Abstract
We prospectively collected clinical data during the period 2001–2006 on 60 hips with symptomatic femoroacetabular impingement that had radiographic evidence of acetabular retroversion defined as a crossover sign on an adequate anteroposterior radiograph or retroversion on magnetic resonance imaging or computed tomography. Our treatment algorithm for acetabular retroversion used measurements of acetabular coverage (lateral center edge angle and the posterior wall sign) and condition of acetabular cartilage to direct treatment of acetabular retroversion. The algorithm directed the surgeon to perform a periacetabular-osteotomy (PAO) in 30 hips and in 30 hips a surgical-dislocation and osteochondroplasty (SDO) of the femoral head-neck junction and acetabular rim. HHS and Tönnis radiographic grading were collected preoperatively and at latest followup. The HHS improved from 52 to 90 in the hips treated with SDO and 72 to 91 in the hips treated with PAO, with an overall survivorship of 96% at four years. Patient follow-up averaged 46 months (range 24–75). Elimination of the crossover sign and correction of the posterior wall sign occurred in over 90% of all patients when present. The results indicate that hips with acetabular retroversion, deficient posterior and/or lateral acetabular coverage and intact hyaline cartilage can be effectively treated with acetabular reorientation while retroverted hips with anterior over-coverage but sufficient posterior coverage are effectively treated with osteochondroplasty of the acetabulum and proximal femur.
Introduction
Within the past decade, the concept of femoroacetabular impingement (FAI) as a cause of hip pain in the young adult and precursor to the development of hip osteoarthritis has been elucidated.1–7 FAI can result from abnormal femoral morphology such as cam impingement from reduced femoral head-neck offset, or from pincer impingement from abnormal acetabular morphology such as acetabular retroversion8–11 or acetabular protrusio.3,12,13
The optimum treatment for the young adult patient with symptomatic femoroacetabular impingement due predominately to acetabular retroversion remains unknown. The retroversion deformity can be associated with a volumetrically deficient or sufficient acetabulum based on the adequacy of lateral and posterior coverage. Further, deficient posterior wall coverage has been found to correlate with the progression of osteoarthritis in hips with cam impingement.1 Current surgical approaches have included both periacetabular osteotomy (PAO)14–16 and either arthroscopic femoral and acetabular osteochondroplasty17–19 or in our study’s case, open osteochondroplasty via surgical dislocation.20–24 Redirectional or anteversion producing PAO, with or without femoral head-neck osteochondroplasty, is aimed at reducing the prominence of the anterior acetabular wall and improving lateral and posterior coverage if deficient. Osteochondroplasty of the femoral head-neck junction and anterior acetabular rim is performed to reduce femoroacetabular abutment without reorientation of the acetabulum.20,23,25–28
Early clinical results of acetabular reorientation for acetabular retroversion in a limited number of patients have been encouraging.16,29–31 A comprehensive analysis of the surgical strategies utilized for treatment of acetabular retroversion, including perioperative clinical and radiographic outcomes has yet to be reported.
The objective of this study was to report pre- and postoperative radiographic features and clinical outcomes of a larger group of patients with symptomatic FAI due primarily to acetabular retroversion who were treated according to the proposed surgical algorithm. We assumed that regional acetabular coverage and condition of the acetabular cartilage should direct treatment of hips with acetabular retroversion. We hypothesized that retroverted hips treated by either arm of the algorithm, osteochondroplasty or PAO, would experience similar and satisfactory clinical results each other and to hips without retroversion treated with PAO or osteochondroplasty.
Patients and Methods
We prospectively collected clinical data during the period 2001–2006 on 54 patients (60 hips, 6 bilateral) with symptomatic FAI who had radiographic evidence of acetabular retroversion. Based on the surgical algorithm (Figure 1), thirty hips were directed to treatment with PAO and 30 hips to SDO; 25 were women (3 bilateral) and 29 men (3 bilateral). For the six patients with bilateral hip involvement, four patients had staged PAO, one patient had staged SDO, and one patient had a SDO followed by a contra-lateral PAO one year later. The average age of patients in the PAO group was 24 years old (range 15–41) and 27 years old in the SDO group (range 16–44) (p=0.21) (Table 1). The average follow-up for all patients was 46 months (range 24–84). This study was approval by our Institutional Board Review.
