Abstract
Objectives
To investigate the effect of hot and cold temperatures on ambulance attendances.
Design
An ecological time-series study.
Setting and participants
The study was conducted in Brisbane, Australia. The authors collected information on 783 935 daily ambulance attendances, along with data of associated meteorological variables and air pollutants, for the period of 2000–2007.
Outcome measures
The total number of ambulance attendances was examined, along with those related to cardiovascular, respiratory and other non-traumatic conditions. Generalised additive models were used to assess the relationship between daily mean temperature and the number of ambulance attendances.
Results
There were statistically significant relationships between mean temperature and ambulance attendances for all categories. Acute heat effects were found with a 1.17% (95% CI 0.86% to 1.48%) increase in total attendances for 1°C increase above threshold (0–1 days lag). Cold effects were delayed and longer lasting with a 1.30% (0.87% to 1.73%) increase in total attendances for a 1°C decrease below the threshold (2–15 days lag). Harvesting was observed following initial acute periods of heat effects but not for cold effects.
Conclusions
This study shows that both hot and cold temperatures led to increases in ambulance attendances for different medical conditions. Our findings support the notion that ambulance attendance records are a valid and timely source of data for use in the development of local weather/health early warning systems.
Article summary
Article focus
To examine the relationship between exposure to hot and cold temperatures and ambulance attendances.
To contribute to the literature concerning effects of climate change on non-fatal health outcomes, specifically ambulance attendances.
Key messages
Hot and cold ambient temperatures affected ambulance attendances for a variety of health outcomes.
There were differences in the temperature–attendance relationship for different medical conditions.
Strengths and limitations of this study
This study adds to the limited literature examining the effects of temperature on non-fatal health outcomes.
Ambulance attendance data could be useful for the development of weather/health early warning systems.
Misclassification bias might exist due to non-standardised coding in administrative ambulance data.
The location of attendance may not always correspond with the location where the patient received the majority of exposure.
Introduction
The effect of climate change on human health has received much attention in response to projected scenarios of both increasing and more variable global temperatures.1 2 It is important to examine these effects as not only will it increase knowledge of the relationships between temperature and human health, but this information will also inform public health policy that seeks to minimise the adverse impacts of climate change on the population, particularly in terms of major chronic conditions, such as cardiovascular and respiratory diseases.3
To date, a large body of research has been devoted to examining the effects of temperature on mortality for different populations, with a particular focus on vulnerable subgroups, such as older people and the frail.4 5 Studies have examined the effects of hot and cold temperatures in terms of same-day and extended periods of exposure (eg, heatwaves), the apparent variation in responses between populations living in different climates and the presence of lagged responses to exposure.6–9 Another important area of study relates to the non-linear nature of the temperature–health relationship, which is sometimes interpreted through the existence of temperature ‘comfort zones’, above and below which the health risk due to increasing or decreasing temperature increases dramatically.10
As opposed to research into fatal health events, there has been much less attention into research of non-fatal health outcomes. To date, only a few studies have concentrated on hospital and/or emergency department admissions data, collected from either hospital or health department information systems.11–13 A number of benefits to using non-fatal event data have been suggested, from the ability to conduct more targeted health intervention strategies throughout the community,14 to the development of early warning assessment systems.15–17 In such applications, other forms of morbidity data such as ambulance attendance records have been cited as being potentially useful for the purposes of capturing those events that, while not leading to immediate death, are important precursors to such incidents and therefore to effective public health intervention strategies.
There have been few attempts to examine the effect of temperature on ambulance attendances.18–20 A number of studies have reported a strong relationship between same-day temperature and emergency admissions by ambulance for cerebrovascular disease21 22 and respiratory disease.23 A study of ambulance response calls and extreme heat in Toronto24 examined the spatial variation in calls across the city, noting that increased call rates during hot periods were related to day-of-week factors and associated population movements. Two recent studies from Toronto25 and Italy26 attempted to quantify the temperature–ambulance attendance relationship for cardiovascular and respiratory disease and heat/cold exposure, after controlling for seasonality, air pollution and day-of-week factors. They found an increase in ambulance attendances for cardiovascular, respiratory and other non-traumatic diseases in relation to exposure to temperatures during the summer period.
To date, there exists a lack of research examining the effects of temperature on morbidity, particularly ambulance attendances, and no studies have been conducted in a subtropical climate to assess both cold and hot temperature effects on ambulance attendances. This study therefore examined the relationship between ambient temperature and ambulance attendances in Brisbane, Australia.
