Abstract
Objectives
Motor vehicle collisions (MVCs) are the second most common cause of non-fatal injury among U.S. adults age 65 years and older. However, the frequency of emergency department (ED) visits, disposition, pain locations, and pain severity for older adults experiencing MVCs have not previously been described. The authors sought to determine these characteristics using information from two nationally representative data sets.
Methods
Data from the 2008 Healthcare Cost and Utilization Project Nationwide Emergency Department Sample (NEDS), and the National Hospital Ambulatory Medical Care Survey (NHAMCS), were used to estimate MVC-related ED visits and ED disposition for patients 65 years and older. NHAMCS data from 2004 through 2008 were used to further characterize MVC-related ED visits.
Results
In 2008, the NEDS contained 28,445,564 patient visits, of which 760,356 (2.7%) were due to MVCs. The NHAMCS contained 34,134 patient visits, of which 1,038 (3.0%) were due to MVCs. National estimates of MVC-related ED visits by patients 65 years and older in 2008 are 226,000 (95% CI = 210,000 to 240,000), for NEDS and 270,000 (95% CI = 185,000 to 355,000) for NHAMCS. Most older adults with MVC-related ED visits were sent home from the ED (proportion discharged NEDS 78%, 95% CI 78% to 79%; NHAMCS 77%, 95% CI 66% to 86%). During the years 2004 through 2008, of MVC-related ED visits by older adults not resulting in hospital admission, moderate or severe pain was reported in 61% (95% CI = 52% to 70%) of those with recorded pain scores. Older patients sent home after MVC-related ED visits were less likely than younger patients to receive analgesics (35%, 95% CI 26% to 43% vs. 47%, 95% CI 44% to 50%) during their ED evaluations, or as discharge prescriptions (52%, 95% CI 41% to 62% vs. 65%, 95% CI = 61% to 68%).
Conclusions
In 2008, adults age 65 years or older made more than 200,000 MVC-related ED visits. Approximately 80% of these visits were discharged home from the ED, but the majority of discharged patients reported moderate or severe pain. Further studies of pain and functional outcomes in this population are needed.
INTRODUCTION
Injuries are a growing and under-recognized problem among older adults in the United States.1,2 Older women have replaced young men as the demographic group most frequently hospitalized due to injury, and the Medicare cost of injuries among individuals age 65 or older now exceeds $8 billion annually.3–5 Motor vehicle collisions (MVCs) are the most common cause of fatal injury in older adults, and are second only to falls as a cause of non-fatal injury.1 The high rate of MVC-related injury in older adults reflects in part a higher rate of police-reported and fatal crashes in adults 65 or older as compared to younger adults.6 As a result of projected growth in the population of older adults and an increase in the number of miles driven, older adult involvement in police-reported crashes is projected to double between 2010 and 2030.6
Although outcomes for older adults experiencing MVCs requiring trauma center admission have been described,7 less is known about outcomes for older adults seeking ED evaluation after MVCs but not requiring hospital admission (so-called “minor” MVC patients). This population is important because persistent pain and disability are well-documented sequelae after minor MVCs in younger adults,8,9 and available data suggest that these outcomes are likely to be even more common and disabling in older adults.8,10–13 A description of the epidemiology of minor MVCs in older U.S. adults would provide a better understanding of the potential effect of such MVCs on the health of this large and growing population.
Two nationally representative data sets contain the necessary information to describe the epidemiology of minor MVCs in older U.S. adults: the Healthcare Cost and Utilization Project (HCUP) Nationwide Emergency Department Sample (NEDS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS). Other nationally representative data sets characterize EDs, but not ED visits, or only characterize those ED visits in which an injury is diagnosed.14 The NEDS and NHAMCS data sets provide patient ages, causes of injury, disposition (i.e. hospital admission or discharge to home), and a weighting system that allows calculation of nationally representative estimates. Comparison of estimates of annual total ED visits from these two data sets have been described,15 but to our knowledge, comparative estimates of the number of ED visits due to a specific injury mechanisms have not been examined.
The primary purpose of this study was to obtain estimates of the number of MVC-related ED visits by adults age 65 and older in the United States. Secondarily, we sought to characterize MVC-related ED visits by older adults in regard to arrival mode and time, rates of discharge to home, and pain location, severity, and management.
