Abstract
Objective
To investigate the efficacy and safety of regional intra-arterial chemotherapy (RIAC) versus systemic chemotherapy for stage III/IV pancreatic cancer.
Methods
Randomized controlled trials of patients with advanced pancreatic cancer treated by regional intra-arterial or systemic chemotherapy were identified using PubMed, ISI, EMBASE, Cochrane Library, Google, Chinese Scientific Journals Database (VIP), and China National Knowledge Infrastructure (CNKI) electronic databases, for all publications dated between 1960 and December 31, 2010. Data was independently extracted by two reviewers. Odds ratios and relative risks were pooled using either fixed- or random-effects models, depending on I2 statistic and Q test assessments of heterogeneity. Statistical analysis was performed using RevMan 5.0.
Results
Six randomized controlled trials comprised of 298 patients met the standards for inclusion in the meta-analysis, among 492 articles that were identified. Eight patients achieved complete remission (CR) with regional intra-arterial chemotherapy (RIAC), whereas no patients achieved CR with systemic chemotherapy. Compared with systemic chemotherapy, patients receiving RIAC had superior partial remissions (RR = 1.99, 95% CI: 1.50, 2.65; 58.06% with RIAC and 29.37% with systemic treatment), clinical benefits (RR = 2.34, 95% CI: 1.84, 2.97; 78.06% with RAIC and 29.37% with systemic treatment), total complication rates (RR = 0.72, 95% CI: 0.60, 0.87; 49.03% with RIAC and 71.33% with systemic treatment), and hematological side effects (RR = 0.76, 95% CI: 0.63, 0.91; 60.87% with RIAC and 85.71% with systemic treatment). The median survival time with RIAC (5–21 months) was longer than for systemic chemotherapy (2.7–14 months). Similarly, one year survival rates with RIAC (28.6%−41.2%) were higher than with systemic chemotherapy (0%−12.9%.).
Conclusion
Regional intra-arterial chemotherapy is more effective and has fewer complications than systemic chemotherapy for treating advanced pancreatic cancer.
Introduction
Pancreatic carcinoma is one of the deadliest cancers. It is the only cancer with relative five-year survival rates that are less than 10%. This is due, in part, to the fact that 80% of patients have advanced unresectable disease at the time of diagnosis [1]. For patients that are not surgical candidates, chemotherapy is typically offered. However, the response rate to standard systemic chemotherapy is very low. Gemcitabine (GEM), the most commonly used first-line drug in pancreatic cancer, only has a 5–15% response rate. In addition, GEM in combination with other anti-cancer drugs does not significantly improve survival [2]. The median survival time for patients with advanced pancreatic cancer is less than 6 months and the 1-year survival rate is less than 18% [3], [4], [5], [6].
Regional chemotherapy, such as regional intra-arterial chemotherapy (RIAC), was introduced as a means of increasing cancer survival rates. Since the 1950s, regional chemotherapy has been evaluated and proven to be effective for some metastatic and localized cancers. Intra-arterial chemotherapy generates high drug concentrations in target areas while maintaining low systemic drug levels. Patients with unresectable colorectal cancer and liver metastasis had high response rates to hepatic arterial infusion (HAI) of chemotherapeutic agents and some tumors also converted to resectability [7], [8]. Clinical trials showed that regional intra-arterial infusion with GEM improved the response and resectability rates for advanced pancreatic cancer (APC), and was well tolerated by patients [9], [10]. However, other research did not show improved tumor response or median survival with regional chemotherapy for pancreatic cancer, thereby casting doubt upon its value as a treatment option for patients with unresectable or recurrent pancreatic cancer [11].
The value of RIAC for treating advanced pancreatic cancer is still unclear. The aim of this study is to clarify the value of RIAC in treating APC by comparing its safety and efficacy with systemic chemotherapy.
