Quirynen and colleagues [22] reported that implant length was directly related to failure rates. By contrast, these conclusions were not clearly observed in the clinical experience of Straumann implants [23–25]. These findings were confirmed by recent reviews on short implants [26–28]. Nevertheless, 8 mm implants were used for placement in sites with limited bone height, especially when observed in the lateral parts of the mandible and the maxilla, where the mandibular nerve and the maxillary sinus had to be avoided. Such an implant length was considered as “short,” even if today short implants are often 6 mm or even less; instead, 6 mm implants are actually not validated by a long-term prognosis in the literature yet [26–28]. Long-term clinical prospective studies on 6 mm implants adequate prognosis are needed to consider 8 mm implants as “standard.”
An obvious conclusion could be that implant design characteristics and the implant-bone interface are important factors in this respect [29, 30].
Draenert et al. in their retrospective analysis have provided, as a recommended option, the association of short and standard implants in fixed prosthetic rehabilitation constructs [31]. It is widely agreed upon that the use of short implants would be better in cases of severely atrophic mandibles and/or pneumatization of the maxillar sinus, due to the fact that if a standard implant were to be inserted it would lead to a more invasive, expensive, and complex surgery (i.e., sinus lift, bone grafting procedures) [32]. In the present report, no association of short and standard implants was included in the follow-up sample, because of the eventual influence of different implant lengths on the long-term implant function; further prospective controlled researches are needed to clarify the real benefit provided by the association of short and standard implants supporting fixed prostheses.
In contrast, as reported by literature on implant therapy, bone quality seems to affect the implants survival rates [33] and long-term prognosis [34]. The implant failures observed in the present study are more frequent in the upper back jaw, where there is a higher chance of the bone being type III-IV [35]. The outcomes seem to agree with other studies, in which implant failure rates in the upper back jaw have been shown to be statistically significant [36]. In a recent systematic paper, Sun et al. reported that most failures of short implants can be attributed to poor bone quality in the maxilla and a machined surface [27]. Although short implants in atrophied jaws can achieve similar long-term prognoses as standard dental implants with a reasonable prosthetic design according to this paper, stronger evidence is essential to confirm this finding.
Several authors confirmed these assumptions: bone quality, surgeon technique, characteristics of the implant's surface [4], width of bone-to-implant contact, parafunctions and overcontact in lateral direction [37], and primary stability [38] seem to significantly influence the prognosis of implants, particularly with reduced bone-to-implant contact, as a reduced fixture length [26].
Furthermore, the literature review by Telleman et al. highlighted how the implant failures in the studies that have excluded smokers were lower when compared to those that included this patients [39]. In the present study no heavy smokers were included in the follow-up sample, so that this possible bias was avoided.
5. Conclusions
The results of this study lead to the following conclusions.
The long-term prognosis of short implants is consistent with those reported in the literature concerning short implants.
Cumulative success and survival rates of short and standard implants were not statistically different: the high reliability of short implants is confirmed.
The prognosis of short implants in posterior regions was comparable to that in anterior regions. Nevertheless, a larger sample is required to confirm this trend.
This study obtained positive results for 8 mm long dental implants. The results of this study may indicate the reliability of short implants, although further research is required to elucidate the most appropriate implant distribution as well as the most favourable prosthetic restoration [40]. Nevertheless, more researches are needed to confirm this trend since the low number of short implants followed, particularly when short implants placed in posterior region were compared to those in anterior region.
Conflict of Interests
The authors declare that they have no conflict of interests.
Acknowledgment
The authors gratefully acknowledge the assistance of Dr. Luca Baucia, Department of Prosthodontics, Dental Clinic, School of Dentistry, University of Milan, Italy in collecting data.
