Abstract
Introduction
Medical trainee interest and participation in global health programs have been growing at unprecedented rates, and the response has been increasing opportunities for medical students and residents. However, at the fellowship level, the number and types of global health training opportunities across specialties have not previously been characterized.
Methods
A cross-sectional survey was conducted between November and December 2010 among all identified global health fellowship programs in the United States. Programs were identified through review of academic and institutional websites, peer-reviewed literature, web-based search engines, and epidemiologic snowball sampling. Identified global health fellowship programs were invited through e-mail invitation and follow-up telephone calls to participate in the web-based survey questionnaire.
Results
The survey identified 80 global health fellowship programs: 31 in emergency medicine, 14 in family medicine, 11 in internal medicine, 10 in pediatrics, 8 interdisciplinary programs, 3 in surgery, and 3 in women's health. Of these, 46 of the programs (57.5%) responded to the survey. Fellowship programs were most commonly between 19 and 24 months in duration and were nearly equally divided among 2 models: (1) fellowship integrated into residency, and (2) fellowship following completion of residency. Respondents also provided information on selection criteria for fellows, fellowship training activities, and graduates' career choices. Nearly half of fellowship programs surveyed were recently established and had not graduated fellows at the time of the study.
Conclusion
Institutions across the nation have established a significant, diverse collection of global health fellowship opportunities. A public online database (www.globalhealthfellowships.org), developed from the results of this study, will serve as an ongoing resource on global health fellowships and best practices.
Editor's Note: The online version of this article contains a table (103KB, doc) of global health fellowship programs by medical specialty.
What was known
A growing number and variety of global health immersion experiences exist for medical students and residents, yet little is known about global health experiences at the fellowship level.
What is new
A cross-sectional survey identified 80 global health fellowship programs in a range of specialties, commonly 19–24 months in duration, and either integrated into residency or entered after residency education.
Limitations
Mail survey with a 50% response rate; data collected in 2010 may not represent the current state of this rapidly evolving field.
Bottom line
This first formal study of cross-specialty global health fellowships produced a website (www.globalhealthfellowships.org) as an ongoing resource for interested individuals and a source of best practices for institutions.
Introduction
There is growing interest among US medical trainees to pursue global health training opportunities. The percentage of medical students who have participated in a global health experience during medical school increased from 6% in 1984 to 31% in 2011.1–3 Similarly, residents across a range of disciplines have increasingly integrated global health electives into their clinical training.4,5
There also has been growing demand for global health training opportunities at the fellowship level.6,7 Until recently, few global health fellowship programs have existed to meet this demand. An exception is the area of international emergency medicine fellowships, which began appearing in the late 1990s.8,9 Today, global health fellowships are becoming increasingly common across medical disciplines and are now available in emergency medicine, family medicine, internal medicine, women's health, psychiatry, pediatrics, surgery, and other disciplines.
Despite anecdotal information on the growth in the number and breadth of global health fellowships, to date, there has been no study of global health fellowships that describes offerings across medical disciplines. The objective of this study was to identify and describe all global health fellowship opportunities currently available in the United States.
Methods
Survey Participants
We established an initial data set of US programs through review of institutional and academic society websites, peer-reviewed medical literature, and web-based search engines. We defined Global health fellowship as “formal training principally focused on global health that is beyond minimum residency requirements—either subsequent to or integrated with residency training.” We included programs for which level of training (residency versus fellowship) was unclear and, ultimately, excluded purely residency-level global health tracks that did not extend beyond the time of residency training. Additionally, to minimize the likelihood of overlooking programs not identified by those methods, we also used epidemiologic snowball sampling and invited each respondent to assist in identifying additional global health fellowship programs. The study was approved by the Institutional Review Board of Partners HealthCare/Massachusetts General Hospital.
Survey Instrument
Our online survey instrument consisted of up to 26 primarily closed-response questions (using skip logic) that assessed the fellowship application process, trainee characteristics, program structure and content, and trainee activities following graduation. For certain questions, such as those related to program characteristics and activities, answer choices were written a priori in closed-response categoric form.