Materials and Methods
Search Strategy
Studies were identified by searching PubMed(1966–2010.12), ISI(1997–2010.12), EMBASE(1984–2010.12), Cochrane Library(Issue 1, 2011), Chinese Scientific Journals Database (VIP: 1977–2010.12), and China National Knowledge Infrastructure (CNKI: 1994–2010.12) electronic databases. The keywords“pancreas/pancreatic cancer”, and the Medical Subject Headings (MeSH) “pancreatic neoplasm” and “intra-arterial chemotherapy”, were combined with exploded index terms and synonyms for searches of keywords, abstracts, and titles. The search strategy used was: 1# pancreatic cancer, 2# pancreas cancer; 3# pancreatic carcinoma; 4# pancreas carcinoma; 5# MeSH descriptor “pancreatic neoplasm” explode all trees; 6# regional arterial infusion; 7# arterial perfusion; 8# regional chemotherapy; 9# intra-arterial chemotherapy; 10# trans-artery chemotherapy; 11# hepatic arterial infusion; 12# celiac artery; 13# drug delivery pathway; 14# splenic artery; 15# regional treatment;16# locally intra-arterial infusion; 17#: 1# or 2# or 3# or 4# or 5#; 18#: 6# or 7# or 8# or 9# or 10# or 11# or 12# or 13# or 14# or 15# or 16#; 19#: 17# and 18#.
Selection Criterion
Only prospective randomized controlled trials (RCT) were selected for inclusion in the study. Patients with APC, regardless of the existence of liver or peritoneal metastasis, were included in this study. Patients were treated with either RIAC (via the cancer feeding artery, hepatic artery, celiac artery, gestroduodenal artery, superior mesenteric artery, common hepatic artery, splenic artery, or other regional arteries, with or without regional embolization), or systemic intravenous chemotherapy (via central or peripheral veins). Systematic reviews of randomized controlled trials were included. Comparative studies (historical and non-randomized) and those where pancreatic cancer was not confirmed by pathology or by imaging (such as CT, MRI) were excluded.
Quality Assessment
We assessed the methodological quality of each RCT using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (CHSRI). The following CHSRI components were assessed by two reviewers (FHL and YT): adequate generation of random sequences (selection bias), allocation concealment (selection bias), blinding (performance bias and detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), source of funding bias, baseline imbalance, and early stoppage. These components were graded as low risk, high risk or unclear. Methodological information for the assessment of validity was extracted by two reviewers (FHL and JWS).
Data Extraction and Analysis
A pre-designed data extraction table was used to extract the characteristic data of the eligible articles by two independent reviewers (FHL and JWS), with reviewer discrepancies resolved by a supervisor (YT). The following information was extracted from each report: authors, time of publication, patient eligibility criteria, number of patients in the RIAC and systemic treatment groups, gender, and route of drug administration. Major end-points extracted for each report were: complete remission (CR), partial remission (PR), clinical benefit, pain-control, and complication rate. The end-point definitions used were: CR was complete disappearance of liver metastasis or the primary pancreatic cancer; PR was the diameter of all liver metastases with no evidence of new or progressive lesions; no change (NC) was a <50% reduction or a <25% increase in diameter; progressive disease (PD) was a >25% increase in diameter of one or more liver metastases, or the occurrence of new liver metastases. Treatments were considered effective for patients achieving CR or PR. Patients achieving pain relief or an increase of (KPS) or (PS) were classified as receiving clinical benefits [12]. Side effects of interest mainly involved the hematological (leucopenia, thrombocytopenia or anemia) and gastrointestinal systems (nausea, vomiting or duodenal ulcer). Embolization, thrombophlebitis and catheter displacement were additional complications of interest.
Statistical heterogeneity among studies was assessed using Q and I2 statistics. Meta-analysis of studies with an acceptable level of heterogeneity (p>0.1, or p≤0.1 but I2≤50%) was conducted using a fixed-effects model. A random-effects model was used for studies where significant heterogeneity was found (p≤0.1, I2>50%). Parameters that were analyzed included the number of the patients, major end-points (CR, PR, clinical benefit, pain relief, response rate, and complication rate), and digestive and hematological side-effects. Statistical significance was P≤0.05. Data from RCTs meeting inclusion criteria were analyzed with Revman 5.0 (RevMan 5.0.23; Cochrane Collaboration, Oxford, UK).
