Abstract
FARS and NASS CDS data were analyzed to determine time and cause of occupant deaths resulting from light vehicle crashes in the early 1990s. The results shows 46 percent of the deaths occurred within half an hour, 24 percent between half an hour and an hour and a half and a total of 90 percent within 24 hours. Of the deaths occurring during the 1.5 hours following injury 52 percent were the result of head injuries and 36 percent were the result of thorax injuries. When compared with the classical Trunkey tri-modal model, the “immediate” deaths are similar in time but somewhat lower in magnitude, the “early” deaths are earlier and somewhat lower in magnitude, and there is no evidence of a “late” peak. These results suggest that the tri-modal model may need to be modified to reflect current conditions.
Recent technological advances bring the possibility of nearly instant notification to prehospital care providers that a motor vehicle crash has occurred, including how severe any resulting injuries might be. This has generated an interest in the time to death and specific cause of death resulting from motor vehicle crashes in order to determine the potential benefits of this technology. This study was undertaken to determine if the traumatic fatal injury pattern identified by Trunkey (1983) was valid for current motor vehicle occupant fatal injuries.
In his study of 862 cases, Trunkey found that more than half of the deaths were “immediate”, occurring within half an hour. The bulk of these immediate deaths occurred in less than 10 minutes, primarily the result of injury to the brain, spinal cord, heart or major blood vessel. Trunkey proposed that few, if any, of these fatalities could be saved. Approximately 30 percent of the total deaths occurred between half an hour and 3 hours post injury, with a peak at about an hour and a half after injury. These “early” deaths often resulted from major internal hemorrhage or severe blood loss. Trunkey argued that early medical intervention could save many of these patients. The remainder of the deaths were classified as “late deaths.” Mostly due to infection or multiple organ failure, they were normally distributed with respect to time, peaking between 3 and 4 weeks following injury.
Two recent studies of the time to traumatic death reevaluated this distribution. Sauaia et al. (1995) found a trimodal distribution but with different peaks than Trunkey. They found fewer prehospital deaths than Trunkey (33 percent), and an increase in transported patients who died within 48 hours (53 percent). They attributed these differences to improvements in prehospital care. The authors report that 73 percent of blunt deaths occurred within 48 hours. Whereas the Trunkey and Sauaia et al. studies were urban, Meislin et al. (1997) did not observe a trimodal distribution in a diverse geographical setting. Approximately half of the deaths were pronounced dead at the scene, primarily the result of self-inflicted gunshot wounds. They found two distinct peaks among those treated at trauma centers. Twenty three percent died within 60 minutes and 35 percent died between 24 and 48 hours. A number of other reports relating to time to death from traumatic motor vehicle injury also show that a high percentage of deaths resulting from motor vehicle injury can be classified as immediate deaths (Table 1).
Table 1.
Summary of Literature Showing Percent of Motor Vehicle Deaths at Scene or Shortly Thereafter
| Geographic Location | Number of Cases | Percent | |||
|---|---|---|---|---|---|
| Dead at Scene | Dead in Transport | Total Dead within 1 hr. | Total Dead within 24 hrs. | ||
| Rural Michigan Preventable Mortality (Mostly motor vehicle) (Maio et al., 1995) | 155 | 58 | 72 | ||
| Rural New South Wales, Australia (Papadimitriou et al. 1994) | 82 | 79 | 11 | 100 | |
| County of Southern Jutland, Denmark (Madsen et al., 1996) | 299 | 60 | 8 | 72 | |
| Connecticut (Thibeault, 1997) | NA | 47 | 77 | ||
| Rural Washington (Grossman et al. 1995) | 13 | 69 | |||
| South Australia(Children 14 and under) (Simpson et al., 1992) | 115 | 68 | |||
A review of the literature on cause of traumatic fatal injury, summarized in Table 2, shows head and thorax injuries, as well as hemorrhage as a leading causes of death from blunt trauma.
Table 2.
