Abstract
Objectives
To develop a new classification method to describe incidence and prevalence of function and disability and their predictors in Chinese older adults.
Methods
Data were obtained from 16,020 older adults in the 2002 wave of Chinese Longitudinal Healthy Longevity Survey (CLHLS). The subtypes of function and disability were defined by combining physical performance (PP) tests and self-reported assessments of activities of daily living (ADL).
Results
The most prevalent subtype involved PP limitations without ADL dependency. Rural living made it more likely that an individual with physical performance limitations would be independent in ADL, whereas city residence made dependence in ADL more likely, regardless of whether performance limitations were present.
Discussion
Self-reported and performance-based tools can be used in combination to estimate conceptually different subtypes of function and disability, with different epidemiological rates of incidence and different social, medical, and environmental predictors.
Keywords: function, disability, ADL, physical performance, China
Introduction
China has the world's largest population of older adults, with 106.1 million people aged 65 or older in 2008, almost double that of India, the country with the second largest population (Kinsella & He, 2009). By 2050, China will have an estimated 459 million people over the age of 60, nearly 32% of the projected Chinese population for the same year (He, Sengupta, Zhang, & Guo, 2007). Such tremendous growth in China's older population will require a major transformation of health care systems in that country (Flaherty et al., 2007; Harwood, Sayer, & Hirschfeld, 2004; He et al., 2007; Ofstedal et al., 2007; Yin, Dai, Xiao, & Xue, 2007). In particular, higher rates of chronic health conditions and disability among older adults are likely to result in substantial economic and public health challenges for China.
Similar to most countries, including the United States, current estimates of unmet need and health service use among older adults in China rely heavily on self-reported difficulty and/or dependence with basic activities of daily living (ADL; Beydoun & Popkin, 2005; Gu & Xu, 2007; Gu & Zeng, 2004; Jiang, Tang, Meng, & Futatsuka, 2002; Liang, Liu, & Gu, 2001; Zimmer & Kwong, 2004). This approach yields a limited snapshot of the full burden of disability in China, however, as it excludes those with functional performance limitations who do not yet have dependence with basic self-care tasks. Numerous researchers have demonstrated the comparable merits of performance-based protocols, such as objectivity, sensitivity, reproducibility, and sensitivity to change (Guralnik, Branch, Cummings, & Curb, 1989; Guralnik et al., 2000, 1994; Onder et al., 2005; Studenski et al., 2003). Researchers also have acknowledged utility in the complementary usage of self-reported and performance-based assessments for characterizing severity of disability in practice (Daltroy et al., 1995; Elam et al., 1991; Kelly-Hayes, Jette, Wolf, D'Agostino, & Odell, 1992; Kempen et al., 1996; Reuben et al., 2004). More important, because physiological limitations and physical performance (PP) restrictions often precede and causally contribute to dependency in self-care (Guralnik et al., 1989, 2000, 1994; Reuben et al., 2004), a measurement framework incorporating performance-based tests may greatly benefit public health systems in countries such as China, where detecting preclinical, more modifiable health limitations has extremely important health and economic implications for vast and rapidly aging populations.
Theoretical models of disability have been evolving since the 1960s (Brandt & Pope, 1997; Nagi, 1965; National Center for Medical Rehabilitation Research [NCMRR], 1993; Pope & Tarlov, 1991; Verbrugge & Jette, 1994; World Health Organization [WHO], 1980, 2001), and a core insight of that evolution is that disability should be understood as a context-embedded outcome rather than a pure biomedical impairment. In particular, various models imply a clear boundary between disability and functional limitation, in which functional limitation refers to “individual capacity without reference to situational requirement”; in contrast, disability refers to “the expression of a functional limitation in a social context” (quoted by Verbrugge & Jette, 1994, p. 3). Such a conceptual distinction is based on the fact that nonphysiological factors such as behavioral, psychological, social, and environmental mechanisms provide alternative intervening forces that potentially cause functional limitation to progress to disability in real living situations.
Current theory also suggests that functional limitations may not necessarily directly translate into difficulties, dependencies, and inability. Disabilities experienced in daily living also may not necessarily be attributed to physiological impairments and functional limitations. As illustration, the following scenarios are possible: (a) If persons with hemiplegia have adequate mobility and assistive devices, and appropriate housing and public transportation design, they may report little dependency with indoor and outdoor mobility, though they may not be able to successfully complete basic performance-based tests; conversely, (b) older adults who score high on objective performance tests may complain of a need for assistance in personal self-care tasks such as bathing and indoor transferring simply due to a lack of household electricity, lighting, and/or personal shower facilities. This could be especially true in developing societies. More intriguingly, it is possible that persons with minor or modest functional limitations could report more or less dependency based purely on whether resources of social support are more or less available or easier to access.
Self-reported and performance-based measurements reflect two of the main components discussed in the above disability models. Combined use of the two types of measures and the creation of new subtypes of function and disability has potential to advance our understanding of the intrinsic structure and transition of disability and associated mechanisms, potentially providing more informative prevalence and incidence data for intervention and policy making.