METHODS
Study Design
This was a retrospective database study and was exempted from formal review by the institutional review board at the University of North Carolina at Chapel Hill.
Study Setting and Population
We examined two data sets, NEDS and NHAMCS, which provide nationally representative estimates of the number of U.S. ED visits and include patient age and cause of injury. We use 2008 data from each of these data sets to describe the number of ED visits and the proportion of patients sent home from the ED. Further, we use NHAMCS data from 2004 through 2008 to characterize these visits in regard to patient demographics and pain location and severity, and data from 2006 through 2008 to characterize pharmacologic pain management.
Age was divided into two categories: 18 to 64 years and ≥65 years. Involvement in an MVC was determined using ICD-9-CM injury codes indicating injury due to MVC (NHAMCS ‘cause of injury recode’ E810–E819.9). This category includes both drivers and passengers, motorcyclists, and bicyclists and pedestrians hit by cars; it does not involve ED visits due to bicycle accidents not involving cars.16 “Discharged home from the ED” excluded patients who were transferred to another facility or who died in the ED.
Data Sets Studied
The NEDS, an annual survey sponsored by the Agency for Healthcare Research and Quality, is compiled annually from the HCUP State Emergency Department Databases and State Inpatient Databases; it contains information on approximately 20% of all ED visits nationally. In 2008, the NEDS included visits from 980 EDs in 28 states. The sample is stratified by geographic region, trauma center designation, urban-rural hospital location, medical school affiliation, and hospital ownership.17 Further description of the NEDS study and data is available on the NEDS website.17
The NHAMCS is an annual survey designed by the National Center for Health Statistics and administered by the U.S. Census Bureau to characterize ambulatory care services at U.S. hospitals. In 2008, NHAMCS collected information about all visits during randomly assigned four-week periods from 357 U.S. EDs at non-institutional general and short-stay hospitals, excluding federal, military, and Veterans Administration hospitals. All data were collected by hospital staff members trained specifically for this survey. The NHAMCS uses a four-stage probability sampling design to obtain estimates of national ED visits. A detailed description of the NHAMCS methodology is available from the National Center for Health Statistics.18
Outcome Measures and Definitions
To determine the total number of MVC-related ED visits, data from 2008 were analyzed because this was the most recent year in which data from both data sets were available. The NHAMCS data from 2004–2008 were used to characterize MVC-related ED visits by older and non-elderly adults in order to ensure sufficient numbers of patients to obtain reliable estimates. Characteristics examined included patient demographics, pain location, pain severity, and analgesia administration. The NEDS data set was not analyzed for secondary outcomes because these variables are not present in the NEDS data set.
Night arrival was defined as an ED arrival occurring after 9 p.m. and before 6 a.m. Pain location was determined from up to three reason-for-visit codes recorded for each visit. Thus, a patient might have three different pain locations. The NHAMCS categorizes pain severity as none, mild, moderate, severe, or missing. We present estimates of the proportion of patients with moderate or severe pain, both using the assumption that patients with missing data had no pain, and excluding patients with missing pain severity data. Medications were categorized based on the eight drug ID code variables available for each visit. Whether the medication was given in the ED or as a discharge prescription was determined using the gpmed variable. Analysis of medications was limited to years 2006 to 2008, since 2006 was the first year in which the NHAMCS differentiated between ED and discharge medications, and used generic medication codes. Analgesics were classified as either an opioid, a nonsteroidal anti-inflammatory drug (NSAID), or acetaminophen. Visits in which patients received combination analgesics were recorded as receiving both an opioid and either an NSAID or acetaminophen, as appropriate.
Data Analysis
All analyses were conducted using Stata IC 11.0 (StataCorp, College Station, TX). HCUP data were purchased and transferred from an Excel file (Microsoft Corporation, Redmond, WA) to Stata. The NHAMCS data were accessed using SAS (SAS Institute Inc, Cary, NC) and transferred to Stata. All analyses used survey procedures with the weights, strata, and primary sampling unit design variables provided by the NHAMCS. For both NEDS and NHAMCS analyses, estimates of population totals and their 95% confidence intervals (CI) were calculated using the Stata command svy:total.19 Characteristics of older and non-elderly adults with MVC-related visits are presented along with 95% CI, which were calculated using the Stata command svy: proportion. All results are based on categories containing at least 30 visits, and with relative standard errors less than 30%.
