Abstract
Background
Atypical forms of pityriasis rosea are often noticed in Indian children.
Main observations
We describe a 9-year-old male child with predominant follicular eruptions on trunk consistent with a clinical diagnosis of pityriasis rosea.
Conclusion
Follicular pityriasis rosea is an extremely rare presentation of the disease. We propose a new classification of clinical variants of pityriasis rosea.
Keywords: atypical, child, follicular, herald plaque, pityriasis rosea
Introduction
Pityriasis rosea (PR), is characterized by the initial eruption of a herald plaque (mother patch), which is followed by generalized scaly oval eruptions typically on the trunk and proximal extremities along the Langer’s lines of cleavage, giving the characteristic "Christmas tree appearance". About 20% of the patients of PR are atypical clinical presentations.[1,2] Atypical features include atypical rash morphology, size of lesions, number of lesions, rash distribution, mucosal involvement, rash symmetry, disease duration, and severity of symptoms. In our experience, Indian children are more prone than Indian adults to present with atypical PR, atopic background being possibly facilitative.
We describe here an Indian child with atypical presentation of follicular lesions of PR on the posterior trunk.
Case Report
A 9-year-old healthy boy suffered from an episode of lowgrade fever, malaise and sore throat of eight days, during which no medical attention was sought by his parents. He presented to us one week after the remission of his respiratory symptoms with sudden eruption of a scaly, mildly pruritic plaques on his abdomen, thighs and groins [Fig. 1]. Close observation of the most initial lesion on the abdomen showed collarette scaling [Fig. 2].
Figure 1.

Scaly, mildly pruritic plaques on abdomen, thighs and groins.
Figure 2.

Close observation of the most initial lesion on the abdomen showed collarette scaling.
Five days later, the child presented with sudden onset of multiple scaly plaques on his posterior trunk. The orientations of most of the eruptions were along the Langer’s lines [Fig. 3]. Upon careful observation, we found that the morphologies were strikingly follicular, with some lesions in groups and some lesions isolated [Fig. 4]. The scaly lesions displayed annular morphology with central clearing and peripheral collarette scaling at places. Other anatomical areas including trunk, neck, face, flexures, genitalia and mucous membranes of nose, genitals and anus were uninvolved.
Figure 3.

The orientations of most of the eruptions on posterior trunk along the Langer’s lines.
Figure 4.

A close view depicting the characteristic follicular morphology of secondary eruptions on the posterior trunk.
His throat was congested, with slight enlargement of his left tonsil and congested mucous membrane. Left cervical lymphadenopathy was noted. Systemic examination revealed no abnormality otherwise.
We re-examined the history. Apart from the mother of our patient with history of atopic dermatitis, there was no history of our patient and his family members having skin diseases including dermatophyte infection and psoriasis. There was no history of asthma, urticaria, drug allergies, chronic rhinosinusitis and genital ulceration for the child and his family members.
Skin scrapings and KOH mount from the initial and subsequent lesions were negative for fungus and yeasts.
Complete blood counts, urinalysis and blood glucose level were normal. VDRL and HIV antibodies were negative. ASO titre was not elevated. Throat swab for culture revealed no growth of pathogenic bacteria. Lesional skin biopsy revealed acute spongiotic dermatitis with inflammatory mononuclear dermal infiltrates around the hair follicles and dermal blood vasculature. Exuded erythrocytes were noted in upper papillary dermis [Fig. 5].
Figure 5.
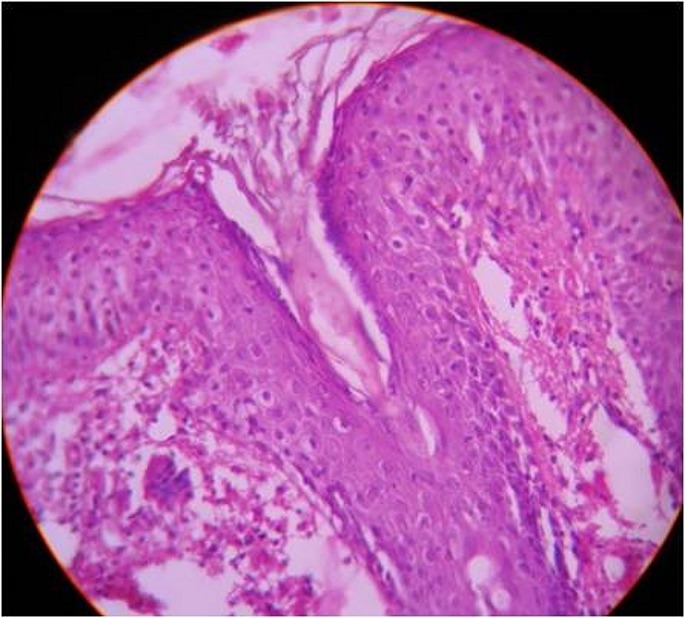
Skin biopsy revealed acute spongiotic dermatitis with inflammatory mononuclear dermal infiltrates around the hair follicles and dermal blood vasculature. Exuded erythrocytes were noted in upper papillary dermis.