Results
Study Characteristics
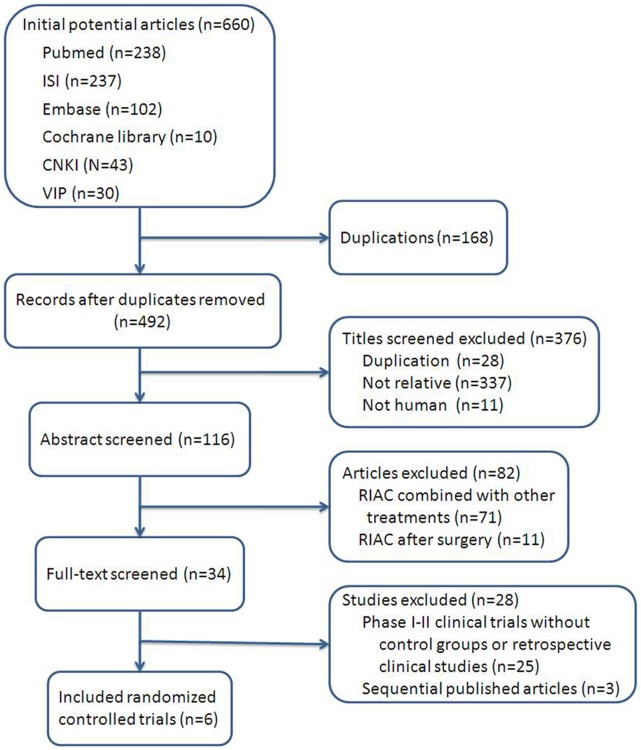
The database search strategy initially retrieved 660 publications, and 168 were eliminated due to duplication (Table 1). English [12], [13], [14], [15] (n = 4) and Chinese [16], [17] (n = 2) language publications met the study’s inclusion criteria. These publications included patients receiving RIAC (n = 155) and systemic chemotherapy (n = 143) (Figure 1). No systematic review or meta-analysis was found.
Table 1. Study characteristics.
| Study, Country | Samplesize | Diagnosis | Liver metastasis n/N | Mean age (y) | Drugs | GenderNo. M/F | Drug delivery routes | Median or mean survival time (ST) | |||||
| LIAC/C | LIAC | C | LIAC | C | LIAC | C | LIAC | C | |||||
| Han. 2006, China [12] | 70/70 | Biopsy proven | NG | 60.2 | FAM | FAM | 110/30 | celiac artery splenicartery | intravenous | 13.5 m | 6.2 m | ||
| Shamseddine.2005,America [15] | 7/4 | Biopsy proven | 4/11 | NR | GEM | GEM | NR | tumor-feeding arteries | intravenous | 5 m | 5.6 m | ||
| Ji. 2003, China [14] | 18/11 | pathological/CT/CA199/MRI | 8/18 | 4/11 | 62.4 | MF | MF | 16/12 | splenic artery, gestroduodenalartery, commonhepatic artery | intravenous | 12.5 m (mean ST) | 4.8 m (mean ST) | |
| Aigner.1998,Gemany [13] | 9/5 | pathological/CT/MRI | 7/9 | 4/5 | 56 | MmMC | MmMC | 11/3 | celiac artery | central venous | 8.9 m | 2.7 m | |
| Liu. 2008, China [17] | 26/27 | pathological/CT/MRI | 7/26 | 9/27 | 61 | GP | GP | 30/23 | superior mesentericartery | intravenous | 21 m | 14 m | |
| Hong. 2007,China [16] | 25/26 | pathological/CT/MRI | 30/51 | NR | GF | GF | NR | tumor-feeding arteries | intravenous | 10 m | 7.3 m | ||
FAM: adriamycin 40 mg/m2, mitomycin (MMC) 6 mg/m2, d1; 5-fluorouracil (5-FU), 375 mg/m2, d2-6.
GEM: Gemcitabine, 1000 mg/m2, day 1, 8.
MF: MMC, 2 mg, d2, 4,6; 5-FU, 750 mg, day 1, 3, 5.
MmMC: Mitomycin C at a total dose of 18 mg/m2, day 1–5; mitoxanthrone, 6 mg/m2, day 6; cisplatin, 30 mg/m2, day 7–8.
GP: Gemcitabine 1000 mg/m2, day 1; cisplatin, 50 mg/m2, day 1.
GF (GEM+5-FU): GEM 1000 mg/m2, day 1; 5-Fu, 600 mg/m2, day 1–5.
NR: not reported.
Figure 1. The process of study selecting of articles.
The process of searching for articles for inclusion in this systematic review: 660 articles were found and 492 articles remained after removal of duplicates. After review of the complete texts, 6 articles met the inclusion criteria and were included in the meta-analysis.