Figure 1.
Algorithm for treatment of femoroacetabular impingement due to acetabular retroversion.
Table 1.
Patient Demographics
| Surgery | Average Age | Gender | Height (Inches) |
Weight (Pounds) |
EBL |
|---|---|---|---|---|---|
| PAO | 24 years (15–41) | 11 M, 19 F | 66.6 | 161 | 611 cc |
| SDO | 27 years (16–44) | 21 M, 9 F | 69.3 | 176 | 265 cc |
| p-value | 0.21 | 0.025* | 0.20 | 0.23 | 0.00003* |
PAO, periacetabular osteotomy
SDO, surgical dislocation and osteochondroplasty
EBL, estimated blood loss
statistically significant difference
The diagnosis of FAI due predominantly to acetabular retroversion was multi-factorial and based upon a detailed clinical and radiographic evaluation. The clinical history for all patients was consistent with femoroacetabular impingement, including pain and functional limitations with activities such as flexion and internal rotation of the hip. A positive impingement sign32 on physical exam was present in all patients. Standard radiographic studies were performed pre and postoperatively and included a standing anteroposterior (AP) pelvis, false profile lateral and/or groin lateral radiographs which were used to detect the presence of a reduced femoral head neck offset.33 All patients demonstrated a positive crossover sign, indicative of acetabular retroversion, on preoperative anteroposterior pelvis radiographs and a subset of patients, as described below, demonstrated a positive posterior wall sign and/or deficient lateral center edge angle.1,9,10,34–37 (Figure 2)
Figure 2.
Case of acetabular retroversion with deficient posterior acetabular coverage. Patient was treated with acetabular reorientation and osteochondroplasty of the head-neck junction.
Figure 2a: Preoperative anteroposterior pelvis radiograph shows acetabular retroversion of the right hip with crossover sign and positive posterior wall sign.
Figure 2b: Postoperative anteroposterior pelvis radiograph with correction to acetabular anteversion and adequate posterior coverage demonstrated by a negative posterior wall sign.
Additional radiographic parameters that were measured preoperatively and at final follow-up included the following: acetabular index, lateral center edge angle of Wiberg9,38, anterior center edge angle9,39, acetabular angle of Sharp, lack of head-neck offset33,40, acetabular version41, crossover sign11, posterior wall sign1,42, and Tonnis grade of osteoarthritis43.
Deficient acetabular coverage was defined as a positive posterior wall sign and/or a center edge angle less than 20 degrees. A posterior wall sign was defined as positive if the posterior wall was medial and negative if even or lateral to the center of the femoral head on the anteroposterior pelvis radiograph.10 In our study, the center of the head was defined on digital radiographs with a PACS statistical circle following the normal contour of the subchondral femoral head contained within the acetabulum.