We made a presumptive diagnosis of PR. We managed the patient with topical white petrolatum jelly and oral desloratidine 5 mg once daily for ten days. All the scaly lesions completely regressed in a span of two weeks, with slight post-inflammatory hypopigmentation. No recurrence was noted in next one year of follow up.
Discussion
The prodrome, clinical progress and resolution occurred in this patient in a time frame of few weeks. We believe that PR represents the most appropriate diagnostic label for this patient, fulfilling the diagnostic criteria of PR.[3] Differential diagnoses such as follicular lichen planus, keratosis pilaris, atopic dermatitis with a follicular element, dermatophytosis, psoriasis, secondary syphilis, drug eruption, erythema multiforme, acral necrolytic erythema, and erythema annulare centrifugum seem unlikely.
Follicular distribution of secondary eruptions in PR is itself a very rare presentation. One case of follicular lesions in a recent epidemiological in PR study from India has been reported.[4] However, it is unclear whether such were isolated or widespread like ours and whether the follicular lesions were seen in primary or secondary eruptions in that study.[4]
A hypothesis of viral origin in pityriasis rosea has been presented in many recent epidemiological and microbial surveys, Human Herpes virus being the most likely etiological agent.[5] It may be speculated that our patient had had a viral upper respiratory infection and may have resulted in the clinical syndrome of PR.
A 5-year-old immunosuppressed boy with spiny follicular papules on face, labeled as virally-induced trichostasis spinulosa, has been recently reported, which responded to oral gancyclovir.[6] However, we were not in a position to investigate our patient from virological perspectives. Once the lesions showed evidence of clinical regression, we considered that antiviral therapy was not warranted. It is known for herpes simplex viruses do affect pilosebaceous apparatus, presenting as viral-folliculitis.[7] In our patient, there was no clinical or laboratory evidence of active herpes simplex infection.
The occurrence of herald patch on anterior trunk, thighs and groins followed by widespread secondary eruptions on follicular location on posterior trunk are atypical features for PR in the case. We revealed the early literature describing PR, and found that follicular PR is enlisted as a variant of popular PR in one of the classifications in PR.[8] [Table 1]. However, we failed to retrieve more description of follicular PR from the early era of PR up to now.
Table 1. The early classification of pityriasis rosea.[8].
| According to rash morphology | According to rash distribution | |||
|---|---|---|---|---|
| Macular – | Punctate Guttate Nummular Circinate Pityriasis rose |
Bilateral Unilateral Generalised Localised |
||
| Urticarial – | Pityriasis rosea urticata of Vorner Urtiée pityriasis rosea of Hallopeau |
Confluent and diffuse – | Pityriasis rosea gigantean of Darier Pityriasis circiné et marginé of Vidal |
|
| Papular – | Maculopapular Follicular Miliary – Large, small |
|||
| Vesicular – | Pityriasis rosea with vesiculation | |||
Amer et al. described in his series of black American children, the natural history of pityriasis rosea quite different from that mentioned in the textbooks.[9]
This case of PR is presented here for its unique clinical features of secondary follicular eruptions on posterior trunk in a child, as a rare clinical entity. We believe that apart from the early classification, this is first formal report describing the features of follicular PR in the English literature.
Table 2. Proposed new classification of pityriasis rosea.*.
