Women are approximately twice as likely to be diagnosed with major depressive disorder than men in the United States (U.S.) (Weissman et al. 1993). One in five American women will be diagnosed with depression over her lifetime with a mean age of onset at 28 years, during the childbearing years (Kessler et al. 1993; Weissman et al. 1993). As hormones have been shown to influence emotions and mood, certain life changes (i.e., puberty, pregnancy, menopause) can make women particularly vulnerable to the onset or return of depressive symptoms (National Institute of Mental Health [NIMH] 2008; Bennett et al. 2004). Approximately 15% of pregnant women have their initial onset of depression during pregnancy (Gaynes et al. 2005). A systematic review determined that 18.4% of pregnant women experience depression during pregnancy based on clinical interview or assessment (Gaynes et al. 2005). The authors also reported that the estimated prevalence of depression during pregnancy was 11.0%, 8.5%, and 8.5% for the first, second, and third trimesters respectively (Gaynes et al. 2005).
Depressive symptoms include sad mood, loss of interest in activities, feelings of helplessness and hopelessness, decreased energy, decision-making difficulties, sleep problems, restlessness, irritability, changes in eating patterns, suicidal ideations or attempts, and persistent physical symptoms that do not respond to treatment (NIMH 2007). When this occurs during pregnancy, the disease poses threats to the mother's health and has implications for the health of her newborn and family (Lusskin et al. 2007; Bowen and Muhajarine 2006). There is evidence of antenatal depression resulting in pregnancy and obstetric complications (Bowen and Muhajarine 2006; Larsson et al. 2004; Bennett et al. 2004), poor health behaviors (Bennett et al. 2004), and risk-taking behaviors (Bowen and Muhajarine 2006; Bennett et al. 2004). Depressed mothers-to-be are also less likely to attend regular prenatal visits (Lusskin et al. 2007; Lee and Chung 2007; Bowen and Muhajarine 2006). Maternal depression may impact the child from the fetal stage through childhood, influencing birth outcomes, mother-infant relations, development, and behavior (Lusskin et al. 2007; Bowen and Muhajarine 2006; Hammond and Crozier 2007; Brown and Solchany 2004).
The most commonly employed treatments for depression are antidepressant medication and psychotherapy though these may not be desirable among pregnant women due to concerns over side effects, stigma, time and financial costs (NIMH 2007; Hammond and Crozier 2007; Bowen and Muhajarine 2006; Daley et al. 2007). This prompts incentive to investigate other treatments for depression (Hammond and Crozier 2007). Several studies have reported on the association between physical activity and depression in non-pregnant populations, mostly finding that being physically active is associated with better mental health (Teychenne et al. 2008). Research is now focusing on the utility of physical activity as a tool to prevent and manage depression (Teychenne et al. 2008). Some studies have shown that physical activity can be as effective a treatment for depression as medication and therapy (Dunn et al. 2005; Craft and Perna 2004; Martinsen 2008).
The risks of participating in moderate intensity physical activity during pregnancy are considered low and may contribute to health benefits for both mother and fetus (Vladutiu et al. In Press; U.S. Department of Health and Human Services [DHHS] 2008; Pivarnik et al. 2006). It is recommended that pregnant women who are not regularly active or who engage in low intensity activity participate in at least 150 minutes/ week of moderate-intensity activity while women who are highly active can continue at their pre-pregnancy activity levels (U.S. DHHS 2008).
Though the role of physical activity in the development and treatment of depression has been studied extensively in general populations, research on pregnant populations is limited. To date, research on pregnant women has focused on total and recreational physical activity. In a number of studies, participation in physical activity was associated with lower levels of depressive symptoms (Pottinger et al. 2009; Orr et al. 2006; Haas et al. 2004, Da Costa et al. 2003; Koniak-Griffin 1994). However, other studies have found primarily no associations between total or recreational physical activity and depressive symptoms (Goodwin et al. 2000; Poudevigne and O'Connor 2005; Symons Downs et al. 2008). These studies have also primarily focused on cross-sectional associations between physical activity and depression, not examining potential longitudinal associations.
The objective of this investigation was to expand previous research and examine the association between overall and domain-specific moderate-to-vigorous physical activity (MVPA) and depressive symptoms during pregnancy.
Methods
Setting and population
This investigation used data from the third phase of the Pregnancy, Infection, and Nutrition Study (PIN3), a prospective cohort of pregnant women. The main objectives of the overall PIN3 Study were to investigate whether physical activity or stress are associated with preterm birth. Women were recruited between January 2001 and June 2005 from prenatal clinics at the University of North Carolina (UNC) Hospitals in Chapel Hill, NC. The Institutional Review Board of the UNC School of Medicine approved the study protocols.
Procedures
Potential participants for PIN3 were identified through medical chart reviews of new prenatal patients at the UNC Hospitals. Written informed consent was obtained from each participant. Women were asked to participate in two research clinic visits (at <20 and 24–29 weeks' gestation) in order to obtain biological samples, two telephone interviews (at 17–22 and 27–30 weeks' gestation), and two self-administered questionnaires which were given at each of the clinic visits and mailed back to study staff. Most psychosocial factors were assessed on the self-administered questionnaires. During the telephone interviews, general health, additional psychosocial measures, sociodemographic information, occupational information, physical activity, reproductive history, and health behaviors were assessed. Medical charts were abstracted after delivery to obtain information on pregnancy complications and outcomes.
Participants
The PIN3 Study recruited women who were less than or equal to 20 weeks gestation at their second prenatal visit. Women were excluded if they were younger than 16 years of age, non-English speaking, were not planning to continue care or give birth at the study site, carrying multiple gestations, or did not have a telephone to complete the phone interviews. Out of 3203 eligible participants, 2006 (63%) women were recruited. Women were allowed to participate in the PIN3 Study for more than one pregnancy. However, this analysis was restricted to the first PIN3 pregnancy, eliminating 274 pregnancies. Women were also excluded if they had no known delivery date (n=57) or no data on physical activity (n=2), depression (n=335) or both (n=117). Additionally, one woman's physical activity level was considered an outlier (≥70 hours/week of total physical activity) so her data was also excluded. This resulted in a total of 1220 participants available for analysis. When compared to the 455 women excluded for incomplete data, our sample was composed of more White (73% vs. 55%) and married (77% vs. 54%) women. The included women were also older (29 vs. 27 years), had more education (16 vs. 14 years), were better off financially (426% vs. 319% of the poverty line), and had higher parity (0.9 vs. 0.7 pregnancies). P-values for these differences were all less than 0.0001.
Physical activity assessment
Structured recall of physical activity performed during the past seven days was recorded during a telephone interview at 17–22 weeks' gestation (median gestational age= 19.4 weeks; Evenson and Wen 2010). The questionnaire was designed to assess the frequency and duration of moderate and vigorous occupational, recreational, household, child and adult care, and transportation activities. Women were asked to report the number of sessions, average duration per session, and perceived intensity level of all activities in those domains. Perceived intensity was assessed based on the Borg scale- fairly light, somewhat hard, and hard or very hard (Borg and Linderholm 1974). Self-report of activities that were “fairly light” corresponded with light activity, “somewhat hard” corresponded to moderate activity, and “hard or very hard” corresponded to vigorous activity.