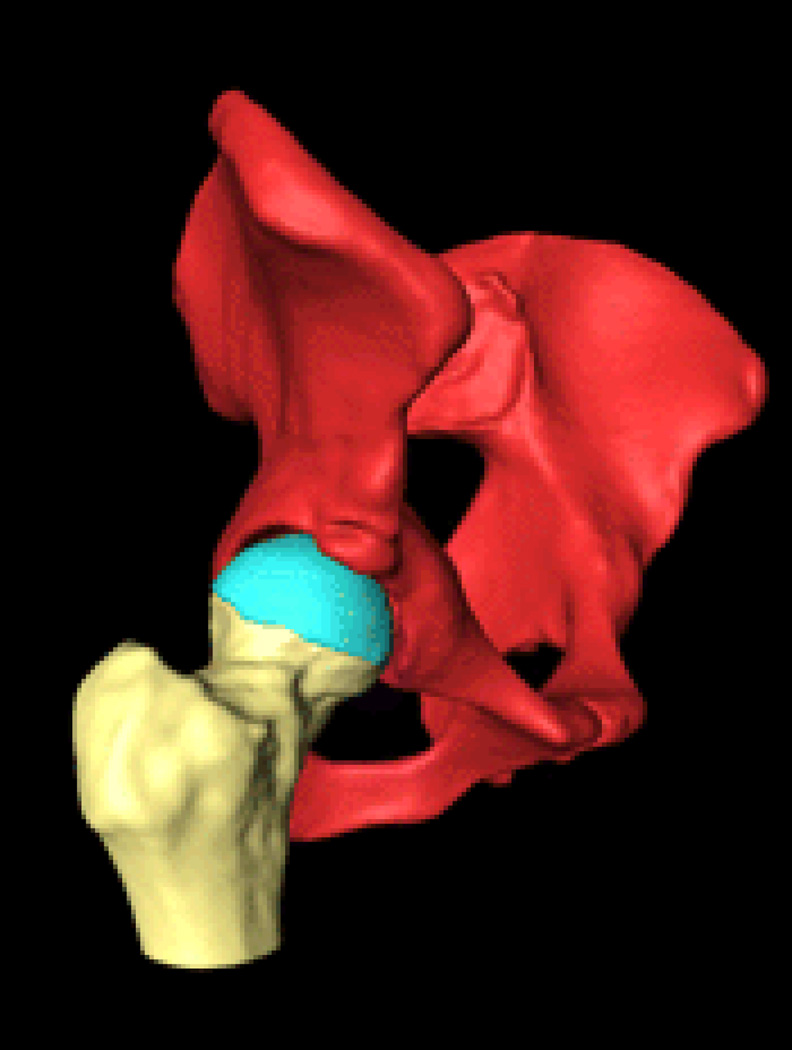
Three-dimensional reconstructions were generated from volumetric computed tomographic arthrography (CT arthrography) was utilized in select cases to further assess acetabular and proximal femoral morphology.44,45 (Figure 3)
Figure 3.
3D reconstructions created by segmenting CT-arthrography images. Anterior reconstruction (Figure 3a) and anterior oblique reconstruction (Figure 3b) clearly show acetabular over-coverage. Posterior deficiency is also noted on the posterior reconstruction (Figure 3c).
Our surgical algorithm for treatment of acetabular retroversion was as follows: Hips underwent PAO when clear lateral and/or posterior acetabular wall insufficiency was present, defined by a lateral center edge angle (LCEA) < 20 degrees and a positive posterior wall sign respectively, or SDO when the lateral and posterior acetabular coverage was sufficient (LCEA > 20 degrees and a negative posterior wall sign respectively).9,10 In addition, when damaged articular cartilage of the anterior portion of acetabular over-coverage was suspected (or confirmed using MR arthrography25) a SDO was performed to avoid rotating injured cartilage into the weight-bearing portion of the acetabulum.27,46 (Figure 1)
Periacetabular osteotomy was performed via a modified Smith-Petersen approach as described previously.16 The osteotomized acetabular fragment was reoriented into a more anteverted position by rotating the anterior aspect of the fragment medially and the posterior aspect laterally while maintaining appropriate medialization of the acetabular center. After provisional fixation, bi-plane image fluoroscopy was used to verify that the posterior wall of the acetabulum extended lateral to the center of the femoral head and the anterior wall remained medial to the center of the femoral head, with walls converging at the lateral margin of the acetabulum. Goal LCEA was 30 to 35 degrees. In all patients, an anterior capsulotomy was performed to scrutinize the acetabular labrum and screen for the presence of residual impingement, which was addressed with osteochondroplasty of the femoral head-neck junction. A typical case with pre and postoperative radiographs and 3D reconstruction from CT arthrography images is shown in Figures 2 and 3.