RESULTS
In 2008, NEDS collected data on 28,445,564 patient visits, and NHAMCS collected data on 34,134 patient visits. Using survey weights and consistent with published results, we estimated the total U.S. ED visits in 2008 to be 124.9 million and 123.8 using NEDS and NHAMCS, respectively (Table 1).20,21 Of these, individuals 65 and older made an estimated 21.3 million (17.1%) and 19.3 million (15.6%) ED visits, and an estimated 226,000 (95% CI 210,000 to 240,000) and 270,000 (95% CI 185,000 to 355,000) MVC-related ED visits, respectively, based on NEDS and NHAMCS. Of these MVC-related ED visits by older adults, the majority were discharged home: NEDS 79% (95% CI 79% to 80%), and NHAMCS 77% (95% CI 66% to 86%).
Table 1.
Sample Numbers and Population Estimates for All Emergency Department Visits, MVC-Related Visits, and Discharged MVC-Related Visits by Age Category, NEDS, and NHAMCS 2008.
| Age, yrs | NEDS | NHAMCS | ||
|---|---|---|---|---|
| Sample | Population × 106 (95% CI) | Sample | Population × 106 (95% CI) | |
| All Visits | ||||
| <18 | 5,980,722 | 26.4 (24.6–28.3) | 7,438 | 27.9 (23.9–31.8) |
| 18–64 | 17,605,186 | 77.2 (73.7–80.7) | 21,489 | 76.6 (68.6–84.6) |
| ≥65 | 4,859,656 | 21.3 (20.3–22.4) | 5,207 | 19.3 (17.3–21.2) |
| Total | 28,445,564 | 124.9 (119.7–130.2) | 34,134 | 123.8 (111.5–136.0) |
| MVC-Related Visit* | ||||
| <18 | 110,341 | 0.49 (0.46–0.52) | 149 | 0.59 (0.438–0.734) |
| 18–64 | 598,829 | 2.63 (2.49–2.77) | 823 | 3.08 (2.62–3.55) |
| ≥65 | 51,246 | 0.23 (0.21–0.24) | 66 | 0.27 (0.185–0.355) |
| Total | 760,416 | 3.34 (3.17–3.51) | 1,038 | 3.94 (3.38–4.50) |
| Discharged MVC-Related Visits^ | ||||
| <18 | 102,586 | 0.45 (0.43–0.48) | 138 | 0.55 (0.41–0.70) |
| 18–64 | 545,611 | 2.38 (2.25–2.51) | 755 | 2.85 (2.42–3.29) |
| ≥65 | 40,598 | 0.18 (0.17–0.19) | 51 | 0.22 (0.14–0.30) |
| Total | 688,795 | 3.00 (2.85–3.16) | 944 | 3.63 (3.10–4.15) |
NEDS = Nationwide Emergency Department Sample; NHAMCS = National Hospital Ambulatory Medical Care Survey; MVC = motor vehicle collision
ICD-9 injury code indicating motor vehicle collision (E810–E819.9)
Excludes patients whose disposition was “transferred” or “died in ED.”
Weighted estimates of MVC-related ED visits by adults age 65 or older for the years 2004 through 2008 obtained using NHAMCS indicate that the majority were female and white (Table 2). Only 5 of the 369 visits in the sample of MVC-related ED visits by older adults were by patients residing in nursing homes. Half of older adults came to the ED by ambulance, a higher percentage than for younger patients, and older adults were less likely to present to the ED at night. Older adults were more likely to report chest pain and less likely to report back pain than younger patients. Neck pain, the most common site of persistent pain in non-elderly adults involved in MVCs,8 was as common in older adults as it was in younger adults. Moderate or severe pain was reported in 47% (95% CI 41% to 54%) of all MVC-related ED visits by older adults and 62% (95% CI 54% to 70%) of visits in which a pain severity score was available. Among MVC-related ED visits by older patients in which the patient was sent home and for which a pain severity score was available, 61% (95% CI 52% to 70%) had moderate or severe pain.
Table 2.