Theoretically projected inconsistencies between functional limitations and self-reported disability provide a basis for researchers to investigate and characterize functionally limited people who report low levels of disability and, similarly, to describe people reporting disability who have low levels of functional limitation. Investigation of the prevalence and incidence of these special subtypes of function and disability and exploration of factors associated with each should be valuable. For example, although many previous studies have identified determinants of disability, it might be more desirable to clarify those factors that help delay or prevent disability in people who already have functional limitation. It is also valuable to know why certain people with disabilities have few functional limitations and could help to identify nonphysiological and/or modifiable factors contributing to dependence. More specific information about these disability subtypes could ultimately help to tailor intervention and policy.
This study is the first population-based study to examine these specific questions with a focus on China as the country hosting the largest older adult population in the world. In this study, we combined self-reported and observed measurements to identified those with (a) isolated functional restrictions as measured by PP testing, (b) isolated self-care restrictions as measured by basic ADL limitations, and (c) those with combined limitations in PP and self-care. We then characterized the prevalence and incidence of these mutually exclusive subtypes of function and disability and examined predictors of 3-year incidence for these subtypes.
Method
Study Design
Our data came from a nation-wide survey in China, the Chinese Longitudinal Healthy Longevity Survey (CLHLS), including 631 counties/cities randomly selected from 22 of 31 provinces, and representative of 85% of the population. The survey's design has been described in previous studies, and data quality was reported as good (Gu, 2008; Zeng, 2008). The baseline data in this study were the third wave of CLHLS in 2002. We choose the 2002 wave as baseline because it was the first wave in CLHLS to include older adults aged 65 to 79. Table 1 shows the sampling structure of the baseline data: The 2002 sample included survivors of the baseline sample (age 80+) who first entered the study in 1998 (n = 2,642), survivors from participants enrolled in 2000 (age 80+; n =3,674), and 9,704 participants (age 65+) added in 2002. All available participants were reinterviewed in 2005.
Table 1.
Sampling Structure of the 2002 CLHLS (Chinese Longitudinal Healthy Longevity Survey) Data
| Follow-up years |
|||
|---|---|---|---|
| 1998 | 2000 | 2002 | |
| Entry cohort | |||
| 1998 | New: 9,093 | Alive: 4,831 [Died: 3,368] [Lost: 894] |
Alive: 2,642 [Died: 1,604] [Lost: 585] |
| 2000 | New: 6,368 | Alive: 3,674 [Died: 1,739] [Lost: 956] |
|
| 2002 | New: 9,704 | ||
| Sample size | 9,093 | 11,199 | 16,020 |
To examine incidence of subtypes of function and disability, we included all participants who were free of both self-reported and performance-based limitations in 2002 and evaluated incidence of different subtypes at the 2005 follow-up. Missing values were not imputed in our statistical analyses in that the nonresponse rates, both at the unit level and item level, are low.
Variables
PP tests included (a) standing from a chair without using hands, (b) lifting a book from the floor, and (c) turning 360°. Individuals who were unable to perform one or more of these tasks independently were determined to have a PP limitation. We examined six self-reported self-care ADLs (bathing, dressing, toileting, transfers, continence, and feeding). Individuals reporting dependence with one or more ADL tasks were considered to have an ADL dependency.
Four mutually exclusive subtypes of function and disability were identified. First, those with no limitations in PP limitations or ADL tasks constituted the reference group (Subtype 0). Next, PP and ADL items were cross-classified to place individuals into one of three remaining subtypes: Subtype 1: those with observed PP limitations but no self-reported dependence with ADL items; Subtype 2: those with self-reported dependence with ADL items but no observed PP limitations; Subtype 3: those with both self-reported dependence for ADL items and observed PP limitations.
In analyses, we have included major covariates previously reported to be associated with health in later life, especially with disability of older adults (e.g., Feinglass et al., 2007; Ferrucci et al., 2003; Liang, Bennett, Sugisawa, Kobayashi, & Fukaya, 2003; Zeng, Gu, & Land, 2007). Gender, ethnicity (Han vs. other), age (years), living environment (urban, town, or rural residence), living arrangements (with household members, institutionalized, or alone), education (years), and previous year household income per capita (yuan) were included. A four-question index of social support (range 0–12) was based on the type of person most frequently consulted about (1) daily activities, (2) general concerns, (3) illness, or (4) seeking help with problems/difficulties. This index captured social ties that can be mobilized by an individual when instrumental and emotional support is needed. Responses were scored for household member or relative (3 points), friend or neighbor (2 points), social worker/nurse (1 point), or nobody (0 point). Cognitive status was assessed using the Chinese version of the Mini-Mental State Examination (MMSE; range = 0–30; Zeng & Vaupel, 2002). Depression was screened with a 5-item index of depression symptoms (score 0–5), and comorbidity was recorded as a count of 23 potential medical conditions such as hypertension, diabetes, heart diseases, and stroke/cerebrovascular diseases, and so on. Proxy reports often are applied in surveys of older adults to control bias in favor of healthy people (Rodgers & Herzog, 1992). We included a variable indicating the proxy status for the self-reported disability, and the proxy rate of the CLHLS is within normal range in comparison with other investigations on older adults (Gu, 2008).
