Abstract
Osteoarthritis (OA) is a progressive degenerative joint disease that has a major impact on joint function and quality of life. Nutraceuticals and dietary supplements derived from herbs have long been used in traditional medicine and there is considerable evidence that nutraceuticals may play an important role in inflammation and joint destruction in OA. We review the biological effects of some medicinal fruits and herbs – pomegranate, green tea, cat’s claw, devil’s claw, ginger, Indian olibaum, turmeric and ananas – in an attempt to understand the pivotal molecular targets involved in inflammation and the joint destruction process and to summarize their toxicities and efficacy for OA management. So far there is insufficient reliable evidence on the effectiveness of ginger, turmeric and ananas. Pomegranate and green tea only have preclinical evidence of efficacy due to the lack of clinical data. In vivo and clinical studies are required to understand their targets and efficacy in OA. Limited in vitro and in vivo evidence is available for cat’s claw and Indian olibaum. More extensive studies are required before long-term controlled trials of whole cat’s claw and Indian olibaum extracts, or isolated active compounds, are carried out in patients with OA to determine their long-term efficacy and safety. Devil’s claw has not been rigorously tested to determine its antiarthritic potential in in vitro and in vivo models. There is strong clinical evidence of the effectiveness of devil’s claw in pain reduction. However, high-quality clinical trials are needed to determine its effectiveness. No serious side effects have been reported for any fruits and herbs. Overall, these studies identify and support the use of nutraceuticals to provide symptomatic relief to patients with OA and to be used as adjunct therapy for OA management. More high-quality trials are needed to provide definitive answers to questions related to their efficacy and safety for OA prevention and/or treatment.
Keywords: cat’s claw, green tea, inflammation, osteoarthritis, pomegranate
Introduction
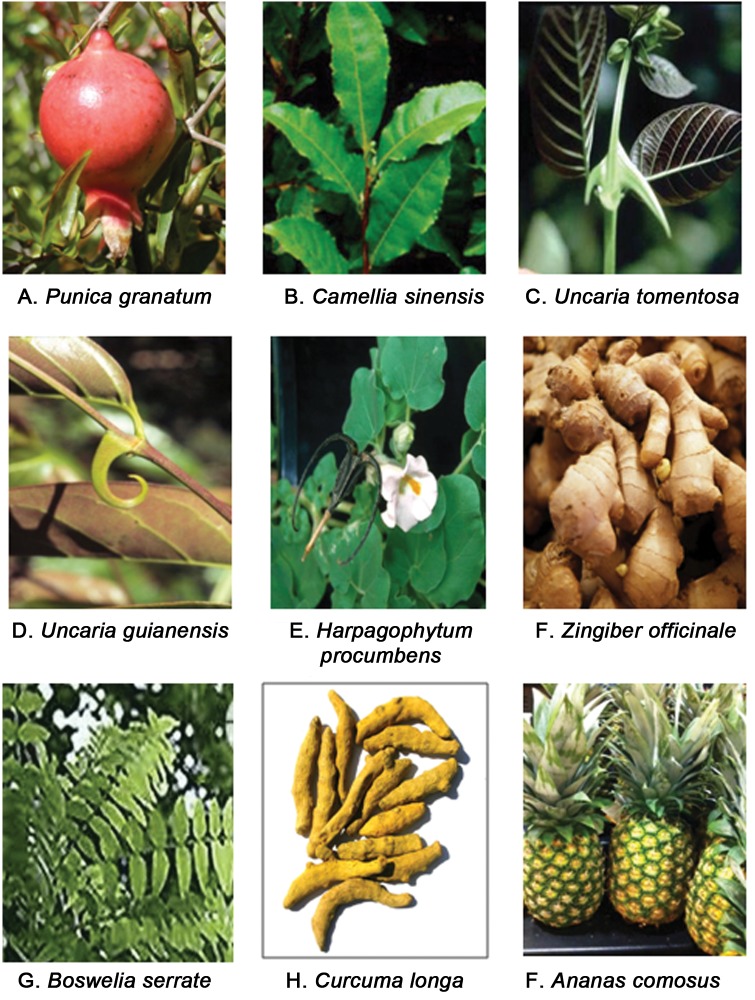
Osteoarthritis (OA) is one of the most prevalent and disabling chronic diseases affecting older people. A high prevalence of OA among older people and women and the moderate to severe impact on daily life pose a significant public health problem [Malemud et al. 2003; Yelin, 2003]. OA involves the erosion of articular cartilage, inflammation of synovial membrane, and resorption of the underlying subchondral bone [van der Kraan and van den Berg, 2000]. These pathological changes are associated with an excessive production of proinflammatory molecules such as interleukin 1β (IL-1β) and tumor necrosis factor α (TNFα), which shift the balance between the synthesis and degradation of matrix components resulting in progressive destruction of the joint tissue [van der Kraan and van den Berg, 2000]. Today, a cure for OA remains elusive. Nonpharmacological management includes physical therapy, aerobic exercises, muscle strengthening, weight reduction, walking aids, knee braces, footwear and insoles, electromagnets, thermal modalities and acupuncture. For OA treatment and prevention, glucosamine and chondroitin sulfate, two of the molecular building blocks found in articular cartilage, are the most commonly used dietary supplements. In randomized trials of variable quality, these compounds show efficacy in reducing symptoms, but neither has been shown to arrest progression of the disease or regenerate damaged cartilage [reviewed in Häuselmann, 2001; Morelli et al. 2003; McAlindon, 2006; Gregory et al. 2008]. Pharmacological management of OA has targeted symptoms of the disease rather than the underlying cause; analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) represent the mainstay of treatment [Altman, 2009]. These drugs generally decrease pain and stiffness and improve function. Although, any beneficial effects to the underlying cartilage and bone associated with the use of these drugs have not been demonstrated, they remain among the most widely prescribed drugs for OA therapy [Abramson, 2003]. Other treatment options are selective cyclooxygenase 2 (COX-2) inhibitors (rofecoxib) for pain management but these drugs are reported to be associated with gastrointestinal [Chan et al. 2010] and cardiovascular [Hsiao et al. 2009] adverse events. Matrix metalloproteinase (MMP) inhibitors have been studied for prevention of cartilage degradation but their clinical use has been limited by severe side effects [Nuti et al. 2009]. Intra-articular therapies like glucocorticoid and hyaluronan injections have been used for pain relief but recent observations suggest that they may accelerate cartilage breakdown [Gonzalez-Fuentes et al. 2010]. Basically, long-term use of available pharmacological agents to relieve OA symptoms is associated with serious adverse events and highlights the importance of developing safer alternative and prevention strategies. Such prevention and alternative/adjunct therapies could come from nutraceuticals. The term ‘nutraceutical’ was coined from ‘nutrition’ and ‘pharmaceutical’ in 1989 by DeFelice and was originally defined as ‘a food (or part of the food) that provides medical or health benefits, including the prevention and/or treatment of a disease’ [Kalra, 2003]. Zeisel distinguished whole foods from the bioactive chemical compounds derived from them and available in a nonfood matrix by using the terms ‘functional foods’ and ‘nutraceuticals’ respectively [Zeisel, 1999]. However, the term nutraceuticals has no regulatory definition and is not recognized by the US Food and Drug Administration (FDA), which uses the term ‘dietary supplements’ instead [Halsted, 2003]. OA as a chronic disease is a perfect paradigm of pathology of treatment, which could be addressed by nutraceuticals and dietary supplements. First, because nutraceuticals only have limited effects on their biological target and significant differences can be reached over time through a buildup effect in which daily benefits add up and the time window for intervention is longer in chronic diseases. Second, nutraceuticals could provide a safer alternative because generally their use is devoid of adverse effects, although this is not universal. Public interest in the benefits provided by nutraceuticals such as medicinal herbs for OA is high and 47% of older adults use nonprescribed alternative medications (dietary supplements) for OA management [Ramsey et al. 2001]. The objective of this review is to discuss the scientific evidence supporting the efficacy of Punica granatum (pomegranate fruit), Camellia sinensis (green tea), Uncaria tomentosa/Uncaria guianensis (cat’s claw), Harpagophytum procumbens (devil’s claw), Zingiber officinale (ginger), Boswellia serrata, Curcuma longa (turmeric) and Ananas comosus in an attempt to understand the pivotal molecular targets involved in inflammation and the joint destruction process and to summarize their toxicities and efficacies for OA management. We have purposely not considered use of glucosamine sulphate and chondroitin sulphate because these compounds have been the main topic of numerous recent reviews [e.g. Häuselmann, 2001; Morelli et al. 2003; McAlindon 2006; Gregory et al. 2008]. For this review a literature search was performed of the Pubmed database and the scientific data with a direct link to OA were selected. We tried to include all the relevant references but the list may not be complete. If some published work is not included, the omission is unintentional.
Punica granatum (pomegranate)
Pomegranate fruit [PF, Figure 1(A)] has been used for centuries to confer health benefits in many cultures. It is native to semitropical Asia and is now being cultivated in Afghanistan, India, China, Russia, Japan and the United States [Palaniswamy, 2003]. Modern use of PF-derived products includes treatment of AIDS [Lee and Watson, 1998], cancer [Kim et al. 2002], cosmetic use [Moayadi, 2004], allergic symptoms [Watanabe and Hatakoshi, 2002], cardiovascular conditions [Aviram and Dornfeld, 2003], oral hygiene [Kim and Kim, 2002] and as ophthalmic ointment [Bruijn et al. 2003]. Edible parts of the PF are composed of 80% juice and 20% seed [Singh et al. 2002b]. PF itself is a rich source of two types of polyphenolic compounds: anthocyanins (such as delphinidin, cyanidin, and pelargonidin) and hydrolyzable tannins (such as punicalin, pedunculagin, punicalagin, gallagic, and ellagic acid esters of glucose), which account for 92% of the antioxidant activity of the whole fruit [Singh et al. 2002b]. Anthocyanins are potent antioxidants, provide the brilliant color of the pomegranate juice, and their administration is reported to significantly decrease the malondialdehyde, hydroperoxide levels, lipid peroxidation and also enhance the activities of catalase, superoxide dismutase, glutathione peroxidase and glutathione reductase in the liver [Sudheesh and Vijayalakshmi, 2005; Gil et al. 2000; Seeram and Nair, 2002]. Punicalagin has been shown to downregulate the expression of IL-2 from anti-CD3/anti-CD28-stimulated murine splenic CD4+ T cells and suppress mixed leukocyte reaction without exhibiting cytotoxicity to the cells via inhibition of nuclear factor of activated T cells [Lee et al. 2008]. This suggests that PF could be a potential candidate for the therapeutics of immune pathologies. We reported that pomegranate fruit extract (PFE)-derived bioavailable compounds suppress COX-2 enzyme activity and IL-1β-induced prostaglandin E2 (PGE2) and nitric oxide (NO) production in OA chondrocytes [Shukla et al. 2008a]. We showed the inhibitory effects of PFE on IL-1β-induced proteoglycan breakdown in cartilage explants in vitro [Ahmed et al. 2005]. We also studied the efficacy of PFE in suppressing joint inflammation and damage using a collagen-induced arthritis mouse model. Consumption of PFE potently delayed the onset and reduced the incidence of collagen-induced arthritis in mice. Histopathology of the arthritic joints from PFE-fed mice demonstrated reduced joint infiltration by the inflammatory cells, and the destruction of bone and cartilage was alleviated with the decrease level of IL-6 [Shukla et al. 2008b]. Activation of mitogen-activated protein kinases (MAPKs) and nuclear factor (NF)-κB is intimately associated with the increased expression of critical mediators of inflammation involved in OA pathogenesis, including the expression of IL-6 and IL-8 [Marcu et al. 2010; Firestein and Manning, 1999]. We recently showed that inhibition of IL-6 and IL-8 by PFE in PMACI (phorbol-12-myristate 13-acetate plus calcium inophore A23187)-stimulated KU812 cells was mediated by inhibition of NF-κB, cJun-N-terminal kinases (JNKs) and the extracellular regulated kinase (ERK)–MAPK pathway [Rasheed et al. 2009a]. We also showed that PFE (6.25–25 mg/liter) inhibits the IL-1β-induced expression of MMP-1, MMP-3 and MMP-13 mRNA and proteins in OA chondrocytes, which was mediated by inhibiting the activation of p38-MAPK and JNK, thereby reducing the available pool of activated c-Jun and activating transcription factor 2 [Ahmed et al. 2005]. Our recent study showed that PFE inhibits the IL-1β-induced activation of MKK3 and the p38α-MAPK isoform and DNA binding activity of the runt-related transcription factor 2 in human chondrocytes [Rasheed et al. 2010]. These results provide an important insight into the molecular basis of the reported cartilage protective and arthritis inhibitory effects of pomegranate [Rasheed et al. 2010].
Figure 1.
Medicinal fruits and herbs commonly used as dietary supplements for the treatment of osteoarthritis.
Sources: Punica granatum: http://web.gccaz.edu/glendalelibrary/GLIS%20Punica%20granatum.htm; Camellia sinensis: http://www.evitamins.com/encyclopedia/assets/nutritional-supplement/green-tea/how-it-works; Uncaria tomentosa: http://www.europhyto.com/phyto-immune-defence/uncaria-tomentosa.asp; Uncaria guianensis: http://www.tradenote.net/claw_3/; Harpagophytum procumbens: http://www.agric.wa.gov.au/objtwr/imported_images/decplants/devilsclaw.gif; Zingiber officinale: http://medicinegardenwellness.com/shoppe/index.php?main_page=product_info&products_id=136; Boswellia serrata: http://www.sssbiotic.com/product/Boswellia.asp; Curcuma longa: http://realnaturals.net/real/index.php?page=shop.product_details&category_id=8&flypage=shop.flypage&product_id=24&option=com_virtuemart&Itemid=42; Ananas comosus: http://www.virboga.de/video/pics/Ananas_comosus_001802.jpg
Repeated administration of high doses of PFE or its constituents ellagitannin and punicalagin to rats resulted in no toxicity in the dosages commonly used in traditional medicine systems [Cerdá et al. 2003]. An acute supplementation with PFE containing 330 mg of punicalagins and 22 mg of ellagic acid in 11 healthy volunteers led to the detection of ellagitannin metabolites, including ellagic acid, urolithin A, hydroxyl urolithin A, urolithin B, urolithin A glucuronideet and dimethyl ellagic acid glucuronide in plasma after 2–24 h [Mertens-Talcott et al. 2006]. In healthy human volunteers who consumed 180 ml of a commercially available pomegranate juice containing 25 mg of ellagic acid, ellagic acid was detected at a maximum concentration of 32 ng/ml in the plasma after 1 h [Seeram et al. 2004]. We also showed that ellagic acid becomes bioavailable 2 h after oral ingestion of PFE [Shukla et al. 2008b]. Ellagic acid has been reported to inhibit the activation of NF-κB and the production of inflammatory mediators [Choi and Yan, 2009].