Characteristics of Adult MVC-Related US Emergency Department Visits, by Age Category, NHAMCS 2004–2008.
| Characteristic | Weighted Proportion, % (95% CI)* | |||
|---|---|---|---|---|
| Age 18 to 64 (N = 4,486) | Age ≥ 65 (N = 369) | |||
| Sex | ||||
| Male | 49 | (47–51) | 43 | (37–49) |
| Female | 51 | (49–53) | 57 | (51–63) |
| Race | ||||
| White | 69 | (66–72) | 81 | (76–86) |
| Black | 28 | (25–31) | 15 | (10–19) |
| Arrival by ambulance | 42 | (40–45) | 55 | (48–61) |
| Arrival at night^ | 22 | (20–23) | 12 | (8–17) |
| Pain location† | ||||
| Head¥ | 14 | (12–15) | 14 | (9–19) |
| Neck | 22 | (21–24) | 21 | (15–26) |
| Chest | 6 | (5–7) | 16 | (11–20) |
| Back | 23 | (21–25) | 13 | (9–17) |
| Lower extremity | 13 | (11–14) | 12 | (7–16) |
| Pain severity | ||||
| None | 8 | (6–9) | 12 | (7–17) |
| Mild | 12 | (11–14) | 17 | (11–22) |
| Moderate | 32 | (30–35) | 28 | (22–34) |
| Severe | 28 | (26–31) | 19 | (13–25) |
| Not reported | 19 | (17–21) | 24 | (18–30) |
Weighted proportions refers to age specific proportions, using the survey weights provided by NHAMCS.
ED arrival between the hours of 9 p.m. and 6 a.m.
Derived from reason for visit classification codes, not mutually exclusive.
Includes eye, ear, mouth, tongue, throat, nose, and sinus pain.
NEDS = Nationwide Emergency Department Sample; NHAMCS = National Hospital Ambulatory Medical Care Survey; MVC = motor vehicle collision
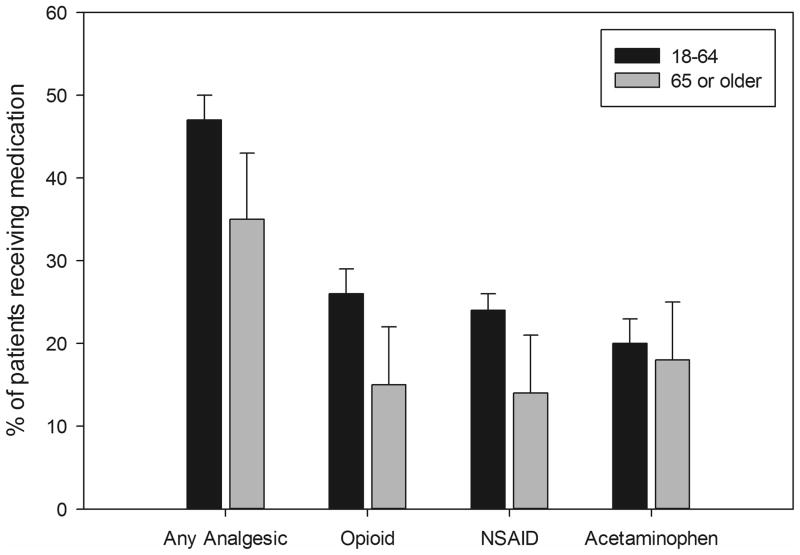
Of patients sent home after MVC-related visits, analgesics were provided in the ED to 35% (95% CI 26% to 43%) of older adults vs. 47% (95% CI 44% to 50%) of non-elderly adults (Figure 1). Among older adults discharged home after MVC-related ED visits and reporting moderate or severe pain, 37% (95% CI 26% to 48%) received analgesics in the ED and 62% (95% CI 51% to 72%) received prescriptions for analgesics to take at home. For younger discharged patients with moderate or severe pain, 55% (95% CI 52% to 59%) received analgesics in the ED and 70% (95% CI 66% to 74%) received prescriptions for analgesics to take at home.
Figure 1.