Statistical Analysis
Proportions were examined for categorical variables and means and standard deviations for continuous variables. Frequency data for PP and ADL tasks were examined separately by age (age 65–79 vs. age 80+). Due to the nonrandom sampling scheme, prevalence statistics are reported with weighting for age, gender, and rural/urban residence (Chinese Longitudinal Healthy Longevity Survey Research Team, 2000). Multinomial logistic regression was used to estimate prevalence and incidence odds ratios for predictor variables for each of three different subtypes of function and disability, using persons with neither ADL dependency nor PP limitations (Subtype 0) as the reference group. Weighting method, however, was not used in regression given that inclusion of variables related to sampling selection produces unbiased coefficients without weights (Winship & Radbill, 1994) and that weighted regression results are likely to enlarge the standard errors (Hendrikx, 2002). We used Stata/SE 10.0 (StataCorp LP, College Station, Texas).
Results
Characteristics of the Baseline Sample (Weighted Results)
As can be seen in Table 2, the average age was 72.5 years. Approximately 47% were male, 94% were of Han ethnicity, and the majority lived in rural areas (65.0%). Most of them lived with their families (85.0%). Participants had an average of 2.6 years formal education, and previous year household income per capita was about 3,000 yuan. The average social support score was 11.0 (SD = 1.9), and mean MMSE score was 22.2. In general, depressive symptoms were minimal (0.7, SD = 0.9), and interviewees had, on average, 1.2 comorbidities (SD = 1.3).
Table 2.
Descriptive Statistics
| Percentage/mean (SD) | Weighted result | |
|---|---|---|
| Proxy (%) | 29.8 | 5.5 |
| Gender (female, %) | 57.4 | 53.0 |
| Age (year) | 86.4 (11.7) | 72.5 (6.1) |
| Ethnicity (non-Han, %) | 5.6 | 5.8 |
| Living environment | ||
| Living in urban area (%) | 24.0 | 19.2 |
| Living in town area (%) | 22.0 | 15.8 |
| Living in rural area (%) | 54.0 | 65.0 |
| Living arrangement | ||
| Living with family (%) | 81.9 | 85.0 |
| Living in institution (%) | 4.6 | 2.4 |
| Living alone | 13.5 | 12.6 |
| Social support (range = 0–12) | 10.7 (2.3) | 11.0 (1.9) |
| Education (year) | 2.0 (3.5) | 2.6 (3.7) |
| Income (10,000 yuan) | 0.3 (0.4) | 0.3 (0.3) |
| MMSE (range = 0–30) | 17.8 (7.7) | 22.2 (4.0) |
| Depression symptom (range = 0–5) | 0.7 (1.0) | 0.7 (0.9) |
| Comorbidity | 1.2 (1.4) | 1.2 (1.3) |
Prevalence of PP and ADL Limitations
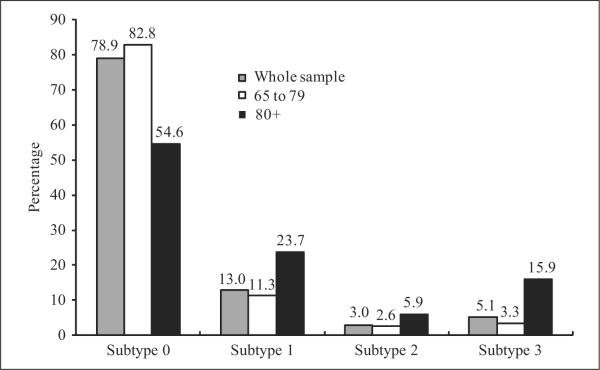
In 2002, approximately 8% of the Chinese older adults had limitations with turning 360°, whereas 9.4% and 11.6% had limitations in picking up a book from the floor and standing from a chair, respectively (Figure 1). Much lower levels of ADL dependency were reported (1.4% to 2.3% reported dependency for feeding, continence, transfers, toileting, and dressing) with the exception of bathing dependency (6.7%). Overall, 8.1% reported one or more limitations in ADL, whereas 18.1% were found to have one or more PP limitations. Relative patterns of prevalence were similar among those aged 80+ in comparison to adults aged 65 to 79 and with the overall cohort, though rates were much higher among older adults aged 80+ for any given type of ADL or PP limitation.
Figure 1.
Prevalence of ADL (activities of daily living) disability and PP (physical performance) limitations in 2002
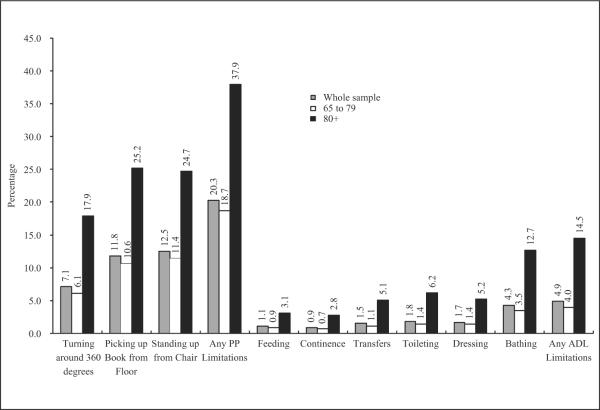
Prevalence of Disability Subtypes
As can be seen in Figure 2, almost 79% of all participants had neither observed PP nor self-reported ADL limitations (Subtype 0); approximately 21% had one of the three subtypes. Similar prevalence was observed in the age group of 65 to 79 when we stratified by age, but among 80+ older adults, 45.4% had one of the 3 disability subtypes. By far the most prevalent disablement pattern was Subtype 1 (~13% of participants), that is, limitation in PP but not in ADL. Subtype 3 (limitation in both PP and ADL) was present in 5.1% of the Chinese older adult population, and Subtype 2 (limitation in ADL but not in PP) was the least prevalent subtype (3.0%).