Physical activity for this analysis was characterized in two ways: hours/week and metabolic equivalent (MET)-hours per week of MVPA, based on perceived and absolute intensity, respectively. Hours per week was calculated by multiplying the number of times a participant reported an activity by the number of hours she reported. MET-hours per week was calculated by multiplying the number of times the participant reported the activity by the number of hours it is reported and then multiplying by the MET value for the activity. The activities were coded based on compendium-established intensities (Pregnancy, Infection, and Nutrition Study 2007; Ainsworth et al. 2000; Ainsworth et al. 1993). Following standards for 20 to 39 year old adults, MET values of 4.8–7.1 were classified as moderate intensity and values of 7.2+ were classified as vigorous activity (Pollock et al. 1998). The exposures of interest for this analysis were total and all domain-specific physical activity measures that were of moderate-to-vigorous intensity at 17–22 weeks' gestation.
We additionally examined if meeting physical activity recommendations was associated with depressive symptoms. We used physical activity recommendations that were in place while these women were pregnant as this corresponds to how women would have been counseled about physical activity. The variable was a comprehensive meets recommendation variable of (1) the moderate intensity recommendation from Centers for Disease Control and Prevention (CDC) and the American College of Sports Medicine (ACSM) of at least 30 minutes on most, preferably all, days of the week (U.S. DHHS 1996; Pate et al. 1995) and (2) the vigorous intensity recommendation from ACSM of 20–60 minutes of activity 3 or more days/week (Pollock et al. 1998). This variable was based on participants' total perceived physical activity.
Evidence for validity and reliability of the physical activity questionnaire was assessed among a sample of pregnant women (Evenson and Wen 2010). To assess concurrent-related validity, 177 pregnant women were asked to wear an accelerometer and keep a physical activity diary for a week. These levels were compared to values reported during a telephone-administered physical activity questionnaire conducted at the end of the week. The questionnaire and structured diary were moderately to substantially correlated (Spearman correlation coefficients ranged from 0.47 to 0.69) for measures of moderate or vigorous physical activity using either perceived or absolute intensity. Spearman correlation coefficients comparing accelerometer physical activity levels with questionnaire-reported MVPA ranged from 0.12 to 0.23 for absolute intensity (MET-hours/week) and 0.28 to 0.34 using perceived intensity (hours/week). For the test-retest reliability analysis, 109 pregnant women participating in the PIN3 Study repeated their physical activity recall within 48 hours of initial assessment. In general, the assessments had moderate to near perfect agreement. The intraclass correlation coefficient was 0.84 (95% CI 0.77–0.89) for perceived MVPA and 0.84 (95% CI 0.78–0.89) for absolute MVPA.
Depression assessment
The Center for Epidemiological Studies-Depression (CES-D) Scale (Radloff 1977) was used to assess depression during pregnancy at <20 and 24–29 weeks' gestation. The scale measures depressive symptoms, particularly depressed mood in the general population; however, the results of the scale can not be used to make a diagnosis of depression. The CES-D is a 20-item, structured self-administered questionnaire. Each response was given a score of 0 to 3. A composite score is calculated summing responses and the score ranges from 0 to 60. A variety of cutoff scores have shown associations with a clinical diagnosis of depression, with a score of 16+ suggested as an appropriate positive screen for depression (Gaynes et al. 2005; Radloff 1977; Weissman 1977). In this analysis, a cutoff of 17 was used as CES-D scores for pregnant women may be higher due to overlap between depressive and pregnancy symptoms (Hoffman and Hatch 2000; Orr and Miller 1995; Klein and Essex 1994/1995). The outcome of interest was depressive symptoms at 24 –29 weeks' gestation. Depressive symptoms at < 20 weeks (median gestational age= 16.7 weeks) was included as a covariate.
Covariates
Factors previously found to be associated with both physical activity and depression in previous research and factors adjusted for in previous analyses were considered potential confounders. This includes sociodemographic variables such as age (≤ 24, 25–29, 30–34, and 35+ years), race (White, Black, or other), and marital status (married or unmarried). Indicators of socioeconomic status included were: education (≤12, 13–15, 16, and 17+), employment status at time of first phone interview (yes, no), and poverty status (≤185% or >185% of the poverty line). Poverty status considers an individual's income and the number of adults and children that live in the home (Proctor and Dalaker 2002). The value of 100 is equivalent to being at the poverty line. The 185% cut point is used as it is the Women, Infants, and Children income guideline cut point (U.S. Department of Agriculture 2009). Health indicators included were: parity (0, 1, and 2+), pre-pregnancy body mass index (Institute of Medicine 1990 categories: <19.8, 19.8–26, >26–29, and >29 kg/m2) based on pre-pregnancy height and weight reported at recruitment, smoking status for first six months of pregnancy (any smoking or nonsmoker), general health status (poor/fair, good, and very good/excellent), vaginal bleeding (any or none), and gestational diabetes (indicated in medical chart or not).
Psychosocial factors include number of negative life events and social support. Life events were assessed in the first telephone interview with the Life Experiences Survey (LES) which examines both acute and chronic life stresses (Sarason et al. 1978). It provides a composite score of life events and the impact of those events. Women are asked if events occurred since the start of pregnancy and, if so, they are asked to report the impact of each item as having a positive (+1 to +3), negative (−1 to −3), or no impact (0). The LES was modified by eliminating the item asking whether the respondent experienced a pregnancy, and combining husband and boyfriend (details of marital status, cohabitation, and relation with the father of the baby are obtained elsewhere), resulting in 39 items from the original 57 in the LES. The composite score of the impact of negative events was examined as a covariate and was categorized as 0− <1, 1−<4, and 4+. Social support was assessed during the first self-administered questionnaire with the Medical Outcomes Study Social Support Scale which assesses the availability of perceived social support in four categories (Sherbourne and Stewart 1991). It uses a five-category Likert response for 19 items. The overall score was used as a covariate and was categorized as 0− <78, 78− <89, and 89+.
Data analysis
Analysis was performed using version 9.1 of the SAS statistical software (SAS Institute Inc, Cary, NC). Univariate analysis was conducted to describe sample characteristics of potential covariates and physical activity. A covariate was considered a confounder in this analysis if it was associated with both physical activity and depressive symptoms (using Chi-square analysis) and changed the estimate of the physical activity-depressive symptoms association by ≥10% in the modeling stage using backwards deletion (Rothman and Greenland 1998). This was performed separately by physical activity domain and for the meeting physical activity recommendations variable. It was determined a priori that depressive symptoms at <20 weeks would be included as a covariate in all adjusted models, as previous history of depression is one of the most significant predictors of later depression (Brown and Solchany 2004; Lusskin et al. 2007; Bowen and Muhajarine 2006) and is expected to be associated with physical activity given previous literature. However, estimates for the final adjusted models without adjustment for depressive symptoms at <20 weeks are also presented for comparison. When no estimates are given, the only variable adjusted for in the final model depressive symptoms at <20 weeks. For each domain-specific model, additional adjustment for other MVPA was also performed to assess potential confounding.