Summary of Literature Showing Causes of Traumatic Death
| Type of Study | Causes of Traumatic Death |
|---|---|
| Cervical injuries in motor vehicle crashes (Huelke et al. 1981) | Cervical injuries |
| Causes of fatal motor vehicle crash injuries (Nagnibeda and Zaitsev, 1984) | A combination of injuries to the skull and brain, the locomotor system, blood loss and shock. |
| Prehospital deaths resulting from motor vehicle injury (Gelroy, 1985) | Aspiration of blood or vomit |
| Aspiration as a cause of death (Ottoson, 1985) | Aspiration |
| Motor vehicle related deaths (Bota and Cox, 1986) | Hemorrhage, airway disfunction, pulmonary contusion and head injuries |
| Motor vehicle crash fatalities (McCoy et al., 1989) | Cerebral injury, uncontrollable hemorrhage, mainly thoracic, a combination of these two |
| Death in a Level 1 trauma center (Shackford et al., 1989) | Central nervous system, hemorrhage |
| Childhood death from motor vehicle, pedestrian or pedal cycle involvements(Simpson et al., 1992) | Devastating brain and/or trunk visceral injuries |
| Prehospital deaths from accidental injury (Hussain and Rend, 1994) | “Important neurological injury” |
| Death in a Level 1 trauma center resulting from blunt trauma (Seigel, 1995) | Isolated brain injury as well as brain injury coupled with another systemic injury |
| Motor vehicle crash injuries with AIS 3+ injuries in at least two body regions (Larsen and Jorgensen, 1995) | Thorax, brain, abdomen |
| All trauma fatalities (Rogers et al., 1997) | Multisystem organ failure for rural deaths, head injury for urban injuries |
| Prehospital resuscitation (Hill et al., 1997) | Head injuries, with associated injuries depending on the GCS value |
DATA
Fatality data were taken from the National Highway Traffic Safety Administration’s (NHTSA) 1995 Fatal Analysis Report System (FARS) file. FARS is a census of all motor vehicle fatalities in the United States. The data are collected by the states from all available sources and put into a consistent format for aggregation into a national database. FARS data for 1995 include 31,897 light vehicle occupant fatalities. (Light vehicles include passenger automobiles and light trucks, which in turn include pickups, vans, and sports utility vehicles.) Data on time from injury to death were available on 29,475 of these, 92 percent of the total.
Cause of death data were taken from the National Automotive Sampling System, Crashworthiness Data System (NASS CDS) databases. This database is a structured sample of police reported crashes in which at least one of the vehicles was towed from the scene. NASS CDS typically collects data on about 6,000 crashes a year, with information on about 450 fatalities. Data are collected by trained crash investigators and injury data are taken from hospital records. The unweighted non-survivor data were aggregated into a single database for the period 1994–1996. The total database included 1337 cases. An additional 45 people were determined to have died from disease. This category includes those cases where the onset of the disease occurred prior to the first harmful event of the crash or when an official medical report verified that death resulted from either a diseased condition or that death was not caused by crash related injuries. NASS CDS data for time of death are available for the period 0 to 1.5 hours, hourly time segments from 1.5 to 23.5 hours, and then by days. Weighted data were also analyzed with similar results. For clarity, only unweighted data are reported in this paper.