Surgical dislocation and osteochondroplasty of the hip was performed via a lateral hip incision and a greater trochanter flip osteotomy as described previously.24 If high grade articular cartilage damage (Outerbridge III and IV) or hyaline delamination was visualized, the labrum was detached in a bucket handle fashion from the acetabular rim, which allowed for resection of the damaged acetabular rim and refixation of the labrum to the new acetabular rim using suture anchors.23,28 Low-grade articular damage was ignored or debrided to stable substance. All femora underwent osteochondroplasty using an osteotome and high-speed rotating burr to improve femoral head-neck offset. During SDO, acetabular articular cartilage damage was graded according to Outerbridge classification, with Outerbridge grade IV being defined as severe damage or delamination of the articular cartilage.5,47 Clinical and radiographic evaluation, including Harris Hip Score (HHS) and Tönnis grading, were determined preoperatively, annually, and at final follow-up.
Data were analyzed with using commercially available software (FileMaker Pro 7.0, Santa Clara, California, and Microsoft Excel, Redmond, Washington). The Student’s t test and chi square distribution table were used to compare differences in age, and pre and postoperative HHS with significance set to p<0.05.
Results
There was a statistically significant difference in the genders between the two groups with the PAO group having a higher ratio of females to males (19:11) compared to the SDO group (9:21) (p=0.025) (Table 1).
The average Harris hip score improved from 52 to 90 (p<0.05) for the PAO group (Group 1) and improved from 72 to 91 (p<0.05) for the SDO group (Group 2). (Table 2) There was a statistically significant difference in the preoperative HHS between the two groups (p=0.0003) with the patients treated with PAO having a preoperative HHS of 52 versus 72 for the hips treated with SDO. There was no statistical difference in postoperative HHS between the two groups.
Table 2.
Preoperative and Postoperative Harris Hip Scores by group.
| Surgery | Preoperative Pain |
Preoperative Function |
Preoperative Total HHS |
Postoperative Pain |
Postoperative Function |
Postoperative Total HHS |
|---|---|---|---|---|---|---|
| PAO | 20 | 25 | 52 pts | 39 | 41 | 90 pts |
| SDO | 31 | 35 | 72 pts | 39 | 45 | 91 pts |
| P-value | 0.00009* | 0.00001* | 0.0003* | 0.72 | 0.002* | 0.65 |
statistically significant difference
SDO, surgical dislocation and osteochondroplasty
PAO, periacetabular osteotomy
HHS: Harris Hip Scores
There was one failure in the PAO group - a deep infection that required subsequent conversion to total hip arthroplasty in a patient with spastic cerebral palsy. No other major complications were noted. There was one failure in the SDO that required conversion to total hip arthroplasty due to severe articular cartilage delamination. Two patients (2 hips) in the SDO group had symptomatic hip pain with radiographic criteria indicative of iatrogenic dysplasia following acetabular rim debridement. Both patients required a subsequent PAO to improve acetabular coverage at six and twelve months postoperatively, respectively.48 These patients had satisfactory and comparable clinical and radiographic results following staged PAO to those patients treated with SDO or PAO alone.
Intraoperative findings
Osteochondroplasty of the femoral head-neck junction was performed on all SDO patients. Anterior acetabular rim debridement was performed in twenty-seven of thirty (90%), in 19 for cartilage lesions and the remaining 8 hips for over-coverage alone. Acetabular articular damage was graded as Outerbridge IV in nineteen hips (63%) at time of SDO, eleven of which had significant hyaline cartilage delamination lesions (11/30, 37%). Four additional hips had Outerbridge III cartilage damage. As is our practice, all 30 hips undergoing PAO had simultaneous anterior arthrotomy to access for labral lesions and decreased offset, and of those, 26 (87%) underwent additional femoral osteochondroplasty to improve offset.
Specific radiographic measurements of the acetabulum for both patient groups are presented in Tables 3 and 4. In the PAO group, of the 30 hips, which were preoperatively retroverted, all but one hip was corrected to anteversion following PAO (converted to total hip arthroplasty following sepsis as described above). Preoperatively, a positive posterior wall sign was present in 27/30 (90 %) hips. However, postoperatively all but 3 hips (3/27, 11%) had a negative posterior wall sign. Two hips progressed from a Tönnis grade 1 to 2.
Table 3.