Methods
The study population
Brisbane is the capital city of Queensland, located on the east coast of Australia (27° 30′ south and 153° 00′ east). It has a subtropical climate and generally experiences mild winters (average minimum and maximum temperature: 9.7°C, 21.3°C) and hot summers (average minimum and maximum temperature: 20.8°C, 28.7°C). The population increased over the study period from 0.88 million in 2000 to 1.01 million in 2007.
Data on meteorological factors, air pollution and ambulance attendances in Brisbane, Australia, for the period from 1 January 2000 to 31 December 2007 were obtained from relevant government agencies. As postcode was the only available geographical location identifier, a list of postcodes for the City of Brisbane was obtained from the Australian Bureau of Statistics and Brisbane City Council to define the area and population of the study.
Ambulance attendance data
Anonymised ambulance attendance data were supplied by the Queensland Ambulance Service, the main provider of out-of-hospital emergency care and ambulance transport in Queensland. The variables extracted from each anonymised attendance record were the date of attendance, sex and age of the patient, postcode of attendance event and the health assessment of the patient, recorded using a specific coding system. The data were collected from the ambulance information management system used by the Queensland Ambulance Service. Ethical approval was obtained prior to the collection of these data.
In this study, we calculated the daily number of attendance events for groups of health assessment codes related to cardiovascular, respiratory or other non-traumatic attendances that may have been related to ambient temperature exposure.
Exposure data
Daily meteorological data from a central monitoring station were obtained from the Bureau of Meteorology, which consisted of observations of daily mean temperature (calculated as the average of the daily minimum and maximum temperatures) and humidity. Air pollution data were obtained from the Department of Environment and Resource Management and consisted of hourly mean concentrations of ozone (O3), nitrogen dioxide (NO2), sulphur dioxide (SO2) and particulate matter of size <10 μm (PM10) from eight monitoring sites throughout Brisbane. Daily mean values were then calculated for all meteorological and environmental data; when a particular station lacked daily environmental data, the average across the remaining stations was calculated. Daily mean temperature was used in the analysis, following several previous studies that have shown it to perform as well as or better than other temperature measures.27–29
Statistical analysis
To better understand the nature of the association between ambulance attendances and temperature, we initially examined the exposure–response curve using generalised additive models. The relationship between same-day temperature and attendances was analysed using a natural cubic spline with 4 degrees of freedom (df). The model also adjusted for the possible confounding effects of humidity, O3, NO2, SO2 and PM10 by using separate cubic splines with 4 df each. The selection of df was based on previous research.30 To control for any secular trends and seasonal effects other than temperature, time was incorporated using a cubic spline with 5 df per year. Effects from both day-of-week and public holidays were incorporated through dummy variables to control for calendar effects.
To derive specific estimates of heat and cold slopes, we applied a distributed lag non-linear model (DLNM) with either a ‘V’- or ‘U’-shape linear threshold.10 31 This involved specifying a single or double threshold for temperature and then estimating a log-linear change in risk of ambulance attendances above (or below) the hot (or cold) threshold(s). To examine the nature of delayed effects of temperature on ambulance attendances, a natural cubic spline was used to incorporate lagged effects up to 27 days.9 An approximate range for threshold value(s) was selected for each attendance group. These ranges were partitioned into 0.5°C increments, and the DLNM model was applied iteratively using each value across the range. The thresholds were then selected based on the model of best fit (lowest deviance) across the values. Using the DLNM with these thresholds, cold effects (1°C decrease in temperature below the threshold) and heat effects (1°C increase in temperature above the threshold) were graphically examined across lags. Based on an examination of the general nature of the exposure–response relationship for lags up to 27 days, parametric effect estimates were obtained using a lag-stratified approach10 for the following lag periods: the average of lag days 0–1, 2–15 and 16–27. Estimates of the per cent change in ambulance attendance corresponded to a 1°C increase (or decrease) in temperature above (or below) the threshold(s). There were no missing values in the ambulance attendance data, and very few missing environmental data after aggregation over all available stations (0.24% temperature data and 0.44% humidity data). All analyses were conducted in SAS V.9.2 (SAS Institute Inc) and R V2.12.2.