Among Adult Patients Sent Home after MVC-related ED Evaluation, Proportions and 95% CIs of Patients Receiving Analgesic Medications by Age Category, Analgesic Type, and Administration in the ED or as a Discharge Prescription, NHAMCS 2006–2008.
a) ED Medications
b) Discharge Medications
DISCUSSION
We found that patients 65 years or older made an estimated 226,000 and 270,000 MVC-related ED visits in 2008 using NEDS and NHAMCS, respectively. Moderate or severe pain was reported in more than half of the visits by older adults for whom a pain score was available, and neck or back pain was reported in more than a third of visits. Most older adults are discharged home after MVC-related ED visits, but only about half of these patients are sent home with prescriptions for pain medication. Even among older adults with moderate or severe pain in the ED, more than a third were not sent home with pain medication.
Among younger adults experiencing MVCs, severity of initial pain has been shown to be the dominant risk factor for persistent pain,22 and the neck and back are the most common locations of persistent pain.22,23 Our results suggest that a substantial number of older adults involved in MVCs each year are at risk for the transition to persistent pain. Further, given the association between persistent pain and functional limitations in older adults,24,25 persistent pain may lead to functional decline in these individuals. Despite this, to the best of our knowledge, to date no studies have examined the incidence and predictors of persistent pain and functional decline in older adults experiencing minor MVCs. Such studies are important because substantial data indicate that the incidence and predictors of persistent pain in older and younger adults may differ,26–28 and because the failure to effectively treat acute pain in older adults is common29 and may predispose patients to functional decline.25
The NEDS and NHAMCS estimates of total U.S. ED visits in 2008 differ by less than 1% (124.9 vs. 123.8 million). However, we found an approximately 20% difference in the point estimates of ED visits by older patients due to MVCs (226,000 vs. 270,000 visits). Since the confidence intervals for the NHAMCS estimate encompass both the upper and lower bounds of the estimate for the NEDS estimate, there is not a statistical difference between the two estimates. Hence, the most likely explanation for the discrepancy in the point estimates from these two surveys is poor precision in the estimate using the NHAMCS data set due to the small sample size. Other possible explanations for the disparities in the point estimates include differences in data collection, weighting, or the selection of geographic regions sampled. Given the much larger sample size obtained using NEDS, 226,000 is probably the best available estimate of MVC-related ED visits by individuals 65 years or older in 2008.
Assuming no changes in the proportion of older adults who are involved in MVCs or seek ED evaluation, the projected 78% increase in the population of adults 65 years and older between 2010 and 203030 will results in an increase in MVC-related ED visits from approximately 226,000 to about 400,000. This projection is likely conservative given the anticipated increase in the proportion of active, independent older adults over the coming decades and the projected doubling of police-reported crashes over the same time period.6 Thus, emergency care and rehabilitation of older adults with MVC-related injuries is likely to be an increasingly important element of health care in the coming decades and an important component of the growing epidemic of injuries in older U.S. adults.3,31,32
The percentage of older adults with MVC-related ED visits arriving by ambulance in this study (55%; 95% CI 48% to 61%) is slightly higher than estimates of ambulance use by adults 65 years and older presenting to the ED in general (38% to 43%).33,34 The higher rate of ambulance transport in older vs. non-older adults that we observe is consistent with previously reported differences in emergency medical services use by older vs. younger adults,33 and may reflect either a higher rate of severe injuries, or increased concern about occult injury in older individuals. Arrival to the ED at night was less common in older adults than younger adults. Most likely this represents reduced driving by older adults at night. Self-regulation to avoid driving during poor lighting conditions may contribute to this difference.35,36
In the present study, the rate of ED analgesic administration for patients with MVC-related ED visits was low overall, and lower in older than in younger adults. This difference is consistent with analyses of analgesia administration among older vs. younger patients for pain-related ED visits in general.29 Given evidence that persistent pain may be a substantial problem in older individuals experiencing minor MVCs, and that effective treatment of acute pain may reduce the risk of chronic pain, studies evaluating methods to improve acute pain management in this population are warranted.