|
Axis 1 – Prodromal symptoms and herald patch Prodromal symptoms – Present (Coryza, fever, generalized muscle pain, fatigue, malaise, arthralgias, gastrointestinal symptoms), Transient/barely noticeable, Absent or unreliable history from patient. Herald patch – Absent, obscure, single, multiple, gigantic, lonely (herald plaque only as manifestation; the disease does not progress beyond the herald plaque). |
|
Axis 2 – Number and distribution of lesions Number – Few lesions (less than five, oligo-lesional), many lesions, sub-erythrodermic, erythroderma due to PR. Distribution – Relatively unilateral, absolutely unilateral, localized, regional, mucosal (mainly oral and genital), acral, PR inversus (PR mainly involving many flexures), shoulders and hips (limb-girdle PR), fewer but larger lesions localized to axillae and groins (pityriasis circinata et marginata of Vidal)**, actinic (photo-distributed), photo-spared. |
|
Axis 3 – Size, morphology, and orientation of lesions Size – Gigantic (PR gigantea of Darier) vs miniature. Morphology – Papular, papulo-squamous, papulo-vesicular, vesicular, lichenoid, urticarial, EM-like, punctuate/ purpuric/ hemorrhagic, follicular.*** Orientation – Typical i.e. along the lines of skin creases (Lines of Langer), – Atypical i.e. not along lines of skin creases: Scattered, Blaschkoid (along lines of Blaschko), Segmental (along a dermatome). |
|
Axis 4 – Symptoms and clinical course Symptoms – Severely pruritic (PR irritata), slightly pruritic, moderately pruritic Non-pruritic/asymptomatic Clinical course – Too short (less than two weeks), too long (more than six months) Recurrent PR |
|
Axis 5: Seasonal morphological variations psoriasiform in summer, crusted/haemalis form in winter |
|
* ICD-10, pityriasis rosea is coded L42X00. Pityriasis rosea due to drug is coded L44X01, signifying that PR-like rash related to
drugs is now considered a distinct condition. This classification scheme therefore excludes PR or PR-like rashes likely to be related to drugs. ** In ICD-9-CM, pityriasis circinata et maculata was listed as a synonym of PR. In ICD-10, pityriasis circinata, pityriasis circinata et marginata of Vidal, and Gibert’s disease are all listed as synonyms of PR. Some of the variants described in the literature as PR inversus might actually be PR of Vidal. *** Follicular PR is the topic of discussion in the current manuscript. |
References
- Chuh A, Zawar V, Lee A. Atypical presentations of pityriasis rosea: case presentations. J Eur Acad Dermatol Venereol. 2005;19:120–126. doi: 10.1111/j.1468-3083.2004.01105.x. [DOI] [PubMed] [Google Scholar]
- González LM, Allen R, Janniger CK, Schwartz RA. Pityriasis rosea: an important papulosquamous disorder. Int J Dermatol. 2005;44:757–764. doi: 10.1111/j.1365-4632.2005.02635.x. [DOI] [PubMed] [Google Scholar]
- Chuh AA. Diagnostic criteria for pityriasis rosea: a prospective case control study for assessment of validity. J Eur Acad Dermatol Venereol. 2003;17:101–103. doi: 10.1046/j.1468-3083.2003.00519_4.x. [DOI] [PubMed] [Google Scholar]
- Sharma L, Shrivastava K. Clinicoepidemiological study of pityriasis rosea. Ind J Dermatol Venereol Leprol. 2008;74:647–649. doi: 10.4103/0378-6323.45113. [DOI] [PubMed] [Google Scholar]
- Drago F, Broccolo F, Rebora A. Pityriasis rosea: an update with a critical appraisal of its possible herpesviral etiology. J Am Acad Dermatol. 2009;61:303–318. doi: 10.1016/j.jaad.2008.07.045. [DOI] [PubMed] [Google Scholar]
- Benoit T, Bacelieri R, Morrell DS, Metcalf J. Viral-associated trichodysplasia of immunosuppression: report of a pediatric patient with response to oral valganciclovir. Arch Dermatol. 2010;146:871–874. doi: 10.1001/archdermatol.2010.175. [DOI] [PubMed] [Google Scholar]
- Fujimoto N, Wakabayashi M, Tanaka T, Minamiguchi H, Hodohara K. Herpes folliculosebaceous ulcer in a patient with chronic lymphocytic leukaemia: an ulcerative variant of herpes folliculitis associated with herpesvirus invasion of folliculosebaceous units in immunocompromised hosts. Clin Exp Dermatol. 2010;35:447–449. doi: 10.1111/j.1365-2230.2009.03632.x. [DOI] [PubMed] [Google Scholar]
- Klauder JV. Pityriasis rosea with particular reference to its unusual manifestations. JAMA. 1924;82:178–183. [Google Scholar]
- Amer A, Fischer H, Li X. The natural history of pityriasis rosea in black American children: how correct is the "classic" description? Arch Pediatr Adolesc Med. 2007;161:503–506. doi: 10.1001/archpedi.161.5.503. [DOI] [PubMed] [Google Scholar]