Logistic regression modeling was utilized to calculate odds ratios (OR) and 95% confidence intervals (CI). Regression models were restricted to participants that had complete data for exposure, outcome, and the covariates of interest that were determined to be potential confounders (n=1077). Depressive symptoms were considered high if the CES-D score was at or above 17; otherwise, it was considered low. Physical activity was modeled as a three-level variable: none (reference), ≤ the median of non-zero values, and > the median of non-zero values. Estimates of the ORs were collapsed for adult and child care activity measured in METS-hours/week due to the precision and because the estimates and the 95% CIs were the same. Logistic B-spline regression analysis (Gregory et al. 2008) was conducted to explore if other forms of the physical activity variables would be informative in describing the association between total physical activity and depressive symptoms, but it did not contribute over and above the logistic model so the results were not presented.
Results
Sample characteristics
Among the 1220 PIN3 participants with physical activity and depressive symptoms data, 26% of the women were classified as having elevated depressive symptoms at 24–29 weeks' gestation. CES-D scores ranged from 0 to 55 with a median value of 10 and an interquartile range (IQR) of 5–17. Table 1 presents selected sample characteristics overall and by depressive symptoms status. The majority of the women were Whites (73%). Approximately one-third (34%) of the women belonged to the age group 30–34 years and 31% were of the age 25–29 years. Over three-quarters (77%) of the participants were married. The sample of women was highly educated, with 63% of the women completing at least 16 years of education. A low proportion of low income women were enrolled in this study sample; 19% of the women met the WIC income eligibility criteria. Most of the women, 53%, were within the normal range of BMI before becoming pregnant. Women with elevated depressive symptoms were younger, had less education, were poorer, and were more likely to be non-White, unmarried, and multiparous than women with non-elevated depressive symptoms.
Table 1.
Selected characteristics of women enrolled in the third phase of the Pregnancy, Infection, and Nutrition Study with non-missing values for physical activity at 17–22 weeks' gestation and depression at 24–29 weeks' gestation overall and by depressive symptoms status (<17 score on the Center for Epidemiological Studies-Depress ion [CES-D] scale versus ≥ 17 score on the CES-D) (n=1220).
| CES-D | ||||
|---|---|---|---|---|
| Total (n=1220) | <17 (n=904) | ≥17 (n=316) | ||
| n (%) | n (%) | n (%) | χ2 (p-value) | |
| Age (years) | 34.27 (<.0001) | |||
| ≤24 | 241 (20) | 143 (16) | 98 (31) | |
| 25–29 | 373 (31) | 289 (32) | 84 (27) | |
| 30–34 | 416 (34) | 323 (36) | 93 (29) | |
| 35+ | 190 (16) | 149 (16) | 41 (13) | |
| Race a | 11.47 (.0029) | |||
| White | 895 (73) | 686 (76) | 209 (66) | |
| Black | 202 (17) | 134 (15) | 68 (22) | |
| Other | 122 (10) | 83 (9) | 39 (12) | |
| Marital status | 58.27 (<.0001) | |||
| Married | 945 (77) | 749 (83) | 196 (62) | |
| Single | 231 (19) | 131 (14) | 100 (32) | |
| Widowed, Divorced, Separated | 44 (4) | 24 (3) | 20 (6) | |
| Education (years) | 103.79 (<.0001) | |||
| ≤12 | 225 (18) | 117 (13) | 108 (34) | |
| 13–15 | 228 (19) | 148 (16) | 80 (25) | |
| 16 | 361 (30) | 291 (32) | 70 (22) | |
| 17+ | 406 (33) | 348 (39) | 58 (18) | |
| Working at time of first phone interview | 13.77 (.0002) | |||
| Yes | 381 (31) | 256 (28) | 125 (40) | |
| No | 839 (69) | 648 (72) | 191 (60) | |
| Income (percent of the poverty line) b | 44.34 (<.0001) | |||
| ≤185 | 222 (19) | 127 (14) | 95 (32) | |
| >185 | 952 (81) | 750 (86) | 202 (68) | |
| Parity | 14.20 (.0008) | |||
| 0 | 678 (56) | 524 (58) | 154 (49) | |
| 1 | 361 (30) | 265 (29) | 96 (30) | |
| 2+ | 181 (15) | 115 (13) | 66 (21) | |
| Pre-pregnancy body mass index (kg/m2) c | 28.92 (<.0001) | |||
| <19.8 | 169 (14) | 139 (16) | 30 (10) | |
| 19.8–26 | 642 (53) | 497 (56) | 145 (46) | |
| >26–29 | 126 (10) | 89 (10) | 37 (12) | |
| >29 | 270 (22) | 169 (19) | 101 (32) | |
| Smoked at least once in first 6 mo | 58.02 (<.0001) | |||
| pregnancy d | ||||
| Yes | 126 (11) | 59 (7) | 67 (22) | |
| No | 1052 (89) | 821 (93) | 231 (78) | |
Missing data on 1 woman
Missing data on 46 women
Missing data on 13 women
Missing data on 42 women
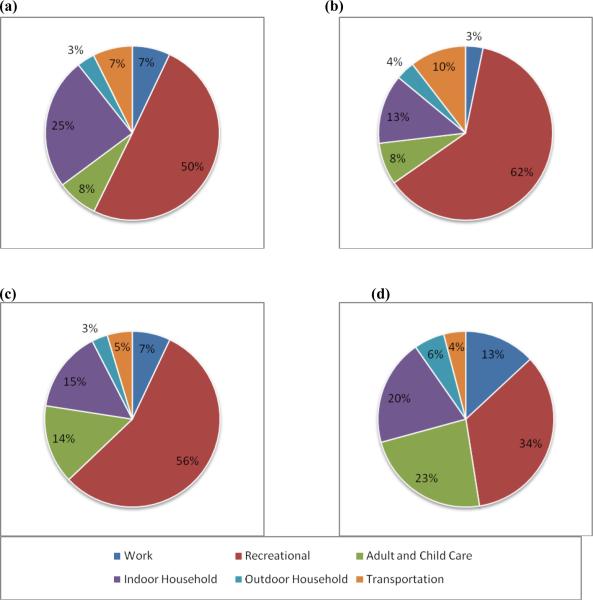
Participation in MVPA was examined descriptively among the women in the study sample who had complete data on the physical activity measures and depressive symptoms (n=1220). A total of 409 (33.5%) women participated in no perceived, self-reported MVPA in hours/week. Median activity levels were 1.17 hours/week with IQR of 0–3.5. The highest proportion of women reported participating in moderate-to-vigorous recreational activity; 43.2% of women participated in recreational activity of perceived moderate-to-vigorous intensity. Women were least likely to participate in outdoor household activity (6%). Figure 1 presents the distribution of domain-specific activities by quartile of total MVPA in hours/week. For women with the highest levels of MVPA, recreational activity comprised the lowest proportion of their total activity as compared to women in other quartiles.