Figure 2.
Prevalence of the four disability subtypes in 2002
Note: Subtype 0 = No physical performance (PP) limitation, no ADL (activities of daily living) disability; Subtype 1 = PP limitation, no ADL disability; Subtype 2 = ADL disability, no PP limitations; and Subtype 3 = PP limitation and ADL disability
Factors Associated With the Prevalence of Disability Subtypes
Column 1 of Table 3 shows that female gender, age, non-Han minority, depression symptom, and comorbid illnesses all increased the risk of having PP limitation but no ADL dependency (Subtype 1), whereas higher cognitive function and more education were protective. Interestingly, rural living (vs. urban residence) dramatically increased risk of being in the Subtype 1 disability in comparison with the reference group with no PP and ADL limitations (Subtype 0).
Table 3.
Odds Ratios of Prevalent Disability Subtypes
| Subtype 1† OR (95% CI) | Subtype 2† OR (95% CI) | Subtype 3† OR (95% CI) | |
|---|---|---|---|
| Proxy | 1.25**[1.09, 1.44] | 2.33**[1.92, 2.83] | 2.63**[2.29, 3.02] |
| Gender (female) | 1.19**[1.07, 1.32] | 1.34**[1.12, 1.59] | 1.34**[1.18, 1.52] |
| Age | 1.07**[1.06, 1.07] | 1.07**[1.06, 1.08] | 1.12**[1.11, 1.13] |
| Ethnicity (non-Han) | 1.17 [0.97, 1.41] | 0.57**[0.38, 0.86] | 0.47**[0.36, 0.62] |
| Living Environment‡ | |||
| Living in Town | 1.15 [0.99, 1.34] | 0.48**[0.38, 0.60] | 0.67**[0.57, 0.80] |
| Living in Rural | 1.27**[1.10, 1.46] | 0.46**[0.37, 0.56] | 0.65**[0.55, 0.75] |
| Living Arrangement§ | |||
| Living in Institution | 1.13 [0.86, 1.47] | 1.13 [0.72, 1.77] | 1.01 [0.74, 1.38] |
| Living Alone | 0.92 [0.80, 1.06] | 0.57**[0.43, 0.75] | 0.57**[0.47, 0.68] |
| Social Support | 0.99 [0.97, 1.02] | 1.06*[1.02, 1.12] | 1.04*[1.01, 1.07] |
| Education (year) | 0.98**[0.96, 0.99] | 1.00 [0.98, 1.03] | 1.02 [1.00, 1.04] |
| Income (per 10,000 yuan) | 0.97 [0.82, 1.13] | 0.97 [0.76, 1.23] | 1.33**[1.12, 1.58] |
| MMSE | 0.91**[0.90, 0.92] | 0.94**[0.92, 0.96] | 0.86**[0.85, 0.87] |
| Depression Symptom | 1.27**[1.21, 1.34] | 1.18**[1.09, 1.29] | 1.51**[1.42, 1.60] |
| Comorbidity | 1.22**[1.17, 1.27] | 1.32**[1.24, 1.39] | 1.45**[1.39, 1.51] |
| R2 = .22−Log likelihood = 12403.5 |
p<0.05;
p<0.01.
The reference group is Subtype 0 = No physical performance limitation, no ADL disability; Subtype 1 = Physical performance limitation, no ADL disability; Subtype 2 = ADL disability, no physical performance limitations; Subtype 3 = Physical performance limitation and ADL disability
The reference group is living in urban areas.
The reference group is living with household member.
Sociodemographic and medical covariates had a similar impact on all subtypes in comparison to the reference group, with a few important exceptions. Notably, city living made it more likely that an individual without PP limitations would have ADL dependency (Subtype 2); in fact, urban residence made it more likely that someone would have ADL dependency, regardless of whether PP limitations were present or not (Subtypes 2 and 3). Non-Han ethnicity was associated with a decreased probability to be classified as Subtype 2 and 3. Another major difference in the associates of the three different subtypes was that living with household members substantially increased the probability of having ADL dependency, regardless of whether PP restrictions were present (see protective OR's for living alone for Subtypes 2 and 3); living arrangements were not significantly associated with Subtype 1. Higher income increased the probability of reporting ADL dependence when PP limitations were present (Subtype 3).
Three-Year Incidence of Disability Subtypes
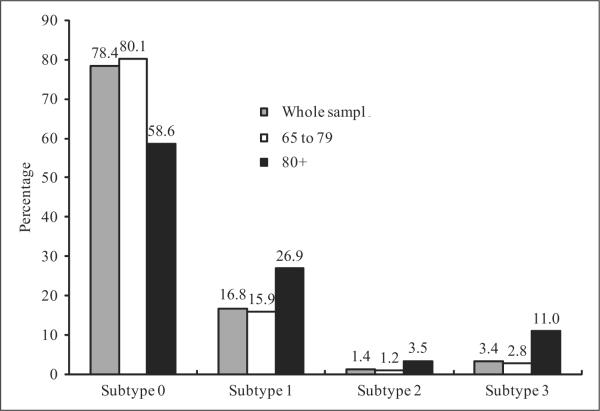
At baseline, 7,649 individuals were free of any type of disability, and over the follow-up period of 3 years, 12.7% were lost to follow-up, 20.1% died, and 67.2% survived (i.e., 5141 cases), who were eligible to be included in the incidence sample. Figure 3 shows 3-year incidence proportions for PP and ADL limitations. Patterns of incident disability for specific tasks were grossly similar to baseline prevalence, with ~5% of the Chinese older adult population and ~14% in the oldest age group reporting new ADL disability. Bathing limitations occurred most frequently; other ADL disabilities occurred at much lower rates. Incidence rates of PP limitation were far greater than those of new ADL limitations and that was especially true for the oldest age group.