Results
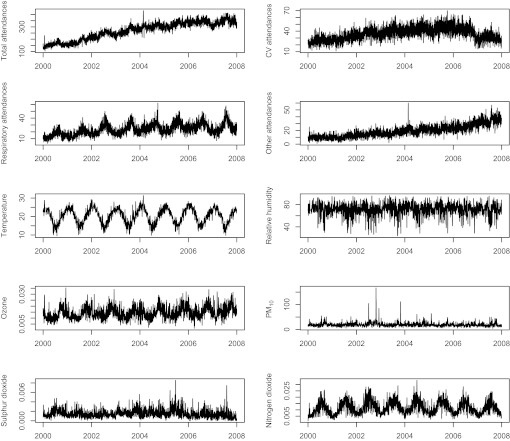
Figure 1 shows the distribution of attendance events through time for all attendance categories, meteorological and air pollution variables. A strong increasing secular trend was apparent for total attendance events over the study period, with a similar but slightly weaker trend for cardiovascular and other non-traumatic attendances. A strong seasonal pattern was observed for respiratory attendances, with increases during the cooler months. A sharp spike in total attendance events occurred during early 2004, which corresponded to a severe heatwave in Brisbane at that time.32 Strong seasonality was observed in temperature, along with O3 and NO2 concentrations, with weaker seasonality present in both relative humidity and SO2 concentrations. There was no apparent seasonal pattern for PM10.
Figure 1.
Distributions of ambulance attendance counts, temperature and air pollutants. CV, cardiovascular.
Table 1 shows that for the period of study from 2000 to 2007, there were 783 935 ambulance attendances, of which 15.3%, 8.7% and 7.1% were cardiovascular, respiratory and other non-traumatic conditions, respectively. Daily mean temperature for the period ranged from 9°C to 34.2°C.
Table 1.
Summary statistics for daily ambulance attendances, meteorological and air pollution variables in Brisbane, 2000–2007
| Variable | No. of days | Mean | Minimum | 25th Percentile | Median | 75th Percentile | Maximum |
| Total (783 935 counts) | 2922 | 268.3 | 104 | 210 | 283.5 | 325 | 432 |
| Cardiovascular (120 041 counts) | 2922 | 41.1 | 11 | 34 | 41 | 48 | 77 |
| Respiratory (68 535 counts) | 2922 | 23.5 | 3 | 18 | 23 | 29 | 62 |
| Other non-traumatic (55 822 counts) | 2922 | 19.1 | 1 | 12 | 18 | 25 | 60 |
| Mean temperature (°C) | 2915 | 20.5 | 9 | 17.1 | 21 | 23.7 | 34.2 |
| Relative humidity (%) | 2909 | 71.4 | 23.8 | 66.3 | 72.6 | 78.5 | 96.3 |
| PM10 (μg/m3) | 2922 | 19.7 | 4.7 | 14.9 | 18.4 | 22.6 | 166.8 |
| Ozone (ppm) | 2922 | 0.0144 | 0.0014 | 0.0107 | 0.0137 | 0.0174 | 0.0353 |
| Sulphur dioxide (ppm) | 2922 | 0.0015 | 0 | 0.0009 | 0.0013 | 0.0019 | 0.0085 |
| Nitrogen dioxide (ppm) | 2922 | 0.0116 | 0.0014 | 0.0077 | 0.0109 | 0.0151 | 0.0333 |
Table 2 shows the correlation coefficients between all attendances and environmental variables. There exists significant, although weak, correlation between temperature, humidity and air pollutants. Temperature and NO2 were found to have the strongest correlation across all variables.
Table 2.
Spearman correlations between environmental variables for Brisbane, 2000–2007
| O3 | PM10 | SO2 | NO2 | |
| Temperature | 0.132** | 0.033 | −0.162** | −0.670** |
| O3 | 0.106** | −0.119** | −0.225** | |
| PM10 | 0.273** | 0.305** | ||
| SO2 | 0.397** |
**p<0.001.
Through the use of a DLNM with a linear threshold model for temperature, it was found that the exposure–response relationship for total, cardiovascular and respiratory attendances was described by a ‘V’ shape with a threshold temperature (of minimum attendance count) of 22°C. The other non-traumatic attendance group was best described by a ‘U’ shape with a large comfort zone between 15.5°C and 28°C.