The e-mail invitation contained a link to the online survey instrument and was e-mailed to the fellowship director or listed contact person for each program. Initial nonresponders were e-mailed reminders, and remaining nonresponders were reminded by telephone.
Data Analysis
Survey responses were analyzed by using traditional, descriptive analyses. Characteristics of fellowship training programs were described by using percentages for categoric variables and means/modes for continuous data. Data collection occurred from November to December 2010.
Results
Characteristics of Responding Programs
Our survey identified 80 global health fellowship programs in 7 specialties across the country, including 31 in emergency medicine (38.8%), 14 in family medicine (17.5%), 11 in internal medicine (13.8%), 10 in pediatrics (12.5%), 8 interdisciplinary programs (10.0%), 3 in surgery (3.8%), and 3 in women's health (3.8%) (list of programs provided as online supplemental material). Denominators vary slightly for each question result because a different number of programs responded to each question. Of these programs, 57.5% (46/80) responded to the survey, and 80.4% of them (37/46) reported having a global health fellowship according to our definition. Of the 19.6% (9/46) of respondents that did not currently have a training program meeting this definition, 22% (2/9) planned to implement a fellowship within the next 2 years.
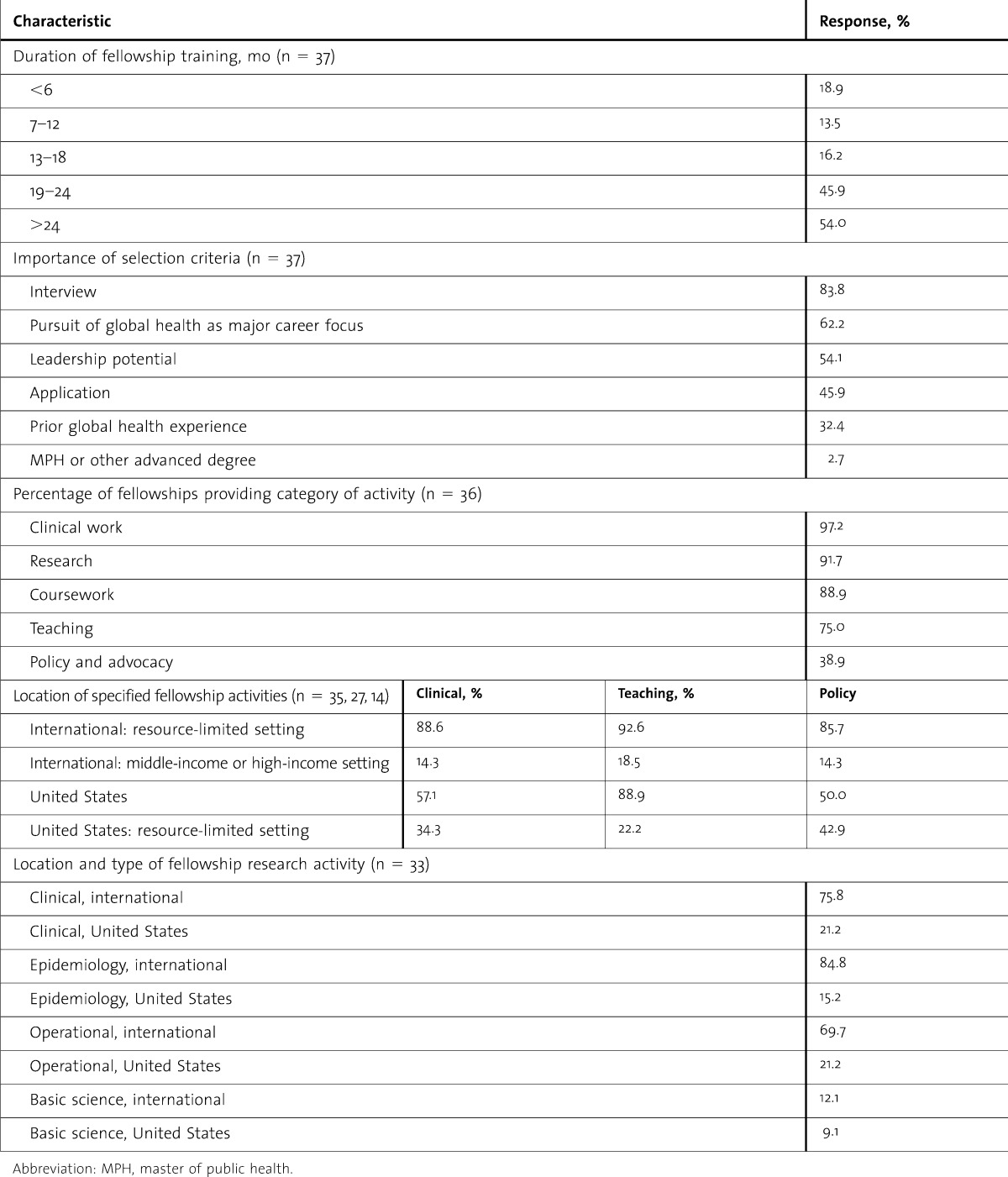
The duration of fellowship training was most commonly between 19 and 24 months (45.9%; 17/37; table), and there was nearly an even split between fellowships being integrated within residency training (52.5%; 21/40) or occurring subsequent to residency training (47.5%; 19/40). Identified programs offered between 1 and 10 positions per year (mode, 2; mean, 2.6) and graduated between 0 and 35 fellows during the past 5 years (mode, 4; mean, 3.7). Only 56.8% (21/37) of programs had already graduated fellows.
TABLE.
Characteristics of Responding Global Health Fellowship Programs
Regarding applicant eligibility, most programs required completion of an application process (89.2%; 33/37) involving an interview (83.8%, 31/37). Sixty-two percent (23/37) of programs did not require any previous global health experience. The interview and career orientation of the applicant were the most important components of selection (table).
Specific Features of Identified Fellowships