Quality Assessment
One study explicitly stated that patients were selected using a random envelope process [17], whereas the other studies did not indicate that random selection was employed. One study could not be assessed for adequate sequence generation [15]. No studies were blinded and there was no evidence of allocation concealment. No funding biases were evident for any studies. There were no studies with incomplete outcome data, early stoppage bias, or baseline imbalances. The risks of bias and corresponding ratios were summarized (Table 2).
Table 2. Evaluation of the quality of RCTs included in the meta-analysis.
| Risk of bias | Random sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective reporting | Other bias |
| Aigner.1998 | Unclear | Unclear | High risk | Low risk | Low risk | Low risk |
| Han. 2006 | Unclear | Unclear | High risk | Low risk | Low risk | Low risk |
| Ji.2003 | Unclear | Unclear | High risk | Low risk | Low risk | Low risk |
| Hong. 2007 | High risk | Unclear | High risk | Low risk | Low risk | Low risk |
| Liu. 2008 | Low risk | Unclear | High risk | Low risk | Low risk | Low risk |
| Shamseddine. 2005 | High risk | Unclear | High risk | Low risk | Low risk | Low risk |
Efficacy
Overall survival
Five studies [12], [13], [15], [16], [17] reported that RIAC median survival times (5–21 months) were longer than for systemic chemotherapy (2.7–14 months).One of these RCTs [13], [16] had survival times in the systemic group of 3.5, 6, 11, 13, 20 months, whereas they were 15, 16, 25, 31, 33, 39, 47, 56, 59 months, for RIAC patients. One of these RCTs [16]had longer RIAC survivorship than for systemic chemotherapy for 6-month (84.0% vs. 52.5%), 9-month (76.0% vs. 38.9%), 1-year overall survival (OS) (48% vs.14.6%) and median survival times (10.0 m vs.7.3 m). These two RCTs demonstrated that patients receiving RIAC had greater 1-year OS (41.2%−28.6%) compared with systemic chemotherapy (0–12.9%). We had tried to contact with authors, but we were unable to obtain further information for inclusion in our meta-analysis.
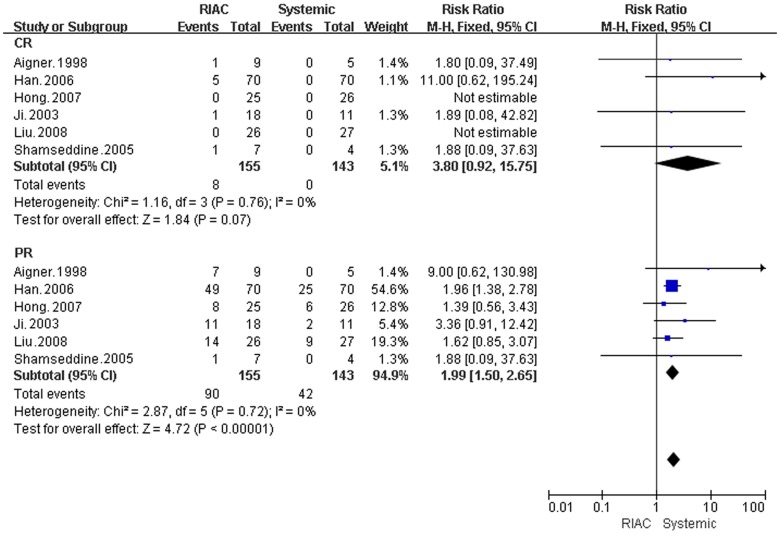
Complete remission and partial remission
Six studies (298 patients) were selected for the meta-analysis. The RIAC and systemic groups did not differ significantly for CR (RR = 3.80, 95% CI: 0.92, 15.75). However, unlike the patients treated with systemic therapy, there were patients that achieved CR with RIAC (n = 8) [12], [13], [14], [17], and one patient became eligible for R0-resection [13]. In addition, patients treated with RIAC (n = 90; 58.06%), had better PR than did patients treated with systemic chemotherapy (n = 42; 29.37%) (RR = 1.99, 95% CI: 1.50, 2.65) (Figure 2).
Figure 2. Meta-analysis of CR and PR.
Diamonds represent pooled effects. CR = complete remission, PR = partial remission.