FIGURE 1.
Percentages of domain-specific moderate-to-vigorous physical activity (MVPA) in hours/week at 17–22 weeks gestation by quartile of total MVPA among women enrolled in the third phase of the Pregnancy, Infection, and Nutrition Study with any MVPA. (a) 1st quartile n=203, range 0.03–1.17 (b) 2nd quartile n=202, range 1.23–2.53 (c) 3rd quartile n=206, range 2.57–5 (d) 4th quartile n=200, range 5.07–63.
Focusing on absolute intensity in MET-hours/week, 742 (60.8%) of the women participated in MVPA; median activity levels and IQR values were all 0. Women were most likely to participate in recreational activity (23.7%) and least likely to participate in adult and child care activity (3%) when assessed in absolute intensity. All women were considered as having no transportation MVPA when using MET-hours/week because walking and biking for transportation have MET values of 4, below the threshold of 4.8 for moderate activity.
Differences in physical activity participation by depressive symptoms status were found. Women with elevated depressive symptoms were more physically active than women with low depressive symptoms overall (p=0.0049) when using perceived intensity values. For women with low depressive symptoms, median (IQR) total activity level was 1 (0–3.15) hour/week. Meanwhile, for women with high depressive symptoms, median total activity level was 1.5 (0–5) hours/week. Though median values for all domain-specific activities for both groups of women were 0, Wilcoxon Rank Sum tests found that women with elevated depressive symptoms also participated in more work (p=0.02), adult and child care (p<0.0001), and indoor household (p<0.0001) MVPA. Median (IQR) of total MVPA using absolute intensity values was 0 (0–6.17) MET-hours/week for women with low depressive symptoms and 0 (0–4) MET-hours/week (p=0.04). Though median values for all domain-specific activities for both groups of women were 0, Wilcoxon Rank Sum tests found that women with elevated depressive symptoms participated in less recreational MVPA (p=0.0002).
Physical activity associations with depressive symptoms
Crude and adjusted models for the associations between perceived MVPA (hours/week) and depressive symptoms are shown in Table 2. Significant associations between total MVPA and depressive symptoms were found in both the crude and adjusted models. In the final model, women who participated in above zero and ≤2.67 total MVPA had a reduced odds of depressive symptoms as compared to inactive women (OR=0.56, 95% CI=0.38, 0.83). There was also a reduction in the odds for women participating in higher levels of total MVPA. There were slight increases in the odds of having elevated depressive symptoms for those active at work as compared to women with no work MVPA. After adjustment, women who participated in any activity but ≤ 2.25 hours/week of adult and child care activity had 1.84 times the odds of elevated depressive symptoms than those who did not (95% CI=1.08, 3.11). Those participating in more adult and child care MVPA also had increased odds, though the association was non-significant. Women who spent more than 1 hour/week in indoor household MVPA had 1.63 times the odds of high depressive symptoms than women with indoor household MVPA (0.98, 2.70). In contrast, women with any but less than 2.25 hours/week of indoor household MVPA had somewhat lower odds. There were no associations between outdoor household or transportation activity and depressive symptoms for crude and adjusted models. When comparing the final adjusted models to models unadjusted for depressive symptoms at <20 weeks gestation, depressive symptoms was found to be a confounder for all associations.
Table 2.
Odds ratios (OR) and 95% confidence intervals (CI) from logistic regression analysis of the association between total and domain-specific moderate-to-vigorous physical activity (MVPA) of somewhat hard and hard/very hard perceived intensity (hours/week) at 17–22 weeks' gestation and depressive symptoms at 24–29 weeks' gestation among women enrolled in the PIN3 Study (n=1077).
| Crude Model |
Final Adjusted Model |
Reduced Modelf |
|||||
|---|---|---|---|---|---|---|---|
| n (%) | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Total MVPA (hrs/wk)a | |||||||
| 0 | 356 (33.1) | 1.00 | -- | 1.00 | -- | -- | -- |
| ≤2.67 | 370 (34.4) | 0.52 | 0.37, 0.73 | 0.56 | 0.38, 0.83 | -- | -- |
| >2.67 | 351 (32.6) | 0.63 | 0.45, 0.88 | 0.73 | 0.50, 1.07 | -- | -- |
| Work MVPA (hrs/wk)b | |||||||
| 0 | 967 (89.8) | 1.00 | -- | 1.00 | -- | 1.00 | -- |
| ≤1.49 | 60 (5.6) | 1.37 | 0.77, 2.42 | 1.47 | 0.76, 2.84 | 1.43 | 0.79, 2.57 |
| >1.49 | 50 (4.6) | 1.95 | 1.08, 3.52 | 1.38 | 0.68, 2.78 | 1.71 | 0.93, 3.14 |
| Recreational MVPA (hrs/wk)c | |||||||
| 0 | 598 (55.5) | 1.00 | -- | 1.00 | -- | 1.00 | -- |
| ≤2 | 271 (25.2) | 0.72 | 0.51, 1.02 | 0.93 | 0.62, 1.38 | 0.81 | 0.56, 1.15 |
| >2 | 208 (19.3) | 0.94 | 0.66, 1.35 | 1.29 | 0.85, 1.98 | 1.07 | 0.74, 1.56 |
| Adult and Child Care MVPA (hrs/wk)d | |||||||
| 0 | 914 (84.9) | 1.00 | -- | 1.00 | -- | 1.00 | -- |
| ≤2.25 | 90 (8.4) | 3.05 | 1.95, 4.75 | 1.84 | 1.08, 3.11 | 2.61 | 1.65, 4.12 |
| >2.25 | 73 (6.8) | 2.54 | 1.55, 4.16 | 1.46 | 0.81, 2.61 | 2.47 | 1.48, 4.10 |
| Indoor Household MVPA (hrs/wk)e | |||||||
| 0 | 843 (78.3) | 1.00 | -- | 1.00 | -- | 1.00 | -- |
| ≤1 | 128 (11.9) | 1.15 | 0.74, 1.76 | 0.77 | 0.46, 1.28 | 0.91 | 0.57, 1.43 |
| >1 | 106 (9.8) | 2.64 | 1.74, 4.00 | 1.63 | 0.98, 2.70 | 2.00 | 1.28, 3.12 |
| Outdoor Household MVPA (hrs/wk)a | |||||||
| 0 | 1009 (93.7) | 1.00 | -- | 1.00 | -- | -- | -- |
| ≤1.5 | 42 (3.9) | 0.95 | 0.46, 1.97 | 0.65 | 0.28, 1.49 | -- | -- |
| >1.5 | 26 (2.4) | 1.62 | 0.71, 3.67 | 2.08 | 0.83, 5.24 | -- | -- |
| Transportation MVPA (hrs/wk)a | |||||||
| 0 | 979 (90.9) | 1.00 | -- | 1.00 | -- | -- | -- |
| ≤0.97 | 46 (4.3) | 1.48 | 0.79, 2.79 | 1.19 | 0.57, 2.50 | -- | -- |
| >0.97 | 52 (4.8) | 0.92 | 0.47, 1.78 | 0.76 | 0.35, 1.62 | -- | -- |
Final adjusted model adjusted for depressive symptoms at <20 weeks' gestation.