The identified programs included a variety of activities, including coursework, policy and advocacy, clinical work, research, and teaching as demonstrated in the table. In most cases (75.0%; 24/32), coursework led to a formal degree or diploma, including a master of public health or diploma in tropical medicine and hygiene. Most programs included clinical experience in resource-limited, international settings (88.6%; 31/35). Ninety-two percent (33/36) of programs offered research experience in a variety of categories and locations. Programs that included teaching responsibilities for their fellows most commonly provided such opportunities in underresourced, international settings (92.6%; 25/27) or academic, US settings (88.9%; 24/27).
Most graduates of identified programs went on to work in non–resource-limited settings within the United States, with 60.6% remaining in university academic centers. Meanwhile, 28.2% of fellowship graduates went on to work predominately in resource-limited, international settings.
Discussion
At all levels of medical training, there is increasing recognition of the unique value of global health training opportunities. Global health experiences greatly benefit trainees by exposing them to a wide spectrum of health conditions and health systems, strengthening physical examination skills, decreasing reliance on technology and laboratory resources, improving awareness of costs and resource allocation, and fostering cultural sensitivity.10–11 Global health opportunities for physicians-in-training can include international electives, global health tracks, global health curricula, and, increasingly, additional training years specifically focused on global health.
These additional years of global health training, generally termed global health fellowships, include both programs that offer traditional fellowships, entered after completion of residency, and programs that offer training integrated with residency training. The aims of global health fellowships are frequently to develop physician leaders for this growing field and to provide physicians with the unique skill sets required to most effectively improve health in resource-limited settings. This study represents a first examination, to our knowledge, of US global health fellowship training for physicians across medical disciplines.
Current global health fellowships are of significant duration, target future global health practitioners with leadership potential, and produce graduates who predominantly work in US academic medical centers after graduation. These characteristics are arguably analogous to the evolution of other subspecialty fellowships and may indicate that global health training could become recognized as a unique, accredited subspecialty.