RESULTS
TIME TO DEATH
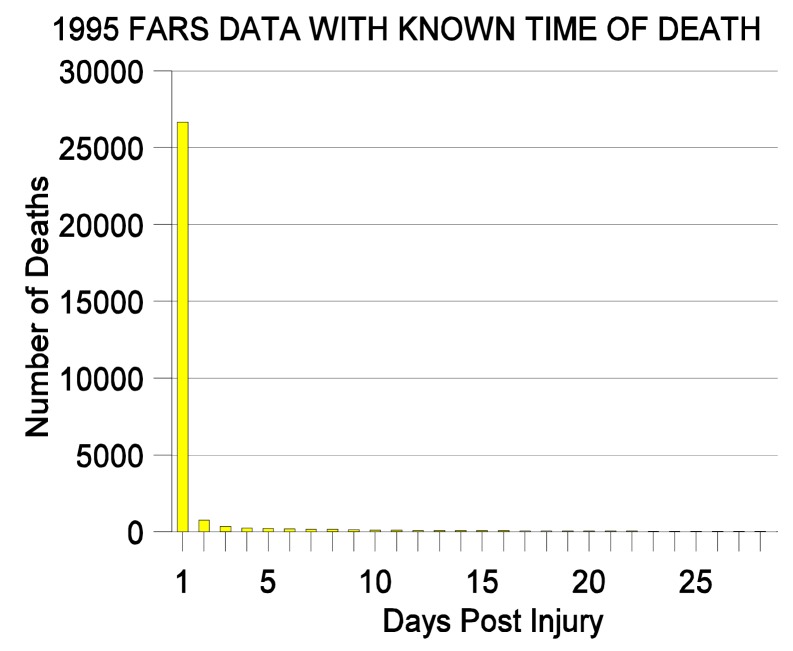
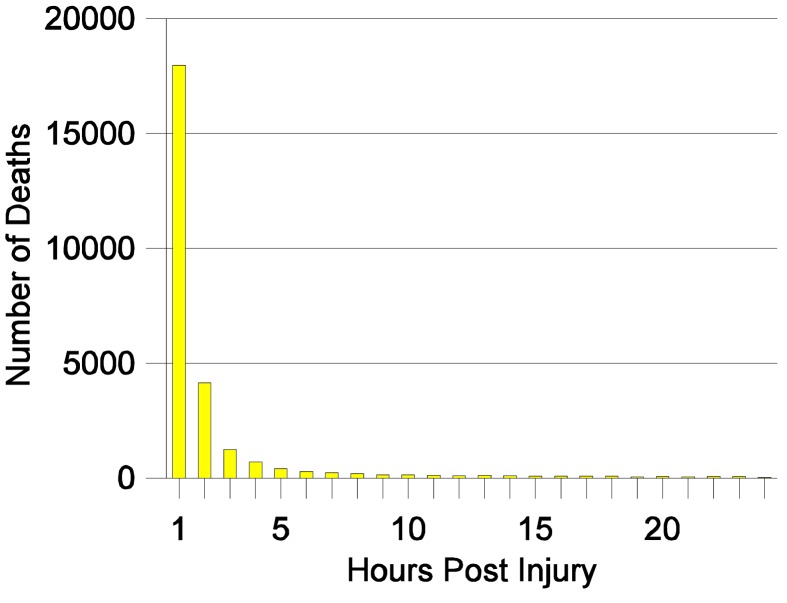
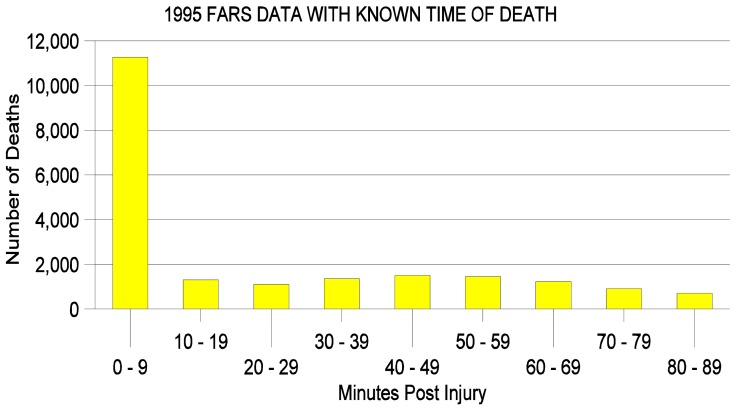
Figures 1, 2, and 3 show the number of people with known time to death who died in a light vehicle crash.
Figure 1.
Figure 2.
LIGHT VEHICLE OCCUPANT DEATHS
Figure 3.
LIGHT VEHICLE OCCUPANT DEATHS
Figure 1 shows the number who died by days, Figure 2 by hours, and Figure 3 by minutes. These figures show that ninety percent of the deaths occurred within 24 hours after injury, 61 percent within an hour and 38 percent within ten minutes.
