Abstract
Background
Aplasia cutis congenita (ACC) is a congenital absence of skin, and a single alopecic lesion on the scalp is the most common form.
Main observation
We present a case of ACC with tetralogy of Fallot-A. Differetial diagnosis included Adams-Oliver syndrome and nevus psiloliparus. Interestingly, our patient showed multiple ACC lesions, which were located along Blaschko’s lines.
Conclusions
As far as we know, our case is the third case of ACC with tetralogy of Fallot-A. Also, this is the first case of ACC associated with Blaschko’s lines.
Keywords: Adams-Oliver syndrome, alopecia, cardiovascular disease, hair loss, scalp
Introduction
Aplasia cutis congenita (ACC) is characterized by the absence of a portion of skin at birth, and the most common site is the scalp. Ulcerated lesions may show complete absence of all layers of the skin and then healed lesions often demonstrate flattened atrophic scar-like appearance. Since ACC usually presents as a single lesion, the occurrence of more than 3 lesions is infrequent.[1] Here, we report a case of ACC with multiple lesions located along Blaschko’s lines in a TOF patient.
Case Report
A 17-year-old boy was referred to our department for evaluation of multiple alopecic lesions from birth. He was a single birth and full-term vaginal delivery without forceps or vacuum extraction techniques. The patient was not a born of parents with consanguineous marriage. He was diagnosed with TOF, and corrective surgery was performed at 3 months of age. No contributory findings were revealed in his family history. On physical examination, there were 3 atrophic scar-like alopecic macules linearly arranged on the right temporal area, which were 5, 9, and 15 mm in size [Fig. 1]. Interestingly, the pattern of distribution was compatible with Blaschko’s lines.[2]
Figure 1.
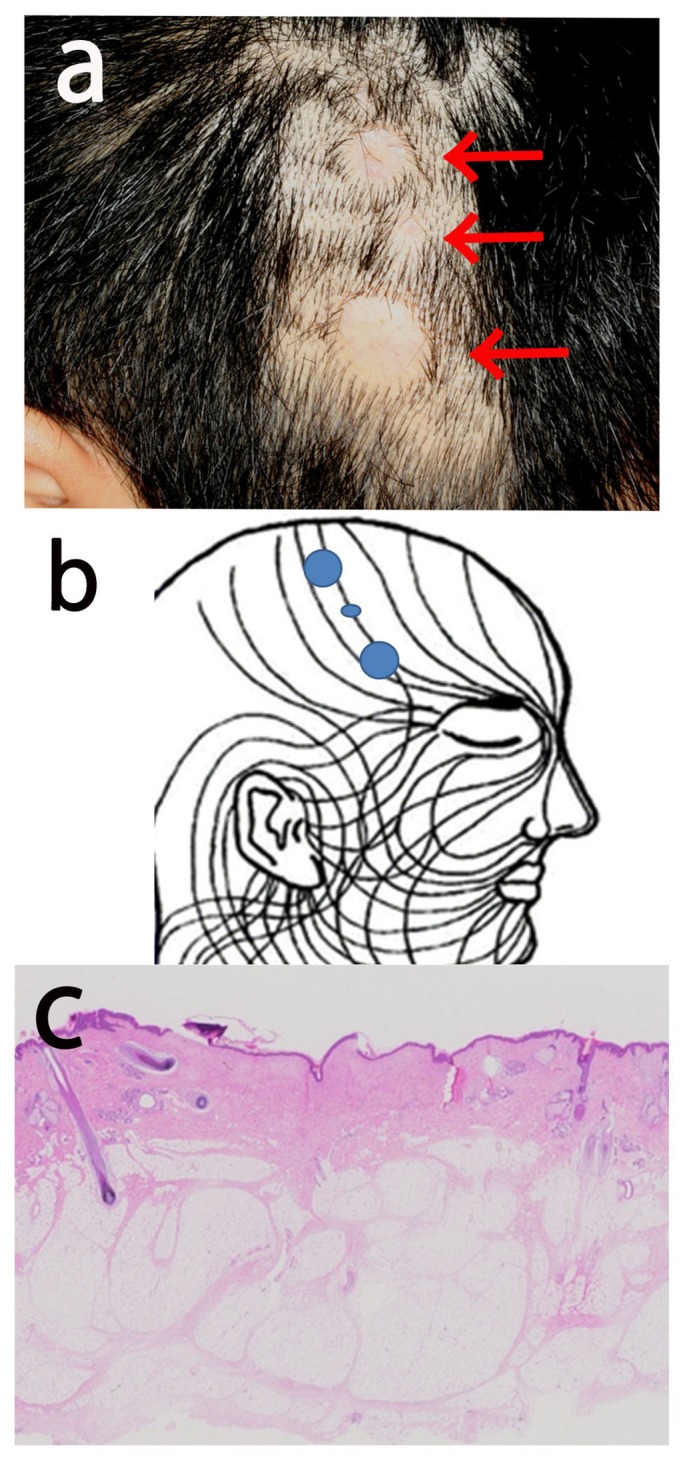
Clinical and histological features. a: There are 3 atrophic scar-like alopecic macules linearly arranged on the right temporal area (arrows). b: Distribution of skin lesions in the present case transposed onto Blaschko’s lines as proposed by Happle et al (2). c: Histological section showing atrophic scar formation, namely, thin epidermis with a reduced number of rete ridges, proliferation of collagen fibers in the dermis, and absence of hair follicles orphaned arrector pili muscles and sweat glands. Original magnification, 10x.