Our primary cross-sectional survey illustrates the diversity of global health fellowship opportunities. Training is available in all major medical disciplines and involves various activities, primarily in low-resource, international and academic US settings. Global health fellows are typically cross-trained in the clinical care of individuals, the care of populations, various research methodologies, and educational pedagogy across a range of settings.
Global health fellowship training appears to be evolving quickly, with more than 40% of current fellowships yet to graduate fellows in the past 5 years. This finding is consistent with the observation that a substantial number of current fellowships have been recently established and that the total number of fellowship programs has likely doubled during the past several years. Moreover, although our study was not designed to survey institutions that will be developing fellowships in the future, a number of forthcoming programs were serendipitously identified. Given the expanding interest in global health, as reported by academic organizations such as the Consortium of Universities for Global Health and others, we fully anticipate continued growth in the number of fellowship programs in the coming years.12,13
Several responding programs had noteworthy, distinctive features, including strong emphasis on research, curriculum development, or partnership with nongovernmental organizations. Many of those programs oriented fellows toward careers outside of traditional clinical roles at US academic institutions. Although the area of policy and advocacy work remained least explored by responding programs, several programs did include formal activities in those areas in both international and US settings. The educational component of responding programs was facilitated mostly through a master of public health degree or a diploma in tropical medicine and hygiene. Aligning with an increasingly interdisciplinary definition of global health, several programs included certificate-level or master-level training in quality improvement, business management, or evaluation science as their educational component.
Our study has several limitations. First, our survey response rate was 57.5%, yet comparable to other mail surveys and more than twice the usual response rate of 25% for electronic surveys.14–17 Second, there likely were fellowship programs we did not identify. We attempted to minimize those omissions by identifying programs through examination of multiple, distinct resources and through peer-snowball sampling. Third, although the results of this survey represent a current snapshot of global health fellowship programs, we recognize that fellowship-level global health training is still changing; the number, structure, and activities of fellowship programs may continue to develop significantly as new needs and opportunities arise. The rapid rate of this development will ultimately make any static, cross-sectional report of program characteristics dated.
In recognition of, and in response to, the evolving, dynamic nature of global health fellowship training, a public, online database has been established, based in large part on the findings of this study. The Global Health Fellowship Database, available at www.globalhealthfellowships.org (figure), uses the current survey findings—as approved by the participating programs—and is augmented by other publicly available information gathered during the study. The objective of the database is to serve as an ongoing resource for trainees and educators by providing a detailed listing of current US global health fellowships and a repository for best practices across medical disciplines.
FIGURE.

Geographic Mapping of Current US Global Health Fellowship Programs From the Online Global Health Fellowship Database That Was Developed as a Result of This Study
Conclusions
Growing trainee interest in global health is driving a proliferation of training opportunities across the country. Our study characterizes global health training at the fellowship level and reveals a field with significant, diverse opportunities. Follow-up studies or the proposed online public database may track new developments in fellowship-level global health training and serve as a valuable resource for medical trainees and educators.
Footnotes
Brett D. Nelson, MD, MPH, DTM&H, is Assistant Professor of Medicine at Harvard Medical School and a Global Health Faculty Member in the Division of Global Health in Pediatrics at Massachusetts General Hospital; Rasa Izadnegahdar, MD, is a Pediatric Global Health Fellow at the Center for Global Health and Development at Boston University; Lauren Hall, MD, MSc, is a Pediatrician working in resource-limited settings with the Texas Children's Global Health Service Corps; and Patrick T. Lee, MD, directs the Global Primary Care Program at Massachusetts General Hospital, is a Clinical Instructor in Medicine at Harvard Medical School, and serves as Medical Director for Tiyatien Health in Liberia.
Funding: The authors report no external funding source for this study.
The authors are sincerely grateful to all of the fellowship directors for their time and effort in participating in this study.