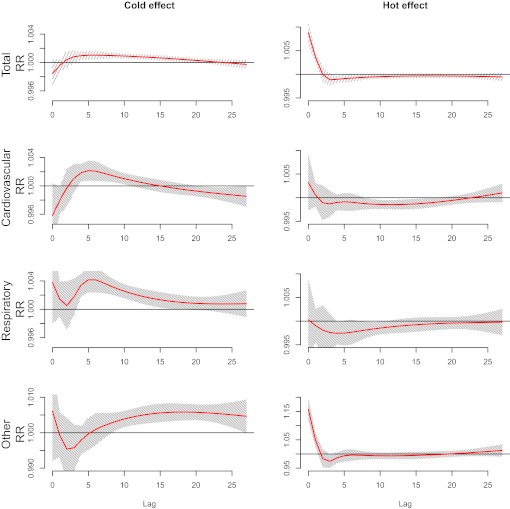
There were similar patterns of lagged effects of both hot (a 1°C increase above the threshold) and cold (a 1°C decrease below the threshold) temperatures on the number of ambulance attendances across all groups (figure 2). Cold effects were found to be delayed, generally occurring 2–3 days following exposure for all groups. The other non-traumatic attendance group was an exception, with effects not occurring until approximately 5–8 days after exposure. The respiratory and other non-traumatic groups also displayed signs of acute cold effects, although these were not statistically significant. Heat effects were found to be acute across all groups, occurring within 0–2 days following exposure.
Figure 2.
Lagged effects for a 1°C decrease (left) and increase (right) in mean temperature below (and above) the threshold temperature for total, cardiovascular, respiratory and other non-traumatic attendances. The shaded region corresponds to the 95% CI.
We calculated parametric effect estimates for the average of lags 0–1, 2–15 and 15–27 (table 3). There were significant heat effects over lags 0–1, with a 1°C increase in temperature above 22°C associated with a 1.17% (95% CI 0.86% to 1.48%) increase in total ambulance attendances. The largest heat effect found was for the other non-traumatic attendance group, with a 1°C increase in temperature resulting in a 20.56% (95% CI 15.15% to 26.10%) increase in attendances.
Table 3.
Temperature effects on ambulance attendances in Brisbane, Australia
| Lag in days | Attendance category (95% CI) |
||||
| Total (22°C) | Cardiovascular (22°C) | Respiratory (22°C) | Other (15.5/28°C) | ||
| Heat effect | 0–1 | 1.17 (0.86 to 1.48) | 0.45 (−0.26 to 1.16) | −0.38 (−1.40 to 0.63) | 20.56 (15.15 to 26.10) |
| 2–15 | −0.82 (−1.35 to −0.30) | −1.85 (−3.06 to −0.64) | −1.99 (−3.72 to −0.25) | −12.37 (−27.06 to 2.48) | |
| 16–27 | −0.47 (−0.97 to 0.04) | −0.35 (−1.51 to 0.81) | −0.72 (−2.38 to 0.94) | 3.19 (−10.30 to 16.83) | |
| Cold effect | 0–1 | −0.16 (−0.40 to 0.08) | −0.62 (−1.17 to −0.06) | 0.63 (−0.09 to 1.34) | −0.38 (−2.12 to 1.38) |
| 2–15 | 1.30 (0.87 to 1.73) | 1.63 (0.64 to 2.62) | 3.65 (2.38 to 4.92) | 3.40 (0.43 to 6.37) | |
| 16–27 | 0.12 (−0.28 to 0.53) | −1.1 (−2.03 to −0.16) | 0.9 (−0.30 to 2.11) | 6.49 (3.62 to 9.36) | |
Significant effects are highlighted in bold.
Effects given as per cent change per 1°C above or below threshold (threshold stated in brackets for each category).
We found that the hot effects on all groups displayed characteristics consistent with harvesting, with a significant decrease in attendances for total (−0.82%, 95% CI −1.35% to −0.30%), cardiovascular (−1.85%, 95% CI −3.06% to −0.64%) and respiratory (−1.99%, 95% CI −3.72% to −0.25%) categories over lags 2–15, which followed the immediate increases in ambulance attendance observed over the first few days of exposure.
Cold effects over lags 2–15 were found for all categories, with the largest increases in attendances associated with respiratory (3.65%, 95% CI 2.38% to 4.92%) and other non-traumatic (3.40%, 95% CI 0.43% to 6.37%) groups. The other non-traumatic attendance group also showed significant cold effects from 15 days onward (6.49%, 95% CI 3.62% to 9.36%). There was no apparent harvesting observed in cold effects, except for the cardiovascular group (For unadjusted effect estimates, see online supplemental material.)