Figure 3.
Incident ADL (activities of daily living) disability and PP (physical performance) limitations, 2002 to 2005
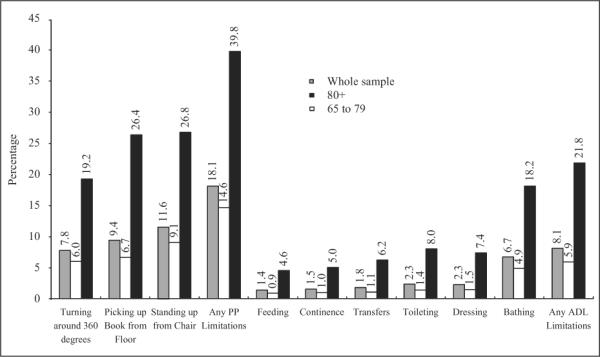
The majority of older adult Chinese remained free of any ADL or PP limitations at 3 years of follow-up (Figure 4). Incidence was highest for sole occurrence of PP limitations (Subtype 1 = 16.8%) and markedly lower for concurrent incidence of PP and ADL (Subtype 3 = 3.5%) and for limitations in ADL without accompanying PP limitations (Subtype 2 = 1.4%). The overall pattern of incidence among the subtypes was similar for younger (aged 65 to 79) and older (aged 80+) age groups, but disability of the older age group was much more prevalent.
Figure 4.
Incidence of the four disability subtypes, 2002 to 2005
Note: Subtype 0 = No physical performance (PP) limitation, no ADL (activities of daily living) disability; Subtype 1 = PP limitation, no ADL disability; Subtype 2 = ADL disability, no PP limitations; and Subtype 3 = PP limitation and ADL disability.
Predictors of Incident Disability Subtypes
Patterns of predictors for the incidence data were similar to the prevalence data (tabular data available upon request), but the much smaller sample of the incidence cohort resulted in fewer statistically significant results. The major difference was that living in an institution significantly increased the incidence of Subtype 1 and 3, but the effect was not significant for prevalence of these subtypes. Overall, however, the general patterns of association paralleled prevalence results, including the adverse impact of urban (vs. rural) residence on incidence of disability.
Discussion
Previous work suggests that self-reported and performance-based tools can be used together to refine the classification of function and disability in older adults (Reuben et al., 2004). In this study, we have shown how self-reported and performance-based tools can be used in combination to estimate conceptually different subtypes of function and disability in Chinese older adults, with different epidemiological rates of incidence and different social, medical, and environmental predictors. Second, our work characterizes distinct subtypes that have not been reported in representative samples of older adults. Sample sizes in the current study were large enough to allow for predictive and controlled estimation of the impact of associates and predictors on prevalent and incident subtypes. Previous efforts at characterizing specific disability subtypes have been limited by sample sizes, which precluded full adjustment for potential confounding and estimation of meaningful predictors within different disability strata. For example, the condition of having self-reported limitations in ADL in the absence of PP limitations was previously reported to be “clinically irrelevant” (Reuben et al., 2004). Our sample was large enough to show that, though this type of disability is indeed rare, in China it is nevertheless a meaningful disability classification group with potentially different predictors compared to healthier individuals and those with other subtypes of functional limitations and disabilities.
The prevalence and incidence of different subtypes of function and disability observed in this study deserves special attention given the large size and rapid growth of the older adult population in China. In general, markedly higher rates of subtypes with functional limitation or disability were observed in the fastest-growing oldest age group (those aged 80+), where 45.4% experienced a prevalent subtype and 39.4% incurred an incident subtype over a 3-year period. It is also striking that the greatest prevalence and incidence was observed for the less severe subtype, that is, Subtype 2, and that increases in disability rates with age were greater for new dependency as opposed to new PP limitations. It is thus possible that earlier identification and intervention development targeted at the less severe subtype may effectively decrease the overall population burden of disability. The fact that self-reported dependency was much higher than performance-based limitations in the older age group (80+) could be partly explained by some characters in the Chinese older adult caring culture: Chinese people older than 80 are often regarded as frail, and household members are morally expected to pay more attentions and offer more assistance for piety concerns. Therefore, proper lifestyle education may help the oldest old group (80+) to maintain independence longer, benefitting both the older adults and their caregivers.
Overall, our findings could be as important in the United States as in China, as both countries have a rapidly aging population and most projected service need, caregiver burden, and older adult active life expectancy rely exclusively on the more traditional self-reported ADL assessments. Someone who has PP limitations but is still independent with self-care activities represents someone who likely is less costly for the health care system and possibly represents ideals espoused by many older adults to remain independent. On the other hand, an individual without PP limitations yet reporting dependency in self-care may indicate situations where physical and sociocultural environments may promote dependency despite fairly good physical abilities or undetected yet potentially treatable sensory or psychological health conditions exist that cause disability.