Ultrasound examination revealed that defect was involved epidermis and dermis but fat tissue and deeper tissue including the cranial bone was normal. There were no other abnormalities such as limb defect or neurological abnormality. From the presenting condition and clinical findings, he was diagnosed as ACC, and the 2 larger alopecic lesions were surgically excised for cosmetic reasons. Histological examination revealed atrophic scar formation, namely, thin epidermis with a reduced number of rete ridges, proliferation of collagen fibers in the dermis, and absence of hair follicles and sweat glands [Fig. 1].
Discussion
ACC is a heterogeneous group of disorders and is considered as the phenotypic result of several disease processes with multiple mechanisms.[3] ACC is complicated by various extracutaneous manifestations, and our case was associated with TOF. Although several reports describe ACC cases with congenital cardiac anomalies, only 2 cases were associated with TOF.[4] As far as we know, our case is the third case of ACC with TOF.
Adams-Oliver syndrome (AOS) is characterized by ACC, transverse limb defects, and congenital vascular and heart malformations. Mutations in the dedicator of cytokinesis 6 gene and the terminal exon of the Rho GTPase-activating protein 31 gene were found in some ACC cases.[5,6] The incidence of cardiac anomalies in AOS is about 20%. However, a recent report that described ACC with congenital cardiovascular disease but without limb defects, similar to this case, indicated the possible presence of an incomplete form of AOS which is group 2 of ACC classification by Frieden.[7,8] Mutational analysis of the causative genes may therefore provide a definite diagnosis, although our patient declined DNA analysis.
Furthermore, differential diagnosis included nevus psiloliparus.[9,10] Although we had no chance to perform MRI examinaion, we could not found neurological, skeletal or ocular abnormalities in the form of encephalocraniocutaneous lipomatosis. Also physical examinations could not show yellowish papules on the forehead or eyelids, and histological examination failed to detect presence of orphaned arrector pili muscles. Therefore, we ruled out nevus psiloliparus. However, we should note that some cases of nevus psiloliparus are associated with ACC.[10]
Interestingly, our patient showed multiple ACC lesions, which were located along Blaschko’s lines. Of all ACC cases, 70% are single lesions, 20% are double, and 8% are triple. The lines of Blaschko represent a classic pattern of cutaneous mosaicism and can be observed in a wide variety of skin disorders.[6] However, there is no report of multiple ACC lesions following Blaschko’s lines. Differential diagnosis of ACC includes focal dermal hypoplasia and dystrophic epidermolysis bullosa characterized also by skin defects. The lesions of those diseases are reported to be distributed along Blaschko’s lines. Similar mechanisms related with cutaneous mosaicisms may be involved in congenital skin defective diseases including ACC.
References
- Ingalls NW. Congenital defects of the scalp: Studies in the pathology of development. Part III. Am J Obstet Gynecol. 1933;25:861–873. [Google Scholar]
- Happle R, Assim A. The lines of Blaschko on the head and neck. J Am Acad Dermatol. 2001;44:612–615. doi: 10.1067/mjd.2001.112386. [DOI] [PubMed] [Google Scholar]
- Martinez-Regueira S, Vazquez-Lopez ME, Somoza-Rubio C, Morales-Redondo R, Gonzalez-Gay MA. Aplasia cutis congenita in a defined population from northwest Spain. Pediatr Dermatol. 2006;23:528–532. doi: 10.1111/j.1525-1470.2006.00303.x. [DOI] [PubMed] [Google Scholar]
- Yildirim SV, Kale-Cekinmez E, Ozcan D, Derbent M. Tetralogy of Fallot and hypertrophic cardiomyopathy in a case of cardiofaciocutaneous syndrome. Turk J Pediatr. 2008;50:275–277. [PubMed] [Google Scholar]
- Shaheen R, Faqeih E, Sunker A, Morsy H, Al-Sheddi T, Shamseldin HE, Adly N, Hashem M, Alkuraya FS. Recessive mutations in DOCK6, encoding the guanidine nucleotide exchange factor DOCK6, lead to abnormal actin cytoskeleton organization and Adams-Oliver syndrome. Am J Hum Genet. 2011;89:328–333. doi: 10.1016/j.ajhg.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southgate L, Machado RD, Snape KM, Primeau M, Dafou D, Ruddy DM, Branney PA, Fisher M, Lee GJ, Simpson MA, He Y, Bradshaw TY, Blaumeiser B, Winship WS, Reardon W, Maher ER, FitzPatrick DR, Wuyts W, Zenker M, Lamarche-Vane N, Trembath RC. Gain-of-function mutations of ARHGAP31, a Cdc42/Rac1 GTPase regulator, cause syndromic cutis aplasia and limb anomalies. Am J Hum Genet. 2011;88:574–585. doi: 10.1016/j.ajhg.2011.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snape KM, Ruddy D, Zenker M, Wuyts W, Whiteford M, Johnson D, Lam W, Trembath RC. The spectra of clinical phenotypes in aplasia cutis congenita and terminal transverse limb defects. Am J Med Genet A. 2009;149A:1860–1881. doi: 10.1002/ajmg.a.32708. [DOI] [PubMed] [Google Scholar]
- Frieden IJ. Aplasia cutis congenita: a clinical review and proposal for classification. J Am Acad Dermatol. 1986;14:646–660. doi: 10.1016/s0190-9622(86)70082-0. [DOI] [PubMed] [Google Scholar]
- Happle R, Küster W. Nevus psiloliparus: a distinct fatty tissue nevus. Dermatology. 1998;197:6–10. doi: 10.1159/000017968. [DOI] [PubMed] [Google Scholar]
- Torrelo A, Boente Mdel C, Nieto O, Asial R, Colmenero I, Winik B, Zambrano A, Happle R. Nevus psiloliparus and aplasia cutis: a further possible example of didymosis. Pediatr Dermatol. 2005;22:206–209. doi: 10.1111/j.1525-1470.2005.22305.x. [DOI] [PubMed] [Google Scholar]