Discussion
In this study, we examined the relationship between temperature and ambulance attendances using time-series modelling techniques. Cold and heat effects were observed for all attendance categories. There was a ‘V’- or ‘U’-shaped relationship between daily mean temperature and ambulance attendances, with statistically significant increases in different attendance categories for a 1°C change in temperature from the thresholds. Cold effects were found to be delayed in onset but last longer than heat effects, which were immediate and short-lived.
There have been few studies of the effects of ambient temperature on ambulance attendances. A Toronto study25 reported large increases in ambulance response calls during the summer period. Similarly, a multicity analysis in Italy26 found an increasing risk of ambulance dispatches for increasing temperature, with the largest same-day heat effects occurring for other non-traumatic and respiratory conditions. However, no cold effect was observed in their study. The short-term nature of the heat effects in these studies has been observed more generally. Heat effects on both cardiovascular and respiratory diseases are often observed to be immediate and short term,25 33 with the strongest heat effects recorded in the first 1–3 days following exposure, before decreasing in magnitude.34 We found similar trends across all attendance categories, with a heat effect observed immediately following exposure. In terms of cold temperature effects, we found a significantly increased risk for all attendance categories. The cold effects on cardiorespiratory attendances are consistent with most previous studies.35–37 Our results indicate that the short exposure lags considered in the Italian study26 may have resulted in an underestimation of the cold effect. Our findings of lagged effect of cold temperatures of up to 15 days following exposure corroborate observations from previous research.35 38
A common pattern across all categories was the slight drop in heat effects between 2 and 15 days, consistent with the harvesting phenomenon found in studies of temperature and mortality.6 The occurrence of such an effect has a clear physiological explanation in terms of fatal health outcomes; however, it is less clear as to what would cause this displacement in out-of-hospital attendances. One factor may be due to an initial large number of transfers and subsequent admissions of seriously ill patients to hospital. Once there, it would be expected that such people would spend a number of days in hospital, thereby removing high-risk individuals from the general population that would further use ambulance services.
An interesting finding was the differences in temperature effects on different categories of ambulance attendance. In our study, for same-day temperature exposure, there was a slight non-significant decrease and increase in heat effect for respiratory and cardiovascular attendances, respectively. In particular, the direction of effect on respiratory attendances is in line with previous results that show a protective effect of hot temperatures on preadmission respiratory morbidity.39 This finding may be due to the fact that in our study, respiratory tract infections made up a large proportion of respiratory attendances, conditions that are more prevalent in cooler weather.23 36 The other non-traumatic attendance category displayed a significantly larger heat effect. This is likely a result of either the higher temperature threshold identified for this subgroup or the fact it contained a large percentage of attendances that were related to psychiatric issues, which have been identified as being strongly influenced by high temperatures.40
This study has a number of strengths. First, given the current lack of research into temperature effects on ambulance attendances, the study contributes to an understanding of how prehospital health conditions are affected by changes in temperature. Second, ambulance attendances often occur for conditions that do not require hospital admission nor cause death. This implies that ambulance attendance data may be useful in surveillance systems as they provide the ability to monitor health outcomes that will not be captured in mortality or admissions data.
Limitations of the study should also be acknowledged. First, compared with other types of health outcomes such as mortality, hospital admissions and emergency admissions, the available coding regime was limited for ambulance attendances, and therefore, the risk of misclassification of health outcomes was potentially higher here than for other types of health outcomes. As the primary purpose of the ambulance data set is for administrative and performance evaluation purposes, codes are not required at the level of detail seen in a hospital setting, as a more thorough diagnosis is made once the patient is admitted. Therefore, the relevant attendance categories were necessarily grouped together. Second, the postcode variable in our data set reflected the location of attendance, not the residential area of the patient. Therefore, the location of attendance may not closely correspond with the location where the patient received the majority of exposure. Finally, the implementation of a new information system and coding regime in 2006 may have produced some measurement error in the data. However, sensitivity analyses using data from each year separately and also data from before the new system was implemented (2000–2005) were found to make little difference to the results.
This research may have several implications, within both the research domain and public health policy arena. First, this study has shown that the effects of ambient temperature on ambulance attendances in a subtropical climate are similar to those found in both hospital admissions and mortality data.5 However, some specific effects on ambulance attendances were found to differ from those on hospital admissions or mortality and also between the different attendance categories; it would therefore be useful to compare different exposure–response relationships in future research.18 In terms of public health policy,24 examining ambulance attendances rather than admission or mortality data would potentially help to pick up the early signs of temperature effects and also the effects on health conditions that cannot be examined through analysis of mortality and hospital admissions data.
