Abstract
Two commercially available computer models were compared for reliability and validity in predicting the peak blood alcohol concentration (BAC) in 113 males and females, ages 21 to 81. All subjects consumed a constant amount of alcohol (30 grams) prior to undergoing breath testing to determine each person’s peak BAC. The observed BACs were then compared to the BACs estimated with each computer model. Both computer models seriously underestimated the observed BACs for these subjects. The results are discussed with particular reference to the need for additional studies of age, gender, and body composition as predictors of peak BACs in heterogeneous subject groups.
Epidemiological studies have determined that alcohol contributes significantly to both the risk [Hurst, 1973] and severity [House, Waller, & Stewart, 1982] of traffic fatalities and injuries. The probability of involvement in a serious crash has been shown to increase dramatically for blood alcohol concentrations (BAC) greater than 0.08 percent [Borkenstein, Crowther, Shumate et al., 1964; Zador, 1989]. In fact, studies have indicated that a driver’s information processing ability and judgment may be seriously degraded at BACs as low as 0.05 percent [NHTSA, 1997].
Nevertheless, the majority of the research on the effects of alcohol consumption on driving ability was carried out more than twenty years ago using relatively high BACs. Early studies of performance decrements in the skills related to driving were conducted at BACs as high as 0.15 percent [Sidell & Pless, 1971]. In contrast, relatively few studies have been conducted at lower BAC levels [Moskowitz, Burns, & Williams, 1985]. This makes it particularly difficult to generalize the results of previous studies of driver impairment to the lower BAC levels that have recently been adopted by several states.
In addition, the accuracy of the data collected in previous studies has been compromised by the lack of experimental rigor in achieving specific BAC levels in heterogeneous subject groups. Due in part to the problem of dosing subjects, the results of many of these studies are reported in terms of the average BAC achieved by a group of individuals. However, without an indication of the range and dispersion of the BAC values that were actually obtained, it is difficult to draw reliable conclusions about the degree of driver impairment that is likely to be associated with various BAC levels.
Another serious drawback of earlier studies lies in the use of predominantly young and middle-age male subjects [Rimm, Sininger, Faherty et al., 1982]. The lack of reliable information concerning alcohol’s effects on the driving ability of females and older persons makes it especially difficult to generalize past research results to the current driving environment. Historically, women and older subjects have been excepted from studies on alcohol and driving in an effort to limit the range of BACs achieved, since these persons typically reach higher BACs when administered doses of alcohol equivalent to that received by younger male subjects. To correct these deficiencies, better experimental methods are necessary so that subjects of all ages and both genders can be tested at lower BAC levels (i.e., in the more relevant range of 0.05 to 0.08 percent).
A number of factors in an individual person’s physiological profile (e.g., age, gender, body size, drinking history) have been investigated as predictors of the amount of alcohol a person must consume to reach a certain BAC. In addition to being useful for predicting BAC in a research setting, these factors are often included in alcohol charts, or nomograms, designed to assist individual drivers in the estimation of their own BAC level [Werch, 1988]. Numerous charts and instruments have been created to inform individuals of the BAC that will likely be reached based upon that person’s body weight, the number of drinks consumed, and the time period during which the alcohol is consumed [e.g., Matthews & Miller, 1979; Miller & Munoz, 1976; Rutgers University Center of Alcohol Studies, 1972].
However, these alcohol nomograms are often confusing and cumbersome to use, and reliance upon them may result in serious underestimation of the BAC that will be reached by anyone other than the average-sized young adult male. Even when they are used properly, these instruments may serve to exaggerate the differences between individuals when relied upon to make BAC estimations over longer periods of drinking time [Werch, 1987]. Failure to recognize the potential for incorrect BAC estimation with these charts can result in devastating consequences for persons who choose to use these devices as guidelines for driving after drinking.
In an effort to provide better clinical and educational tools for understanding blood alcohol calculation and prediction, investigators have developed computer models to assist in the estimation of peak BAC. The Computerized Blood Alcohol Calculator [cBAC; Addiction Research Foundation, 1991] and the Blood Alcohol Content Estimator [BACest; National Highway Traffic Safety Administration, 1994] are two of the models that have recently been developed. Although one purpose of these models is to assist researchers in accurately dosing subjects in alcohol studies, few validation studies have been conducted to assess the usefulness of these computer models for predicting BAC in a research setting [Breslin, Kapur, Sobell et al., 1997; Kapur, 1991].
The present study provides a test of the reliability and validity of each of the computer models for predicting peak BACs in a relatively heterogeneous subject group. The BACs observed within a group of normal weight and overweight male and female subjects after a single acute dose of alcohol are compared with the predicted BACs generated with the two commercially available computer programs. An identical amount of alcohol was given to each subject, thereby allowing for a direct comparison of the observed BACs obtained for these subjects with the BACs predicted by each computer model.