Overall, these data indicate that consumption of PF may be beneficial and of value in developing adjunct preventive and/or therapeutic approaches to the prevention and treatment of OA. However, clinical trials showing the benefit of pomegranate fruit or its extracts on inflammation and OA are lacking. Based on published evidence, further in vivo evaluation and clinical testing for the efficacy of PF in OA are needed [Khalifé and Zafarullah, 2011].
Camellia sinensis (green tea)
Tea is a widely consumed beverage throughout the world and is reported to possess significant health-promoting effects (reviewed by Cabrera and colleagues and reference therein) [Cabrera et al. 2006]. Green tea [Figure 1(B)] contains proteins (15%), amino acids (4%), fiber (26%), other carbohydrates (7%), lipids (7%), pigments (2%), minerals (5%), and phenolic compounds (catechins; 30%). The principal catechins found in green tea are epicatechin (6.4%), epicatechin-3-gallate (13.6%), epigallocatechin (19%) and epigallocatechin-3-gallate (EGCG; 59%), and account for 30–40% of its dry weight [Cabrera et al. 2006]. Green tea catechins, especially EGCG, have been reported to have antimutagenic [Cheng et al. 2009], anticancer [Johnson et al. 2010], antidiabetic [Zhang et al. 2010], anti-inflammatory [Danesi et al. 2010], antibacterial [Osterburg et al. 2009], antiviral [Xiao et al. 2008], antiobesity [Moon et al. 2007] and neuroprotective effects [Smith et al. 2010]. The strong antioxidant activity of green tea catechins has been widely demonstrated in vitro and in vivo [reviewed in Cabrera et al. 2003, 2006; Frei and Higdon, 2003]. Several studies have shown that EGCG blunts reactive oxygen species (ROS)-mediated cytotoxicity in human chondrocytes [Lo et al. 1996]. EGCG has been reported to increase the activities of catalase, superoxide dismutase, and glutathione peroxidase, which are essential components of a robust antioxidant defense system [Meng et al. 2001]. The potential disease-modifying effects of green tea on arthritis came to light through our study, when in a mouse model of rheumatoid arthritis (RA) induction and severity of arthritis was ameliorated by the prophylactic administration of green tea polyphenols in drinking water [Haqqi et al. 1999]. The anti-inflammatory and antiarthritic effects of EGCG are supported by several studies, indicating that green tea or its component EGCG can regulate the expression of cytokines, chemokines, MMPs, aggrecanase, ROS, NO, COX-2, and PGE2 in cell types relevant to the pathogenesis of OA [reviewed in Singh et al. 2010; Akhtar and Haqqi, 2011]. We recently studied the global effect of EGCG on IL-1β-induced expression of cytokines and chemokines associated with OA pathogenesis in human chondrocytes. Our results suggest that the potential of EGCG in OA treatment and prevention may be related to its ability to globally suppress the IL-1β-induced inflammatory response in human chondrocytes [Akhtar and Haqqi, 2011]. Similarly, others have shown the inhibitory effects of EGCG on IL-1β, TNFα, IL-6, regulated upon activation normal T-cell expressed and secreted (RANTES), monocyte chemotactic protein 1, epithelial neutrophil activating peptide-78, and growth-related oncogene α expression in RA synovial fibroblasts and other cell types [Shen et al. 2009; Shin et al. 2006; Ahmed et al. 2006]. NF-κB and MAPKs are involved in the regulation of genes important in high expression of several mediators of inflammation in OA [Marcu et al. 2010; Firestein and Manning, 1999]. EGCG has been reported to downregulate IL-6 expression by inducing alternative splicing of gp130 mRNA resulting in enhanced sgp130 production in RA synovial fibroblasts [Ahmed et al. 2008]. High levels of nitrates/nitrites have been found in the synovial fluid and serum of patients with OA [Farrell et al. 1992]. Studies from our laboratory have shown that EGCG inhibits NO production in IL-1β-stimulated human OA chondrocytes by suppressing the expression of inducible nitric oxide synthase (iNOS) mRNA, which was mediated in part by inhibition of NF-κB/p65 [Singh et al. 2002a, 2003]. COX-2 is the rate limiting enzyme in the production of PGE2 and we reported that EGCG inhibited the PGE2 production via inhibition of COX-2 expression in IL-1β-stimulated human OA chondrocytes [Ahmed et al. 2002]. However, Koeberle and colleagues reported that microsomal prostaglandin-E synthase 1 (mPGES-1) is a molecular target of EGCG, and inhibition of mPGES-1 is seemingly the predominant mechanism underlying suppression of cellular PGE2 biosynthesis by EGCG in vitro [Koeberle et al. 2009]. Age-related accumulation of advance glycation end products (AGEs) produced by the nonenzymatic glycation of macromolecules could be an important contributing factor for the development of OA. We recently reported that EGCG inhibited AGE-stimulated expression and production of TNFα and MMP-13 and this inhibitory effect was mediated at least in part via suppression of p38-MAPK, JNK, and NF-κB activation in human OA chondrocytes [Rasheed et al. 2009b]. EGCG has also been reported to inhibit the degradation of human cartilage proteoglycan and type II collagen and selectively inhibit the expression of ADAMTS-1,-4 and -5 (A Disintegrin And Metalloproteinase with Thrombospondin Motifs), which are known to cleave aggrecan [Vankemmelbeke et al. 2003]. Previously we showed that EGCG significantly inhibited the expression and activities of MMP-1 and MMP-13 in OA chondrocytes at physiologically achievable doses [Ahmed et al. 2004]. We and others have also shown that EGCG inhibits NF-κB activation by inhibition of proteosome activity, inhibition of IκB-α phosphorylation or inhibition of IKK-β kinase activity in human OA chondrocytes [Singh et al. 2002a; Andriamanalijaona et al. 2005; Rasheed et al. 2009b]. We have also shown that EGCG selectively inhibited IL-1β-induced activation of JNK, without significantly inhibiting the phosphorylation of p38-MAPK or ERK p44/ p42 in human OA chondrocytes [Singh et al. 2003]. Activator protein (AP)-1 transcription factor is a heterodimer of Jun and Fos proteins and plays an important role in the inflammatory response [Okamoto et al. 2008]. EGCG was found to inhibit the activation and DNA binding activity of AP-1 in human OA chondrocytes [Andriamanalijaona et al. 2005; Ahmed et al. 2002].
Tea consumption in general has not displayed any acute or chronic toxic effects, and in fact, it is health promoting. Schwarz and colleagues described regular tea drinkers as people with a generally healthy lifestyle [Schwarz et al.1994]. However, harmful effects of ‘overconsumption’ of green tea cannot be ruled out and could be due to two main factors: caffeine content, and the presence of aluminum [Bruneton, 2001; Minoia et al. 1994]. Due to their relatively low absorption, rapid metabolism and elimination from the body, consumption of large amounts of flavonols is well tolerated by humans. At present the safe upper limit for chronic ingestion is about 1 g of flavonols/day [de Mejia et al. 2009]. The health benefits of tea consumption in preventing cancer have been intensively investigated [Khan and Mukhtar, 2008]. However, limited information is available about the protective effect of consumption of green tea or its bioactive components in OA. The bioavailability of EGCG or other catechins is relatively low and this may be due to the short half life, which ranges from 1.87 to 4.58 h for a 50–1600-mg dose (approximately 0.7–23 mg/kg body weight, based on 70 kg body weight) [Ullmann et al. 2003]. This might be overcome by repeated administration of EGCG because of its reported low toxicity and high tolerance by humans, even when given in doses as high as 1600 mg [van het Hof et al. 1999], which can achieve a maximum human plasma level of 7.6 μmol/liter [Ullmann et al. 2003]. These studies point out that a pharmaceutically prepared formulation of green tea catechins could reach plasma levels equivalent to effective in vitro doses and can be used as adjunct therapy for the treatment and prevention of OA [Katiyar and Raman, 2011]. Currently, there is sufficient in vitro and in vivo data available showing the anti-inflammatory and antiarthritic potential of green tea and its constituent EGCG. Hence, more in vivo and clinical studies are required to evaluate its efficacy for OA.
Uncaria tomentosa and Uncaria guianensis (cat’s claw)
Cat’s claw is a vine from the basin of the Amazon River. There are two species, U. tomentosa [Figure 1(C)] and U. guianensis [Figure 1(D)] that are traditionally used in South America for their anti-inflammatory properties. Cat’s claw bark contains oxindole alkaloids (virtually absent in U. guianensis), polyphenols (flavonoids, proanthocyanidins, and tannins), quinovic acid α-glycosides, pentacyclic alkaloids, and sterols [Ganzera et al. 2001]. Traditionally, the bark of cat’s claw is prepared as a decoction, said to be beneficial in the treatment of arthritis, bursitis, lupus, chronic fatigue syndrome, and for stomach and intestine disorders [Foster, 1996; reviewed in Williams, 2001]. The most investigated of the active constituents in U. tomentosa extract for immune-modulating and anti-inflammatory effects are pentacyclic oxindole alkaloids [Williams, 2001]. However, the antioxidant and anti-inflammatory effects of the extracts of U. tomentosa and U. guianensis appear to be independent of their alkaloid content as in several assays both species of Uncaria were reported to be a strong free radical scavenger [Sandoval et al. 2000, 2002; reviewed in Rosenbaum et al. 2010]. We reported that U. guianensis in combination with Lepidium meyenii had chondroprotective properties in human cartilage. This action was mediated in part through upregulation of gene expression of the anabolic insulin-like growth factor 1 in IL-1β-stimulated chondrocytes [Miller et al. 2006]. Pretreatment with a hydroalcholic extract (500 μg/ml) of U. tomentosa inhibited COX-1 and COX-2 via inhibition of the activation of NF-κB in Jurkat T cells [Aguilar et al. 2002]. Uncaria has been found to inhibit lipopolysaccharide (LPS)-induced iNOS gene expression, TNFα, PGE2 and NO production, and cell death via inhibiting the activation of NF-κB [Sandoval-Chacón et al. 1998; Allen-Hall et al. 2010].
Recent studies support the use of Uncaria alone or in combination with other medicinal herbs for OA management [Piscoya et al. 2001; Miller et al. 2005; Mehta et al. 2007]. The available animal toxicological data did not indicate any severe toxicity by the oral intake of Uncaria [Piscoya et al. 2001; Valerio and Gonzales, 2005]. In some cases, mild nausea and diarrhea may occur upon ingestion of crude extracts [Piscoya et al. 2001; Santa Maria et al. 1997]. Several other groups have documented the safety and pharmacological profile of cat’s claw in animal models and also showed that cat’s claw was non-toxic in vitro [Williams, 2001; Sandoval et al. 2002; Fetrow and Avila, 1999 and references therein]. Although in recommended dosages use of cat’s claw is considered nontoxic, this aspect has not been rigorously investigated. Piscoya and colleagues evaluated the safety and side effects of U. guianensis extract in patients with OA of the knee [Piscoya et al. 2001]. Pain associated with activities of daily living was significantly reduced, however pain at rest or at night was not reduced during this 4-week trial period. In another study, a combination of a natural mineral supplement (Sierrasil, Sierra Mountain Minerals Inc., Bozeman, MT, USA) with a cat’s claw extract (Vincaria, Rainforest Nutritionals Inc., Raleigh, NC, USA) showed therapeutic potential in mild to moderate knee OA [Miller et al. 2005]. The Western Ontario and McMaster Universities Arthritis Index (WOMAC) and visual analog scale (VAS) scores were improved after 8 weeks compared with placebo. Rescue medication use was 28–23% lower in the herbomineral combination. Comparison of Reparagen (Rainforest Nutritionals, Inc., Raleigh, NC, USA) (1800 mg/day), a mixture of U. guianensis and L. meyenii with glucosamine sulfate (1500 mg/day) was also studied in patients with OA in a multicenter, randomized, double-blind trial. Reparagen and glucosamine sulfate produced substantial improvements in pain, stiffness and function in patients with mild to moderate OA as evidenced by improved WOMAC and VAS scores [Mehta et al. 2007]. More extensive studies employing animals and in vitro models are required before long-term controlled trials of Uncaria extracts (Table 1), or active compounds therein, can be initiated in a large number of human subjects to determine their long-term efficacy and safety profile.
Table 1.