Radiographic Measures of the Acetabulum
| PAO | Acetabular Index | LCEA | ACEA | AA of Sharp | ||||
|---|---|---|---|---|---|---|---|---|
| n=30 | preop | postop | preop | postop | preop | postop | preop | postop |
| average | 15 | −0.6 | 15.7 | 35.8 | 17.7 | 35.6 | 45.5 | 33.8 |
| min | 1 | −11 | −18 | 15 | −10 | 13 | 36 | 24 |
| max | 33 | 17 | 34 | 56 | 53 | 55 | 60 | 44 |
| Stddev | 9.38 | 7.6 | 12.6 | 10.2 | 18.1 | 12.1 | 5 | 4.8 |
| SDO | Acetabular Index | LCEA | ACEA | AA of Sharp | ||||
|---|---|---|---|---|---|---|---|---|
| n=30 | preop | postop | preop | postop | preop | postop | preop | postop |
| average | 5 | 6 | 28 | 26 | 31 | 29 | 39 | 41 |
| min | −6 | −5 | 3 | 9 | 6 | 13 | 29 | 36 |
| max | 21 | 23 | 41 | 42 | 47 | 46 | 49 | 50 |
| Stddev | 7 | 6 | 9 | 8 | 14 | 10 | 4 | 4 |
| p-value | 0.0005* | 0.005* | 0.0007* | 0.002* | 0.01* | 0.39 | 0.00001* | 0.00009* |
statistically significant difference
LCEA, lateral center edge angle
ACEA, anterior center edge angle
AA, acetabular angle of Sharp
SDO, surgical dislocation and osteochondroplasty
PAO, periacetabular osteotomy
Table 4.
Radiographic Evaluation of Wall Relationships, Coverage and Tönnis grade
| PAO (n=30) | SDO (n=30) | |||
|---|---|---|---|---|
| preoperative | postoperative | preoperative | postoperative | |
| Anteversion | 0 | 29 | 0 | 27 |
| Retroversion | 30 | 1 | 30 | 3 |
| Crossover sign | 30 | 1 | 30 | 3 |
| Posterior wall sign | 27 | 3 | 11 | 11 |
| Tönnis Grade 0 | 12 | 7 | 11 | 8 |
| Tönnis Grade 1 | 18 | 21 | 19 | 17 |
| Tönnis Grade 2 | 0 | 2 | 0 | 4 |
| Tönnis Grade 3 | 0 | 0 | 0 | 1 |
SDO, surgical dislocation and osteochondroplasty
PAO, periacetabular osteotomy
Preoperatively, all 30 hips in the SDO group had a crossover sign. Postoperatively, the crossover sign was absent in 90% (27/30) of the hips. One hip progressed from Tönnis grade 0 to 2 and subsequently required a total hip arthroplasty. One hip progressed from grade 1 to 3 and currently has a HHS of 90 at 5 years after surgery.
Discussion
Acetabular retroversion is present when the acetabular opening is posterior rather than anterior in the sagittal plane. Some have understood acetabular retroversion to be a volumetrically sufficient acetabulum that is malrotated while others have postulated that it results from posterior insufficiency or anterior over-coverage. We find that retroversion can be associated with regional over and under-coverage in the same hip and yield symptoms ranging from instability to impingement or both. While the understanding of the pathomorphology of acetabular retroversion is still evolving, the appropriate treatment strategy of retroversion is in even a more primordial state, ranging from rim trimming to reorientation, with limited clinical data to direct one to either.
The clinical and radiographic results of acetabular reorientation for retroverted hips have been reported in a limited number of patients. Siebenrock et al. studied 29 hips with a crossover sign, 24 of which had a posterior wall sign.49 All underwent PAO with average follow up 30 months (range 24–49) with good to excellent result in 26. Reynolds et al. described “encouraging results” in 12 patients treated with PAO but provided no detailed analysis of the preoperative and postoperative parameters that characterize retroversion such as the crossover sign and posterior wall sign.11 Our results also indicate encouraging clinical outcomes with reliable elimination of the crossover sign and correction of the posterior wall sign in over 90% of patients utilizing our proposed surgical algorithm.