Final adjusted model adjusted for depressive symptoms at <20 weeks' gestation and social support.
Final adjusted model adjusted for depressive symptoms at <20 weeks' gestation, social support, body mass index, smoking.
Final adjusted model adjusted for depressive symptoms at <20 weeks' gestation, negative life events.
Final adjusted model adjusted for depressive symptoms at <20 weeks' gestation, social support, negative life events, smoking.
Reduced models are not adjusted for depressive symptoms at <20 weeks' gestation.
Crude and adjusted models for the association between absolute MVPA (MET-hours/week) and depressive symptoms associations are presented in Table 3. In the adjusted model, women with >9 MET-hours/week of total MVPA were 31% less likely to have elevated depressive symptoms than those with less activity (OR=0.69, 95% CI=0.46, 1.06); this was in the opposite direction from the crude model. Women with any but less than 9 MET-hours/week of total MVPA also had lower odds. There was no association between work MVPA, recreational MVPA, and outdoor household MVPA with depressive symptoms in adjusted models. The association between adult and child care activity showed a larger inverse association when adjusted as compared to the crude model, but it was still non-significant and precision was poorer. Participation in more than 6 MET-hours/week of indoor household MVPA was significantly associated with depressive symptoms in the adjusted model (OR=3.00, 95% CI=1.34, 6.72) while women with any but less than 6 MET-hours/week of indoor household MVPA had 14% lower odds of having elevated depressive symptoms (OR=0.86, 95% CI=0.38, 1.94). There was no association between outdoor physical activity and depressive symptoms in either the crude or adjusted models. When comparing the final adjusted models to models unadjusted for depressive symptoms at <20 weeks gestation, depressive symptoms was found to be a confounder for all associations except indoor household MVPA.
Table 3.
Odds ratios (OR) and 95% confidence intervals (CI) from logistic regression analysis of the association between total and domain-specific physical activity of absolute moderate and vigorous intensity (MET-hours/week) at 17–22 weeks' gestation and depressive symptoms at 24–29 weeks' gestation among women enrolled in the PIN3 Study (n=1077).
| Crude Model |
Final Adjusted Model |
Reduced Modeld |
|||||
|---|---|---|---|---|---|---|---|
| n (%) | OR | 95%CI | OR | 95% CI | OR | 95% CI | |
| Total MVPA (MET-hrs/wk)a | |||||||
| 0 | 640 (59.4) | 1.00 | -- | 1.00 | -- | 1.00 | -- |
| ≤9 | 224 (20.8) | 0.76 | 0.48, 1.19 | 0.71 | 0.42, 1.18 | 0.78 | 0.49, 1.24 |
| >9 | 213 (19.8) | 1.14 | 0.80, 1.63 | 0.69 | 0.46, 1.06 | 0.78 | 0.53, 1.15 |
| Work MVPA (MET-hrs/wk)a | |||||||
| 0 | 991 (92.0) | 1.00 | -- | 1.00 | -- | 1.00 | -- |
| ≤4 | 48 (4.5) | 0.51 | 0.23, 1.15 | 0.65 | 0.26, 1.63 | 0.64 | 0.28, 1.48 |
| >4 | 38 (3.5) | 1.38 | 0.68, 2.77 | 1.76 | 0.79, 3.90 | 1.60 | 0.78, 3.29 |
| Recreational MVPA (MET-hrs/wk)a | |||||||
| 0 | 808 (75.0) | 1.00 | -- | 1.00 | -- | 1.00 | -- |
| ≤10.5 | 146 (13.6) | 0.65 | 0.42, 1.01 | 1.20 | 0.73, 1.98 | 0.98 | 0.62, 1.55 |
| >10.5 | 123 (11.4) | 0.42 | 0.25, 0.72 | 0.91 | 0.50, 1.63 | 0.62 | 0.36, 1.08 |
| Adult and Child Care MVPA (MET-hrs/wk)b | |||||||
| 0 | 1045 (97.0) | 1.00 | -- | 1.00 | -- | 1.00 | -- |
| >0 | 32 (3.0) | 0.69 | 0.20, 2.44 | 0.44 | 0.15, 1.30 | 0.50 | 0.19, 1.30 |
| Indoor Household MVPA (MET-hrs/wk)c | |||||||
| 0 | 998 (92.7) | 1.00 | -- | 1.00 | -- | -- | -- |
| ≤6 | 46 (4.3) | 0.87 | 0.43, 1.78 | 0.86 | 0.38, 1.94 | -- | -- |
| >6 | 33 (3.1) | 2.94 | 1.46, 5.91 | 3.00 | 1.34, 6.72 | -- | -- |
| Outdoor Household MVPA (MET-hrs/wk)c | |||||||
| 0 | 1030 (95.6) | 1.00 | -- | 1.00 | -- | -- | -- |
| ≤5.5 | 26 (2.4) | 0.93 | 0.37, 2.33 | 0.67 | 0.23, 1.95 | -- | -- |
| >5.5 | 21 (2.0) | 2.81 | 1.18, 6.68 | 2.44 | 0.88, 6.75 | -- | -- |
Fully adjusted model adjusted for depressive symptoms at <20 weeks' gestation, education.
Fully adjusted model adjusted for depressive symptoms at <20 weeks' gestation, social support, smoking.
Fully adjusted model adjusted for depressive symptoms at <20 weeks' gestation.
Reduced models are not adjusted for depressive symptoms at <20 weeks' gestation.
For domain-specific measures of both perceived and absolute intensities, we re-ran all adjusted models, adding a covariate for MVPA outside of the specific domain of interest to account for this potential confounding. For example, the recreational activity model was adjusted for total activity subtracting out recreational activity. The models did not substantially change when other domains were included as covariates.