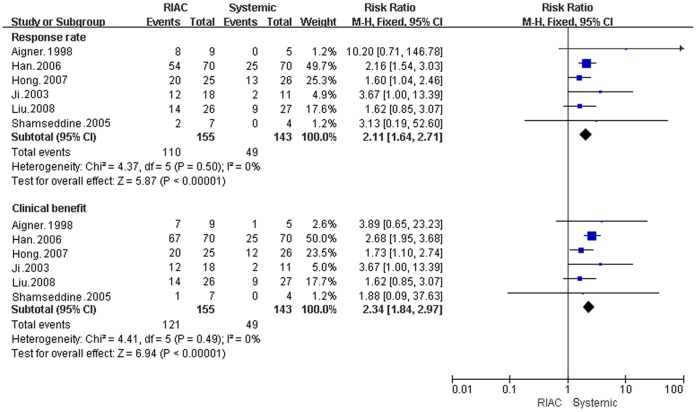
Clinical benefit and response rates
Patients in the RIAC group received more clinical benefits (78.06% )(RR = 2.34, 95% CI: 1.84, 2.97) and better response rates (70.97%) (RR = 2.11, 95% CI: 1.64, 2.71) than the systemic group (29.37% and 34.27%, respectively) (Figure 3).
Figure 3. Meta-analysis of response rates and clinical benefits.
Diamonds represent pooled effects.
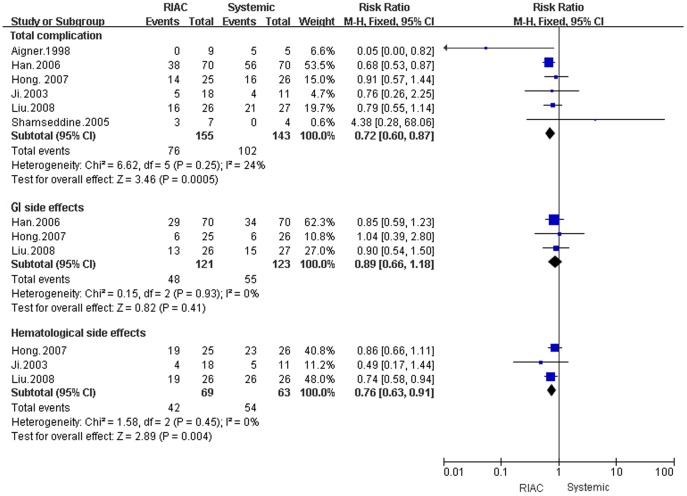
Complications
Gastrointestinal and hematological side effects
The overall incidence of complications was lower in RIAC patients (49.03%) than those receiving systemic chemotherapy (71.33%) (RR = 0.72, 95% CI: 0.60, 0.87). No deaths due to drug toxicity were reported, and there were no differences in gastrointestinal side effects (RR = 0.82, 95% CI: 0.66, 1.18). However, the RIAC group (60.87%) had fewer hematological side effects than the systemic group (85.71%) (RR = 0.76, 95% CI: 0.63, 0.91) (Figure 4).
Figure 4. Meta-analysis of the incidence of complications using Regional Intra-Arterial Chemotherapy or systemic administration of chemotherapeutics.
Diamonds represent pooled effects. Total complications and hematological system side effects differed between Regional Intra-Arterial Chemotherapy and systemically treated patients (P = 0.01). Gastrointestinal system side effects did not differ between treatment groups (P = 0.35).
Catheter complications
Catheter displacement was found in one patient [16]. No patients developed embolization or thrombophlebitis associated with catheter implantation.
Discussion
Our meta-analysis of six prospective RCTs included 298 patients with APC. Compared with systemic chemotherapy for treatment of APC, RIAC resulted in higher PR, clinical benefits, and response rates with fewer complications.
Efficacy
Pancreatic cancer is relatively resistant to chemotherapy. GEM is the first-line chemotherapy drug for APC (5–15% efficiency). Combinations of GEM with other anti-cancer drugs do not significantly improve the survival of patients (OS was 5.6–8.2 months) [18], [19], [20], [21].