Summary of clinical trials on neutraceuticals and evidence of their safety and efficacy.
| References | Product | Dose and comparator | Design and duration | Study population | Other outcome reported | Side effects |
|---|---|---|---|---|---|---|
| Uncaria tomentosa and Uncaria guianensis (cat’s claw) | ||||||
| [Piscoya et al. 2001] | Aqueous extract of cat’s claw bark (U. guianensis) | Treatment group (1 capsule 100 mg/ day). Placebo group 100 mg excipients without cat’s claw | Multicenter randomized double-blind placebo-controlled trial, 4 weeks | Men with OA aged 45–75 with grade II–III of Kellgren/Lawrence classification (n = 45; placebo group n = 15, treatment group n = 30) | Effective in knee OA (improvement in pain, disease indices) | No change in safety parameters and frequency of side effects (vomiting, dizziness and headache) were no different between groups |
| [Mehta et al. 2007] | Reparagen, a blend of two natural products – Vincaria (300 mg; U. guianensis) and RNI 249 (1500 mg; Lepidium meyenii) | Treatment 1800 mg as two capsules twice a day. Glucosamine sulfate (1500 mg; comparator) | Multicenter randomized double-blind trial with positive control, 8 weeks | Patients with OA (n = 95) men and women, Indian population >20 years of age, grade II–III of Kellgren/Lawrence classification and a baseline functional assessment of overall pain of at ≥40 mm and ≤80 mm on a 100 mm VAS score | Glucosamine (89%) and Reparagen (94%) showed substantial reduction in pain and significant benefits in WOMAC and VAS (45–62% reduction). Rescue medication use was significantly lower in the Reparagen group at each assessment period | Tolerability was excellent, no serious adverse events were noted and safety parameters were unchanged. Serum IGF-1 levels were unaltered by treatments |
| [Miller et al. 2005] | Sierrasil, a natural mineral product with or without Vincaria (containing U. guianensis extract) | High-dose Sierrasil (3 g/day), low-dose Sierrasil (2 g/day), low-dose Sierrasil (2 g/day) + Vincaria (100 mg/day) and placebo | Multicenter randomized double-blind placebo-controlled trial, 8 weeks | Patients with OA (n = 107), men and women, Indian population >20 years of age, grade II–III of Kellgren/Lawrence classification and a baseline functional assessment of overall pain of at ≥50 mm on a 100 mm VAS score | Combination of Sierrasil and Vincaria was effective in relief of OA symptoms (improved physical activity, VAS pain score) and 28% reduction in rescue medication (paracetamol) was observed | Tolerability was good for all groups, no serious adverse events were noted and safety parameters remained unchanged |
| Zingiber officinale (ginger) | ||||||
| [Bliddal et al. 2000] | EV.ext-33 ginger extract | Ginger extract (170 mg). Iboprofen (400 mg; comparator) as placebo, two capsules twice a day. Rescue medication acetaminophen 3 g/day throughout study | Randomized double-blind double-dummy placebo-controlled crossover study with a wash-out period of 1 week followed by 3 treatment periods in a randomized sequence, each of 3 weeks | Hip OA (n = 20) and knee OA (n = 36), aged 24–87 years, men and women (15:41) | Ranking of efficacy of three treatment periods for VAS and the Lequesne Functional Index was Ibuprofen>ginger extract>placebo Statistically significant effect of ginger extract was only demonstrated by explorative statistical methods in the first period of treatment before crossover, while a significant difference was not observed in the study as a whole | No serious adverse events reported during the periods with active medications |
| [Altman and Marcussen, 2001] | EV.EXT 77 highly concentrated extract of 2 ginger species, Z. officinale and Alpinia galanga | Ginger extract (each capsule contained 255 mg of EV.EXT 77, extracted from 2,500–4,000 mg of dried ginger rhizomes and 500–1,500 mg of dried galanga rhizomes) versus placebo daily | Randomized double-blind placebo-controlled multicenter parallel-group trial, 6 weeks | Knee OA (n = 247), moderate to severe pain, aged 45–72 years, men and women. Patients had to show OA grade II–IV of Kellgren/Lawrence classification | In 247 evaluated patients there was a reduction in knee pain on standing in ginger extract group compared with placebo (63% versus 50%). Secondary efficacy variables also showed reduction in knee pain on standing (24.5 versus 16.4 mm), reduction in knee pain after walking 50 ft (15.1 versus 8.7 mm), and reduction in the WOMAC OA index (12.9 versus 9.0 mm. Reduction in intake of rescue medication (acetaminophen) in the ginger extract group. | Good safety profile, with mostly mild GI adverse events in the ginger extract group compared with placebo group (59 patients versus 21 patients). |
| Boswellia serrata (Indian olibaum) | ||||||
| [Kulkarni et al. 1991] | Articulin-F, herbomineral formulation containing roots of Wifhania somnifera (450 mg), the stem of B. serrata (100 mg), rhizomes of Curcuma longa (50 mg) and a zinc complex(50 mg) | Articulin-F, two capsules every 8 h | Randomized double-blind placebo-controlled crossover study, 3 months. After a 15-day wash-out period the patients were transferred to the other treatment for a further period of 3 months | Patients with OA (n = 42) aged 48–50 years, men and women (10:32) | Treatment with the herbomineral formulation significantly altered only the severity of pain and disability score. Other parameters, including morning stiffness, Ritchie Articular Index, grip strength and joint score, showed favorable changes but were not statistically significant. Out of 42 patients, 39 preferred the herbomineral preparation, two the placebo and one was equivocal | Safety parameters were unchanged. Two patients complained of nausea, three with dermatitis and three with pain in the abdomen |
| [Kimmatkar et al. 2003] | B. serrata extract (333 mg) containing 65% organic acids or minimum 40% total boswellic acids | Boswellia serrata extract (300 mg/capsule). Placebo group starch powder (333 mg) three times a day | Randomized double-blind placebo-controlled crossover study, 8 weeks | Patients with knee OA (n = 30), aged 45–72 years, men and women (12:18) | Reduced joint pain and swelling and improved the loss of function in terms of increased knee flexion, stair climbing and walking distance. No change was observed radiologically | Boswellia serrata was well tolerated except for minor GI complaints, including loose motions in one patient, epigastric pain and nausea in one patient. |
| [Sengupta et al. 2008] | 5-Loxin, a novel B. serrata extract enriched with 30% 3-O-acetyl-11-keto-beta-boswellic acid | 100 mg (n = 25) or 250 mg (n = 25) of 5-Loxin or a placebo (n = 25) daily | Randomized double-blind placebo-controlled trial, 90 days | Patients with knee OA (n = 75) aged 45–72 years, men and women. Severity was measured using VAS, WOMAC pain score and the Lequesne Functional Index | Both doses of 5-Loxin conferred significant improvements in pain and physical function scores, significant reduction in synovial fluid matrix metalloproteinase-3 | Safety parameters were almost unchanged in the treatment groups compared with placebo |
| [Sengupta et al. 2010] | BE-30 (5-Loxin; 30% 3-O-acetyl-11-keto-β-boswellic acid) and Aflapin novel synergistic composition of O-acetyl-11-keto-β-boswellic acid and B. serrata, nonvolatile oil | 100 mg (n = 20) of 5-Loxin or 100 mg (n = 20) of Aflapin or a placebo (n = 20) daily for 90 days | Randomized double-blind placebo-controlled trial, 90 days | Patients with moderate to mild knee OA (n = 60) aged 40–80 years, both men and women. Severity was measured using VAS, WOMAC pain score and the Lequesne Functional Index | 5-Loxin and Aflapin conferred clinically and statistically significant improvements in pain scores and physical function scores. Significant improvements in functional ability after 7 days with 100 mg Aflapin. Aflapin exhibited better efficacy compared with 5-Loxin | Safety parameters were unchanged compared with placebo group |
| Curcuma longa (turmeric) | ||||||
| [Kulkarni et al. 1991] | Articulin-F, a herbomineral formulation containing roots of W. somnifera (450 mg), the stem of B. serrata (100 mg), rhizomesof C. longa (50 mg) and a zinc complex (50 mg) | Articulin-F, two capsules every 8 h | Randomized double-blind placebo-controlled crossover study, 3 months. After a 15-day wash-out period the patients were transferred to the other treatment for a further period of 3 months | Patients with OA (n = 42), aged 48–50, men and women (10:32) | Treatment with the herbomineral formulation significantly altered only the severity of pain and disability score. Other parameters, including morning stiffness, Ritchie Articular Index, grip strength and joint score, showed favorable changes but were not statistically significant. Out of 42 patients, 39 preferred the herbomineral preparation, two the placebo and one was equivocal. | Safety parameters were unchanged. Two patients complained of nausea, three had dermatitis and three had pain in the abdomen |
| Harpagophytum procumbens (devil’s claw) | ||||||
| [Bélaiche, 1982] | Harpagophytum extract (3000 mg) | Harpagophytum extract 3000 mg and 9000 mg/day containing herpagoside concentration of 90–270 mg/day | Observational 12–24 week study | Primary and secondary OA of knee, hip, finger and spine, men and women (n = 630) | Dependent on the condition and dosage. Improvement seen 14.9–56.2% in patients at 3000 mg/day dose; and 13.9–39.08% at 9000 mg/day dose | Mild GI disturbances reported |
| [Lecomte and Costa, 1992] | Harpagophytum extract (2010 mg) | Harpagophytum extract (2010 mg) versus placebo group containing herpagoside concentration of 60 mg/day | Randomized double blind placebo-controlled trial, 8 weeks | Patients with OA (n = 89) | Significant decrease in VAS pain score compared with placebo group after day 30 and 60. Significant improvement in mobility | No adverse effect reported. Safety profile normal |
| [Schmelz et al. 1997] | Harpagophytum extract (2500 mg) | Harpagophytum extract (2500 mg containing herpagoside concentration of 30 mg/day) versus placebo group | Randomized double blind placebo-controlled trial, 30 days | Patients with OA with chronic back pain and myalgia (n = 100). Severity was measured using a Likert scale | Harpagophytum extract showed better results than placebo group. Out of all treated patients six showed strong pain and one mild pain compared with placebo, for which 32 had strong pain and nine medium pain | Safety parameters were unchanged compared with placebo group |
| [Rutten and Schafer, 2000] | Harpagophytum extract (960 mg) | Harpagophytum extract (960 mg/day) plus twice weekly injection | Observational 6-week study | Patients (n = 99) with acute and chronic spinal disorder (n = 23) and OA of knee (n = 76) | 68% of patients were pain free with significant reduction in symptoms | Good tolerability |
| [Leblan et al. 2000] | H. procumbens extract (2610 mg) | Harpagophytum extract (2610 mg/day containing herpagoside concentration of 57 mg/day). Diacerhein (100–150 mg/day; comparator) | Multicenter randomized double-blind parallel-group study, 16 weeks | OA of hip and knee (n = 122). Severity was measured using VAS pain score | Harpagophytum extract was equally effective as diacerhein | Significantly lower adverse effects in Harpagophytum extract treated group compared to Diacerhein. Most common adverse complications were diarrhea and flatulence. |
| [Chantre et al. 2000] | Harpadol containing cryoground powder H. procumbens (435 mg) | Harpadol group (6 capsules/day). Diacerhein (100 mg/day; comparator) | Randomized double-blind multicenter study, 4 months | Patients with OA of knee or hip (n = 122), aged 30–79 years, had to show grade I–III on the Kellgren/Lawrence classification, a baseline functional assessment of overall pain of ≥50 mm on a 100 mm VAS and a score of at least 4 on the Lequesne Functional Index | Spontaneous pain showed a significant improvement and reduction in the Lequesne Functional Index in both groups. No significant difference in efficacy between the two groups. Harpadol group used significantly less NSAIDs and antalgic drugs | The adverse effect reported was diarrhea, which was low in the Harpadol group (8.1%) compared with the diacerhein group (26.7%) |
| [Frerick et al. 2001] | Harpagophytum extract (960 mg) | Harpagophytum extract (960 mg/day containing herpagoside concentration of 30 mg/day) versus placebo group | Randomized double-blind placebo-controlled trial, 20 weeks | OA of hip (n = 46). Severity was measured using WOMAC pain intensity | Significant improvement in WOMAC and stiffness scores in treatment group compared with placebo | An adverse reaction of one patient in treatment group, epigastric discomfort with suspected cholelithiasis |
| [Chrubasik et al. 2002] | Doloteffin a proprietary Harpagophytum extract (60 mg tablets) | Doloteffin (60 mg) two tablets three times a day. Back group with nonspecific pain, knee OA pain group and hip OA pain group. Patients were allowed to continue with their concomitant treatments and to supplement medication with other analgesics | Observational 8-week study (post-market surveillance of the effectiveness and safety) | Total patients (n = 250) with nonspecific low back pain (n = 104) or OA pain in the knee (n = 85) or hip (n = 61). Men (30%) and women (70%). Severity was measured using Arhus Low Back Pain Index, WOMAC index | Multivariate analysis confirmed that in all groups, the generic and disease-specific outcome measures improved by week 4 and further by week 8. Hip group tended to improve more than the back group. Improvement in the knee group was less than the back group. Back patients who required NSAIDs during the 8 weeks used significantly more per patient than other two groups | About 10% of the patients suffered from minor adverse events that could possibly have been attributable to Doloteffin. Between 50% and 70% of the patients benefited from Doloteffin with few adverse effects |
| [Warnock et al. 2007] | Harpagophytum extract tablets (480 mg) | Harpagophytum extract tablets twice daily | Single group open study, 8 weeks | Mild to moderate rheumatic disorder having pain (rated 2–7 on 10-point scale) including patients with OA (n = 222), men (n = 82) and women (n = 140), aged 18–75 years. Effectiveness was assessed by numeric rating scales, WOMAC Index and the Algofunctional Hand Osteoarthritis Index and quality of life was measured by SF-12 | Improvements in patient assessment of global pain, stiffness, function and quality of life. Reductions in mean pain scores for hand, wrist, elbow, shoulder, hip, knee and back pain. 60% of patients either reduced or stopped concomitant pain medication | No serious adverse events were reported and all were moderate GI complaints |