There is close agreement between the time to death data from the FARS and NASS CDS data sets. The NASS data show that 77 percent of the deaths occurred in the first hour and a half, and the FARS data show 71 percent. For the period 1.5 hours to 2.5 hours the NASS data show 6 percent and FARS data show 7 percent. In the following hour both show 3 percent of the fatalities occurring in that period.
CAUSE OF DEATH
A quarter of all the fatalities in the 1994–1996 NASS CDS file experienced an MAIS 6 injury, including one in ten with a MAIS 6 head injury and an additional one in ten with a MAIS 6 thorax injury. Overall, nearly half of the non-survivors had a head injury as the MAIS injury. Slightly more than a quarter had a thoracic injury as the most severe injury. Non-survivors had an average of 15 injuries per person, with lower extremity injuries predominating as the non-MAIS injuries.
The similarity among the percentage of deaths in similar time periods for the FARS and NASS CDS data sets suggests that the cause of death seen in the NASS data for the different time periods following injury can be considered relevant to the fatalities seen in FARS. During the first 1.5 hours following injury -- the earliest time reported in the NASS CDS data set -- 905 deaths occurred, and of these 559 records (62 percent) included information on the “1st Medically Reported Cause of Death.” This variable indicates the cause of death based on information provided by the medical professional completing the report or by trained NASS Zone Center injury coders based on the official medical records. Table 3 summarizes these injuries. Note that the body regions are as defined in the AIS 90 dictionary.
Table 3.
Fatal Injury Pattern during 1.5 Hours Post Injury 1994–1996 Unweighted NASS CDS Non-Survivors with listed Cause of Death
| Body Region | AIS LEVEL | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| Head | 10 | 26 | 63 | 62 | 95 | 33 | 289 | |
| Face | 1 | 1 | 2 | |||||
| Neck | 1 | 3 | 1 | 5 | ||||
| Thorax | 2 | 28 | 68 | 101 | 3 | 202 | ||
| Abdomen | 1 | 3 | 5 | 9 | ||||
| Spine | 11 | 6 | 6 | 15 | 38 | |||
| Upper Ext. | 0 | |||||||
| Lower Ext. | 1 | 1 | ||||||
| External | 2 | 1 | 10 | 13 | ||||
| Total | 3 | 22 | 37 | 94 | 142 | 224 | 37 | 559 |
During the first hour and a half, 40 percent of the reported cause of death injuries were at the AIS 6 level, and 25 percent were at the AIS 5 level. Considering the body region of the reported cause of death, 52 percent were head injuries and 36 percent were thorax injuries. Cause of death injuries at the AIS 1 level appear to be an artifact of the analytical procedures used to sort the NASS CDS data. In each of these cases there were other injuries with unknown severity levels (that is associated injuries at the AIS 7 level).
DISCUSSION
These results suggest that the classical tri-modal pattern of time to death described by Trunkey is not valid for current motor vehicle occupant deaths.
The “immediate” deaths from motor vehicle crashes appear to be in general agreement with the Trunkey model with a very large portion of the deaths occurring in a relatively short time. However the 38 percent of the deaths in the first ten minutes and 46 percent within the first half hour, are somewhat lower than the more than 50 percent in the first half hour in the Trunkey data. During the 1.5 hours following injury, 40 percent of the deaths are reported as AIS 6 injuries. By definition, AIS 6 injuries are not presently medically treatable. Even though it is not known when these deaths occurred during the 1.5 hour period, it is reasonable to assume that they would likely to have occurred earlier rather than later during the period, supporting the 38 percent of deaths within ten minutes.
There appears to be a second mode in the FARS data, similar to Trunkey’s “early” deaths, but this too has a smaller portion of the total deaths than would be expected from the Trunkey model. This second peak also occurs earlier, centered around the 45 minute period rather than an hour and a half reported by Trunkey.