The effect of chemotherapy is concentration dependent. Intra-arterial infusion generates higher drug concentrations within targeted regions with lower systemic drug concentrations [22], [23], [24]. This reduces the risks of systemic toxicity while increasing target tissue drug efficacy. Shamseddine [15] measured plasma concentrations of dFdU (2′-2′-Difluorodeoxyuridine; the deammoniated metabolic product of Gemcitabine) 30 minutes and 270 minutes after administration. The concentration of dFdU in patients receiving systemic treatment was higher than for RIAC patients (RR 30 min = −5.10, 95% CI: −8.02, −2.17; RR 270 min = −173.36, 95% CI: −263.80, −82.93; P<0.05). Yang [25] found reduced hepatic metastasis (RR = 0.46, 95% CI: 0.31–0.69) and longer mean survival times (RR = 0.44, 95% CI: 0.28–0.68). in RIAC treated mice with APC. High response rates (complete response 8.7% and partial response 65.2%) in a descriptive study of 31 patients with advanced pancreatic cancer that received RIAC were accompanied by 1-, 2- and 3-year survival rates of 90.9, 42.8 and 18.3% [26], respectively. Similarly, Nakchbandi [27] demonstrated improved median survival times (12.7 months) for patients with metastatic pancreatic cancer treated with RIAC. This study identified two RCTs [13], [16] where RIAC improved the 1-year OS (41.2%−28.6%), compared with systemic chemotherapy (0−12.9%).
Complications
Side effects of chemotherapy were dependent upon the drug regimen used and the drug administration route. Common side effects included nausea, vomiting, hair loss, and bone marrow suppression. This meta-analysis result showed that overall complications for RIAC (49.03%) were less than for systemic chemotherapy (71.33%), and there were no treatment associated deaths [14], [16], [17]. However, the only statistically significant difference was for hematologic side effects (RR = 0.76, 95% CI: 0.63, 0.91; 60.87% for RIAC and 85.71% for systemically treated individuals) [12], [16], [17], and only 0.1% patients experienced severe complications. Pharmacokinetic data indicated that systemic concentrations of the drug were lower for RIAC than with systemic chemotherapy, which could be the basis for the reduction in complications for RIAC [22], [28], [29], [30], [31].
Although the value of regional chemotherapy has been demonstrated, expansion of its clinical use is constrained by some drawbacks. For example, RIAC is generally much more difficult to administer than systemic chemotherapy; it is an invasive procedure with increased time and costs of hospitalization; as well as having increased local complications. However, RIAC has superior clinical benefits and fewer systemic complications. This makes RIAC a good strategy for treatment of APC, as well as a good option for palliative or neoadjuvant therapy, especially in patients who don’t respond to standardized therapy.
Limitations
This meta-analysis has limitations. Bias may have been introduced because nonpublished data was not included and the relatively few numbers of patients in our study. Larger and more methodologically rigorous clinical trials are needed to confirm these findings.
Acknowledgments
The authors thank the Evidence-Based Medicine Center of Lanzhou University for literature searches. We are grateful to Professors Jinhui Tian, Hongliang Tian and Rao Sun for comments on the manuscript.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported by the National Natural Science Foundation of China (NSFC) 30973490, and Tianjin education committee foundation 10JCZDJC202000, 20101202110002. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Philip PA. Locally advanced pancreatic cancer: where should we go from here? J Clin Oncol. 2011;29:4066–4068. doi: 10.1200/JCO.2011.37.2532. [DOI] [PubMed] [Google Scholar]