The subtypes identified in this study may help us to better understand the inconsistencies between functional limitations and self-reported disabilities as has been acknowledged in current disability models. This new classification of function and disability are based on the rationale underpinning WHO/ICF (International Classification of Functioning, Disability, and Health) disability classification models, that is, that disability cannot be fully characterized by focusing on an individual's physical limitations, but must be considered with regard to different social and environmental contexts (WHO, 2001). Moreover, our findings challenge the often-assumed notion that development of dependency in self-care has to occur via functional limitation. Our results suggest that various contextual factors may disturb such a pathway and it is likely that at least some people reporting dependency may not have any major physical limitation. This new classification may provide new opportunities to better explore “modifying factors” (Verbrugge & Jette, 1994) or “contextual factors” (WHO, 2001) in established disability models.
One novel and important finding in this study was that different cultural, social, and environmental factors in rural and urban regions of China were associated with different subtypes of function and disability. Rural residence promoted independence in ADLs even when performance limitations were present, whereas city residence increased the risk of reported dependence even when performance limitations were absent. Although specific aspects of rural-urban differences were not investigated in details here, there may be physical and/or sociocultural characteristics of Chinese rural environments that lead individuals to report less dependency in the face of physical limitations. For instance, the less polluted environment and the lifestyle of agricultural production may encourage more physical activities among these older adults so that the dependence was delayed or avoided; lack of public transportation system or walking-assistance facility may make rural older adults more adaptive to keep independent in mobility, though they have developed certain physical limitations; the huge immigration of young rural workers into urban areas often leaves many older adults living without enough social support and, thus, force them to remain independent; and the underdeveloped socioeconomic and medical conditions in the Chinese rural regions may lower expectation of life quality for local older adults and reduce their reports of dependency when physical limitation is present. A more delicate issue is that urban Chinese older adults may actually tend to report dependency as a marker of “successful aging.” Whereas Western standards of successful aging often emphasize the capacity to maintain functional independence, many Chinese older adults may view dependence on their families and their families' “willingness to meet their needs” as a sign of successful aging (Torres, 1999).
The effect of urban residence on old age dependency may have serious implications for China. Urban populations worldwide are growing at a faster rate than rural residents, but particularly in China because of rapid urbanization and large rural-urban migration (Shen, Feng, & Wong, 2006; Zhang & Song, 2003), which by the end of 2008 will cause the urban population growth in China to equal the total population growth in this country throughout recorded history (United Nations Population Fund, 2007). Overcrowding, poverty, greater levels of pollution or environments that preclude safe recreation and/or physical activity have all been proposed as possible explanations for why city residence might promote dependency in aging (Feng, Purser, Zhen, & Duncan, 2011; United Nations Population Fund, 2007; Zeng, Gu, Purser, & Hoenig, 2007). There could alternatively be substantial unmet needs in rural environments if the low self-reported dependence in ADLs is not due to better health per se but due to inadequate resources available to allow physically limited individuals to depend on others or on equipment for assistance. Further research on the natural history of these disability subtypes is needed to better understand their meaning and impact.
This study had several limitations. First, although it provides useful data on the current population prevalence and short-term incidence of disability, causal effects of the disability subtypes on important health outcomes need to be determined. An additional limitation is that the study sample was characterized by survivors as well as new participants from previous waves of CLHLS. Although comprehensive in terms of geographical coverage, the sample it is not a random sample of the Chinese population. Nevertheless, based on our weighted estimates, the relative ordering of prevalence rates for individual tasks (e.g., high rates of bathing disability compared to other ADL tasks) appears comparable to representative samples in other countries. We believe these weighted estimates give the most representative and detailed estimates to date of old-age disablement in China. Next, though our incidence study covered a period as long as 3 years, we are still unable to collect information on all possible episodes of disability transitions during this period, which may bring some bias in our estimation. Moreover, only the transition toward functional limitation and disability has been discussed in the article, not the other way around. In addition, the three performance tests used in this study primarily target motor skills. It is possible that other performance-based tests that target function of other organ systems such as cardiopulmonary and sensory functions would provide additional value in the classification of disability.
In conclusion, this study provides important and unique data identifying subtypes of function and disability that appear to represent clinically distinct entities and also provide critical support for the disability model with regard to the inconsistencies between functional limitations and self-reported disability. We believe the use of performance tools in combination with the more traditional self-reported tools may help to better understand and risk-stratify substantively different and clinically relevant disablement groups, especially at potentially earlier stages of limitation (e.g., Subtypes 1 and 2)—when sub-type-specific interventions could be particularly effective at preventing dependency and reducing personal and public health costs in this rapidly growing sector of the Chinese, and world, population.
Acknowledgments
Funding The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a grant from the Provost Common Fund of Duke University, Duke's NIH/NIA Claude D. Pepper Older Americans Independence Center Grant 5P60AG11268, NIH Grant K01HD049593 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development, and a pilot grant from Duke University's Global Health Institute. The data analyzed were originally collected as part of the Chinese Longitudinal Healthy Longevity Survey (CLHLS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health.