It has been shown that the posterior wall sign is a significant factor found to affect the progression of osteoarthritis in hips with cam impingement and therefore was included in our treatment algorithm.1 Our treatment algorithm for hips with FAI due to acetabular retroversion with a deficient posterior wall (a volumetrically deficient acetabulum) and “intact” acetabular articular cartilage is to perform acetabular reorientation with PAO. In our experience, these patients are typically younger, female, and have radiographic acetabular criteria that are also commonly associated with hip instability in addition to the acetabular retroversion. We have shown, as have others, that acetabular retroversion may constitute up to one third of hips with acetabular dysplasia.50
Conversely, we believe hips with acetabular retroversion and normal lateral and posterior coverage may be best treated with osteochondroplasty the anterior acetabular rim and femoral head-neck junction. These hips frequently have anterior acetabular articular cartilage lesions that need to be addressed.2 These patients are more likely to be older, male, and have radiographic criteria that reflect normal volumetric acetabula with adequate acetabular coverage in addition to acetabular retroversion.
This study found statistically significant differences in radiographic measures in the subpopulations of patients with acetabular retroversion as well as recognizable demographic/clinical characteristics. First, there were statistically more female patients amongst those treated with PAO and male patients treated with SDO. Ninety percent (27/30) of hips which underwent PAO had a positive posterior wall sign (the other 10% had deficient lateral coverage) but only 37 % (11/30) of hips which underwent SDO (these hips had either suspicion or preoperative evidence on advanced imaging of acetabular cartilage lesions).
There is evidence that pincer impingement due to acetabular retroversion is associated with labral injury.2,51 However, compared to cam impingement, pincer is thought to cause less damage to the underlying acetabular articular cartilage, most often leading to lesions limited to the outermost rim.5 Nevertheless, because most impingement deformities are combinations of cam and pincer components (reported as high as 72%)5,51 the constellation of labral and cartilage lesions will likely necessitate a combination of strategies to address chondrolabral pathology.5
Our data indicates that all but three of the patients treated with SDO had sufficient resection of anterior wall to eliminate the crossover sign. In general, we have used the extent of damaged articular cartilage to direct the amount of anterior acetabular osteochondroplasty rather than intra-operative imaging directed at producing a negative crossover sign. This approach with additional femoral debridement appears to provide sufficient anterior hip clearance with infrequent production of iatrogenic hip dysplasia.27,28,32
Clinically, patients in both treatment groups experienced statistically significant improvement in the HHS and at latest followup only one patient in each group required conversion to total hip arthroplasty. Two patients treated with SDO and anterior rim trimming for the retroversion and underlying hyaline cartilage subsequently required acetabular reorientation to improve coverage but both went on to excellent clinical results. Although the reported results for PAO in this study are specific to acetabular retroversion, the overall improvement in HHS and absolute magnitude of the post-operative HHS are similar to the larger population of patients treated with PAO at our institution.16 Similarly, the clinical improvement of patients treated with SDO due to acetabular retroversion are similar to what has been previously reported.20 We believe this demonstrates that the algorithm appropriately directed these patients with symptomatic acetabular retroversion to the correct surgery based upon the condition of their acetabular cartilage and adequacy of acetabular coverage.
The current work has several limitations, foremost of which is the fact that the treatment groups were not randomized and that the surgical decision making process evolved over the time of the study. Additionally, clinical and radiographic followup was not long-term and development of osteoarthritis commonly takes several years. Our study did not include arthroscopy in the treatment algorithm. However, arthroscopic osteochondroplasty could be used as an alternative to surgical dislocation while allowing the same principles to direct surgical decision-making.