References
- 1.Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. Journal of Clinical Periodontology. 2002;29(supplement 3):197–212. doi: 10.1034/j.1600-051x.29.s3.12.x. [DOI] [PubMed] [Google Scholar]
- 2.Misch CE, Steigenga J, Barboza E, Misch-Dietsh F, Cianciola LJ. Short dental implants in posterior partial edentulism: a multicenter retrospective 6-year case series study. Journal of Periodontology. 2006;77(8):1340–1347. doi: 10.1902/jop.2006.050402. [DOI] [PubMed] [Google Scholar]
- 3.Fugazzotto PA, Beagle JR, Ganeles J, Jaffin R, Vlassis J, Kumar A. Success and failure rates of 9 mm of shorter implants in the replacement of missing maxillary molars when restored with individual crowns: preliminary results 0 to 84 months in function. A retrospective study. Journal of Periodontology. 2004;75(2):327–332. doi: 10.1902/jop.2004.75.2.327. [DOI] [PubMed] [Google Scholar]
- 4.Menchero-Cantalejo E, Barona-Dorado C, Cantero-Álvarez M, Fernández-Cáliz F, Martínez-González JM. Meta-analysis on the survival of short implants. Medicina Oral, Patologia Oral y Cirugia Bucal. 2011;16(4):e546–e551. doi: 10.4317/medoral.16.e546. [DOI] [PubMed] [Google Scholar]
- 5.Rossi F, Ricci E, Marchetti C, Lang NP, Botticelli D. Early loading of single crowns supported by 6-mm-long implants with a moderately rough surface: a prospective 2-year follow-up cohort study. Clinical Oral Implants Research. 2010;21(9):937–943. doi: 10.1111/j.1600-0501.2010.01942.x. [DOI] [PubMed] [Google Scholar]
- 6.Renouard F, Nisand D. Short implants in the severely resorbed maxilla: a 2-year retrospective clinical study. Clinical Implant Dentistry and Related Research. 2005;7(1):S104–S110. doi: 10.1111/j.1708-8208.2005.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 7.Maló P, De Araújo Nobre M, Rangert B. Short implants placed one-stage in maxillae and mandibles: a retrospective clinical study with 1 to 9 years of follow-up. Clinical Implant Dentistry and Related Research. 2007;9(1):15–21. doi: 10.1111/j.1708-8208.2006.00027.x. [DOI] [PubMed] [Google Scholar]
- 8.Sánchez-Garcés MA, Costa-Berenguer X, Gay-Escoda C. Short implants: a descriptive study of 273 implants. doi: 10.1111/j.1708-8208.2010.00301.x. Clinical Implant Dentistry and Related Research. In press. [DOI] [PubMed] [Google Scholar]
- 9.van Steenberghe D, Lekholm U, Bolender C, et al. Applicability of osseointegrated oral implants in the rehabilitation of partial edentulism: a prospective multicenter study on 558 fixtures. The International Journal of Oral & Maxillofacial Implants. 1990;5(3):272–281. [PubMed] [Google Scholar]
- 10.Romeo E, Lops D, Margutti E, Ghisolfi M, Chiapasco M, Vogel G. Implant-supported fixed cantilever prostheses in partially edentulous arches. A seven-year prospective study. Clinical Oral Implants Research. 2003;14(3):303–311. doi: 10.1034/j.1600-0501.2003.120905.x. [DOI] [PubMed] [Google Scholar]
- 11.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. The International Journal of Oral & Maxillofacial Implants. 1986;1(1):11–25. [PubMed] [Google Scholar]
- 12.Roos J, Sennerby L, Lekholm U, Jemt T, Gröndahl K, Albrektsson T. a qualitative and quantitative method for evaluating implant success: a 5-year retrospective analysis of the Brånemark implant. International Journal of Oral and Maxillofacial Implants. 1997;12(4):504–514. [PubMed] [Google Scholar]
- 13.Mombelli A, Lang NP. Clinical parameters for the evaluation of dental implants. Periodontology 2000. 1994;4:81–86. doi: 10.1111/j.1600-0757.1994.tb00008.x. [DOI] [PubMed] [Google Scholar]
- 14.Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontology 2000. 1998;17(1):63–76. doi: 10.1111/j.1600-0757.1998.tb00124.x. [DOI] [PubMed] [Google Scholar]
- 15.Kalbleish JD, Prentice RL. Failure Time Data. The Statistical Analysis of Failure Time Data. 1st edition. New York, NY, USA: John Wiley & Sons; 1980. [Google Scholar]
- 16.Colton T. Calcolo delle Tabelle di Sopravvivenza. Statistica in Medicina. 1st edition. Padova, Italy: Piccin; 1988. [Google Scholar]
- 17.Barberi B. Rappresentazione Statistica delle Distribuzioni di Frequenze. Nozioni di Calcolo Statistico. 1st edition. Florence, Italy: 1962. (P. Borlingheri, editor). [Google Scholar]
- 18.Mombelli A. Prevention and therapy of peri-implant infections. Proceedings of the 3rd European Workshop on Periodontology. Implant Dentistry; 1999; Berlin, Germany. Quintessence; pp. 281–303. [Google Scholar]
- 19.Lekholm U, Ericsson I, Adell R, Slots J. The condition of the soft tissues at tooth and fixture abutments supporting fixed bridges. A microbiological and histological study. Journal of clinical periodontology. 1986;13(6):558–562. doi: 10.1111/j.1600-051x.1986.tb00847.x. [DOI] [PubMed] [Google Scholar]
- 20.Jokstad A. The evidence for endorsing the use of short dental implants remains inconclusive. Evidence-Based Dentistry. 2011;12(4):99–101. doi: 10.1038/sj.ebd.6400821. [DOI] [PubMed] [Google Scholar]