| Ananas comosus | ||||||
| [Tilwe et al. 2001] | Phlogenzyme (contains the proteolytic enzymes bromelain, trypsin and rutin) | Bromelain (1890 mg/day). Diclofenac (100–150 mg/day; comparator) | Prospective randomized controlled single-blind study with positive control, 7 weeks | Patients with knee OA (n = 50) aged 40–75 years | Equivalence not tested. Reduction in pain, tenderness and swelling in both groups | Well tolerated, no specific adverse events reported |
| [Klein and Kullich, 2000] | Phlogenzyme | Bromelain (540 mg/day). Diclofenac (100–150 mg/day; comparator) | Randomized double-blind trial with positive control, 4 weeks | Patients with knee OA (n = 73) | Reduction in pain indices by 80% at 4 weeks post treatment | No serious adverse events reported |
| [Singer et al. 2001] | Phlogenzym | Bromelain (540 mg/day). Diclofenac (100–150 mg/day; comparator) | Randomized double-blind controlled trial with positive control, 4 weeks | Patients with knee OA | Bromelain group showed reduction in pain score compared with diclofenac | No serious adverse events reported |
| [Brien et al. 2006] | Bromelain | Bromelain (800 mg/day) or placebo group | Randomized double-blind placebo-controlled trial, 12 weeks | Patients with moderate to severe knee OA (n = 47). Severity was measured using WOMAC and SF-36 questionnaires | No statistically significant differences were observed between groups for the primary outcome nor the WOMAC subscales or SF-36 | Adverse events were generally mild in nature |
GI, gastrointestinal; IGF-1, insulin-like growth factor 1; NSAID, nonsteroidal anti-inflammatory drug; OA, Osteoarthritis; SF-36, 36-item Short Form Health Survey; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
Harpagophytum procumbens (devil’s claw)
For more than 50 years preparations of H. procumbens [devil’s claw, Figure 1(E)] have been used in Europe for the treatment of rheumatic entities. Devil’s claw is native to the southern part of the African continent and may be found in Namibia, Botswana, South Africa, Angola, Zambia, and Zimbabwe [Anonymous, 2008; Qi et al. 2006]. Historically, devil’s claw has been used as an analgesic, for fevers and allergies, appetite stimulation, wounds and skin rashes, dyspepsia, liver and kidney disorders, as diuretic and sedative, and to treat degenerative disorders of the musculoskeletal system [Blumenthal, 1998; Stewart and Cole, 2005; Qi et al. 2006; Ragusa et al. 1984]. The major chemical constituents of devil’s claw are iridoid glycosides (primarily harpagoside, harpagide, and procumbide), sugars (mainly the tetrasaccharide, stachyose), triterpenoids (oleanolic and ursolic acid), phytosterols (primarily β-sitosterol), aromatic acids (caffeic, cinnamic, and chlorogenic acids), and flavonoids such as luteolin and kaempferol [Bradley, 1992]. Harpagoside, harpagide, and procumbide, found in the tubers of the plant, appear to be the most therapeutically important constituents. Whole-plant extracts appear to have a better therapeutic effect than those prepared from isolated parts [Qi et al. 2006]. A large body of evidence indicates that devil’s claw may be an effective treatment for OA because of its pain-relieving and anti-inflammatory actions. Higher concentrations of serum oxygen-free radicals prevalent with arthritis may alter the oxidant/antioxidant balance, thus facilitating lipid peroxidation and leading to tissue damage [Jaswal et al. 2003]. Devil’s claw extract has been shown to increase superoxide dismutase, catalase, glutathione peroxidase enzyme activities in a dose-dependent manner and a reduction in lipid peroxidation was also noted in vivo, which contribute to its antioxidant effects [Bhattacharya and Bhattacharya, 1998]. The flavonoids and plant phenols present in devil’s claw extracts may be the constituents responsible for the observed antioxidant activity [Dugas et al. 2000; Sawa et al. 1999]. Devil’s claw has been found to scavenge both superoxide and peroxyl radicals [Langmead et al. 2002]. A recent study also showed that both root tuber extract of devil’s claw and tincture are effective as free radical scavengers and inhibit LPS-induced nitrite levels in RAW 264.6 macrophages [Grant et al. 2009]. Significant antioxidant effects by an aqueous extract of devil’s claw and by the flavonoid constituents lutteolin and kaempferol have also been noted [Betancor-Fernández et al. 2003]. A dried aqueous extract (5 and 10 mg/kg) of devil’s claw has been shown to exert a significant dose-dependent analgesic and anti-inflammatory effect in rats. However, carrageenan-induced paw edema was not affected by harpagoside, suggesting harpagoside may not have an anti-inflammatory effect at least in the doses used in vivo [Lanhers et al. 1992]. In vitro data also demonstrated that the active principle (sum of coactive constituents) of devil’s claw inhibits not only inflammatory mediators such as iNOS and COX-2 mediated PGE2 production [Fiebich et al. 2001; Jang et al. 2003; Huang et al. 2005] or leukotriene release [Loew et al. 2001] but also mediators of cartilage destruction, such as TNFα, IL-1β, IL-6, MMPs, NO [Fiebich et al. 2001; Huang et al. 2005; Schulze-Tanzil et al. 2004a], and elastase [Boje et al. 2003]. Reported chondroprotective effects of devil’s claw may be due to suppression of NF-κB activation, thereby inhibiting inflammation [Huang et al. 2005].
Devil’s claw extract appears to be safe when used in appropriate dosages. The side effects are few, usually limited to gastrointestinal upset, dyspepsia and loss of taste; no long-term toxicities or drug-interactions are known [Vlachojannis et al. 2008]. Devil’s claw extract exerts a peripheral analgesic effect as it has been demonstrated to decrease pain in knee and hip OA [reviewed in Ameye and Chee, 2006; Chrubasik et al. 2002; Chantre et al. 2000]. The effectiveness of certain devil’s claw preparations has been tested with a daily dose of 360 mg of harpagoside (a coactive ingredient) in the treatment of painful OA of the hip, knee and nonspecific low back pain. Multivariate analysis confirmed that in all groups, both the generic and disease-specific outcome measures improved by week 4 and further by week 8 [Chrubasik et al. 2002]. H. procumbens powder was equally effective as diacerhein in reducing pain as measured using a 100 mm VAS. This study constitutes moderate evidence that 4 months’ daily use of 2610 mg H. procumbens powder is not significantly different from 100 mg diacerhein, producing comparable improvements in pain [Leblan et al. 2000]. Studies on devil’s claw extracts, containing 50–100 mg harpagoside daily, have shown the best results [Brien et al. 2006]. In a clinical study, 89 patients with OA were randomized to receive placebo or devil’s claw at a total daily dose of 2010 mg/day for 8 weeks. The study identified that after 30 and 60 days of treatment, patients who received devil’s claw had a significant reduction in pain (p = 0.018 after 30 days and p = 0.012 after 60 days of treatment) compared with placebo [Lecomte and Costa, 1992]. Effectiveness, safety and tolerability of Harpagophytum was studied in rheumatic disorders including OA for 8 weeks (259 patients). There were statistically significant (p < 0.0001) improvements in patient assessment of global pain, stiffness, function and quality of life. There were also statistically significant reductions in mean pain scores for hand, wrist, elbow, shoulder, hip, knee and back pain [Warnock et al. 2007]. Numerous trials have been conducted using several devil’s claw extracts for OA (Table 1 and rheumatism [Rutten and Schafer, 2000; Bélaiche,1982; Lecomte and Costa, 1992; Schmelz et al.1997; Frerick et al. 2001; Chrubasik et al. 2002; Chantre et al. 2000; Leblan et al. 2000; Warnock et al. 2007]. Unfortunately, the results of many of the studies are of questionable value because of methodological flaws. However, devil’s claw appears to be effective in the reduction of pain. More high-quality trials are needed to assess the effectiveness and efficacy of devil’s claw to determine whether this is a beneficial remedy for the treatment of OA.
Zingiber officinale (ginger)
Ginger, the rhizome of Z. officinale [Figure 1(F)], is one of the most widely used species of the ginger family (Zingiberaceae) and is a common condiment for various foods and beverages. Ginger has a long history of medicinal use dating back 2,500 years in China and India for conditions such as headaches, motion sickness, nausea, vomiting, vascular conditions, cold and arthritis, and as a antimicrobial and antifungal [reviewed in White, 2007; Afzal et al. 2001]. Characterized in traditional Chinese medicine as spicy and hot, ginger is claimed to warm the body and treat cold extremities, improve a weak and tardy pulse, address a pale complexion, and strengthen the body after blood loss [Chang et al. 1995]. The major constituents of ginger include volatile oils, oleoresin (gingerol), linoleic acid and trace elements such as magnesium, phosphorus, and potassium. The pungent phenolic constituent of ginger, [6]-gingerol, inhibited LPS-induced iNOS expression and production of NO and other reactive nitrogen species in macrophages and blocked peroxynitrite-induced oxidation and nitration reactions in vitro [Ippoushi et al. 2003]. These results suggest that [6]-gingerol is a potent inhibitor of NO synthesis and also an effective protector against peroxynitrite-mediated damage. Another in vitro study showed that ginger extract was effective in inhibiting the production of PGE2, TNFα, and COX-2 expression in human synoviocytes by regulating NF-κB activation and degradation of its inhibitor IkB-α [Thomson et al. 2002]. Similarly, ginger extract decreased the IL-1β and LPS-induced production of NO and PGE2 in OA cartilage [Shen et al. 2003]. It has also been reported to decrease the IL-1β-induced expression of TNFα expression and TNFα-induced production of COX-2 and activation of NF-κB in synoviocytes [Frondoza et al. 2004]. Use of ginger extract also decreased carrageenan-induced edema in rats [Jana et al. 1999].
Ginger is on the US FDA’s generally recognized as safe (GRAS) list. The British Herbal Compendium documents no adverse effects of ginger consumption [Bradley, 1990]. Ginger extract has been studied as an alternative to NSAID therapy for arthritic conditions and had moderately positive results (Table 1) [Altman and Marcussen, 2001; reviewed in Ameye and Chee, 2006]. A randomized, placebo-controlled, crossover study comparing ginger extracts and ibuprofen was performed and included 75 people with OA of the hip or knee [Bliddal et al. 2000]. Patients received 170 mg ginger extract, 400 mg ibuprofen, or placebo three times per day and were followed for 3 weeks. The study revealed significant improvement in symptoms for both groups before crossover; however, at the study’s end there was no difference between ginger and placebo. No side effects were noted in the ginger group [Bliddal et al. 2000]. A randomized, double-blind, placebo-controlled trial studied the effects of ginger in the treatment of knee OA in 261 patients. During the treatment period patients ingested 255 mg of EV.EXT 77, a patented ginger and galangal, a spice that is closely related to ginger and is of the ginger extract, which contained 500–4000 mg of dried ginger rhizomes and 500–1500 mg of dried galangal rhizomes and was given twice daily. The primary endpoint of the study was pain on standing after 6 weeks. In the ginger extract group 63% versus 50% in the placebo group showed improvement (p < 0.048). The study failed to show improvement in quality of life, decrease in the consumption of the rescue analgesic (acetaminophen). The dosage of medications used in this study was based empirically on what is typically consumed in Europe. Those receiving the ginger extract experienced more gastrointestinal side effects (116 events in 59 patients, 45%) than those who received placebo (28 events in 21 patients, 16%) [Altman and Marcussen, 2001]. While a significant number of patients experienced side effects, they were mild and mostly gastrointestinal conditions, dyspepsia, and nausea. In some studies, consumption of ginger extract was found to alleviate pain and associated symptoms in patients with OA. At present, ginger extract appears to be of limited efficacy for OA and current evidence is weak. However, these results are strong enough to advocate and support further studies using different doses and duration of treatment to assess the efficacy of ginger extract alone or in combination with other drugs for the treatment of OA.
Boswellia serrata (Indian olibaum)
The Boswellia spp., which is native to India, Ethiopia, Somalia, and the Arabic peninsula, produce a gum resin that is known as olibanum (frankincense). The resin of B. carteri and B. serrata [Figure 1(G)] is used for the treatment of arthritis and other inflammatory diseases in the traditional medicine system in many countries [Safayhi and Ammon, 1997; Chevrier et al. 2005]. Besides their renowned anti-inflammatory activity, boswellic acids have been extensively investigated for their chemopreventive effects [Glaser et al. 1999; Zhao et al. 2003]. B. frereana extracts have also been reported to inhibit IL-1β and oncostatin M induced MMP-9 and MMP-13 expression in cartilage explants culture [Blain et al. 2010]. Further, boswellic acids have been reported as inhibitors of 5-lipoxygenase, the key enzyme for leukotriene biosynthesis in inflammatory disorders [Safayhi et al. 1992; Gupta et al. 1997] and human leukocyte elastase a member of serine proteases subfamily, which can hydrolyze collagen IV and elastin of the extracellular matrix [Safayhi and Ammon, 1997]. Thus, its use may be beneficial in inhibiting the progression of OA. Recently, we studied the efficacy of a herbal-leucine mix (HLM) containing B. serrata as one of the constituents. HLM was found to be an effective anti-inflammatory agent, as evidenced by strong inhibition of iNOS, MMP-9 and MMP-13 expression and NO production in IL-1β-stimulated OA chondrocytes in vitro. IL-1β-induced cartilage matrix breakdown was also inhibited by HLM, as evidenced by inhibition of glycosaminoglycan (GAG) release from human cartilage explants in vitro. These inhibitory effects of HLM on the inflammatory and cartilage catabolic factors were mediated by inhibiting the activation of NF-κB in human OA chondrocytes [Akhtar et al. 2011]. A novel composition of B. serrata extract (Aflapin, Indian Patent Application No. 2229/CHE/2008) showed anti-inflammatory and antiarthritic potential in a rat model. Aflapin showed significant protection from IL-1β-induced death of human primary chondrocytes, improved glycosaminoglycans production and inhibited MMP-3 production [Sengupta et al. 2011].