LIMITATIONS
Some limitations of our analyses reflect the limited information provided in the NEDS and NHAMCS databases.37 We do not know details of the MVCs, including whether the patient was a driver or passenger, why some patients with pain did not receive analgesics, or whether recipients of analgesics experienced effective relief of pain during their ED visits. As has previously been described using NHAMCS data, pain severity data were more likely to be missing in older than younger adults.38 Although we present both the proportion of the total sample with moderate or severe pain, and the proportion among those reporting pain, we favor the latter estimate. Missing pain data in NHAMCS has been associated with visits by older patients, self-pay patients, and higher illness or injury severity.38 Additionally, among NHAMCS visits in which pain was part of the chief complaint, pain scores were missing in 17% to 24% of adults.29 Thus, missing pain scores in NHAMCS are likely a failure to record pain scores rather than the absence of pain. Although NHAMCS uses a nationally representative sampling method, the small number of MVC-related visits by patients 65 years or older in the sample resulted in broad CIs around estimates of total visits and the characteristics of these patients. We used the publicly available, masked NHAMCS data, meaning that the four stratification variables are simplified into a clustered sampling scheme to prevent identification of the study hospitals. Use of masked data has a minimal effect on point estimates, but increases the confidence intervals by 12% to 45% when compared to unmasked data.39
This analysis relies in ICD-9 injury codes to identify MVC-related ED visits from both the NHAMCS and HCUP datasets. Although these codes are generally considered reliable,40 injury codes may not capture all patients experiencing MVCs, and so may result in an underestimate of the actual number of patients with MVC-related ED visits. Similarly, we defined analgesic as an opioid, NSAID, or acetaminophen. This approach would not capture patients who received other forms of analgesics such as muscle relaxants or non-pharmacologic pain management. The National Electronic Injury Surveillance System – All Injury Program (NEISS-AIP) data set, which also contains patient-level data based on a nationally representative survey of ED visits, was not examined in this study because it is restricted to patients diagnosed with injuries. Because persistent pain after MVCs often occurs in patients without identified injuries, this restriction would underestimate the number of older adults experiencing MVCs and at risk for adverse health outcomes after MVCs.
CONCLUSIONS
Adults age 65 years or older made an estimated 210,000 to 240,000 MVC-related ED visits in 2008. Most of these patients were discharged to home after ED evaluation. Although moderate or severe pain was common among these patients, only a minority were treated with pain medication during their ED visits. Further research is needed to assess long-term pain and functional outcomes in this important, growing, and vulnerable population.
Acknowledgments
Funding: Dr. Platts-Mills is supported by Award Number KL2 RR025746 and Dr. Esserman is supported by Award Number UL1 RR025747 from the National Center for Research Resources through the North Carolina Translational and Clinical Science Institute. The content is solely the responsibility of the authors, and does not necessarily represent the official views of the National Center for Research Resources, the National Institutes of Health, or the North Carolina Translational and Clinical Science Institute.
Footnotes
Offprints: Offprints will not be available from the author.
Presentations: Presented at the Society for Academic Emergency Medicine annual meeting, Boston MA, June 2011.
Disclosures: Dr. McLean is supported in part by a National Institute of Arthritis and Musculoskeletal and Skin Diseases, RO1 research grant. The rest of the authors have no disclosures or conflicts of interest to report.
References
