Abstract
Purpose
Magnetic resonance imaging (MRI) is often used in the evaluation of lower back pain in adolescents. The purpose of our study is to report on the frequency of MRI missing spondylolysis in adolescents with back pain in a pediatric orthopaedic practice.
Methods
A retrospective review of all patients with a diagnosis of spondylolysis who presented from January 2000 to March 2010 was performed. All patients were evaluated at a single institution by the senior author. Inclusion criteria were patients with spondylolysis confirmed on computed tomography (CT) or plain film that also received an MRI.
Results
Eleven patients with spondylolysis had an MRI performed. The mean age of the study patients was 14.2 years (range 10–17). The diagnosis of spondylolysis was missed in the MRI radiology reading in 7 out of 11 (64 %) studies.
Conclusions
MRI missed a spondylolysis in over half of the adolescents in this consecutive series. In patients with a history or physical findings suggestive of spondylolysis, such as localized pain of the lumbar spine with back extension, further radiographic evaluation should be considered, even if an MRI is negative.
Level of evidence
III, retrospective review.
Keywords: Spondylolysis, Radiology, Adolescent back pain
Introduction
Back pain in the pediatric and adolescent population is an increasingly common clinical entity seen in primary and specialty pediatric clinics, with a prevalence of between 20 and 50 % in North America and Europe [1, 2]. Spondylolysis is one of the most common causes of low back pain, with a reported incidence of 4.4 % in the pediatric population and up to 6 % or more in the adult population [3–6].
Spondylolysis, a defect in the pars interarticularis of the vertebrae, can be unilateral or bilateral [7]. This entity is especially common in adolescent athletes, particularly among gymnasts [8]. The radiographic diagnosis is frequently made with lateral and oblique spine radiographs or computed tomography (CT). Nuclear medicine studies, particularly single-photon emission computed tomography (SPECT) scans, can be used to differentiate acute from chronic spondylolytic lesions.
Magnetic resonance imaging (MRI) is ordered by many primary care and specialty physicians in the evaluation of children and adolescents with back pain, sometimes replacing plain radiographs as the “first-line” imaging [9, 10]. However, studies have reported that MRI misses up to 30 % of spondylolysis that were diagnosed on CT scan [11]. In contrast, others have reported that MRI is an accurate diagnostic tool for the evaluation of spondylolysis and have recommended the use of MRI as a first-line study. Campbell et al. [12] achieved more accurate results using a standardized imaging protocol and found that MRI detected a signal change or morphological abnormality in 98 % (39/40) of pars defects, but still failed to accurately diagnose 25 % (10/40) of the pars fractures when compared to CT.
Patients with back pain are often referred to pediatric orthopaedists after an MRI has been obtained. In the senior author’s practice, we have noticed that MRI misses the diagnosis of spondylolysis in the pediatric and adolescent population more frequently than the existing radiology literature would suggest. The purpose of this study was to determine how frequently MRI misses the diagnosis of spondylolysis when otherwise seen on plain radiography or CT scan in a pediatric orthopaedic practice.
Methods
We retrospectively reviewed the charts and images of all patients with a diagnosis of spondylolysis who presented from July 2000 to March 2010 after obtaining Institutional Review Board approval. We included any patients diagnosed with spondylolysis by plain radiography or CT that also had an MRI. There were a total of 74 children seen in the study period with a diagnosis of spondylolysis. All of these patients were seen and evaluated by the senior author, a pediatric spine surgeon, at a single institution. We excluded all patients without MRI studies. Of the 74 patients with spondylolysis, 11 patients (15 %) met the inclusion criteria and comprise the study group. We recorded the subjects’ ages, gender, duration and quality of symptoms, physical examination findings, and imaging findings.
Results
The mean age of the study subjects was 14.2 years (range 10–17). There were 5 females and 6 males. At the time of presentation to our institution, all 11 patients (100 %) had symptomatic low back pain. The most common physical examination finding was pain with hyperextension, which was seen in 8 out of 11 patients (73 %). The most common vertebra with a pars defect was L5 (9/11 patients, 82 %) (Fig. 1). The other two spondylolysis lesions in our study were seen at L4.
Fig. 1.
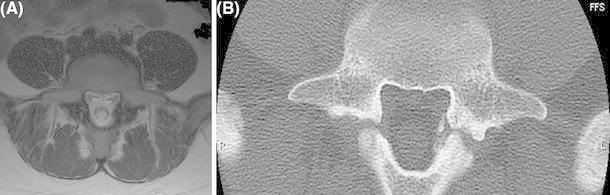
a An axial magnetic resonance imaging (MRI) at the level of L5 of a symptomatic patient with spondylolysis. This MRI was interpreted as nondiagnostic for spondylolysis in the radiology report. b An axial computed tomography (CT) scan of the same patient at the same vertebral level showing the pars defect, indicating that this patient has bilateral spondylolysis
Of the 11 subjects evaluated, we found that MRI did not detect the spondylolysis in 7 out of the 11 subjects (64 %) (see Table 1). In total, 9 of the 11 spondylolysis cases were confirmed by CT (82 %) and two were confirmed by plain radiograph. Of the seven patients not diagnosed with spondylolysis by MRI, two had signal abnormalities on MRI, but these changes were insufficient to diagnose spondylolysis. All of the children with missed spondylolysis by MRI were symptomatic at the time of their evaluation and diagnostic imaging studies. Three patients presented to our clinic with both an MRI and CT demonstrating spondylolysis that were both performed by outside institutions prior to visiting our clinic.