In summary, the rationale of treating FAI due predominantly to acetabular retroversion in younger, more active patients with lateral and/or posterior wall insufficiency and intact articular cartilage with PAO, and patients with evidence of normal lateral and posterior acetabular coverage and compromised articular cartilage with SDO appears sound based on the clinical and radiologic results using our proposed surgical algorithm. Nevertheless, the decision regarding the best surgical management of the patient with FAI and associated acetabular retroversion remains difficult and depends on a thorough consideration of the hip 3D morphology and the degree of articular cartilage damage. (Figure 3)
References
- 1.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91(2):162–169. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 2.Tannast M, Goricki D, Beck M, Murphy SB, Siebenrock KA. Hip damage occurs at the zone of femoroacetabular impingement. Clin Orthop Relat Res. 2008;466(2):273–280. doi: 10.1007/s11999-007-0061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip : an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chladek P, Trc T. Femoroacetabular impingement syndrome--pre-arthritis of the hip. Acta Chir Orthop Traumatol Cech. 2007;74(5):354–358. [PubMed] [Google Scholar]
- 5.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 6.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–177. [PubMed] [Google Scholar]
- 7.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 8.Banks KP, Grayson DE. Acetabular retroversion as a rare cause of chronic hip pain: recognition of the "figure-eight" sign. Skeletal Radiol. 2007;36(Suppl 1):S108–S111. doi: 10.1007/s00256-006-0150-0. [DOI] [PubMed] [Google Scholar]
- 9.Mast JW, Brunner RL, Zebrack J. Recognizing acetabular version in the radiographic presentation of hip dysplasia. Clin Orthop. 2004;(418):48–53. doi: 10.1097/00003086-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop. 2003;(417):263–269. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 11.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81(2):281–288. doi: 10.1302/0301-620x.81b2.8291. [DOI] [PubMed] [Google Scholar]
- 12.McCarthy JC, Lee JA. Arthroscopic intervention in early hip disease. Clin Orthop. 2004;429:157–162. doi: 10.1097/01.blo.0000150118.42360.1d. [DOI] [PubMed] [Google Scholar]
- 13.McBride MT, Muldoon MP, Santore RF, Trousdale RT, Wenger DR. Protrusio acetabuli: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9(2):79–88. doi: 10.5435/00124635-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop. 1988;(232):26–36. [PubMed] [Google Scholar]
- 15.Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007;89(7):1417–1423. doi: 10.2106/JBJS.F.00493. [DOI] [PubMed] [Google Scholar]
- 16.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88(9):1920–1926. doi: 10.2106/JBJS.E.00515. [DOI] [PubMed] [Google Scholar]
- 17.Wettstein M, Dienst M. Hip arthroscopy for femoroacetabular impingement. Orthopade. 2006;35(1):85–93. doi: 10.1007/s00132-005-0897-3. [DOI] [PubMed] [Google Scholar]
- 18.Guanche CA, Bare AA. Arthroscopic treatment of femoroacetabular impingement. Arthroscopy. 2006;22(1):95–106. doi: 10.1016/j.arthro.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 19.Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25(2):299–308. ix. doi: 10.1016/j.csm.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Peters CL, Schabel K, Anderson L, Erickson J. Open treatment of femoroacetabular impingement is associated with clinical improvement and low complication rate at short-term followup. Clin Orthop Relat Res. 468(2):504–510. doi: 10.1007/s11999-009-1152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res. 468(2):555–564. doi: 10.1007/s11999-009-1138-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop. 2004;(418):67–73. [PubMed] [Google Scholar]
- 23.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88(5):925–935. doi: 10.2106/JBJS.E.00290. [DOI] [PubMed] [Google Scholar]
- 24.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–1124. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 25.Kohnlein W, Ganz R, Impellizzeri FM, Leunig M. Acetabular morphology: implications for joint-preserving surgery. Clin Orthop Relat Res. 2009;467(3):682–691. doi: 10.1007/s11999-008-0682-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Philippon MJ, Schenker ML. A new method for acetabular rim trimming and labral repair. Clin Sports Med. 2006;25(2):293–297. ix. doi: 10.1016/j.csm.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 27.Anderson LA, Crofoot CD, Erickson JA, Peters CL. Staged surgical dislocation and redirectional periacetabular osteotomy: a report of five cases. J Bone Joint Surg Am. 2009;91(10):2469–2476. doi: 10.2106/JBJS.H.00066. [DOI] [PubMed] [Google Scholar]