Footnotes
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Reference
- Beydoun MA, Popkin BM. The impact of socio-economic factors on functional status decline among community-dwelling older adults in China. Social Science and Medicine. 2005;60:2045–2057. doi: 10.1016/j.socscimed.2004.08.063. [DOI] [PubMed] [Google Scholar]
- Brandt EN, Pope AM. Enabling America: Assessing the role of rehabilitation science and engineering. National Academy Press; Washington, DC: 1997. [PubMed] [Google Scholar]
- Chinese Longitudinal Healthy Longevity Survey Research Team Chapter 5: Weighting method. 2000 Retrieved from http://www.geri.duke.edu/china_study/Weighting%20method.pdf.
- Daltroy LH, Philips CB, Eaton HM, Larson MG, Partridge AJ, Logigian M, Liang MH. Objective measuring physical ability in elderly persons: The physical capacity evaluation. American Journal of Public Health. 1995;85(4):558–560. doi: 10.2105/ajph.85.4.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elam JT, Craney MJ, Beaver T, El Derwi D, Applegate WB, Miller ST. Comparison of subjective ratings of function with observed functional ability of frail older persons. American Journal of Public Health. 1991;81(9):1127–1130. doi: 10.2105/ajph.81.9.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinglass J, Lin S, Thompson J, Sudano J, Dunlop D, Song J, Baker DW. Baseline health, socioeconomic status, and 10-year mortality among older middle-aged Americans: Findings from the Health and Retirement Study, 1992–2002. Journal of Gerontology: Social Sciences. 2007;62(4):209–217. doi: 10.1093/geronb/62.4.s209. [DOI] [PubMed] [Google Scholar]
- Feng Q, Purser JL, Zhen Z, Duncan PW. Less exercise and more TV in modernization: Trend of physical activity in Shanghai elder, 1998 to 2008. Journal of Public Health. 2011;33(4):543–550. doi: 10.1093/pubmed/fdr031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrucci L, Turchi A, Fumagallo S, Di-Bari M, Silvestrini G, Zacchei S, Marchionni N. Sex-related differences in the length of disability prior to death in older persons. Aging Clinical Experimental Research. 2003;15(4):310–314. doi: 10.1007/BF03324515. [DOI] [PubMed] [Google Scholar]
- Flaherty JH, Liu M, Ding L, Dong B, Ding Q, Li X, Xiao S. China: The ageing giant. Journal of the American Geriatrics Society. 2007;55(8):1295–1300. doi: 10.1111/j.1532-5415.2007.01273.x. [DOI] [PubMed] [Google Scholar]
- Gu D. General data assessment of the Chinese Longitudinal Healthy Longevity Survey in 2002. In: Zeng Y, Poston DL, Vlosky DA, Gu D, editors. Healthy longevity in China: Demographic, socioeconomic, and psychological dimensions. Springer; Dordrecht, Netherlands: 2008. pp. 39–59. [Google Scholar]
- Gu D, Xu Q. Sociodemographic effects on the dynamics of task-specific ADL functioning at the oldest-old ages: The case of China. Journal of Cross-Culture Gerontology. 2007;22(1):61–81. doi: 10.1007/s10823-006-9024-0. [DOI] [PubMed] [Google Scholar]
- Gu D, Zeng Y. Sociodemographic effects on the onset and recovery of ADL disability among Chinese oldest-old. Demographic Research. 2004;11:1–42. [Google Scholar]
- Guralnik JM, Branch LG, Cummings SR, Curb JD. Physical performance measures in ageing research. Journals of Gerontology: Medical Sciences. 1989;44(5):141–146. doi: 10.1093/geronj/44.5.m141. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Pieperet CF, Leveille SG, Markides KS, Ostir GV, Wallace RB. Lower extremity function and subsequent disability: Consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. Journal of Gerontology: Medical Sciences. 2000;55:221–231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Wallace RB. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journals of Gerontology: Medical Sciences. 1994;49(2):85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Harwood RH, Sayer AA, Hirschfeld M. Current and future worldwide prevalence of dependency, its relationship to total population, and dependency ratios. Bulletin of the World Health Organization. 2004;82(4):251–258. [PMC free article] [PubMed] [Google Scholar]
- He W, Sengupta M, Zhang K, Guo P. U.S. Census Bureau, international population reports, P95/07-2: Health and health care of the older population in urban and rural China: 2000. U.S. Government Printing Office; Washington, DC: 2007. [Google Scholar]
- Hendrikx J. The impact of weights on standard errors. Presented at the Annual Meeting of the Association for Survey Computing; 2002, April 17; London, UK: Imperial College; [Google Scholar]
- Jiang J, Tang Z, Meng XJ, Futatsuka M. Demographic determinants for change in activities of daily living: A cohort study of the elderly people in Beijing. Journal of Epidemiology. 2002;12(3):280–286. doi: 10.2188/jea.12.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly-Hayes M, Jette AM, Wolf PA, D'Agostino RB, Odell PM. Functional limitation and disability among elders in the Framingham study. American Journal of Public Health. 1992;82(6):841–845. doi: 10.2105/ajph.82.6.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempen GI, van Heuvelen MJ, van den Brink RH, Kooijman AC, Klein M, Houx PJ, Ormel J. Factors affecting contrasting results between self-reported and performance-based levels of physical limitations. Age and Ageing. 1996;25:458–464. doi: 10.1093/ageing/25.6.458. [DOI] [PubMed] [Google Scholar]