Toxicity studies of Boswellia in rats and primates showed no pathological changes in hematological, biochemical, or histological parameters at doses up to 1000 mg/kg and the LD50 was established at >2 g/kg [Singh and Atal, 1986]. A trial of a herbomineral formulation containing B. serrata as one of the components also showed significant reduction in severity of pain and disability score in OA [Kulkarni et al. 1991]. A randomized clinical trial of multiplant ayurvedic drugs containing B. serrata demonstrated the potential efficacy and safety in the symptomatic treatment of knee OA over 32 weeks of therapy [Chopra et al. 2004]. A B. serrata extract (5-Loxin, US Patent publication no.: 2004/0073060A1) alone with O-acetyl-11-keto-β-boswellic acid (AKBA) (Aflapin) or AKBA (30%; Loxin) alone was tested in patients with knee OA . Both treatments were effective in reducing pain and significantly improved physical functioning and stiffness scores. However, Aflapin was more effective than Loxin [Sengupta et al. 2010]. In a double-blind, placebo-controlled trial, Boswellia demonstrated a beneficial effect on knee OA [Kimmatkar et al. 2003]. Thirty patients were given either 1000 mg Boswellia daily or placebo in three divided doses for 8 weeks. Patients in the Boswellia group experienced a significant decrease in pain and swelling and increase in range of motion compared with placebo [Kimmatkar et al. 2003]. B. serrata extract containing 5-Loxin with 3-O-acetyl-11-keto-β-boswellic acid (30%) inhibited the 5-lipoxygenase enzyme. A 90-day, placebo-controlled study was conducted to evaluate the efficacy and safety of 5-Loxin in the treatment of OA of the knee with 75 patients. The patients received either 100 mg (n = 25) or 250 mg (n = 25) of 5-Loxin daily or a placebo (n = 25) for 90 days. Both doses of 5-Loxin conferred clinically and statistically significant improvements in pain scores and physical function scores in patients with OA. A significant reduction in synovial fluid MMP-3 was also noted. In comparison with placebo, the safety parameters were almost unchanged in the treatment groups and it was concluded that 5-Loxin reduces pain and improves physical functioning significantly in patients with OA; and it is safe for human consumption [Sengupta et al. 2008]. So far the in vitro, in vivo and clinical evidence (Table 1) for the effectiveness of Boswellia is encouraging but existing data do warrant further investigations [Moussaieff and Mechoulam, 2009].
Curcuma longa (turmeric)
Turmeric is a widely used spice and coloring/ flavoring agent that comes from the root of C. longa [Figure 1(H)] [Aggarwal and Shishodia, 2004]. Turmeric is on the GRAS substance list of the US FDA. In Ayurveda, turmeric has been used for various medicinal conditions including rhinitis, wound healing, common cold, skin infections, liver and urinary tract diseases, and as a ‘blood purifier’ [Aggarwal and Shishodia, 2004; Chainani-Wu, 2003]. Turmeric was found to be effective even when given by different routes, including topical, oral or by inhalation, dependent on the intended use. The major constituent of turmeric is curcumin (diferuloylmethane), which constitutes up to 90% of total the curcuminoid content, with demethoxycurcumin and bis-demethoxycurcumin comprising the remainder [Aggarwal and Shishodia, 2004]. Curcumin has been extensively investigated due to its antitumor, antioxidant, anti-inflammatory, and analgesic properties [reviewed in Henrotin et al. 2010]. The anti-arthritic potential of curcumin has been widely studied in vitro. Curcumin was found to downregulate the catabolic and degradative effects in cartilage explants or chondrocytes stimulated with IL-1β, LPS, and TNFα and inhibited the production of MMP-3, MMP-9, and MMP-13 [Liacini et al. 2003; Schulze-Tanzil et al. 2004b; Shakibaei et al. 2007; Mathy-Hartert et al. 2009] and restored type II collagen and GAG synthesis [Shakibaei et al. 2005; Toegel et al. 2008]. In human chondrocytes, curcumin significantly inhibited MMP-3 and MMP-13 gene expression by inhibiting the JNK, AP-1 and NF-κB pathways [Liacini et al. 2002]. Other studies have shown that curcumin blocks LPS and interferon-induced production of NO and TNFα in vitro by inhibiting the activation of NF-κB and AP-1 [reviewed in Aggarwal and Shishodia, 2004]. Curcumin also inhibited the incorporation of arachidonic acid into membrane lipids, PGE2 production, leukotriene B4 and leukotriene C4 synthesis, as well as the secretion of collagenase, elastase, and hyaluronidase by macrophages [Wallace, 2002].
Curcumin has also demonstrated antiapoptotic activity in chondrocytes [Shakibaei et al. 2005]. However, toxic effects of curcumin have been reported at high dosage (50 mM) without any beneficial effect on cartilage matrix [Toegel et al. 2008]. This study was performed using immortalized human OA chondrocytes, which can explain the discordance with previous studies. No clinical data are available for the effect of pure curcumin in OA. However, one study tested the clinical efficacy of a herbomineral formulation containing a component rich in curcumin in people with OA in a randomized, double-blind, placebo-controlled, crossover study [Kulkarni et al. 1991]. Positive results in pain management and mobility were obtained in the treated group. Use of curcumin for the treatment of OA is of significant current research interest but more studies are needed before coming to any conclusion on its antiarthritis potential.
Ananas comosus
Bromelain [Figure 1(I)] is a crude, aqueous extract obtained from the stems and immature fruits of the pineapple plant (A. comosus Merr, from the family of bromeliaceae), which contains a number of proteolytic enzymes. There are some in vitro and in vivo reports of antiedematous, anti-inflammatory, antithrombotic, and fibrinolytic effects of bromelain [Maurer, 2001; Brien et al. 2004]. Experimental evidence suggests that bromelain’s action as an anti-inflammatory is mediated via decreasing levels of PGE2, thromboxane A2 and through modulation of certain immune cell surface adhesion molecules, which play a role in the pathogenesis of arthritis [Hale et al. 2002; Kumakura et al. 1988]. Pretreatment of Sprague-Dawley rats with bromelains (10 mg/kg intravenously) completely prevented the potentiation of inflammation by ramipril [Caspritz et al. 1986]. Due to its efficacy after oral administration, its safety and lack of undesired side effects, bromelain has earned growing acceptance and compliance among patients as a phytotherapeutical drug. The majority of studies assessing bromelain for OA have been either open studies or equivalence studies designed to assess comparative effectiveness and safety against standard NSAID treatment (Table 1). The majority of the studies have methodological issues that make it difficult to draw definite conclusions. Three different preparations containing bromelain mixed with diverse enzymes have been tested in knee OA: Phlogenzyme (Mucos Parma, Geretsried, Germany), which contains the proteolytic bromelain (90 mg/tablet), trypsin, and rutin; Wobenzym (Mucos Parma, Geretsried, Germany), which contains bromelain (45 mg/tablet), papain, trypsin, chymotrypsin, pancreatin, lipase, and amylase; and Wobenzym N (Mucos Parma, Geretsried, Germany), which contains bromelain (45 mg/tablet), trypsin, papain, chymotrypsin, pancreatin and rutin [reviewed in Brien et al. 2004]. In a double-blind, randomized, controlled trial of 73 patients with knee OA commercial proteolytic enzyme preparation (Phlogenzym) containing bromelain was compared with a dose of diclofenac (100–150 mg/day). An equivalent reduction in pain indices (80%) for the two treatments during 3 weeks of therapy and 4 weeks of follow up with few adverse reactions to either treatment has been reported [Klein and Kullich, 2000]. In contrast, efficacy of bromelain (800 mg/day) in treating knee OA was studied in a randomized, double-blind placebo-controlled 12-week trial. No statistically significant differences were observed between groups for the primary outcome, nor the WOMAC subscales. This study suggests that bromelain is not efficacious as an adjunctive treatment of moderate to severe OA, but its limitations support the need for a follow-up study [Brien et al. 2006]. Two more published studies reported trials to assess the effectiveness of bromelain for knee OA [Singer et al. 2001; Tilwe et al. 2001]. These studies used 3- or 4-weeks period and doses of a standard treatment, diclofenac (150–100 mg/day); however, different doses of bromelain were tested (range from 540 to 1890 mg/day). Tilwe and colleagues compared a daily bromelain dose of 1890 mg/day (Phlogenzym) with the diclofenac comparative group [Tilwe et al. 2001]. Both groups showed reduced symptoms of pain, swelling and joint tenderness but the improvement was significantly better in the phlogenzym group. Singer and colleagues compared bromelain (Phlogenzym) at a dose of 540 mg/day with diclofenac [Singer et al. 2001]. This study demonstrated that bromelain showed significantly better improvement in both the primary outcome and summary pain scores compared with diclofenac. In conclusion, bromelain appears to have potential for the treatment of knee OA. However, there is not enough evidence to support recommending bromelain for the treatment of OA at this stage. It is important to note that there are a number of methodological issues that are common to the studies reported, including the possibility of inadequate power, duration of the study, inadequate treatment periods, inadequate or non-existent follow-up to monitor possible adverse drug reactions. Furthermore, the optimum dosage for this condition remains unclear. More trials of higher quality are needed to confirm the efficacy of bromelain in OA.
Conclusion
At present, the current modalities for treating OA are symptomatic and have not been shown to block or reverse the cartilage degradation and joint destruction. This has resulted in heightened interest in the use of nutraceuticals for OA management. Many studies have been carried out to highlight the potency of several nutraceuticals and dietary supplements for the treatment of OA. Nutraceuticals offer a large variety of products with a wide range of effects. They open new and large horizons for the treatment of degenerative joint diseases. Many nutraceuticals and dietary supplements are claimed to provide pain relief in OA and they have a great potential but there is a need for more substantial data. We have gathered studies and clinical trials of selected neutraceuticals and some results are really promising and encouraging. However, there is a need for serious, well designed, good quality clinical trials that can address most of the questions about the safety and efficacy of such fruit and plant-derived products. This could help in recommending them for OA treatment either alone or in combination with NSAIDs.
Footnotes
This work was supported in part by grants from the National Institute of Health/National Centre for Complimentary and Alternative Medicine (RO1 AT-003267, RO1-AT-005520, R21-AT504615) and funds from the Metro Health Medical Centre.
The authors declare that there is no conflict of interest.
Contributor Information
Nahid Akhtar, Department of Medicine/Rheumatology, MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH, USA.
Tariq M. Haqqi, Department of Medicine/Rheumatology, Rammelkamp-327, MetroHealth Medical Center/Case Western Reserve University, 2500 Metro Health Drive, Cleveland, OH 44109, USA
References
- Abramson S.B. (2003) The role of NSAIDs in the treatment of osteoarthritis. In Brandt K.D., Doherty M., Lohmander L.S. (eds), Osteoarthritis. Oxford: Oxford University Press, pp. 251–258 [Google Scholar]
- Afzal M., Al-Hadidi D., Menon M., Pesek J., Dhami M.S. (2001) Ginger: an ethnomedical, chemical and pharmacological review. Drug Metabol Drug Interact 18: 159–190 [DOI] [PubMed] [Google Scholar]
- Aggarwal B.B., Shishodia S. (2004) Suppression of the nuclear factor-κB activation pathway by spice-derived phytochemicals: reasoning for seasoning. Ann N Y Acad Sci 1030: 434–441 [DOI] [PubMed] [Google Scholar]
- Aguilar J.L., Rojas P., Marcelo A., Plaza A., Bauer R., Reininger E., et al. (2002) Anti-inflammatory activity of two different extracts of Uncaria tomentosa (Rubiaceae). J Ethnopharmacol 81: 271–276 [DOI] [PubMed] [Google Scholar]
- Ahmed S., Marotte H., Kwan K., Ruth J.H., Campbell P.L., Rabquer B.J., et al. (2008) Epigallocatechin-3-gallate inhibits IL-6 synthesis and suppresses trans signaling by enhancing soluble gp130 production. Proc Natl Acad Sci U S A 105: 14692–14697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S., Pakozdi A., Koch A.E. (2006) Regulation of interleukin-1beta-induced chemokine production and matrix metalloproteinase 2 activation by epigallocatechin-3-gallate in rheumatoid arthritis synovial fibroblasts. Arthritis Rheum 54: 2393–2401 [DOI] [PubMed] [Google Scholar]
- Ahmed S., Rahman A., Hasnain A., Lalonde M., Goldberg V.M., Haqqi T.M. (2002) Green tea polyphenol epigallocatechin-3-gallate inhibits the IL-1 beta-induced activity and expression of cyclooxygenase-2 and nitric oxide synthase-2 in human chondrocytes. Free Radical Biol Med 33: 1097–1105 [DOI] [PubMed] [Google Scholar]
- Ahmed S., Wang N., Hafeez B.B., Cheruvu V.K., Haqqi T.M. (2005) Punica granatum L. extract inhibits IL-1beta-induced expression of matrix metalloproteinases by inhibiting the activation of MAP kinases and NF-kappaB in human chondrocytes in vitro. J Nutr 135: 2096–2102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S., Wang N., Lalonde M., Goldberg V.M., Haqqi T.M. (2004) Green tea polyphenol epigallocatechin-3-gallate (EGCG) differentially inhibits interleukin-1 beta-induced expression of matrix metalloproteinase-1 and -13 in human chondrocytes. J Pharmacol Exp Ther 308: 767–773 [DOI] [PubMed] [Google Scholar]
- Akhtar N., Haqqi T.M. (2011) Epigallocatechin-3-gallate suppresses the global interleukin-1beta-induced inflammatory response in human chondrocytes. Arthritis Res Ther 13: R93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akhtar N., Mark J.S.M., Haqqi T.M. (2011) Effect of a Herbal-Leucine mix on the IL-1β-induced cartilage degradation and inflammatory gene expression in human chondrocytes. BMC Complement Altern Med 11: 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen-Hall L., Arnason J.T., Cano P., Lafrenie R.M. (2010) Uncaria tomentosa acts as a potent TNF-alpha inhibitor through NF-kappaB. J Ethnopharmacol 127: 685–693 [DOI] [PubMed] [Google Scholar]
- Altman R.D. (2009) Practical considerations for the pharmacologic management of osteoarthritis. Am J Manag Care 15 (8 Suppl.): S236–S243 [PubMed] [Google Scholar]
- Altman R.D., Marcussen K.C. (2001) Effects of a ginger extract on knee pain in patients with osteoarthritis. Arthritis Rheum 44: 2531–2538 [DOI] [PubMed] [Google Scholar]
- Ameye L.G., Chee W.S. (2006) Osteoarthritis and nutrition from nutraceuticals to functional foods: a systematic review of the scientific evidence. Arthritis Res Ther 8: R127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andriamanalijaona R., Kypriotou M., Baugé C., Renard E., Legendre F., Raoudi M., et al. (2005) Comparative effects of 2 antioxidants, selenomethionine and epigallocatechin-gallate, on catabolic and anabolic gene expression of articular chondrocytes. J Rheumatol 32: 1958–1967 [PubMed] [Google Scholar]
- Anonymous (2008) Devil’s claw tuber. http://www.altcancer.com/phyto/devils_claw.htm (Accessed 6 January 2012).