- 28.Espinosa N, Beck M, Rothenfluh DA, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. Surgical technique. J Bone Joint Surg Am. 2007;89(Pt 1) Suppl 2:36–53. doi: 10.2106/JBJS.F.01123. [DOI] [PubMed] [Google Scholar]
- 29.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique. J Bone Joint Surg Am. 2006;88(Pt 1) Suppl 1:65–83. doi: 10.2106/JBJS.E.00887. [DOI] [PubMed] [Google Scholar]
- 30.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. 1988. Clin Orthop. 2004;(418):3–8. [PubMed] [Google Scholar]
- 31.Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239–245. [PubMed] [Google Scholar]
- 32.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults. J Bone Joint Surg Am. 2006;88(8):1735–1741. doi: 10.2106/JBJS.E.00514. [DOI] [PubMed] [Google Scholar]
- 33.Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15(7):475–481. doi: 10.1097/00005131-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Jessel RH, Zurakowski D, Zilkens C, Burstein D, Gray ML, Kim YJ. Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am. 2009;91(5):1120–1129. doi: 10.2106/JBJS.G.00144. [DOI] [PubMed] [Google Scholar]
- 35.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005;87(2):254–259. doi: 10.2106/JBJS.D.02093. [DOI] [PubMed] [Google Scholar]
- 36.Omeroglu H, Bicimoglu A, Agus H, Tumer Y. Measurement of center-edge angle in developmental dysplasia of the hip: a comparison of two methods in patients under 20 years of age. Skeletal Radiol. 2002;31(1):25–29. doi: 10.1007/s002560100402. [DOI] [PubMed] [Google Scholar]
- 37.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis : a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466(3):677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wiberg G. Studies on Dysplastic Acetabula and Congenital Subluxation of the Hip Joint with Special Reference to the Complication of Osteoarthritis. Acta Chir Scandinavica. 1953;83:1–135. [Google Scholar]
- 39.Lequesne M, de S. False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies. Rev Rhum Mal Osteoartic. 1961;28:643–652. [PubMed] [Google Scholar]
- 40.Stahelin L, Stahelin T, Jolles BM, Herzog RF. Arthroscopic offset restoration in femoroacetabular cam impingement: accuracy and early clinical outcome. Arthroscopy. 2008;24(1):51–57. e1. doi: 10.1016/j.arthro.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 41.Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91(8):1031–1036. doi: 10.1302/0301-620X.91B8.22389. [DOI] [PubMed] [Google Scholar]
- 42.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):263–269. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 43.Tonnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976;(119):39–47. [PubMed] [Google Scholar]
- 44.Peters CL, Erickson JA, Anderson L, Anderson AA, Weiss J. Hip-preserving surgery: understanding complex pathomorphology. J Bone Joint Surg Am. 2009;91(Suppl 6):42–58. doi: 10.2106/JBJS.I.00612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Anderson AE, Peters CL, Tuttle BD, Weiss JA. Subject-specific finite element model of the pelvis: development, validation and sensitivity studies. J Biomech Eng. 2005;127(3):364–373. doi: 10.1115/1.1894148. [DOI] [PubMed] [Google Scholar]
- 46.Yasunaga Y, Ikuta Y, Kanazawa T, Takahashi K, Hisatome T. The state of the articular cartilage at the time of surgery as an indication for rotational acetabular osteotomy. J Bone Joint Surg Br. 2001;83(7):1001–1004. doi: 10.1302/0301-620x.83b7.12171. [DOI] [PubMed] [Google Scholar]
- 47.Anderson LA, Peters CL, Park BB, Stoddard GJ, Erickson JA, Crim JR. Acetabular cartilage delamination in femoroacetabular impingement. Risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am. 2009;91(2):305–313. doi: 10.2106/JBJS.G.01198. [DOI] [PubMed] [Google Scholar]
- 48.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 49.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85-A(2):278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 50.Werner CM, Copeland CE, Ruckstuhl T, Stromberg J, Seifert B, Turen CH. Prevalence of acetabular dome retroversion in a mixed race adult trauma patient population. Acta Orthop Belg. 2008;74(6):766–772. [PubMed] [Google Scholar]
- 51.Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240(3):778–785. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]