Following the “early” death surge, there appears to be a nearly linear decrease in the number of deaths over time, with no evidence of a surge in “late” deaths. This agrees with the reports of Sauaia et al. and Meislin et al.
The cause of death pattern found here agrees with the Trunkey model for the “immediate deaths” being largely the result of head and thorax injuries. Fifty two percent of fatal injuries during the 1.5 hours following injury are identified as head injuries and 36 percent are identified as thoracic injuries in the NASS CDS data. This too is in agreement with the Trunkey model.
There are insufficient data to identify the causes of the”early” deaths and as noted, there is no evidence of a surge in “late” deaths as a result of infection or multiple organ failure.
The results of this study are in general agreement with the literature on time and cause of death from traumatic injury, primarily motor vehicle related. The bulk of the reports in the literature are based on prospective studies with the number of cases varying from roughly 10 to less than 1,000. However, several limitations that must be kept in mind when making comparisons. In particular, all of the problems inherent with the use of retrospective data are applicable to these results.
One concern is that the data used to determine the time to death and cause of death were taken from two different retrospective data bases covering different time periods. The FARS data are applicable to 1995, and the NASS CDS data cover the period 1994 to 1996. This concern is somewhat mitigated by the overlap of the NASS and FARS time periods.
Although the time to death data from the FARS database is based on a relatively large number of cases, nearly 30,000, with 92 percent of the cases reporting a time of death, the time from injury to death must be questioned. The time of injury and time of death are recorded by different people in different circumstances. Time of injury is most suspect as it is likely to have been reported by a police officer in the field. Brodsky (1993) has shown that there is an over reporting of times by police at 5 minute intervals for urban deaths and 5 and 15 minute intervals for rural deaths. Time to death is likely to have been reported by a physician, as emergency medical technicians are often not authorized to pronounce death. However, if a person is reported as dead at the scene it is difficult to ascertain when the person was injured and when they died.
Among the limitations inherent in the cause of death taken from the NASS CDS data is the relatively small sample size and the use of 1.5 hours as the earliest recorded time. Even taking three years of data, there are only 1,337 cases. Of these cases, those of particular interest, that is those deaths occurring in the earliest time period, only 62 percent had a listed cause of death. Another limitation is that it cannot be determined if the cause of death listing reflects the opinion of a physician or of a nosoligist’s reading from the medical records.
CONCLUSION
Consideration should be given to modifying the Trunkey tri-modal model of traumatic injury deaths when applying it to current motor vehicle fatal injuries. Based on an analysis of FARS and NASS CDS data the “immediate” death portion of the tri-modal model appears to be valid for current motor vehicle occupant deaths with respect to time, but there appear to be fewer deaths during this time frame than would be expected from the model. There is evidence of an “early” death mode, but there appear to be fewer deaths and they are occurring earlier than would be expected from the model. There is no evidence of a “late” death mode either in the more recent literature or in the results of the analysis reported here.