- Aviram M., Dornfeld L. (2003) Methods of using pomegranate extracts for causing regression in lesions due to arteriosclerosis in humans. US Patent 6: 641 [Google Scholar]
- Bélaiche P. (1982) Clinical study of 630 patients with arthritis treated with the herbal remedy Harpagophytum procumbens [in French]. Phytothérapy 1: 22–28 [Google Scholar]
- Betancor-Fernández A., Pérez-Gálvez A., Sies H., Stahl W. (2003) Screening pharmaceutical preparations containing extracts of turmeric rhizome, artichoke leaf, devil’s claw root and garlic or salmon oil for antioxidant capacity. J Pharm Pharmacol 55: 981–986 [DOI] [PubMed] [Google Scholar]
- Bhattacharya A., Bhattacharya S. (1998) Antioxidant activity of Harpagophytum procumbens. Br J Phytother 5: 68 [Google Scholar]
- Blain E.J., Ali A.Y., Duance V.C. (2010) Boswellia frereana (frankincense) suppresses cytokine-induced matrix metalloproteinase expression and production of pro-inflammatory molecules in articular cartilage. Phytother Res 24: 905–912 [DOI] [PubMed] [Google Scholar]
- Bliddal H., Rosetzsky A., Schlichting P., Weidner M.S., Andersen L.A., Ibfelt H.H. (2000) A randomized, placebo-controlled, cross-over study of ginger extracts and ibuprofen in osteoarthritis. Osteoarthritis Cartilage 8: 9–12 [DOI] [PubMed] [Google Scholar]
- Blumenthal M. (1998) The Complete German Commission E Monographs. Austin, TX: American Botanical Council, pp. 120–121 [Google Scholar]
- Boje K., Lechtenberg M., Nahrstedt A. (2003) New and known iridoid- and phenylethanoid glycosides from Harpagophytum procumbens and their in vitro inhibition of human leukocyte elastase. Planta Med 69: 820–825 [DOI] [PubMed] [Google Scholar]
- Bradley P. (ed) (1990) British Herbal Compendium. Bournemouth, UK: British Herbal Medical Association [Google Scholar]
- Bradley P.R. (ed) (1992) British Herbal Compendium. Dorset, UK: British Herbal Medicine Association [Google Scholar]
- Brien S., Lewith G.T., McGregor G. (2006) Devil’s claw (Harpagophytum procumbens) as a treatment for osteoarthritis: a review of efficacy and safety. J Altern Complement Med 12: 981–993 [DOI] [PubMed] [Google Scholar]
- Brien S., Lewith G., Walker A., Hicks S.M., Middleton D. (2004) Bromelain as a treatment for osteoarthritis: a review of clinical studies. Evid Based Complement Alternat Med 1: 251–257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brien S., Lewith G., Walker A.F., Middleton R., Prescott P., Bundy R. (2006) Bromelain as an adjunctive treatment for moderate-to-severe osteoarthritis of the knee: a randomized placebo-controlled pilot study. QJM 99: 841–850 [DOI] [PubMed] [Google Scholar]
- Bruijn C.D., Christ F.R., Dziabo A.J. (2003) Ophthalmic, pharmaceutical and other healthcare preparations with naturally occurring plant compounds, extracts and derivatives. US Patent Application 20030086986
- Bruneton J. (2001) Pharmacognosie, Phytochimie, Plantes Medicina-les. Paris: Technique et Documentation-Lavoisier [Google Scholar]
- Cabrera C., Artacho R., Gimenez R. (2006) Beneficial effects of green tea – a review. J Am Coll Nutr 25: 79–99 [DOI] [PubMed] [Google Scholar]
- Cabrera C., Giménez R., López M.C. (2003) Determination of tea components with antioxidant activity. J Agric Fd Chem 51: 4427–4435 [DOI] [PubMed] [Google Scholar]
- Caspritz G., Alpermann H.G., Schleyerbach R. (1986) Influence of the new angiotensin converting enzyme inhibitor ramipril on several models of acute inflammation and the adjuvant arthritis in the rat. Arzneimittelforschung 36: 1605–1608 [PubMed] [Google Scholar]
- Cerdá B., Cerón J.J., Tomás-Barberán F.A., Espín J.C. (2003) Repeated oral administration of high doses of the pomegranate ellagitannin punicalagin to rats for 37 days is not toxic. J Agric Fd Chem 51: 3493–3501 [DOI] [PubMed] [Google Scholar]
- Chainani-Wu N. (2003) Safety and anti-inflammatory activity of curcumin: a component of turmeric (Curcuma longa). J Altern Complement Med 9: 161–168 [DOI] [PubMed] [Google Scholar]
- Chan F.K., Cryer B., Goldstein J.L., Lanas A., Peura D.A., Scheiman J.M., et al. (2010) A novel composite endpoint to evaluate the gastrointestinal (GI) effects of nonsteroidal anti-inflammatory drugs through the entire GI tract. J Rheumtol 37: 167–174 [DOI] [PubMed] [Google Scholar]
- Chang C.P., Chang J.Y., Wang F.Y., Chang J.G. (1995) The effect of Chinese medicinal herb Zingiberis rhizoma extract on cytokine secretion by human peripheral blood mononuclear cells. J Ethnopharmacol 48: 13–19 [DOI] [PubMed] [Google Scholar]
- Chantre P., Cappelaere A., Leblan D., Guedon D., Vandermander J., Fournie B. (2000) Efficacy and tolerance of Harpagophytum procumbens versus diacerhein in treatment of osteoarthritis. Phytomedicine 7: 177–183 [DOI] [PubMed] [Google Scholar]
- Cheng K.W., Wong C.C., Chao J., Lo C., Chen F., Chu I.K., et al. (2009) Inhibition of mutagenic PhIP formation by epigallocatechin gallate via scavenging of phenylacetaldehyde. Mol Nutr Food Res 53: 716–725 [DOI] [PubMed] [Google Scholar]
- Chevrier M.R., Ryan A.E., Lee D.Y., Zhongze M., Wu-Yan Z., Via C.S. (2005) Boswellia carterii extract inhibits TH1 cytokines and promotes TH2 cytokines in vitro. Clin Diagn Lab Immunol 12: 575–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi Y.H., Yan G.H. (2009) Ellagic acid attenuates immunoglobulin E-mediated allergic response in mast cells. Biol Pharm Bull 32: 1118–1121 [DOI] [PubMed] [Google Scholar]
- Chopra A., Lavin P., Patwardhan B., Chitre D. (2004) A 32-week randomized, placebo-controlled clinical evaluation of RA-11, an Ayurvedic drug, on osteoarthritis of the knees. J Clin Rheumatol 10: 236–245 [DOI] [PubMed] [Google Scholar]
- Chrubasik S., Thanner J., Künzel O., Conradt C., Black A., Pollak S. (2002) Comparison of outcome measures during treatment with the proprietary Harpagophytum extract Doloteffin in patients with pain in the lower back, knee, or hip. Phytomedicine 9: 181–194 [DOI] [PubMed] [Google Scholar]
- Danesi F., Philpott M., Huebner C., Bordoni A., Ferguson L.R. (2010) Food-derived bioactives as polyphenol epigallocatechin-3-gallate inhibits advanced glycation end product induced potential regulators of the IL-12/IL-23 pathway implicated in inflammatory bowel diseases. Mutat Res 690: 139–144 [DOI] [PubMed] [Google Scholar]
- de Mejia E.G., Ramirez-Mares M.V., Puangpraphant S. (2009) Bioactive components of tea: cancer, inflammation and behavior. Brain Behav Immun 23: 721–731 [DOI] [PubMed] [Google Scholar]
- Dugas A.J., Jr, Castañeda-Acosta J., Bonin G.C., Price K.L., Fischer N.H., Winston G.W. (2000) Evaluation of the total peroxyl radical-scavenging capacity of flavonoids: structure–activity relationships. J Nat Prod 63: 327–331 [DOI] [PubMed] [Google Scholar]
- Farrell A.J., Blake D.R., Palmer R.M., Moncada S. (1992) Increased concentrations of nitrite in synovial fluid and serum samples suggest increased nitric oxide synthesis in rheumatic diseases. Ann Rheum Dis 51: 1219–1222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fetrow C.W., Avila J.R. (1999) Professional’s Handbook of Complementary and Alternative Medicines. Springhouse, PA: Springhouse [Google Scholar]
- Fiebich B.L., Heinrich M., Hiller K.O., Kammerer N. (2001) Inhibition of TNF-alpha synthesis in LPS-stimulated primary human monocytes by Harpagophytum extract SteiHap 69. Phytomedicine 8: 28–30 [DOI] [PubMed] [Google Scholar]
- Firestein G.S., Manning A.M. (1999) Signal transduction and transcription factors in rheumatic disease. Arthritis Rheum 42: 609–621 [DOI] [PubMed] [Google Scholar]
- Foster S. (1996) Herbs for your health. Loveland, CO: Interweave Press [Google Scholar]
- Frei B., Higdon J.V. (2003) Antioxidant activity of tea polyphenols in vivo: evidence from animal studies. J Nutr 133: 3275S–3284S [DOI] [PubMed] [Google Scholar]
- Frerick H., Biller A., Schmidt U. (2001) Hip osteoarthritis: double blind study with devil claw [in German]. Der Kassenarzt 5: 34–41 [Google Scholar]
- Frondoza C.G., Sohrabi A., Polotsky A., Phan P.V., Hungerford D.S., Lindmark L. (2004) An in vitro screening assay for inhibitors of proinflammatory mediators in herbal extracts using human synoviocyte cultures. In Vitro Cell Dev Biol Anim 40: 95–101 [DOI] [PubMed] [Google Scholar]
- Ganzera M., Muhammad I., Khan R.A., Khan I.A. (2001) Improved method for the determination of oxindole alkaloids in Uncaria tomentosa by high performance liquid chromatography. Planta Med 67: 447–450 [DOI] [PubMed] [Google Scholar]
- Gil M.I., Tomás-Barberán F.A., Hess-Pierce B., Holcroft D.M., Kader A.A. (2000) Antioxidant activity of pomegranate juice and its relationship with phenolic composition and processing. J Agric Fd Chem 48: 4581–4589 [DOI] [PubMed] [Google Scholar]
- Glaser T., Winter S., Groscurth P., Safayhi H., Sailer E.R., Ammon H.P., et al. (1999) Boswellic acids and malignant glioma: induction of apoptosis but no modulation of drug sensitivity. Br J Cancer 80: 756–765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Fuentes A.M., Green D.M., Rossen R.D., Ng B. (2010) Intra-articular hyaluronic acid increases cartilage breakdown biomarker in patients with knee osteoarthritis. Clin Rheumatol 29: 619–624 [DOI] [PubMed] [Google Scholar]
- Grant L., McBean D.E., Fyfe L., Warnock A.M. (2009) The inhibition of free radical generation by preparations of Harpagophytum procumbens in vitro. Phytother Res 23: 104–110 [DOI] [PubMed] [Google Scholar]
- Gregory P.J., Sperry M., Wilson A.F. (2008) Dietary supplements for osteoarthritis. Am Fam Physician 77: 177–184 [PubMed] [Google Scholar]
- Gupta I., Parihar A., Malhotra P., Singh G.B., Lüdtke R., Safayhi H., et al. (1997) Effects of Boswellia serrata gum resin in patients with ulcerative colitis. Eur J Med Res 2: 37–43 [PubMed] [Google Scholar]
- Hale L.P., Greer P.K., Sempowski G.D. (2002) Bromelain treatment alters leukocyte expression of cell surface molecules involved in cellular adhesion and activation. Clin Immunol 104: 183–190 [DOI] [PubMed] [Google Scholar]
- Halsted C.H. (2003) Dietary supplements and functional foods: 2 sides of a coin? Am J Clin Nutr 77: 1001S–1007S [DOI] [PubMed] [Google Scholar]
- Haqqi T.M., Anthony D.D., Gupta S., Ahmad N., Lee M.S., Kumar G.K., et al. (1999) Prevention of collagen-induced arthritis in mice by a polyphenolic fraction from green tea. Proc Natl Acad Sci U S A 96: 4524–4529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Häuselmann H.J. (2001) Nutripharmaceuticals for osteoarthritis. Best Pract Res Clin Rheumatol 15: 595–607 [DOI] [PubMed] [Google Scholar]
- Henrotin Y., Clutterbuck A.L., Allaway D., Lodwig E.M., Harris P., Mathy-Hartert M., et al. (2010) Biological actions of curcumin on articular chondrocytes. Osteoarthritis Cartilage 18: 141–149 [DOI] [PubMed] [Google Scholar]
- Hsiao F.Y., Tsai Y.W., Huang W.F. (2009) Changes in physicians’ practice of prescribing cyclooxygenase-2 inhibitor after market withdrawal of rofecoxib: a retrospective study of physician–patient pairs in Taiwan. Clin Ther 31: 2618–2627 [DOI] [PubMed] [Google Scholar]
- Huang T.H., Tran V.H., Duke R.K., Tan S., Chrubasik S., Roufogalis B.D. (2005) Harpagoside suppresses lipopolysaccharide-induced iNOS and COX-2 expression through inhibition of NF-kB activation. J Ethnopharmacol 13: 11–15 [DOI] [PubMed] [Google Scholar]
- Ippoushi K., Azuma K., Ito H., Horie H., Higashio H. (2003) [6]-Gingerol inhibits nitric oxide synthesis in activated J774.1 mouse macrophages and prevents peroxynitrite-induced oxidation and nitration reactions. Life Sci 73: 3427–3437 [DOI] [PubMed] [Google Scholar]
- Jana U., Chattopadhayay R.N., Shaw B.P. (1999) Preliminary studies on anti-inflammatory activity of Zingiber officinale Rosc., Vitex negundo Linn. and Tinospora cordifolia (Willid) miers in albino rats. Indian J Pharmacol 31: 232–233 [Google Scholar]