This study found significant effects of both cold and hot temperatures and lagged effects of up to 15 days on cardiorespiratory attendances, which contributes to the currently limited research of temperature effects on ambulance attendances. The use of ambulance data in epidemiological research is needed in order to assess a wider range of non-fatal health outcomes, with its analysis particularly useful in the development of more responsive early warning and health surveillance systems.
Supplementary Material
Acknowledgments
The authors thank Emma Enraght-Mooney and Jamie Quinn at the Queensland Ambulance Service for their help in obtaining and analysing the health data. The authors also thank Adrian Barnett and Yuming Guo for their advice during analysis.
Footnotes
To cite: Turner LR, Connell D, Tong S. Exposure to hot and cold temperatures and ambulance attendances in Brisbane, Australia: a time-series study. BMJ Open 2012;2:e001074. doi:10.1136/bmjopen-2012-001074
Contributors: LRT carried out the data analysis and produced the final manuscript. ST was responsible for the design and coordination of the study, and helped with the preparation and revision of the manuscript. DC read and revised the manuscript. All authors read and approved the final manuscript.
Funding: This research was partly funded by the Australian Research Council (DP1095752 to ST and DC). ST is supported by an NHMRC Research Fellowship (553043).
Competing interests: None.
Ethics approval: Ethics approval was provided by the QUT Human Research Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 2009;373:1693–733 [DOI] [PubMed] [Google Scholar]
- 2.Patz JA, Campbell-Lendrum D, Holloway T, et al. Impact of regional climate change on human health. Nature 2005;438:310–17 [DOI] [PubMed] [Google Scholar]
- 3.Lin S, Luo M, Walker RJ, et al. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 2009;20:738–46 [DOI] [PubMed] [Google Scholar]
- 4.Barnett AG. Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology 2007;18:369–72 [DOI] [PubMed] [Google Scholar]
- 5.Hajat S, Kovats RS, Lachowycz K. Heat-related and cold-related deaths in England and Wales: who is at risk? Occup Environ Med 2007;64:93–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu W, Mengersen K, Hu W, et al. Assessing the relationship between global warming and mortality: lag effects of temperature fluctuations by age and mortality categories. Environ Pollut 2011;159:1789–93 [DOI] [PubMed] [Google Scholar]
- 7.Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health 2009;8:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martiello MA, Giacchi MV. High temperatures and health outcomes: a review of the literature. Scand J Public Health 2010;38:826–37 [DOI] [PubMed] [Google Scholar]
- 9.Guo Y, Barnett AG, Pan X, et al. The impact of temperature on mortality in Tianjin, China: a case-crossover design with a distributed lag nonlinear model. Environ Health Perspect 2011;119:1719–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Armstrong B. Models for the relationship between ambient temperature and daily mortality. Epidemiology 2006;17:624–31 [DOI] [PubMed] [Google Scholar]
- 11.Schwartz J, Samet JM, Patz JA. Hospital admissions for heart disease: the effects of temperature and humidity. Epidemiology 2004;15:755–61 [DOI] [PubMed] [Google Scholar]
- 12.Liang WM, Liu WP, Chou SY, et al. Ambient temperature and emergency room admissions for acute coronary syndrome in Taiwan. Int J Biometeorol 2008;52:223–9 [DOI] [PubMed] [Google Scholar]
- 13.Knowlton K, Rotkin-Ellman M, King G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect 2009;117:61–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGeehin MA, Mirabelli M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ Health Perspect 2001;109(Suppl 2):185–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bassil KL, Cole DC, Moineddin R, et al. Development of a surveillance case definition for heat-related illness using 911 medical dispatch data. Can J Public Health 2008;99:339–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Claessens YE, Taupin P, Kierzek G, et al. How emergency departments might alert for prehospital heat-related excess mortality? Crit Care 2006;10:R156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.English PB, Sinclair AH, Ross Z, et al. Environmental health indicators of climate change for the United States: findings from the State Environmental Health Indicator Collaborative. Environ Health Perspect 2009;117:1673–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cerutti B, Tereanu C, Domenighetti G, et al. Temperature related mortality and ambulance service interventions during the heat waves of 2003 in Ticino (Switzerland). Soz Praventivmed 2006;51:185–93 [DOI] [PubMed] [Google Scholar]