REFERENCES
- Bota GW, Cox JE. Motor vehicle accidents in northeastern Ontario: Are preadmission deaths inevitable? Can Med Assoc J. 1986;134:1369–1372. [PMC free article] [PubMed] [Google Scholar]
- Brodsky H. The call for help after an injury road accident. Accident Analysis and Prevention. 1993;25(2):123–130. doi: 10.1016/0001-4575(93)90051-w. [DOI] [PubMed] [Google Scholar]
- Gelroy D. Deaths (144) from road traffic accidents occurring before arrival at hospital. Injury. 1985;16(4):241–242. doi: 10.1016/s0020-1383(85)80009-7. [DOI] [PubMed] [Google Scholar]
- Grossman DC, et al. From roadside to bedside: the regionalization of trauma care in a remote rural county. J Trauma. 1995;38:14–21. doi: 10.1097/00005373-199501000-00006. [DOI] [PubMed] [Google Scholar]
- Hill DA, Delaney LM, Roncal S. A chi-square automatic interaction detection (CHAID) analysis of factors determining trauma outcomes. J Trauma. 1995;42:62–66. doi: 10.1097/00005373-199701000-00011. [DOI] [PubMed] [Google Scholar]
- Huelke DF, O’Day J, Mendelsohn RA. Cervical injuries in automobile crashes. J Neursurg. 1981;54(3):316–322. doi: 10.3171/jns.1981.54.3.0316. [DOI] [PubMed] [Google Scholar]
- Hussain LM, Rend AD. Are Prehospital deaths from accidental injury preventable? BMJ. 1994;308(6936):1077–1080. doi: 10.1136/bmj.308.6936.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen MS, Jorgensen HR. Mortality among victims of traffic accident with multiple injuries. A descriptive study 1986–1990. Ugeskr Laeger. 1995;157(48):6716–6719. (Article in Danish) [PubMed] [Google Scholar]
- Madsen FQ, Hartmann-Andersen JF. Fatal traffic accidents in Denmark, survival time and factors of importance in the prehospital phase. Ugeskr Laeger. 1996;158:5432–5437. [PubMed] [Google Scholar]
- McCoy GF, et al. A review of fatal accidents in Oxfordshire over a 2 year period. Injury. 1989;20(2):65–68. doi: 10.1016/0020-1383(89)90141-1. [DOI] [PubMed] [Google Scholar]
- Meislin H, Criss EA, Judkins D, et al. Fatal trauma: The modal distribution of time to death is a function of patient demographics and regional resources. J Trauma. 1997;43:433–440. doi: 10.1097/00005373-199709000-00008. [DOI] [PubMed] [Google Scholar]
- Nagnibeda AN, Zaitsev EI. Analysis of the causes of the fatal outcome of injuries in traffic accidents and their diagnosis (in Russian) Vestn Khir. 1984;138(8):80–83. [PubMed] [Google Scholar]
- Ottoson A. Aspiration and obstructed airways as the cause of death in 158 consecutive traffic fatalities. J Trauma. 1985;25(6):538–540. doi: 10.1097/00005373-198506000-00012. [DOI] [PubMed] [Google Scholar]
- Papadimitriou DG, Mathur MN, Hill DA.A survey of rural road fatalities. Aust N Z J Surg 64479–483.1994 [DOI] [PubMed] [Google Scholar]
- Rogers FB, Shackford SR, Hoyt DB, Camp I, Osler TM, Mackersie RC, Davis JW. Trauma deaths in a mature urban vs rural trauma system. A comparison. Arch Surg. 1997;132(4):376–381. doi: 10.1001/archsurg.1997.01430280050007. [DOI] [PubMed] [Google Scholar]
- Sauaia A, Moore FA, Moore EE, et al. Epidemiology of traumatic deaths: a reassessment. J Trauma. 1995 Feb;38(2):185–193. doi: 10.1097/00005373-199502000-00006. [DOI] [PubMed] [Google Scholar]
- Seigel JH. The effect of associated injuries, blood loss, and oxygen debt on death and disability in blunt traumatic brain injury: the need for early physiologic predictors of severity. J Neurotrauma. 1995;12:579–590. doi: 10.1089/neu.1995.12.579. [DOI] [PubMed] [Google Scholar]
- Shackford SE, Mackersie RD, Davis JW, Wolf PL, Hoyt DB. Epidemiology and pathology of traumatic deaths occurring at a Level I Trauma center in a regionalized system: the importance of secondary brain injury. J Trauma. 1989;29(10):1392–1397. doi: 10.1097/00005373-198910000-00018. [DOI] [PubMed] [Google Scholar]
- Simpson DA, et al. Head Injuries in infants and children: measures to reduce mortality and morbidity in road accidents. World J Surg. 1992;16:403–409. doi: 10.1007/BF02104439. [DOI] [PubMed] [Google Scholar]
- Thibeault L. Connecticut Healthcare Research and Education Foundation. 1997 Sep 10; Personal Communication. [Google Scholar]
- Trunkey DD. a. Scientific American. 1983;294(2):28–35. [PubMed] [Google Scholar]