Table 1.
Results of the imaging studies for all subjects
| Subject | MRI | X-ray | CT |
|---|---|---|---|
| 1 | + | + | |
| 2 | − | − | + |
| 3 | − | − | + |
| 4 | + | + | |
| 5 | − | − | + |
| 6 | − | + | |
| 7 | + | + | |
| 8 | − | + | |
| 9 | − | + | + |
| 10 | + | + | + |
| 11 | − | + | + |
“+” indicates spondylolysis detected; “−” indicates no spondylolysis detected
Plain radiographic studies (in addition to an MRI) were performed in eight patients, of which 3 (38 %) failed to diagnose spondylolysis and required a CT to demonstrate the spondylolysis. Of the six subjects with an MRI negative for spondylolysis, three subjects (50 %) had negative radiographs. Three of the five subjects with radiographs demonstrating spondylolysis received a CT for treatment planning.
Discussion
Spondylolysis is a common cause of low back pain in the pediatric and adolescent population [3–5]. Fredrickson et al. [6] reported an incidence of spondylolysis of 4.4 % among children under 6 years of age and an incidence of approximately 6 % in adulthood.
In the evaluation of spondylolysis, plain radiographs are commonly used as the first-line imaging [13]. Prior to CT (the current gold standard) and MRI, the imaging modality of choice was plain radiography, with lateral and oblique radiographs of the lumbar spine to evaluate for defects of the pars interarticularis. Since the advent and development of CT, many studies support that CT is more sensitive than plain radiographs in detecting early spondylolytic lesions [14, 15]. In our study, we found that plain radiographs missed the diagnosis of spondylolysis in 38 % (3 of 8) of the subjects in which it was used and that, after a negative MRI, radiographs missed spondylolysis 50 % of the time. These results are consistent with previous studies finding that over half of spondylolysis lesions (53 %) can be missed on plain films alone [15]. Additionally, even in patients with radiographs demonstrating spondylolysis, a CT scan was often obtained for treatment planning to assess the acuity of the spondylolytic lesion [16, 17].
Although CT is the current gold standard for the diagnosis of spondylolysis, recent advancements in imaging and reports in the literature have led to the increased use of MRI as a first-line study in the diagnosis of spondylolysis [9, 10]. MRI has the advantage of minimizing radiation exposure and improved imaging of soft tissue structures. As such, MRI can be a useful tool for evaluating the acuteness of spondylolysis (with the presence of edema being indicative of a more acute lesion), which may help guide treatment decisions [9]. Studies from the radiology literature report that MRI has a sensitivity of up to 86 %, a specificity of 82 %, a positive predictive value of 18 %, and a negative predictive value of 99 % in the diagnosis of spondylolysis [10]. Therefore, MRI has been suggested to be a good screening tool for spondylolysis. A retrospective study by Ulmer et al. [11] reported that up to 30 % (20/66) of lumbar spondylolysis cases may be misdiagnosed by MRI. In a separate study by Campbell et al., 22 patients with spondylolysis underwent an imaging protocol, which included CT, SPECT, and MRI studies all performed on the same day to evaluate for pars defects, using CT as the gold standard. Although they found that 98 % of the 40 pars defects evaluated by MRI demonstrated either a signal change or morphological abnormality under their imaging protocol, they also reported that these MRI abnormalities did not always lead to a correct diagnosis. In their study, MRI failed to correctly identify 1 of every 4 cortical pars fractures (25 %, 10/40 pars fractures) when compared to CT [12]. In comparison, our study shows that, in a clinical practice setting, MRI can miss an even higher number of spondylolysis cases. We found that up to 64 % of spondylolysis cases (7/11) in symptomatic patients seeing a pediatric orthopaedic surgeon can be missed if MRI is the only diagnostic imaging study performed. Given the results of our study and review of the literature, it is now standard protocol at our institution to obtain a limited CT scan when presented with a patient with a history and physical examination suggestive of spondylolysis and an MRI that appears “normal.”
The limitations of our study include the fact that it is retrospective and has a relatively small population size. In addition, since many of the patients who present to our office are referred from other centers, a number of patients present with MRI studies already obtained from an outside facility, so the imaging techniques for this study were not standardized. However, we believe that our results more accurately reflect the experiences a practicing orthopaedic surgeon sees in the “real world”.