Women who met the physical activity recommendations according to perceived intensities at 17–22 weeks' gestation had 1.35 (95% CI=0.98, 1.86) times the odds of having elevated depressive symptoms at 24–29 weeks' gestation after adjusting for depressive symptoms at <20 weeks' gestation. For both intensity types, we combined participation levels of work, adult and child care, indoor household, outdoor household, and transportation activities into one measure to represent non-elective (vs. recreational) activity. For those participating in some MVPA but less than or equal to the median (2 hours) of non-elective MVPA, the odds of developing elevated depressive symptoms at 24–29 weeks' gestation compared to women with no MVPA was 0.69 (95% CI=0.46, 1.06) after adjusting for depressive symptom at <20 weeks' gestation and life events. However, those with more than 2 hours of non-elective MVPA were more likely to develop high depressive symptoms (OR=1.73, 95% CI=1.17, 2.56). There was a null association between non-elective activity in METS and depressive symptoms at 24–29 weeks' gestation among women with any MVPA but less than or equal to the median of 4.89 METS (OR=0.96, 95% CI=0.55, 1.66) with adjustment for depressive symptoms at <20 weeks' gestation and education, but those with more than the median METS of non-elective activity had 1.77 times the odds of developing elevated depressive symptoms (95% CI=1.08, 2.88).
Discussion
We found few associations between total and domain-specific MVPA at 17–22 weeks' gestation and depressive symptoms at 24–29 weeks' gestation. Total perceived MVPA was associated with reduced odds of elevated depressive symptoms. Associations between recreational activity and depressive symptoms, the mostly frequently investigated physical activity domain, produced estimates close to the null in adjusted modeling. Women who participated in adult and child care activity of perceived moderate-to-vigorous intensity had increased odds of having high depressive symptoms. Women participating in high amounts of indoor household activity had increased odds of having high depressive symptoms. Increased odds of elevated depressive symptoms were found among women who met physical activity recommendations and participated in more than median levels of non-elective MVPA for both perceived and absolute intensities.
There has been limited previous research into associations of physical activity with depression in pregnant populations. Most studies reported cross-sectional associations between physical activity and depressive symptoms or mood, failing to examine the longitudinal associations between physical activity and subsequent depression. Associations have been found with total or recreational activities and depressive symptoms and depressed mood among pregnant adolescents self-selected to participate in a trial in Los Angeles (Koniak-Griffin 1994) and cross-sectional analysis of pregnant Canadian women (Da Costa et al. 2003), pregnant California women (Haas et al. 2004), pregnant African-American women in Baltimore (Orr et al. 2006), and pregnant women in Jamaica (Pottinger et al. 2009). In each study, active women were less likely to have depressive symptoms than inactive women; however, Pottinger et al. (2009) found decreased odds for occasional exercise, but not frequent exercise. Other studies have found primarily no associations between total or recreational physical activity and depressive symptoms (Goodwin et al. 2000; Poudevigne and O'Connor 2005; Symons Downs et al. 2008).
Symons Downs et al. (2008) was the only previous study reporting on the association between physical activity during the second trimester and depressive symptoms during the third trimester. They found no association for leisure-time physical activity, which corresponds with our reported findings on the association between recreational MVPA and depressive symptoms. We also found increased odds of high depressive symptoms with adult and child care MVPA and indoor household MVPA. These tasks are associated with home-keeping. A study of pregnant Italian women found that being a housewife was associated with increased odds of minor depression as compared to being a student, unemployed, or employed (Marchesi et al. 2009). We found that higher levels of non-elective MVPA (participation in work, adult and child care, indoor household, outdoor household, and transportation activities) was associated with increased odds of developing elevated depressive symptoms. In comparison to recreational activities, these activities are not usually performed for enjoyment or electively and may be considered burdensome. Molarius et al. (2009) found that the odds of being moderately or extremely depressed or anxious increased as the more burdensome the participants rated their domestic work. Simply higher participation levels in housework may be considered burdensome for women, which may explain why women with those with low levels of both indoor and household MVPA have a slightly reduced odds of having elevated depressive symptoms while those with higher than median levels have increased odds.
Strengths and Limitations
There are some limitations in our study. First, self-report depression scales such as the CES-D measure depressive symptoms. Clinical assessment is needed to diagnose depression. However, clinical assessments in population studies are costly and timely. Depression screening tools are frequently used in depression research involving large samples. The CES-D is a commonly used, reliable, and valid measurement of depressive symptoms that correlates well with clinical ratings (Radloff 1997; Weissman et al. 1977). Overall, investigating depression during pregnancy is difficult. Self-reported screening tools tend to focus on somatic symptoms, including symptoms that overlap between pregnancy and depression, which makes determining depression status difficult in a pregnant population (Ryan et al. 2005; Brown and Solchany 2004; Misri 2007; Klein and Essex 1994). To address this, we used a slightly higher threshold for high depressive symptoms than used in the general population. This cut point of 17 was compared to a method suggested by Hoffman and Hatch (2000) where the four scale items related to pregnancy are removed and the remaining items inflated so the scale range remains 0–60 and the 16 cut point is still used. The scores calculated by each method were highly correlated with each other (Pearson's r=0.98) and the women were largely categorized into the same binary depressive symptoms category (χ2=849.64, p<0.0001). When these re-categorized depressive symptoms scores were used in modeling, they performed similarly to our original scoring method and there was no change in the interpretation of the results.
Determining if physical activity is a causal factor of elevated depressive symptoms is not possible in this study. We did not assess levels of depressive symptoms or diagnoses of depressive disorders for the pre-pregnancy period. Therefore, our case group is a mix of individuals with incident, recurrent, and persistent elevated symptoms. However, we did control for depressive symptoms at <20 weeks in all adjusted models. Furthermore, depression is not an acute condition; it is likely that it takes an extended period of time for physical activity to have an effect on depression. The physical activity and depressive symptoms measures in our study may be too close together in time; two weeks separated the end of the physical activity assessment and the start of the depressive symptoms assessment. In this exploratory study we have tested many associations, but chose not to adjust for multiple testing. Therefore, significance should be interpreted with caution, and replication of results is needed.
Physical activity assessment was more extensive than conducted in previous pregnancy studies. From self-reported data of frequency and duration of various activities and compendium-established MET values, we were able to calculate activity levels of both perceived and absolute intensity and examine differences the associations with depressive symptoms by domain. Another concern is that the MET values used for determining absolute intensity are not specific to pregnant populations, and pregnancy increases a woman's resting metabolic rate by 15–20% (Clapp 2002). Therefore, these values may not be the most appropriate to use in this sample. However, no standards have yet been established for pregnant women and they may change over the course of pregnancy. Physical activity in this sample was low, particularly for most domain-specific activities. It is possible that different associations would be suggested in samples of more active women with wider ranges of physical activity levels. Another concern is that physical activity was only assessed during the past week. Physical activity behavior can change from week to week and the reported values may not be representative of usual behavior.
Generalizability of the results may be of concern in this investigation as this sample was mostly White, well-educated, married, and financially stable. Also, the women in the final sample may not be representative of the overall PIN3 study sample. We excluded women who had no usable physical activity or depressive symptoms data (n=455). Excluded women were more likely to be a minority, unmarried, younger, less education, and poorer. These factors are related to physical activity and depression and this may create bias in the associations.