References
- 1.Association of American Medical Colleges. 1984 Medical School Graduation Questionnaire: All Schools Report. Washington, DC: Association of American Medical Colleges; 1984. [Google Scholar]
- 2.Association of American Medical Colleges. 2011 Medical School Graduation Questionnaire: All Schools Report. Washington, DC: Association of American Medical Colleges; 2011. [Google Scholar]
- 3.Drain PK, Primack A, Hunt DD, Fawzi WW, Holmes KK, Gardner P. Global health in medical education: a call for more training and opportunities. Acad Med. 2007;82(3):226–230. doi: 10.1097/ACM.0b013e3180305cf9. [DOI] [PubMed] [Google Scholar]
- 4.Torjesen K, Mandalakas A, Kahn R, Duncan B. International child health electives for pediatric residents. Arch Pediatr Adolesc Med. 1999;153(12):1297–1302. doi: 10.1001/archpedi.153.12.1297. [DOI] [PubMed] [Google Scholar]
- 5.Nelson BD, Lee AC, Newby PK, Chamberlin MR, Huang CC. Global health training in pediatric residency programs. Pediatrics. 2008;122(1):28–33. doi: 10.1542/peds.2007-2178. [DOI] [PubMed] [Google Scholar]
- 6.Nelson BD, Herlihy JM, Burke TF. Proposal for fellowship training in pediatric global health. Pediatrics. 2008;121(6):1261–1262. doi: 10.1542/peds.2008-0932. [DOI] [PubMed] [Google Scholar]
- 7.Leow JJ, Kingham TP, Casey KM, Kushner AL. Global surgery: thoughts on an emerging surgical subspecialty for students and residents. J Surg Educ. 2010;67(3):143–148. doi: 10.1016/j.jsurg.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 8.VanRooyen MJ, Clem KJ, Holliman CJ, Wolfson A. B, Green G, Kirsch TD. Proposed fellowship training program in international emergency medicine. Acad Emerg Med. 1999;6(2):145–149. doi: 10.1111/j.1553-2712.1999.tb01053.x. [DOI] [PubMed] [Google Scholar]
- 9.Society for Academic Emergency Medicine. SAEM fellowship list, http://www.saem.org/saemdnn/Home/Communities/Fellows/Fellowship/tabid/78/Default.aspx. Accessed March 14, 2012. [Google Scholar]
- 10.Federico S, Zachar P, Oravec C, Mandler T, Goldson E, Brown J. A successful international child health elective: the University of Colorado Department of Pediatrics' experience. Arch Pediatr Adolesc Med. 2006;160(2):191–196. doi: 10.1001/archpedi.160.2.191. [DOI] [PubMed] [Google Scholar]
- 11.Godkin M, Savageau J. The effect of medical students' international experiences on attitudes toward serving underserved multicultural populations. Fam Med. 2003;35(3):273–278. [PubMed] [Google Scholar]
- 12.Merson MH, Page KC. The dramatic expansion of university engagement in global health: implications for U.S. policy—a report of the CSIS Global Health Policy Center, 2009, http://csis.org/publication/dramatic-expansion-university-engagement-global-health. Accessed September 1, 2011. [Google Scholar]
- 13.Consortium of Universities for Global Health. CUGH survey of university-based global health programs: a summary. http://www.cugh.org/sites/default/files/survey-summary.pdf. Updated September 2009. Accessed September 1, 2011. [Google Scholar]
- 14.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 15.Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires. Health Serv Res. 2001;35(6):1347–1355. [PMC free article] [PubMed] [Google Scholar]
- 16.Sheehan K. E-mail survey response rates: a review. J Computo-Mediated Commun. 2001;6(2) http://jcmc.indiana.edu/vol6/issue2/sheehan.html. Accessed March 14, 2012. [Google Scholar]
- 17.McMahon SR, Iwamoto M, Massoudi MS, et al. Comparison of e-mail, fax, and postal surveys of pediatricians. Pediatrics. 2003;111(4, pt 1):e299–303. doi: 10.1542/peds.111.4.e299. http://pediatrics.aappublications.org/content/111/4/e299.full.html. Accessed March 14, 2012. [DOI] [PubMed] [Google Scholar]