- 2.Xie DR, Liang HL, Wang Y, Guo SS, Yang Q. Meta-analysis on inoperable pancreatic cancer: a comparison between gemcitabine-based combination therapy and gemcitabine alone. World J Gastroenterol. 2006;12:6973–6981. doi: 10.3748/wjg.v12.i43.6973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berlin JD, Catalano P, Thomas JP, Kugler JW, Haller DG, et al. Phase III study of gemcitabine in combination with fluorouracil versus gemcitabine alone in patients with advanced pancreatic carcinoma: Eastern Cooperative Oncology Group Trial E2297. J Clin Oncol. 2002;20:3270–3275. doi: 10.1200/JCO.2002.11.149. [DOI] [PubMed] [Google Scholar]
- 4.Burris HA, III, Moore MJ, Andersen J, Green MR, Rothenberg ML, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol. 1997;15:2403–2413. doi: 10.1200/JCO.1997.15.6.2403. [DOI] [PubMed] [Google Scholar]
- 5.Colucci G, Labianca R, Di Costanzo F, Gebbia V, Carteni G, et al. Randomized phase III trial of gemcitabine plus cisplatin compared with single-agent gemcitabine as first-line treatment of patients with advanced pancreatic cancer: the GIP-1 study. J Clin Oncol. 2010;28:1645–1651. doi: 10.1200/JCO.2009.25.4433. [DOI] [PubMed] [Google Scholar]
- 6.Moore MJ, Goldstein D, Hamm J, Figer A, Hecht JR, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2007;25:1960–1966. doi: 10.1200/JCO.2006.07.9525. [DOI] [PubMed] [Google Scholar]
- 7.Kingham TP, D’Angelica M, Kemeny NE. Role of intra-arterial hepatic chemotherapy in the treatment of colorectal cancer metastases. J Surg Oncol. 2010;102:988–995. doi: 10.1002/jso.21753. [DOI] [PubMed] [Google Scholar]
- 8.Bouchahda M, Adam R, Giacchetti S, Castaing D, Brezault-Bonnet C, et al. Rescue chemotherapy using multidrug chronomodulated hepatic arterial infusion for patients with heavily pretreated metastatic colorectal cancer. Cancer. 2009;115:4990–4999. doi: 10.1002/cncr.24549. [DOI] [PubMed] [Google Scholar]
- 9.Aigner KR, Gailhofer S. Celiac axis infusion and microembolization for advanced stage III/IV pancreatic cancer–a phase II study on 265 cases. Anticancer Res. 2005;25:4407–4412. [PubMed] [Google Scholar]
- 10.Li Q, Wang MQ, Duan LX, Song P, Ao GK. Regional arterial infusion chemotherapy with lipid emulsion as a solvent for the treatment of advanced pancreatic cancer: A preliminary clinical study. J Interv Radiol. 2009;18:275–277. [Google Scholar]
- 11.Lorenz M, Petrowsky H, Heinrich S, Janshon G, Staib-Sebler E, et al. Isolated hypoxic perfusion with mitomycin C in patients with advanced pancreatic cancer. Eur J Surg Oncol. 1998;24:542–547. doi: 10.1016/s0748-7983(98)93572-7. [DOI] [PubMed] [Google Scholar]
- 12.Han GH, Yin ZX, Meng XJ, He CY, Zhang HB, et al. Prospective randomized clinical trial of two drug delivery pathway in the treatment of inoperable advanced pancreatic carcinoma. Chin J Diges Dis. 2006;7:45–48. doi: 10.1111/j.1443-9573.2006.00243.x. [DOI] [PubMed] [Google Scholar]
- 13.Aigner KR, Gailhofer S, Kopp S. Regional versus systemic chemotherapy for advanced pancreatic cancer: A randomized study. Hepato-Gastroenterology. 1998;45:1125–1129. [PubMed] [Google Scholar]
- 14.Ji ZZ, Wang YX, Chen X, Wu T. Peripancreatic artery ligation and artery infusion chemotherapy for advanced pancreatic carcinoma. Chin Med J. 2003;116:89–92. [PubMed] [Google Scholar]
- 15.Shamseddine AI, Khalifeh MJ, Mourad FH, Chehal AA, Al-Kutoubi A, et al. Comparative pharmacokinetics and metabolic pathway of gemcitabine during intravenous and intra-arterial delivery in unresectable pancreatic cancer patients. Clin Pharmacokinet. 2005;44:957–967. doi: 10.2165/00003088-200544090-00005. [DOI] [PubMed] [Google Scholar]
- 16.Hong GB, Zhou JX, Liang BL. A Clinical Study on Continuous Transarterial Infusion Chemotherapy with Gemcitabine and 5-fluorouracil in Treating Patients with Advanced Pancreatic Carcinoma. Cancer prev. 2007;33:54–56. doi: 10.7314/apjcp.2012.13.6.2669. [DOI] [PubMed] [Google Scholar]