METHOD
SUBJECTS
One hundred-thirteen volunteer subjects (57 males and 56 females), ages 21–81, participated in the study. Subjects were recruited for three age groups (21–25; 35–48; and 59–81) to represent Young, Middle-age, and Older subjects. These are the ages at which the most dramatic changes in body composition have been noted across the life span [Watson, Watson & Batt, 1980].
Potential subjects were screened by investigators and queried with respect to known health conditions, prescription drug use, and current alcohol use. A modified version of the Khavari Alcohol Test [Khavari & Farber, 1978] was used to determine that participants could be considered “moderate” consumers of alcohol. Potential subjects were eliminated for any of the following reasons: evidence of problem drinking or recent drug use; being an abstainer or infrequent drinker; or the presence of physical illness or condition contraindicating the use of alcohol. Subjects were instructed to refrain from eating for at least 4 hours prior to testing. Written informed consent was obtained from each participant, and subjects were compensated $20.00 upon completing the testing procedure.
PROCEDURES
Alcohol Dose
A constant amount of alcohol was administered to each subject: 40 ml of 95% alcohol, or 30 grams alcohol by weight. This amount was chosen to ensure a medically safe and experimentally relevant range of BACs. Based on past research [Goist & Sutker, 1985; Sutker, Tabakoff, Goist et al., 1983] the projected range of BACs was 0.04 to 0.10. All subjects received the alcohol mixed in approximately 200 ml sugar-free non-carbonated fruit flavored beverage. This 20% concentration of alcohol is a commonly adopted dosing procedure [Radlow & Hurst, 1985; Savoie, Emory, & Moody-Thomas, 1988].
Testing Procedure
Subjects were tested in groups of 2–3. Testing took place at the same time each day (beginning at 12:00 Noon) to minimize possible circadian effects on the metabolism of alcohol [e.g., Lawrence, Herbert, & Jeffcoate, 1983]. Subjects had their height and weight measured, and initial breath tests were conducted to establish alcohol-free status prior to testing.
A 15 minute period was allowed for consumption of the alcoholic beverage, after which subjects rinsed their mouths with tap water and waited for an additional 15 minutes before beginning breath testing. Breath tests were conducted every 5–7 minutes using the Alcomonitor CC (Intoximeters Inc., St. Louis) until each subject’s peak BAC could be determined. Breath testing ceased when all subjects’ BACs indicated descent (i.e., two successively declining BAC measurements). At this time, subjects were offered food and soft drinks, and allowed to read or watch a movie. Subjects were allowed to leave the testing facility when their BACs had dropped below 0.03 percent.
Computer Software
The cBAC model uses height, weight, gender, and age (for males only) to provide an estimate of each subject’s body water [Watson et al., 1980]. The predicted cBAC for each subject is then based on the individual’s estimated body water, the number of drinks consumed, and the drinking time. The cBAC program calculates a standard drink as 13.5 grams of alcohol, thus the 30 grams of alcohol received by each participant was the equivalent of 2.22 standard drinks. The drinking time period was estimated at 0.5 hour to include the time allowed for consumption of the alcoholic beverage plus the 15 minute waiting period before breath testing began.
The BACest computer program utilizes only body weight and gender as subject variables. The predicted BACest is then estimated using population averages for the percentage of body water typically found in a person of a given body weight and gender. The BACest model assumes that there are approximately 12.6 grams of alcohol in one 12-oz.beer. Thus, the calculated equivalent number of beers consumed by each subject was 2.38, and the drinking time was estimated at 0.5 hour.
Bioelectrical Impedance Analysis (BIA)
The BIA-101A instrument (RJL Systems, Detroit) was used to determine each subject’s body water for comparison with the body water estimated with the cBAC program. A detailed description of the BIA procedure may be found in York and Pendergast (1990). Briefly, tetrapolar skin electrodes are attached to the hands and feet, and a constant (800 μA, 50KHz) alternating current is applied to measure the resistance to the passage of the electrical current through the body. With measurements of body length and impedance to the flow of electrical current (i.e., height2/resistance), the volume of the conducting medium (or total body water; TBW) can be reliably estimated [Kushner, Schoeller, Fjeld et al., 1992]. The reliability of BIA in determining TBW has been confirmed in comparison with isotope dilution techniques [Lukaski, 1987]. The software provided with the body composition analyzer utilizes an equation modeled by Lukaski (1987) to calculate the liters of TBW and the percentage of the body’s weight represented by body water.
DATA ANALYSES
Measures of dispersion for each set of scores by age/gender group were used to construct 95% confidence intervals around the mean values obtained with each method of BAC determination (i.e., observed BAC, cBAC prediction, and BACest prediction).
RESULTS
Neither of the computerized BAC prediction programs selected for this study reveals the algorithm used to calculate the predicted BAC. Thus, analyses are limited to general comparisons between the BAC values obtained with each model and the observed BACs for each group of subjects.