- 19.Palecki MA, Changnon SA, Kunkel KE. The nature and impacts of the July 1999 heat wave in the midwestern United States: learning from the lessons of 1995. Bull Am Meteorol Soc 2001;82:1353–67 [Google Scholar]
- 20.Nitschke M, Tucker GR, Hansen AL, et al. Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: a case-series analysis. Environ Health 2011;10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Makie T, Harada M, Kinukawa N, et al. Association of meteorological and day-of-the-week factors with emergency hospital admissions in Fukuoka, Japan. Int J Biometeorol 2002;46:38–41 [DOI] [PubMed] [Google Scholar]
- 22.Wang H, Matsumura M, Kakehashi M, et al. Effects of atmospheric temperature and pressure on the occurrence of acute myocardial infarction in Hiroshima City, Japan. Hiroshima J Med Sci 2006;55:45–51 [PubMed] [Google Scholar]
- 23.Abe T, Tokuda Y, Ohde S, et al. The relationship of short-term air pollution and weather to ED visits for asthma in Japan. Am J Emerg Med 2009;27:153–9 [DOI] [PubMed] [Google Scholar]
- 24.Dolney TJ, Sheridan SC. The relationship between extreme heat and ambulance response calls for the city of Toronto, Ontario, Canada. Environ Res 2006;101:94–103 [DOI] [PubMed] [Google Scholar]
- 25.Bassil KL, Cole DC, Moineddin R, et al. The relationship between temperature and ambulance response calls for heat-related illness in Toronto, Ontario, 2005. J Epidemiol Community Health 2011;65:829–31 [DOI] [PubMed] [Google Scholar]
- 26.Alessandrini E, Zauli Sajani S, Scotto F, et al. Emergency ambulance dispatches and apparent temperature: a time series analysis in Emilia-Romagna, Italy. Environ Res 2011;111:1192–200 [DOI] [PubMed] [Google Scholar]
- 27.Barnett AG, Tong S, Clements AC. What measure of temperature is the best predictor of mortality? Environ Res 2010;110:604–11 [DOI] [PubMed] [Google Scholar]
- 28.Hajat S, Kosatky T. Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health 2010;64:753–60 [DOI] [PubMed] [Google Scholar]
- 29.Yu W, Vaneckova P, Mengersen K, et al. Is the association between temperature and mortality modified by age, gender and socio-economic status? Sci Total Environ 2010;408:3513–18 [DOI] [PubMed] [Google Scholar]
- 30.Ren C, Williams GM, Tong S. Does particulate matter modify the association between temperature and cardiorespiratory diseases? Environ Health Perspect 2006;114:1690–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Stat Med 2010;29:2224–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tong S, Ren C, Becker N. Excess deaths during the 2004 heatwave in Brisbane, Australia. Int J Biometeorol 2010;54:393–400 [DOI] [PubMed] [Google Scholar]
- 33.Ye X, Wolff R, Yu W, et al. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect 2012;120:19–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ostro B, Rauch S, Green R, et al. The effects of temperature and use of air conditioning on hospitalizations. Am J Epidemiol 2010;172:1053–61 [DOI] [PubMed] [Google Scholar]
- 35.Hajat S, Haines A. Associations of cold temperatures with GP consultations for respiratory and cardiovascular disease amongst the elderly in London. Int J Epidemiol 2002;31:825–30 [DOI] [PubMed] [Google Scholar]
- 36.Falagas ME, Theocharis G, Spanos A, et al. Effect of meteorological variables on the incidence of respiratory tract infections. Respir Med 2008;102:733–7 [DOI] [PubMed] [Google Scholar]
- 37.Li Y, Du T, Lewin MR, et al. The seasonality of acute coronary syndrome and its relations with climatic parameters. Am J Emerg Med 2011;29:768–74 [DOI] [PubMed] [Google Scholar]
- 38.Hajat S, Bird W, Haines A. Cold weather and GP consultations for respiratory conditions by elderly people in 16 locations in the UK. Eur J Epidemiol 2004;19:959–68 [DOI] [PubMed] [Google Scholar]
- 39.Pudpong N, Hajat S. High temperature effects on out-patient visits and hospital admissions in Chiang Mai, Thailand. Sci Total Environ 2011;409:5260–7 [DOI] [PubMed] [Google Scholar]
- 40.Kovats RS, Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health 2008;29:41–55 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.