- 1.Dellinger AM, Stevens JA. The injury problem among older adults: mortality, morbidity and costs. J Safety Res. 2006;37:519–22. doi: 10.1016/j.jsr.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Carter MW, Gupta S. Characteristics and outcomes of injury-related ED visits among older adults. Am J Emerg Med. 2008;26:296–303. doi: 10.1016/j.ajem.2007.05.033. [DOI] [PubMed] [Google Scholar]
- 3.Shinoda-Tagawa T, Clark DE. Trends in hospitalization after injury: older women are displacing young men. Inj Prev. 2003;9:214–9. doi: 10.1136/ip.9.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bishop CE, Gilden D, Blom J, et al. Medicare spending for injured elders: are there opportunities for savings? Health Aff (Millwood) 2002;21:215–23. doi: 10.1377/hlthaff.21.6.215. [DOI] [PubMed] [Google Scholar]
- 5.Carter MW, Porell FW. The effect of sentinel injury on Medicare expenditures over time. J Am Geriatr Soc. 2011;59:406–16. doi: 10.1111/j.1532-5415.2010.03283.x. [DOI] [PubMed] [Google Scholar]
- 6.Lyman S, Ferguson SA, Braver ER, Williams AF. Older driver involvements in police reported crashes and fatal crashes: trends and projections. Inj Prev. 2002;8:116–20. doi: 10.1136/ip.8.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perdue PW, Watts D, Kaufmann CR, Chistoph R, Trask AL. Differences in mortality between elderly and younger adult trauma patients: geriatric stauts increases risk of delayed death. J Trauma. 1998;45:805–10. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 8.Suissa S, Harder S, Veilleux M. The relation between initial symptoms and signs and the prognosis of whiplash. Eur Spine J. 2001;10:44–9. doi: 10.1007/s005860000220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Freeman MD, Croft AC, Rossignol AM, Weaver DS, Reiser M. A review and methodologic critique of the literature refuting whiplash syndrome. Spine (Phila) 1999;24:86–96. doi: 10.1097/00007632-199901010-00022. [DOI] [PubMed] [Google Scholar]
- 10.Edwards RR, Fillingim RB, Ness TJ. Age-related differences in endogenous pain modulation: a comparison of diffuse noxious inhibitory controls in healthy older and younger adults. Pain. 2003;101:155–65. doi: 10.1016/s0304-3959(02)00324-x. [DOI] [PubMed] [Google Scholar]
- 11.Riley JL, 3rd, King CD, Wong F, Fillingim RB, Mauderli AP. Lack of endogenous modulation and reduced decay of prolonged heat pain in older adults. Pain. 2010;150:153–60. doi: 10.1016/j.pain.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harder S, Veilleux M, Suissa S. The effect of socio-demographic and crash-related factors on the prognosis of whiplash. J Clin Epidemiol. 1998;51:377–84. doi: 10.1016/s0895-4356(98)00011-0. [DOI] [PubMed] [Google Scholar]
- 13.Wilber ST, Blanda M, Gerson LW, Allen KR. Short-term functional decline and service use in older emergency department patients with blunt injuries. Acad Emerg Med. 2010;17:679–86. doi: 10.1111/j.1553-2712.2010.00799.x. [DOI] [PubMed] [Google Scholar]
- 14.National Electronic Injury Surveillance System (NEISS) [Accessed Apr 7, 2012];Homepage. Available at: http://www.cpsc.gov/library/neiss.html.
- 15.Owens PL, Barrett ML, Gibson TB, Andrews RM, Weinick RM, Mutter RL. Emergency department care in the United States: a profile of national data sources. Ann Emerg Med. 2010;56:150–65. doi: 10.1016/j.annemergmed.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. [Accessed Apr 7, 2012];Matrix of E-code Groupings. Available at: http://www.cdc.gov/injury/wisqars/ecode_matrix.html.
- 17.Healthcare Cost and Utilization Project. [Accessed Apr 7, 2012];Overview of the Nationwide Emergency Department Sample. Available at: http://www.hcup-us.ahrq.gov/nedsoverview.jsp.
- 18.Centers for Disease Control and Prevention. [Accessed Apr 8, 2012];Ambulatory Health Care Data; About NAMCS/NHAMCS. Available at: http://www.cdc.gov/nchs/ahcd.htm.
- 19.Pitblado J. [Accessed Apr 7, 2012];Survey data analysis in Stata. Available at: http://www.stata.com/meeting/canada09/ca09_pitblado_handout.pdf.
- 20.National Hospital Ambulatory Care Survey. [Accessed Apr 7, 2012];Emergency Department Visits. Available at: http://www.cdc.gov/nchs/fastats/ervisits.htm.
- 21.Healthcare Cost and Utilization Project. [Accessed Apr 7, 2012];Statistical Brief #100, emergency department visits for adults in community hospitals. Available at: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb100.pdf.