- 21.Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. Journal of Periodontology. 1991;62(1):2–4. doi: 10.1902/jop.1991.62.1.2. [DOI] [PubMed] [Google Scholar]
- 22.Quirynen M, Naert I, van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Brånemark system. Clinical oral implants research. 1992;3(3):104–111. doi: 10.1034/j.1600-0501.1992.030302.x. [DOI] [PubMed] [Google Scholar]
- 23.Szmukler-Moncler S, Bernard JP. Short implants in the posterior region. Proceedings of the Annual ITI Meeting; 1999; Swizerland. Films; [Google Scholar]
- 24.Nedir R, Bischof M, Briaux JM, Beyer S, Szmukler-Monder S, Bernard JP. A 7-year life table analysis from a prospective study on ITI implants with special emphasis on the use of short implants. Results from a private practice. Clinical Oral Implants Research. 2004;15(2):150–157. doi: 10.1111/j.1600-0501.2004.00978.x. [DOI] [PubMed] [Google Scholar]
- 25.Romeo E, Ghisolfi M, Rozza R, Chiapasco M, Lops D. Short (8-mm) dental implants in the rehabilitation of partial and complete edentulism: a 3- to 14-year longitudinal study. International Journal of Prosthodontics. 2006;19(6):586–592. [PubMed] [Google Scholar]
- 26.Carr AB. Survival of short implants is improved with greater implant length, placement in the mandible compared with the maxilla, and in nonsmokers. Journal of Evidence-Based Dental Practice. 2012;12(1):18–20. doi: 10.1016/j.jebdp.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 27.Sun HL, Huang C, Wu YR, Shi B. Failure rates of short (≤ 10 mm) dental implants and factors influencing their failure: a systematic review. The International Journal of Oral & Maxillofacial Implants. 2011;26(4):816–825. [PubMed] [Google Scholar]
- 28.Raviv E, Turcotte A, Harel-Raviv M. Short dental implants in reduced alveolar bone height. Quintessence International. 2010;41(7):575–579. [PubMed] [Google Scholar]
- 29.Wilke H, Claes L, Steinemann S. The influence of various titanium surfaces on the interface shear strenght between implant and bone. In: Heimke U, Lee A, editors. Clinical Implant Material Advances in Biomaterials. Vol. 9. Amsterdam, The Netherlands: Elsevier Science; 1990. [Google Scholar]
- 30.Buser D, Schenk RK, Steinemann S, Fiorellini JP, Fox CH, Stich H. Influence of surface characteristics on bone integration of titanium implants. A histomorphometric study in miniature pigs. Journal of Biomedical Materials Research. 1991;25(7):889–902. doi: 10.1002/jbm.820250708. [DOI] [PubMed] [Google Scholar]
- 31.Draenert FG, Sagheb K, Baumgardt K, Kämmerer PW. Retrospective analysis of survival rates and marginal bone loss on short implants in the mandible. doi: 10.1111/j.1600-0501.2011.02266.x. Clinical Oral Implants Research. In press. [DOI] [PubMed] [Google Scholar]
- 32.Etöz OA, Ulu M, Kesim B. Treatment of patient with Papillon-Lefevre syndrome with short dental implants: a case report. Implant Dentistry. 2010;19(5):394–399. doi: 10.1097/ID.0b013e3181ed0798. [DOI] [PubMed] [Google Scholar]
- 33.Morand M, Irinakis T. The challenge of implant therapy in the posterior maxilla: providing a rationale for the use of short implants. The Journal of oral implantology. 2007;33(5):257–266. doi: 10.1563/1548-1336(2007)33[257:TCOITI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 34.Annibali S, Cristalli MP, Dell'Aquila D, Bignozzi I, La Monaca G, Pilloni A. Short dental implants: a systematic review. Journal of Dental Research. 2012;91(1):25–32. doi: 10.1177/0022034511425675. [DOI] [PubMed] [Google Scholar]
- 35.Lekholm U, Zarb G. Patient selection and preparation. In: Brånemark PI, Zarb G, Albrektsson T, editors. Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. Chicago, Ill, USA: Quintessence; 1985. pp. 199–209. [Google Scholar]
- 36.Pommer B, Frantal S, Willer J, Posch M, Watzek G, Tepper G. Impact of dental implant length on early failure rates: a meta-analysis of observational studies. Journal of Clinical Periodontology. 2011;(9):856–863. doi: 10.1111/j.1600-051X.2011.01750.x. [DOI] [PubMed] [Google Scholar]
- 37.Chang SH, Lin CL, Hsue SS, Lin YS, Huang SR. Biomechanical analysis of the effects of implant diameter and bone quality in short implants placed in the atrophic posterior maxilla. Medical Engineering and Physics. 2012;34(2):153–160. doi: 10.1016/j.medengphy.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 38.Eduardo Anitua GO, Aguirre JJ, Andía I. Five-year clinical evaluation of short dental implants placed in posterior areas: a retrospective study. Journal of Periodontology. 2008;79(1):42–48. doi: 10.1902/jop.2008.070142. [DOI] [PubMed] [Google Scholar]
- 39.Telleman G, Raghoebar GM, Vissink A, Den Hartog L, Huddleston Slater JJR, Meijer HJA. A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. Journal of Clinical Periodontology. 2011;38(7):667–676. doi: 10.1111/j.1600-051X.2011.01736.x. [DOI] [PubMed] [Google Scholar]
- 40.Yi YS, Emanuel KM, Chuang SK. Short (5.0 × 5.0 mm) implant placements and restoration with integrated abutment crowns. Implant Dentistry. 2011;20(2):125–130. doi: 10.1097/ID.0b013e31820fb67e. [DOI] [PubMed] [Google Scholar]