Despite these limitations, there are several strengths of our study. It is a large, prospective cohort study that measured a variety of factors relevant to the health of pregnant women. The longitudinal design of the study allowed us to examine the association with earlier physical activity with later depressive symptoms. Reliable and valid assessment tools were used to measure physical activity (Evenson and Wen 2010), depression (Radloff 1977; Weissman et al. 1977), and a number of the covariates (Sarason et al. 1978; Sherbourne and Stewart 1991). The physical activity assessment was comprehensive- collecting data on duration, frequency, intensity, and domain. Previous research has only investigated leisure-time or total activity. Data collection was extensive which allowed for good control for confounders; however, as in any observational study, there may still be residual confounding.
Conclusion
This study investigates how the association between physical activity and depressive symptoms differs by domain of activity in a pregnant population. We found that participation in total MVPA reduced the odds of high depressive symptoms, but that participation in adult and child care MPVA and indoor household MVPA may heighten depressive symptoms rather than be beneficial. Future research should explore how the association between physical activity and depressive symptoms differs by domain. Furthermore, studies should investigate differences in association by intensity of activity (perceived vs. absolute and including light activities vs. MPVA). There has been an increased focus on the potential for physical activity to serve as a non-drug treatment for depression as antidepressant use concerns both mother and health providers (Hammond and Crozier 2007; Bowen and Muhajarine 2006; Manber et al. 2002). Physical activity is a good candidate as it has minimal side effects, is cost-effective, and has been shown to be as effective as antidepressants and psychotherapy in non-pregnant populations (Daley et al 2007; Dunn et al. 2005; Craft and Perna 2004; Martinsen 2008). Given adequate evidence from studies using pregnant populations, physical activity may be a useful treatment for depression.
Acknowledgements
The third phase of the Pregnancy, Infection, and Nutrition Study (PIN3) was supported by National Institutes of Health (NIH) grants from the National Institute of Child Health and Human Development (#HD37584, HD39373), the National Institute of Diabetes and Digestive and Kidney Diseases (DK61981, DK56350), the National Cancer Institute (#RO1CA109804), and the General Clinical Research Center (#RR00046). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors would like to thank Drs. David Savitz and John Thorp, Principal Investigators of the PIN3 Study, for their support of this analysis and Chyrise Bradley, Kathryn Carrier, Diane Kaczor, and Fang Wen for their assistance.
References
- Ainsworth BE, Haskell WL, Leon AS, Jacobs DR, Jr, Montoye HJ, Sallis JF, Paffenbarger RS., Jr Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25(10):71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, Jacobs DR, Jr, Leon AS. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl):S498–516. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstet Gynecol. 2004;103:698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- Borg G, Linderholm H. Perceived exertion and pulse rate during graded exercise in various age groups. Acta Med Scand. 1974;472:194–206. [Google Scholar]
- Bowen A, Muhajarine N. Antenatal depression. Can Nurse. 2006;102(9):27–30. [PubMed] [Google Scholar]
- Brown M-A, Solchany JE. Two overlooked mood disorders in women: subsyndromal depression and prenatal depression. Nurs Clin N Am. 2004;39:83–95. doi: 10.1016/j.cnur.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Clapp JF., III . Exercising through your pregnancy. Addicus Books; Omaha, NE: 2002. [Google Scholar]
- Craft LL, Perna FM. The benefits of exercise for the clinically depressed. Prim Care Companion J Clin Psychiatry. 2004;6:104–111. doi: 10.4088/pcc.v06n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Costa D, Rippen N, Drista M, Ring A. Self-reported leisure-time physical activity during pregnancy and relationship to psychological well-being. J Psychosom Obstet Gynaecol. 2003;24(2):111–9. doi: 10.3109/01674820309042808. [DOI] [PubMed] [Google Scholar]
- Daley AJ, MacArthur C, Winter H. The role of exercise in treating postpartum depression: a review of the literature. J Midwifery Womens Health. 2007;52:56–62. doi: 10.1016/j.jmwh.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28:1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Wen F. Measuring physical activity in pregnant women: validity and reliability of a structured one-week recall questionnaire. Int J Behav Nutr Phys Act. 2010;7:21. doi: 10.1186/1479-5868-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC. AHRQ Publication No. 05-E006-2. Agency for Healthcare Research and Quality; Rockville, MD: 2005. Perinatal Depression: prevalence, screening accuracy, and screening outcomes. evidence report/technology assessment No. 119 (Prepared by the RTI-University of North Carolina Evidence-based Practice Center, under Contract No. 290-02-0016) [Google Scholar]
- Goodwin A, Astbury J, McMeeken J. Body image and psychological well-being in pregnancy: a comparison of exercisers and non-exercisers. Aust N Z J Obstet Gynaecol. 2000;40:43–7. doi: 10.1111/j.1479-828x.2000.tb01178.x. [DOI] [PubMed] [Google Scholar]
- Gregory M, Ulmer H, Pfeiffer KP, Lang S, Strasak AM. A set of SAS macros for calculating and displaying adjusted odds ratios (with confidence intervals) for continuous covariates in logistic B-spline regression models. Comput Methods Programs Biomed. 2008;92:109–114. doi: 10.1016/j.cmpb.2008.05.004. [DOI] [PubMed] [Google Scholar]
- Haas JS, Jackson RA, Fuentes-Afflick E, Stewart AL, Dean ML, Brawarsky P, Escobar G. Changes in the health status of women during and after pregnancy. J Gen Intern Med. 2004;20:45–51. doi: 10.1111/j.1525-1497.2004.40097.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond S, Crozier K. Depression: assessing the causes. Midwives. 2007;10(8):365–368. [PubMed] [Google Scholar]
- Hoffman S, Hatch MC. Depressive symptomatology during pregnancy: Evidence for an association with decreased fetal growth in pregnancies of lower social class women. Health Psychol. 2000;19(6):535–543. [PubMed] [Google Scholar]
- Institute of Medicine . Nutrition during pregnancy. National Academy Press; Washington, DC: 1990. [Google Scholar]
- Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey 1: Lifetime prevalence, chronicity, and recurrence. J Affect Disord. 1993;29:85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- Klein MH, Essex MJ. Pregnant or depressed? The effect of overlap between symptoms of depression and somatic complaints of pregnancy on rates of major depression in the second trimester. Depression. 1994/1995;2(6):308–314. [Google Scholar]