- Jang M.H., Lim S., Han S.M., Park H.J., Shin I., Kim J.W., et al. (2003) Harpagophytum procumbens suppresses lipopolysaccharidestimulated expressions of cyclooxygenase-2 and inducible nitric oxide synthase in fibroblast cell line L929. J Pharmacol Sci 93: 367–371 [DOI] [PubMed] [Google Scholar]
- Jaswal S., Mehta H., Sood A., Kaur J. (2003) Antioxidant status in rheumatoid arthritis and role of antioxidant therapy. Clinica Chimica Acta 338: 123–129 [DOI] [PubMed] [Google Scholar]
- Johnson J.J., Bailey H.H., Mukhtar H. (2010) Green tea polyphenols for prostate cancer chemoprevention: a translational perspective. Phytomedicine 17: 3–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalra E.K. (2003) Nutraceutical – definition and introduction. AAPS PharmSci 5: E25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katiyar S.K., Raman C. (2011) Green tea: a new option for the prevention or control of osteoarthritis. Arthritis Res Ther 13: 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalifé S., Zafarullah M. (2011) Molecular targets of natural health products in arthritis. Arthritis Res Ther 13: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan N., Mukhtar H. (2008) Multitargeted therapy of cancer by green tea polyphenols. Cancer Lett 269: 269–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M.M., Kim S. (2002) Composition for improving oral hygiene containing Punica granatum L. extract. Korean Patent: KR 2002066042
- Kim N.D., Mehta R., Yu W., Neeman I., Livney T., Amichay A., et al. (2002) Chemopreventive and adjuvant therapeutic potential of pomegranate (Punica granatum) for human breast cancer. Breast Cancer Res Treat 71: 203–217 [DOI] [PubMed] [Google Scholar]
- Kimmatkar N., Thawani V., Hingorani L., Khiyani R. (2003) Efficacy and tolerability of Boswellia serrata extract in treatment of osteoarthritis of knee – a randomized double blind placebo controlled trial. Phytomedicine 10: 3–7 [DOI] [PubMed] [Google Scholar]
- Klein G., Kullich W. (2000) Short-term treatment of painful osteoarthritis of the knee with oral enzymes: a randomised, double-blind study versus Diclofenac. Clin Drug Invest 19:15–23 [Google Scholar]
- Koeberle A., Bauer J., Verhoff M., Hoffmann M., Northoff H., Werz O. (2009) Green tea epigallocatechin-3-gallate inhibits microsomal prostaglandin E(2) synthase-1. Biochem Biophy Res Commun 388: 350–354 [DOI] [PubMed] [Google Scholar]
- Kulkarni R.R., Patki P.S., Jog V.P., Gandage S.G., Patwardhan B. (1991) Treatment of osteoarthritis with a herbomineral formulation: a double-blind, placebo-controlled, cross-over study. J Ethnopharmacol 33: 91–95 [DOI] [PubMed] [Google Scholar]
- Kumakura S., Yamashita M., Tsurufuji S. (1988) Effect of bromelain or kaolin induced inflammation in rats. Eur J Pharmacol 150: 295–301 [DOI] [PubMed] [Google Scholar]
- Langmead L., Dawson C., Hawkins C., Banna N., Loo S., Rampton D. (2002) Antioxidant effects of herbal therapies used by patients with inflammatory bowel disease: an in vitro study. Aliment Pharmacologic Ther 16: 197–205 [DOI] [PubMed] [Google Scholar]
- Lanhers M.C., Fleurentin J., Mortier F., Vinche A., Younos C. (1992) Antiinflammatory and analgesic effects of an aqueous extract of Harpagophytum procumbens. Planta Med 58: 117–123 [DOI] [PubMed] [Google Scholar]
- Leblan D., Chantre P., Fournié B. (2000) Harpagophytum procumbens in the treatment of knee and hip osteoarthritis. Four-month results of a prospective, multicenter, double-blind trial versus diacerhein. Joint Bone Spine 67: 462–467 [PubMed] [Google Scholar]
- Lecomte A., Costa J.P. (1992) Harpagophytum in osteoarthritis. Double-blind, placebo-controlled study. Le Magazine 37: 27–30 [Google Scholar]
- Lee S.I., Kim B.S., Kim K.S., Lee S., Shin K.S., Lim J.S. (2008) Immune-suppressive activity of punicalagin via inhibition of NFAT activation. Biochem Biophys Res Commun 371: 799–803 [DOI] [PubMed] [Google Scholar]
- Lee J., Watson R.R. (1998) Pomegranate: a role in health promotion and AIDS? In Watson R.R. (ed.), Nutrients and Foods in AIDS. Boca Raton, FL: CRC Press, p. 179 [Google Scholar]
- Liacini A., Sylvester J., Li W.Q., Huang W., Dehnade F., Ahmad M., et al. (2003) Induction of matrix metalloproteinase-13 gene expression by TNF-alpha is mediated by MAP kinases, AP-1, and NF-kappaB transcription factors in articular chondrocytes. Exp Cell Res 288: 208–217 [DOI] [PubMed] [Google Scholar]
- Liacini A., Sylvester J., Li W.Q., Zafarullah M. (2002) Inhibition of interleukin-1stimulated MAP kinases, activating protein-1 (AP-1) and nuclear factor kappa B (NF-kB) transcription factors down-regulates matrix metalloproteinase gene expression in articular chondrocytes. Matrix Biol 21: 251–262 [DOI] [PubMed] [Google Scholar]
- Lo Y.Y., Wong J.M., Cruz T.F. (1996) Reactive oxygen species mediate cytokine activation of c-Jun NH2-terminal kinases. J Biol Chem 271: 15703–15707 [DOI] [PubMed] [Google Scholar]
- Loew D., Mollerfeld J., Schrodter A., Puttkammer S., Kaszkin M. (2001) Investigations on the pharmacokinetic properties of Harpagophytum extracts and their effects on eicosanoid biosynthesis in vitro and ex vivo. Clin Pharmacol Ther 69: 356–364 [DOI] [PubMed] [Google Scholar]
- Malemud C.J., Islam N., Haqqi T.M. (2003) Pathophysiological mechanisms in osteoarthritis lead to novel therapeutic strategies. Cells Tissues Organs 174: 34–48 [DOI] [PubMed] [Google Scholar]
- Marcu K.B., Otero M., Olivotto E., Borzi R.M., Goldring M.B. (2010) NF-kappaB signaling: multiple angles to target OA. Curr Drug Targets 11: 599–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathy-Hartert M., Jacquemond-Collet I., Priem F., Sanchez C., Lambert C., Henrotin Y. (2009) Curcumin inhibits pro-inflammatory mediators and metalloproteinase-3 production by chondrocytes. Inflamm Res 58: 899–908 [DOI] [PubMed] [Google Scholar]
- Maurer H.R. (2001) Bromelain: biochemistry, pharmacology and medical use. Cell Mol Life Sci 58: 1234–1245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlindon T.E. (2006) Nutraceuticals: do they work and when should we use them? Best Pract Res Clin Rheumatol 20: 99–115 [DOI] [PubMed] [Google Scholar]
- Mehta K., Gala J., Bhasale S., Naik S., Modak M., Thakur H. (2007) Comparison of glucosamine sulfate and a polyherbal supplement for the relief of osteoarthritis of the knee: a randomized controlled trial [ISRCTN25438351]. BMC Complement Altern Med 7: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng Q., Velalar C.N., Ruan R. (2001) Effects of epigallocatechin-3-gallate on mitochondrial integrity and antioxidative enzyme activity in the aging process of human fibroblast. Free Radic Biol Med 44: 1032–1041 [DOI] [PubMed] [Google Scholar]
- Mertens-Talcott S.U., Jilma-Stohlawetz P., Rios J., Hingorani L., Derendorf H. (2006) Absorption, metabolism, and antioxidant effects of pomegranate (Punica granatum L.) polyphenols after ingestion of a standardized extract in healthy human volunteers. J Agric Fd Chem 54: 8956–8961 [DOI] [PubMed] [Google Scholar]
- Miller M.J., Ahmed S., Bobrowski P., Haqqi T.M. (2006) The chrondoprotective actions of a natural product are associated with the activation of IGF-1 production by human chondrocytes despite the presence of IL-1beta. BMC Complement Altern Med 6: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M.J., Mehta K., Kunte S., Raut V., Gala J., Dhumale R., et al. (2005) Early relief of osteoarthritis symptoms with a natural mineral supplement and a herbomineral combination: a randomized controlled trial [ISRCTN38432711]. Inflamm (Lond) 2: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minoia C., Sabbioni E., Ronchi A., Gatti A. (1994) Trace element reference values in tissues from inhabitants of the European Community. IV. Influence of dietary factors. Sci Total Environ 141: 181–195 [Google Scholar]
- Moayadi A. (2004) Mixtures of pomegranate seed oils for cosmetics. Japanese Patent: JP 2004083544 A2 20040318
- Moon H.S., Lee H.G., Choi Y.J., Kim T.G., Cho C.S. (2007) Proposed mechanisms of (−)-epigallocatechin-3-gallate for anti-obesity. Chem Biol Interac 167: 85–98 [DOI] [PubMed] [Google Scholar]
- Morelli V., Naquin C., Weaver V. (2003) Alternative therapies for traditional disease states: osteoarthritis. Am Fam Physician 67: 339–344 [PubMed] [Google Scholar]
- Moussaieff A., Mechoulam R. (2009) Boswellia resin: from religious ceremonies to medical uses: a review of in-vitro, in-vivo and clinical trials. J Pharm Pharmacol 61: 1281–1293 [DOI] [PubMed] [Google Scholar]
- Nuti E., Casalini F., Avramova S.I., Santamaria S., Cercignani G., Marinelli L., et al. (2009) N-O-isopropyl sulfonamido-based hydroxamates: design, synthesis and biological evaluation of selective matrix metalloproteinase-13 inhibitors as potential therapeutic agents for osteoarthritis. J Med Chem 52: 4757–4773 [DOI] [PubMed] [Google Scholar]
- Okamoto H., Cujec T.P., Yamanaka H., Kamatani N. (2008) Molecular aspects of rheumatoid arthritis: Role of transcription factors. FEBS J 275: 4463–4470 [DOI] [PubMed] [Google Scholar]
- Osterburg A., Gardner J., Hyon S.H., Neely A., Babcock G. (2009) Highly antibiotic-resistant Acinetobacter baumannii clinical isolates are killed by the green tea polyphenol (−)-epigallocatechin-3-gallate (EGCG). Clin Microbiol Infect 15: 341–346 [DOI] [PubMed] [Google Scholar]
- Palaniswamy R. (2003) A Guide to Medicinal Plants of Asian Origin and Culture. Newbury, UK: CPL Press [Google Scholar]
- Piscoya J., Rodriguez Z., Bustamante S.A., Okuhama N.N., Miller M.J., Sandoval M. (2001) Efficacy and safety of freeze-dried cat’s claw in osteoarthritis of the knee: mechanisms of action of the species Uncaria guianensis. Inflamm Res 50: 442–448 [DOI] [PubMed] [Google Scholar]
- Qi J., Chen J., Cheng Z., Zhou J., Yu B., Qui S. (2006) Iridoid glycosides from Harpagophytum procumbens D.C. (devil’s claw). Phytochemistry 67: 1372–1377 [DOI] [PubMed] [Google Scholar]
- Ragusa S., Circosta C., Galati E.M., Tumino G. (1984) A drug used in traditional medicine. Harpagophytum procumbens DC. I. Scanning electron microscope observations. J Ethnopharmcol 11: 245–257 [DOI] [PubMed] [Google Scholar]
- Ramsey S.D., Spencer A.C., Topolski T.D., Belza B., Patrick D.L. (2001) Use of alternative therapies by older adults with osteoarthritis. Arthritis Rheum 45: 222–227 [DOI] [PubMed] [Google Scholar]
- Rasheed Z., Akhtar N., Anbazhagan A.N., Ramamurthy S., Shukla M., Haqqi T.M. (2009a) Polyphenol-rich pomegranate fruit extract (POMx) suppresses PMACI-induced expression of pro-inflammatory cytokines by inhibiting the activation of MAP Kinases and NF-kappaB in human KU812 cells. J Inflamm (Lond) 8: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasheed Z., Akhtar N., Haqqi T.M. (2010) Pomegranate extract inhibits the interleukin-1β-induced activation of MKK-3, p38α-MAPK and transcription factor RUNX-2 in human osteoarthritis chondrocytes. Arthritis Res Ther 12: R195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasheed Z., Anbazhagan A.N., Akhtar N., Ramamurthy S., Voss F.R., Haqqi T.M. (2009b) Green tea expression of tumor necrosis factor-alpha and matrix metalloproteinase-13 in human chondrocytes. Arthritis Res Ther 11: R71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum C.C., O’Mathúna D.P., Chavez M., Shields K. (2010) Antioxidants and antiinflammatory dietary supplements for osteoarthritis and rheumatoid arthritis. Altern Ther Health Med 16: 32–40 [PubMed] [Google Scholar]
- Rutten S., Schafer I. (2000) Einsatz der afrikanischen Teufelskralle [Allya] bei Erkrankungen des Stutz unde Bewegungsapparates. Ergebnisse einer Anwendungscbeobachtung Acta Biol 2: 5–20 [Google Scholar]
- Safayhi H., Ammon H.P.T. (1997) Pharmakologische Aspecte von Weihrauch und Boswelliasäuren. Pharmazeutisch Zeitung 142: 3277–3280 [Google Scholar]