- 22.Carroll LJ, Hogg-Johnson S, Cote P, et al. Course and prognostic factors for neck pain in workers: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008;33:S93–100. doi: 10.1097/BRS.0b013e31816445d4. [DOI] [PubMed] [Google Scholar]
- 23.Berglund A, Alfredsson L, Cassidy JD, Jensen I, Nygren A. The association between exposure to a rear-end collision and future neck or shoulder pain: a cohort study. J Clin Epidemiol. 2000;53:1089–94. doi: 10.1016/s0895-4356(00)00225-0. [DOI] [PubMed] [Google Scholar]
- 24.Zhu K, Devine A, Dick IM, Prince RL. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine (Phila Pa 1976) 2007;32:2012–8. doi: 10.1097/BRS.0b013e318133fb82. [DOI] [PubMed] [Google Scholar]
- 25.Morrison RS, Flanagan S, Fischberg D, Cintron A, Siu AL. A novel interdisciplinary analgesic program reduces pain and improves function in older adults after orthopedic surgery. J Am Geriatr Soc. 2009;57:1–10. doi: 10.1111/j.1532-5415.2008.02063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cook AJ, Brawer PA, Vowles KE. The fear-avoidance model of chronic pain: validation and age analysis using structural equation modeling. Pain. 2006;121:195–206. doi: 10.1016/j.pain.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 27.Edmond SL, Felson DT. Prevalence of back symptoms in elders. J Rheumatol. 2000;27:220–5. [PubMed] [Google Scholar]
- 28.Jacobs JM, Hammerman-Rozenber R, Cohen A, Stessman J. Chronic back pain among the elderly: prevalence, associations, and predictors. Spine (Phila Pa 1976) 2006;31:E203–7. doi: 10.1097/01.brs.0000206367.57918.3c. [DOI] [PubMed] [Google Scholar]
- 29.Platts-Mills TF, Esserman DA, Brown DL, Bortsov AV, Sloane PD, McLean SA. Older US emergency departments are less likely to receive pain medication than younger patients: results from a national survey. Ann Emerg Med. 2011 doi: 10.1016/j.annemergmed.2011.09.014. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.U.S. Census Bureau. U.S. Population Projections. [Accessed Apr 7, 2012];Interim Projections of the Population by Selected Age Groups for the United States and States: April 1, 2000 to July 1, 2030. Available at: http://www.census.gov/population/www/projections/files/SummaryTabB1.pdf.
- 31.Clark DE, Chu MK. Increasing importance of the elderly in a trauma system. Am J Emerg Med. 2002;20:108–11. doi: 10.1053/ajem.2002.31576. [DOI] [PubMed] [Google Scholar]
- 32.Helmkamp JC, Carter MW. ATV deaths among older adults in West Virginia: evidence suggesting that “60 is the new 40!”. South Med J. 2009;102:465–9. doi: 10.1097/SMJ.0b013e31819d97f2. [DOI] [PubMed] [Google Scholar]
- 33.Platts-Mills TF, Leacock B, Cabanas JG, Shofer FS, McLean SA. Emergency medical services use by the elderly: analysis of a statewide database. Prehosp Emerg Care. 2010;14:329–33. doi: 10.3109/10903127.2010.481759. [DOI] [PubMed] [Google Scholar]
- 34.Shah MN, Bazarian JJ, Lerner EB, et al. The epidemiology of emergency medical services use by older adults: an analysis of the National Hospital Ambulatory Medical Care Survey. Acad Emerg Med. 2007;14:441–7. doi: 10.1197/j.aem.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 35.Freeman EE, Munoz B, Turano KA, West SK. Measures of visual function and their association with driving modification in older adults. Invest Ophthalmol Vis Sci. 2006;47:514–20. doi: 10.1167/iovs.05-0934. [DOI] [PubMed] [Google Scholar]
- 36.Baldock MRJ, Mathias JL, McLean AJ, Berndt A. Self-regulation of driving and its relationship to driving ability in older adults. Accid Anal Prev. 2006;38:1038–45. doi: 10.1016/j.aap.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 37.Hirshon JM, Warner M, Irvin CB, et al. Research using emergency department-related data sets: current status and future directions. Acad Emerg Med. 2009;16:1103–9. doi: 10.1111/j.1553-2712.2009.00554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iyer RG. Pain documentation and predictors of analgesic prescribing for elderly patients during emergency department visits. J Pain Symptom Manage. 2011;41(2):367–73. doi: 10.1016/j.jpainsymman.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 39.Zhu M, Chu H, Rice TM, Carter MW. Implications of conducting trend analyses of emergency department visits using publicly released masked design variables. Ann Emerg Med. 2011;57:683–7. doi: 10.1016/j.annemergmed.2010.12.025. [DOI] [PubMed] [Google Scholar]
- 40.LeMier M, Cummings P, West TA. Accuracy of external cause of injury codes reported in Washington State hospital discharge records. Inj Prev. 2000;7:334–8. doi: 10.1136/ip.7.4.334. [DOI] [PMC free article] [PubMed] [Google Scholar]