- Kinsella K, He W. U.S. Census Bureau, international population reports, P95/09-1: An ageing world: 2008. U.S. Government Printing Office; Washington, DC: 2009. [Google Scholar]
- Liang J, Bennett J, Sugisawa H, Kobayashi E, Fukaya T. Gender differences in old age mortality: Roles of health behavior and baseline health status. Journal of Clinical Epidemiology. 2003;56:572–82. doi: 10.1016/s0895-4356(03)00060-x. [DOI] [PubMed] [Google Scholar]
- Liang J, Liu X, Gu SZ. Transitions in functional status among older people in Wuhan, China: Socioeconomic differentials. Journal of Clinical Epidemiology. 2001;54:1126–1138. doi: 10.1016/s0895-4356(01)00390-0. [DOI] [PubMed] [Google Scholar]
- Nagi S. Some conceptual issues in disability and rehabilitation. In: Sussman M, editor. Sociology and rehabilitation. American Sociological Association; Washington, DC: 1965. pp. 100–113. [Google Scholar]
- National Center for Medical Rehabilitation Research . Research plan for the National Center for Medical Rehabilitation Research. Author; Rockville, MD: 1993. [Google Scholar]
- Ofstedal MB, Zimmer Z, Hermalin AI, Chan A, Chuang Y, Natividad J, Tang Z. Short-term trend in functional limitation and disability among older Asians: A comparison of five Asian settings. Journal of Cross-Culture Gerontology. 2007;22:243–261. doi: 10.1007/s10823-006-9025-z. [DOI] [PubMed] [Google Scholar]
- Onder G, Penninx BW, Ferrucci L, Fried LP, Guralnik JM, Pahor M. Measures of physical performance and risk for progressive and catastrophic disability: Results from the Women's Health and Aging Study. Journal of Gerontology: Medical Sciences. 2005;60(1):74–79. doi: 10.1093/gerona/60.1.74. [DOI] [PubMed] [Google Scholar]
- Pope AM, Tarlov AR. Disability in America: Toward a national agenda for prevention. National Academy Press; Washington, DC: 1991. [Google Scholar]
- Reuben DB, Seeman TE, Keeler E, Hayes RP, Bowman L, Sewall A, Guralnik JM. Refining the categorization of physical functional status: The added value of combining self-reported and performance-based measures. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2004;59(10):1056–1061. doi: 10.1093/gerona/59.10.m1056. [DOI] [PubMed] [Google Scholar]
- Rodgers WL, Herzog AR. Collecting data about the oldest: Problems and procedures. In: Suzman RM, Willis DP, Manton KG, editors. The oldest old. Oxford University Press; New York, NY: 1992. pp. 135–156. [Google Scholar]
- Shen JF, Feng ZQ, Wong KY. Dual-track urbanization in a transitional economy: The case of Pearl River Delta in South China. Habitat International. 2006;30(3):690–705. [Google Scholar]
- Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, Guralnik JM. Physical performance measures in the clinical setting. Journal of the American Geriatrics Society. 2003;51(3):314–322. doi: 10.1046/j.1532-5415.2003.51104.x. [DOI] [PubMed] [Google Scholar]
- Torres S. A culturally relevant theoretical framework for the study of successful ageing. Ageing and Society. 1999;19(1):33–51. [Google Scholar]
- United Nations Population Fund State of world population 2007: Unleashing the potential of urban growth. 2007 Retrieved from http://www.unfpa.org/swp/
- Verbrugge LM, Jette AM. The disablement process. Social Science & Medicine. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Winship C, Radbill L. Sampling weights and regression analysis. Sociological Methods Research. 1994;23:230–257. [Google Scholar]
- World Health Organization . International classification of impairment, disability and handicap. Author; Geneva, Switzerland: 1980. [Google Scholar]
- World Health Organization . International classification of functioning, disability and health: ICF. Author; Geneva, Switzerland: 2001. [Google Scholar]
- Yin Z, Dai H, Xiao Z, Xue H. A research study into the requirement of disabled residents for rehabilitation service in Beijing. Disability and Rehabilitation. 2007;29(10):825–833. doi: 10.1080/09638280600919657. [DOI] [PubMed] [Google Scholar]
- Zeng Y. Introduction to the Chinese Longitudinal Healthy Longevity Survey. In: Zeng Y, Poston DL, Vlosky DA, Gu D, editors. Healthy longevity in China: Demographic, socioeconomic, and psychological dimensions. Springer; Dordrecht, Netherlands: 2008. pp. 23–37. [Google Scholar]
- Zeng Y, Gu D, Land KC. The association of childhood socioeconomic conditions with healthy longevity at the oldest-old ages in China. Demography. 2007;44(3):497–518. doi: 10.1353/dem.2007.0033. [DOI] [PubMed] [Google Scholar]
- Zeng Y, Gu D, Purser J, Hoenig H. Effects of environmental factors on healthy longevity in China. Gerontologist. 2007;47:560. [Google Scholar]
- Zeng Y, Vaupel JW. Functional capacity and self-evaluation of health and life of the oldest-old in China. Journal of Social Issues. 2002;58:733–748. [Google Scholar]
- Zhang KH, Song SF. Rural-urban migration and urbanization in China: Evidence from time-series and cross-section analyses. China Economic Review. 2003;14:386–400. [Google Scholar]
- Zimmer Z, Kwong J. Socioeconomic status and health among older adults in rural and urban China. Journal of Aging and Health. 2004;16(1):44–70. doi: 10.1177/0898264303260440. [DOI] [PubMed] [Google Scholar]