In summary, relying solely on the MRIs done in this patient population, the diagnosis of spondylolysis would have been missed in more than half of the children in this series. We recommend that, if the history and physical examination are suspicious for spondylolysis, further radiographic evaluation be considered, even in the setting of a “normal” MRI.
Conflict of interest
None.
References
- 1.Burton AK, Clarke RD, McClune TD, Tillotson KM. The natural history of low back pain in adolescents. Spine (Phila Pa 1976) 1996;21(20):2323–2328. doi: 10.1097/00007632-199610150-00004. [DOI] [PubMed] [Google Scholar]
- 2.Skaggs DL, Early SD, D’Ambra P, Tolo VT, Kay RM. Back pain and backpacks in school children. J Pediatr Orthop. 2006;26(3):358–363. doi: 10.1097/01.bpo.0000217723.14631.6e. [DOI] [PubMed] [Google Scholar]
- 3.Faingold R, Saigal G, Azouz EM, Morales A, Albuquerque PA. Imaging of low back pain in children and adolescents. Semin Ultrasound CT MR. 2004;25(6):490–505. doi: 10.1053/j.sult.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Micheli LJ, Wood R. Back pain in young athletes. Significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995;149(1):15–18. doi: 10.1001/archpedi.1995.02170130017004. [DOI] [PubMed] [Google Scholar]
- 5.Ralston S, Weir M. Suspecting lumbar spondylolysis in adolescent low back pain. Clin Pediatr (Phila) 1998;37(5):287–293. doi: 10.1177/000992289803700502. [DOI] [PubMed] [Google Scholar]
- 6.Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984;66(5):699–707. [PubMed] [Google Scholar]
- 7.Logroscino G, Mazza O, Aulisa G, Pitta L, Pola E, Aulisa L. Spondylolysis and spondylolisthesis in the pediatric and adolescent population. Childs Nerv Syst. 2001;17(11):644–655. doi: 10.1007/s003810100495. [DOI] [PubMed] [Google Scholar]
- 8.El Rassi G, Takemitsu M, Woratanarat P, Shah SA. Lumbar spondylolysis in pediatric and adolescent soccer players. Am J Sports Med. 2005;33(11):1688–1693. doi: 10.1177/0363546505275645. [DOI] [PubMed] [Google Scholar]
- 9.Leone A, Cianfoni A, Cerase A, Magarelli N, Bonomo L. Lumbar spondylolysis: a review. Skeletal Radiol. 2011;40(6):683–700. doi: 10.1007/s00256-010-0942-0. [DOI] [PubMed] [Google Scholar]
- 10.Saifuddin A, Burnett SJ. The value of lumbar spine MRI in the assessment of the pars interarticularis. Clin Radiol. 1997;52(9):666–671. doi: 10.1016/S0009-9260(97)80029-3. [DOI] [PubMed] [Google Scholar]
- 11.Ulmer JL, Mathews VP, Elster AD, Mark LP, Daniels DL, Mueller W. MR imaging of lumbar spondylolysis: the importance of ancillary observations. AJR Am J Roentgenol. 1997;169(1):233–239. doi: 10.2214/ajr.169.1.9207531. [DOI] [PubMed] [Google Scholar]
- 12.Campbell RS, Grainger AJ, Hide IG, Papastefanou S, Greenough CG. Juvenile spondylolysis: a comparative analysis of CT, SPECT and MRI. Skeletal Radiol. 2005;34(2):63–73. doi: 10.1007/s00256-004-0878-3. [DOI] [PubMed] [Google Scholar]
- 13.Mason DE. Back pain in children. Pediatr Ann. 1999;28(12):727–738. doi: 10.3928/0090-4481-19991201-07. [DOI] [PubMed] [Google Scholar]
- 14.Harvey CJ, Richenberg JL, Saifuddin A, Wolman RL. The radiological investigation of lumbar spondylolysis. Clin Radiol. 1998;53(10):723–728. doi: 10.1016/S0009-9260(98)80313-9. [DOI] [PubMed] [Google Scholar]
- 15.Anderson K, Sarwark JF, Conway JJ, Logue ES, Schafer MF. Quantitative assessment with SPECT imaging of stress injuries of the pars interarticularis and response to bracing. J Pediatr Orthop. 2000;20(1):28–33. [PubMed] [Google Scholar]
- 16.Sairyo K, Sakai T, Yasui N. Conservative treatment of lumbar spondylolysis in childhood and adolescence: the radiological signs which predict healing. J Bone Joint Surg Br. 2009;91(2):206–209. doi: 10.1302/0301-620X.91B2.21256. [DOI] [PubMed] [Google Scholar]
- 17.McClellan JW, Ryschon K, Stamm S (2009) Healing rate for 124 adolescent lumbar pars interarticularis fractures treated conservatively. Paper presented at the Scoliosis Research Society (SRS) 44th annual meeting & course, San Antonio, TX, USA, 23–26 September 2009