- Koniak-Griffin D. Aerobic exercise, psychological well-being, and physical discomforts during adolescent pregnancy. Res Nurs Health. 1994;17(4):253–63. doi: 10.1002/nur.4770170404. [DOI] [PubMed] [Google Scholar]
- Larsson C, Sydsjö G, Josefsson A. Health, sociodemographic data, and pregnancy outcome in women with antepartum depressive symptoms. Obstet Gynecol. 2004;104:459–66. doi: 10.1097/01.AOG.0000136087.46864.e4. [DOI] [PubMed] [Google Scholar]
- Lee DTS, Chung TKH. Postnatal depression: an update. Best Pract Res Clin Obstet Gynaecol. 2007;21(2):183–191. doi: 10.1016/j.bpobgyn.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Lusskin SI, Pundiak TM, Habib SM. Perinatal depression: hiding in plain sight. Can J Psychiatry. 2007;52:479–88. doi: 10.1177/070674370705200802. [DOI] [PubMed] [Google Scholar]
- Manber R, Allen JJB, Morris MM. Alternative treatments for depression: Empirical support and relevance for women. J Clin Psychiatry. 2002;63:628–640. doi: 10.4088/jcp.v63n0716. [DOI] [PubMed] [Google Scholar]
- Marchesi C, Bertoni S, Maggini C. Major and minor depression in pregnancy. Obstet Gynecol. 2009;113:1292–8. doi: 10.1097/AOG.0b013e3181a45e90. [DOI] [PubMed] [Google Scholar]
- Martinsen EW. Physical activity in the prevention and treatment of anxiety and depression. Nord J Psychiatry. 2008;62(Suppl 47):25–29. doi: 10.1080/08039480802315640. [DOI] [PubMed] [Google Scholar]
- Misri S. Suffering in silence: The burden of perinatal depression. Can J Psychiatry. 2007;52(8):477–478. doi: 10.1177/070674370705200801. [DOI] [PubMed] [Google Scholar]
- Molarius A, Berglund K, Eriksson C, Eriksson HG, Lindén-Boström M, Nordström E, Persson C, Sahlqvist L, Starrin B, Ydreborg B. Mental health symptoms in relation to socioeconomic conditions and lifestyle factors- a population-based study in Sweden. BMC Public Health. 2009;9:302. doi: 10.1186/1471-2458-9-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health . NIH Publication No. 07-3561. U.S. Department of Health & Human Services, National Institutes of Health, National Institute of Mental Health; Bethesda, MD: 2007. Depression. [Google Scholar]
- National Institute of Mental Health . Women and depression: discovering hope. U.S. Department of Health & Human Services, National Institutes of Health, National Institute of Mental Health; Bethesda, MD: 2008. [Google Scholar]
- Orr ST, James SA, Garry J, Newton E. Exercise participation before and during pregnancy among low-income, urban, Black women: The Baltimore Preterm Birth Study. Eth Dis. 2006;16:909–913. [PubMed] [Google Scholar]
- Orr ST, Miller CA. Maternal depressive symptoms and the risk of poor pregnancy outcome: review of literature and preliminary findings. Epidemiol Rev. 1995;17:165–71. doi: 10.1093/oxfordjournals.epirev.a036172. [DOI] [PubMed] [Google Scholar]
- Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC, Kriska A, Leon AS, Marcus BH, Morris J, Paffenbarger RS, Jr, Patrick K, Pollock ML, Rippe JM, Sallis J, Wilmore JH. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–7. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- Pivarnik JM, Chambliss HO, Clapp JF, Dugan SA, Hatch MC, Lovelady CA, Mottola MF, Williams MA. Impact of physical activity during pregnancy and postpartum on chronic disease risk. Med Sci Sports Exerc. 2006;38(5):989–1006. doi: 10.1249/01.mss.0000218147.51025.8a. [DOI] [PubMed] [Google Scholar]
- Pollock M, Gaesser G, Butcher J, Després J-P, Dishman RK, Franklin BA, Garber CE. American College of Sports Medicine position stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30(6):975–91. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- Pottinger AM, Trotman-Edwards H, Younger N. Detecting depression during pregnancy and associated lifestyle practices and concerns among women in a hospital-based obstetric clinic in Jamaica. Gen Hosp Psychiatry. 2009;31:254–261. doi: 10.1016/j.genhosppsych.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Poudevigne MS, O'Connor PJ. Physical activity and mood during pregnancy. Med Sci Sports Exerc. 2005;37(8):1374–1380. doi: 10.1249/01.mss.0000174907.27818.ff. [DOI] [PubMed] [Google Scholar]
- Pregnancy, Infection, and Nutrition Study [Accessed 5 July 2009];PIN3 Physical Activity. 2007 http://www.cpc.unc.edu/projects/pin/design_pin3/docs_3/PIN-MET-Table-080207.pdf.
- Proctor BD, Dalaker J. Current Population Reports. U.S. Government Printing Office; Washington, DC: 2002. U.S. Bureau of the Census; p. 5. (Series P60-219, Poverty in the United States: 2001). [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- Rothman KJ, Greenland S. Modern Epidemiology. 2nd edn Lippincott-Raven Publishers; Baltimore: 1998. pp. 256–257. [Google Scholar]
- Ryan D, Milis L, Misri N. Depression during pregnancy. Can Fam Physician. 2005;51:1087–1093. [PMC free article] [PubMed] [Google Scholar]
- Sarason IG, Johnson JH, Siegel JM. Assessing the impact of the life experiences survey. J Consult Clin Psychol. 1978;46:932–46. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- Sherborne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Symons Downs D, DiNallo JM, Kirner TL. Determinants of pregnancy and postpartum depression: prospective influences of depressive symptoms, body image satisfaction, and exercise behavior. Ann Behav Med. 2008;36:54–63. doi: 10.1007/s12160-008-9044-9. [DOI] [PubMed] [Google Scholar]
- Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: a review. Prev Med. 2008;46:397–411. doi: 10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture, Food and Nutrition Service Special supplemental nutrition program for Women, Infants and Children (WIC): income eligibility guidelines. Fed Regist. 2009;74(43):9780–9782. [Google Scholar]
- U.S. Department of Health and Human Services . ODPHP Publication No. U0036. U.S. Department of Health & Human Services; Bethesda, MD: 2008. [Accessed 1 June 2009]. 2008 Physical activity guidelines for Americans. http://www.health.gov/paguidelines. [Google Scholar]
- US Department of Health and Human Services . NIH Publication No. 07-3561. Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health; Bethesda, MD: 2007. [Accessed 17 July 2009]. Depression. http://www.nimh.nih.gov/health/publications/depression/nimhdepression.pdf. [Google Scholar]
- U.S. Department of Health and Human Services . Physical activity and health: a report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; Atlanta, GA: 1996. [Google Scholar]
- Vladutiu C, Evenson KR, Marshall S. Physical activity and injuries during pregnancy. J Phys Act Health. doi: 10.1123/jpah.7.6.761. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity: Best practices and research recommendations. Med Sci Sports Exerc. 2005;37(11 Suppl):S582–S588. doi: 10.1249/01.mss.0000185292.71933.91. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bland R, Joyce PR, Newman S, Wells JE, Wittchen H-U. Sex differences in rates of depression: cross-national perspectives. J Affect Disord. 1993;29(2–3):77–84. doi: 10.1016/0165-0327(93)90025-f. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106(3):203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]