- 17.Liu HQ, Li Y, Huang RW, Huang XP. Clinical Observation of Transarterial Infusion Chemotherapy of GP for Treatment of Advanced Pancreatic Carcinoma. Jof Bas Clin Oncol. 2008;21:479–481. [Google Scholar]
- 18.Arshad A, Al-Leswas D, Stephenson J, Metcalfe M, Dennison A. Potential applications of fish oils rich in n-3 fatty acids in the palliative treatment of advanced pancreatic cancer. Br J Nutr. 2011;106:795–800. doi: 10.1017/S0007114511003060. [DOI] [PubMed] [Google Scholar]
- 19.Bayraktar S, Rocha-Lima CM. Advanced or metastatic pancreatic cancer: molecular targeted therapies. Mt Sinai J Med. 2010;77:606–619. doi: 10.1002/msj.20217. [DOI] [PubMed] [Google Scholar]
- 20.Friess H, Langrehr JM, Oettle H, Raedle J, Niedergethmann M, et al. A randomized multi-center phase II trial of the angiogenesis inhibitor Cilengitide (EMD 121974) and gemcitabine compared with gemcitabine alone in advanced unresectable pancreatic cancer. BMC Cancer. 2006;6:285. doi: 10.1186/1471-2407-6-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gillen S, Schuster T, Meyer Zum Buschenfelde C, Friess H, Kleeff J. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med. 2010;7:e1000267. doi: 10.1371/journal.pmed.1000267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haramoto M, Kohno M, Nakajima O, Horibe T, Kiyohara M, et al. Pancreatic cancer therapy with a novel pump for controlled drug release. Oncol Rep. 2010;23:365–370. [PubMed] [Google Scholar]
- 23.Tanaka T, Yamamoto K, Sho M, Nishiofuku H, Inoue M, et al. Pharmacokinetic evaluation of pancreatic arterial infusion chemotherapy after unification of the blood supply in an animal model. J Vasc Interv Radiol. 2010;21:116–121. doi: 10.1016/j.jvir.2009.09.027. [DOI] [PubMed] [Google Scholar]
- 24.Xie YB, Wang Z, Han ZK, Li AD, Zhang ZQ, et al. Anti-tumor efficacy of interventional chemotherapy with liposomal doxorubicin for hepatic metastasis of pancreatic cancer in nude mouse model. Natl Med J China. 2010;90:2126–2129. [PubMed] [Google Scholar]
- 25.Yang M, Li JQ, Tang ZQ, Zhao P. Study on pharmacokinetics of PLGA-gemcitabine sustained-release microspheres in nude mice with pancreatic cancer. Chin Pharmaceutical J. 2010;45:295–299. [Google Scholar]
- 26.Homma H, Doi T, Mezawa S, Takada K, Kukitsu T, et al. A novel arterial infusion chemotherapy for the treatment of patients with advanced pancreatic carcinoma after vascular supply distribution via superselective embolization. Cancer. 2000;89:303–313. [PubMed] [Google Scholar]
- 27.Nakchbandi W, Muller H, Singer MV, Lohr JM, Nakchbandi IA. Prospective study on warfarin and regional chemotherapy in patients with pancreatic carcinoma. J Gastrointestin Liver Dis. 2008;17:285–290. [PubMed] [Google Scholar]
- 28.Fu D, Ni Q, Yu X, Zhang Q, Hua Y, et al. Regional intra-arterial infusion chemotherapy for pancreatic cancer: an experimental study. Natl Med J China. 2002;82:371–375. [PubMed] [Google Scholar]
- 29.Li Q, Wang MQ, Duan LX, Song P, Ao GK, et al. Regional intra-arterial infusion chemotherapy for pancreatic cancer of dogs with the mixture of lipid emulsion-cisplatin: An experimental study. Chin J Radiol. 2009;43:191–195. [Google Scholar]
- 30.Mitsutsuji M, Suzuki Y, Iwanaga Y, Fujino Y, Tanioka Y, et al. An experimental study on the pharmacokinetics of 5-fluorouracil regional chemotherapy for pancreatic cancer. Ann Surg Oncol. 2003;10:546–550. doi: 10.1245/aso.2003.07.018. [DOI] [PubMed] [Google Scholar]
- 31.Tanaka T, Yamamoto K, Sho M, Nishiofuku H, Inoue M, et al. Pharmacokinetic Evaluation of Pancreatic Arterial Infusion Chemotherapy after Unification of the Blood Supply in an Animal Model. J Vasc Interv Radiol. 2010;21:116–121. doi: 10.1016/j.jvir.2009.09.027. [DOI] [PubMed] [Google Scholar]