- Safayhi H., Mack T., Sabieraj J., Anazodo M.I., Subramanian L.R., Ammon H.P. (1992) Boswellic acids: novel, specific, nonredox inhibitors of 5-lipoxygenase. J Pharmacol Exp Ther 261: 1143–1146 [PubMed] [Google Scholar]
- Sandoval M., Chaarbonnett R.M., Okuhama N.N., Roberts J., Krenova Z., Trentacosti A.M. (2000) Cat’s claw inhibits TNFa production and scavenges free radicals: role in cytoprotection. Free Rad Biol Med 29: 71–78 [DOI] [PubMed] [Google Scholar]
- Sandoval M., Okuhama N.N., Zhang X.J., Condezo L.A., Lao J., Angeles F.M. (2002) Anti-inflammatory and antioxidant activities of cat’s claw (Uncaria tomentosa and Uncaria guianensis) are independent of their alkaloid content. Phytomedicine 9: 325–337 [DOI] [PubMed] [Google Scholar]
- Sandoval-Chacón M., Thompson J.H., Zhang X.J., Liu X., Mannick E.E., Sadowska-Krowicka H., et al. (1998) Antiinflammatory actions of cat’s claw: the role of NF-kappaB. Aliment Pharmacol Ther 12: 1279–1289 [DOI] [PubMed] [Google Scholar]
- Santa Maria A., Lopez A., Diaz M.M., Alban J., Galan de Mera. A., Vicente Orellana J.A., et al. (1997) Evaluation of the toxicity of Uncaria tomentosa by bioassays in vitro. J Ethnopharmacol 57: 183–187 [DOI] [PubMed] [Google Scholar]
- Sawa T., Nakao M., Akaike T., Ono K., Maeda H. (1999) Alkylperoxyl radical-scavenging activity of various flavonoids and other phenolic compounds: implications for the antitumor- promoter effect of vegetables. J Agric Food Chem 47: 397–402 [DOI] [PubMed] [Google Scholar]
- Schmelz H., Haemmerle H.D., Springorum H.W. (1997) Analgesic effectiveness of Devil claw root excerpt in different chronic-degenerative joint illnesses [in German]. In: Chrubasik S., Wink M. (eds), Rheumatherapie mit Phytopharmaka. Stuttgart: Hippokrates [Google Scholar]
- Schulze-Tanzil G., Hansen C., Shakibaei M. (2004a) Effect of a Harpagophytum procumbens DC extract on matrix metalloproteinases in human chondrocytes in vitro. Arzneimittel-Forsch 54: 213–220 [DOI] [PubMed] [Google Scholar]
- Schulze-Tanzil G., Mobasheri A., Sendzik J., John T., Shakibaei M. (2004b) Effects of curcumin (diferuloylmethane) on nuclear factor kappaB signaling in interleukin-1beta-stimulated chondrocytes. Ann N Y Acad Sci 1030: 578–586 [DOI] [PubMed] [Google Scholar]
- Schwarz B., Bischof H.P., Kunze M. (1994) Coffee, tea and lifestyle. Prev Med 23: 377–384 [DOI] [PubMed] [Google Scholar]
- Seeram N.P., Lee R., Heber D. (2004) Bioavailability of ellagic acid in human plasma after consumption of ellagitannins from pomegranate (Punica granatum L.) juice. Clin Chim Acta 348: 63–68 [DOI] [PubMed] [Google Scholar]
- Seeram N.P., Nair M.G. (2002) Inhibition of lipid peroxidation and structure–activity-related studies of the dietary constituents anthocyanins, anthocyanidins, and catechins. J Agric Fd Chem 50: 5308–5312 [DOI] [PubMed] [Google Scholar]
- Sengupta K., Alluri K.V., Satish A.R., Mishra S., Golakoti T., Sarma K.V., et al. (2008) A double blind, randomized, placebo controlled study of the efficacy and safety of 5-Loxin for treatment of osteoarthritis of the knee. Arthritis Res Ther 10: R85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sengupta K., Kolla J.N., Krishnaraju A.V., Yalamanchili N., Rao C.V., Golakoti T., et al. (2011) Cellular and molecular mechanisms of anti-inflammatory effect of Aflapin: a novel Boswellia serrata extract. Mol Cell Biochem 354: 189–197 [DOI] [PubMed] [Google Scholar]
- Sengupta K., Krishnaraju A.V., Vishal A.A., Mishra A., Trimurtulu G., Sarma K.V., et al. (2010) Comparative efficacy and tolerability of 5-Loxin® and Aflapin® against osteoarthritis of the knee: a double blind, randomized, placebo controlled clinical study. Int J Med Sci 7: 366–377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakibaei M., John T., Schulze-Tanzil G., Lehmann I., Mobasheri A. (2007) Suppression of NF-kappaB activation by curcumin leads to inhibition of expression of cyclo-oxygenase-2 and matrix metalloproteinase-9 in human articular chondrocytes: implications for the treatment of osteoarthritis. Biochem Pharmacol 73: 1434–1445 [DOI] [PubMed] [Google Scholar]
- Shakibaei M., Schulze-Tanzil G., John T., Mobasheri A. (2005) Curcumin protects human chondrocytes from IL-l1beta-induced inhibition of collagen type II and beta1-integrin expression and activation of caspase-3: an immunomorphological study. Ann Anat 187: 487–497 [DOI] [PubMed] [Google Scholar]
- Shen C.L., Hong K.J., Kim S.W. (2003) Effects of ginger (Zingiber officinale Rosc.) on decreasing the production of inflammatory mediators in sow osteoarthrotic cartilage explants. J Med Fd 6: 323–328 [DOI] [PubMed] [Google Scholar]
- Shen Y.J., Li W.G., Zhang H., Li B., Yuan H.X., Zhang J.J. (2009) Effects of (−)-epigallocatechin-3-gallate on interleukin-1beta expression in mouse wound healing. Fen Zi Xi Bao Sheng Wu Xue Bao 42: 179–185 [PubMed] [Google Scholar]
- Shin H.Y., Kim S.H., Jeong H.J., Kim S.Y., Shin T.Y., Um J.Y., et al. (2006) Epigallocatechin- 3-gallate inhibits secretion of TNF-alpha, IL-6 and IL-8 through the attenuation of ERK and NF-kappaB in HMC-1 cells. Int Arch Allergy Immunol 142: 335–344 [DOI] [PubMed] [Google Scholar]
- Shukla M., Gupta K., Rasheed Z., Khan K.A., Haqqi T.M. (2008a) Bioavailable constituents/metabolites of pomegranate (Punica granatum L) preferentially inhibit COX2 activity ex vivo and IL-1beta-induced PGE2 production in human chondrocytes in vitro. J Inflamm (Lond) 5: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shukla M., Gupta K., Rasheed Z., Khan K.A., Haqqi T.M. (2008b) Consumption of hydrolyzable tannins-rich pomegranate extract suppresses inflammation and joint damage in rheumatoid arthritis. Nutrition 24: 733–743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer F., Singer C., Oberleitner H. (2001) Phlyoenzym versus diclofenac in the treatment of activated osteoarthritis of the knee. Int J Immunother 17: 135–141 [Google Scholar]
- Singh G.B., Atal C.K. (1986) Pharmacology of an extract of salai guggal ex-Boswellia serrata, a new nonsteroidal anti-inflammatory agent. Agents Actions 18: 407–412 [DOI] [PubMed] [Google Scholar]
- Singh R., Ahmed S., Islam N., Goldberg V.M., Haqqi T.M. (2003) Epigallocatechin-3-gallate inhibits selectively inhibits interleukin-1beta-induced activation of mitogen activated protein kinase subgroup c-Jun N-terminal kinase in human osteoarthritis chondrocytes. J Orthop Res 21: 102–109 [DOI] [PubMed] [Google Scholar]
- Singh R., Ahmed S., Malemud C.J., Goldberg V.M., Haqqi T.M. (2002a) Epigallocatechin-3-gallate interleukin-1beta-induced expression of nitric oxide synthase and production of nitric oxide in human chondrocytes: suppression of nuclear factor kappaB activation by degradation of the inhibitor of nuclear factor kappaB. Arthritis Rheum 46: 2079–2086 [DOI] [PubMed] [Google Scholar]
- Singh R., Akhtar N., Haqqi T.M. (2010) Green tea polyphenol epigallocatechi3-gallate: Inflammation and arthritis. Life Sci 86: 907–918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R.P., Chidambara-Murthy K.N., Jayaprakasha G.K. (2002b) Studies on the antioxidant activity of pomegranate (Punica granatum) peel and seed extracts using in vitro models. J Agric Fd Chem 50: 81–86 [DOI] [PubMed] [Google Scholar]
- Smith A., Giunta B., Bickford P.C., Fountain M., Tan J., Shytle R.D. (2010) Nanolipidic particles improve the bioavailability and alpha-secretase inducing ability of epigallocatechin-3-gallate (EGCG) for the treatment of Alzheimer’s disease. Int J Pharm 389: 207–212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart K., Cole D. (2005) The commercial harvest of devil’s claw ( Harpagophytum spp.) in southern Africa: the devil’s in the details; J Ethnopharmacol 100: 225–236 [DOI] [PubMed] [Google Scholar]
- Sudheesh S., Vijayalakshmi N.R. (2005) Flavonoids from punica granatum-potential antiperoxidative agents. Fitoterapia 76: 181–186 [DOI] [PubMed] [Google Scholar]
- Thomson M., Al-Qattan K.K., Al-Sawan S.M., Alnaqeeb M.A., Khan I., Ali M. (2002) The use of ginger (Zingiber officinale Rosc.) as a potential anti-inflammatory and antithrombotic agent. Prostaglandins Leukot Essent Fatty Acids 67: 475–478 [DOI] [PubMed] [Google Scholar]
- Tilwe G.H., Beria S., Turakhia N.H., Daftary G.V., Schiess W. (2001) Efficacy and tolerability of oral enzyme therapy as compared to diclofenac in active osteoarthritis of the knee joint: an open randomised controlled clinical trial. J Assoc Physicians India 49: 621–626 [PubMed] [Google Scholar]
- Toegel S., Wu S.Q., Piana C., Unger F.M., Wirth M., Goldring M.B., et al. (2008) Comparison between chondroprotective effects of glucosamine, curcumin, and diacerein in IL-1beta-stimulated C-28/I2 chondrocytes. Osteoarthritis Cartilage 16: 1205–1212 [DOI] [PubMed] [Google Scholar]
- Ullmann U., Haller J., Decourt J.P., Girault N., Girault J., Richard-Caudron A.S. (2003) A single ascending dose study of epigallocatechin gallate in healthy volunteers. J Int Med Res 31: 88–101 [DOI] [PubMed] [Google Scholar]
- Valerio L.G., Jr, Gonzales G.F. (2005) Toxicological aspects of the South American herbs cat’s claw (Uncaria tomentosa) and Maca (Lepidium meyenii): a critical synopsis. Toxicol Rev 24: 11–35 [DOI] [PubMed] [Google Scholar]
- van der Kraan W.B., van den Berg P.M. (2000) Anabolic and destructive mediators in osteoarthritis. Curr Opin Clin Nutr Metab Care 3: 205–211 [DOI] [PubMed] [Google Scholar]
- Vankemmelbeke M.N., Jones G.C., Fowles C., Ilic M.Z., Handley C.J., Day A.J., et al. (2003) Selective inhibition of ADAMTS-1,-4 and -5 by catechin gallate esters. Eur J Biochem 270: 2394–2403 [DOI] [PubMed] [Google Scholar]
- van het Hof K.H., Wiseman S.A., Yang C.S., Tijburg L.B. (1999) Plasma and lipoprotein levels of tea catechins following repeated tea consumption. Proc Soc Exp Biol Med 220: 203–209 [DOI] [PubMed] [Google Scholar]
- Vlachojannis J., Roufogalis B.D., Chrubasik S. (2008) Systematic review on the safety of Harpagophytum preparations for osteoarthritic and low back pain. Phytother Res 22: 149–152 [DOI] [PubMed] [Google Scholar]
- Wallace J.M. (2002) Nutritional and botanical modulation of the inflammatory cascade eicosanoids, cyclooxygenases, and lipoxygenases – as an adjunct in cancer therapy. Integr Cancer Ther 1: 7–37 [DOI] [PubMed] [Google Scholar]
- Warnock M., McBean D., Suter A., Tan J., Whittaker P. (2007) Effectiveness and safety of devil’s claw tablets in patients with general rheumatic disorders. Phytother Res 21: 1228–1233 [DOI] [PubMed] [Google Scholar]
- Watanabe K., Hatakoshi M. (2002) Punica granatum leaf extracts for inactivation of allergen. Japanese patent JP 2002370996, A2 20021224, 5
- White B. (2007) Ginger: an overview. Am Fam Physician 75: 1689–1691 [PubMed] [Google Scholar]
- Williams J.E. (2001) Review of antiviral and immunomodulating properties of plants of the Peruvian rainforest with a particular emphasis on unade Gato and Sangre de Grado. Altern Med Rev 6: 567–579 [PubMed] [Google Scholar]
- Xiao X., Yang Z.Q., Shi L.Q., Liu J., Chen W. (2008) Antiviral effect of epigallocatechin gallate (EGCG) on influenza A virus. Zhongguo Zhong Yao Za Zhi 3: 2678–2682 [PubMed] [Google Scholar]
- Yelin E. (2003) The economics of osteoarthritis. In Brandt K.D., Doherty M., Lohmander L.S. (ed), Osteoarthritis. Oxford: Oxford University Press, pp. 17–21 [Google Scholar]
- Zeisel S.H. (1999) Regulation of ‘nutraceuticals’. Science 285: 1853–1855 [DOI] [PubMed] [Google Scholar]
- Zhang Z.F., Li Q., Liang J., Dai X.Q., Ding Y., Wang J.B., et al. (2010) Epigallocatechin-3-O-gallate(EGCG) protects the insulin sensitivity in rat L6 muscle cells exposed to dexamethasone condition. Phytomedicine 17: 14–18 [DOI] [PubMed] [Google Scholar]
- Zhao W., Entschladen F., Liu H., Niggemann B., Fang Q., Zenker K.S., et al. (2003) Boswellic acid acetate induced differentiation and apoptosis in highly metastatic [DOI] [PubMed]