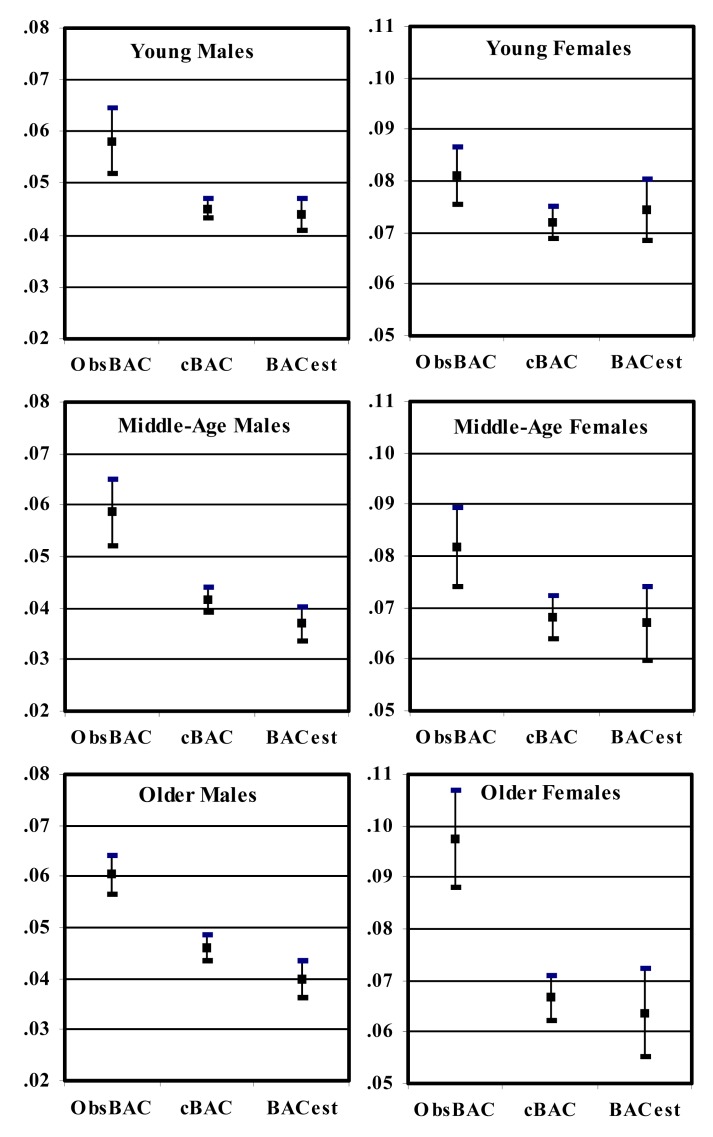
In light of the many variables that can make BAC estimations uncertain, researchers have proposed that estimated BACs should be reported as a range of predicted values, or 95% confidence intervals within which the observed value is expected to lie [O’Neill, Williams, & Dubowski, 1983; Arstein-Kerslake, 1986]. Thus, an analysis of the data was conducted to construct 95% confidence intervals around the mean values for each age/gender group using each BAC prediction model. As one can see, the cBAC and BACest predicted scores for each subject markedly underestimate the obtained BACs in a majority of the cases (Figure 1).
Figure 1.
BAC values obtained for each age/gender group.
(Note: Different BAC scales used for males and females).
Legend: - Upper and Lower 95% Confidence Limits
▪ Mean (Observed BAC, cBAC, and BACest models)
Figure 1 presents the mean values obtained with each of the models discussed in the previous section (cBAC, BACest, and observed BAC) as well as the 95% confidence intervals (CI) for each group of scores by age and gender. Note that the range of BAC values used to present the data for males is 0.02 to 0.08 percent, while the scale used for females is 0.05 to 0.11 percent.
Following the rationale for constructing CIs, one would expect the two computer models to be able to predict the mean BAC that would be observed in this group of subjects at least 95% of the time. However, the data indicate that the upper limits of the cBAC and BACest prediction models are both markedly different from the observed BAC for all groups except the Young Females. In fact, at no point do the 95% CIs for the three models overlap in the remaining 5 groups of subjects. Thus, the predicted BAC results generated by the two computer models would not have been optimal for estimating the peak BACs likely to be obtained in these subjects.
Table 1 presents the mean values (±SD) for each of the subject variables by age and gender group. As expected, the percentage of body fat increases across the ages for both males and females, with a corresponding decrease in percent body water [Watson et al., 1980]. However, multiple regression analyses demonstrated very little correlation between percent body fat or percent body water and the BACs that were observed for these subjects (R2 = .061 and .047, respectively). Thus, neither of these variables would be useful for estimating peak BAC.
Table 1.
Mean values (±SD) for each of the subject variables by each age and gender group.
| SUBJECT GROUP | AGE (yrs) | Ht. (cm) | Wt. (kg) | % FAT | % H2O | TBW (liters) | Dose (g/kg) | Dose (g/L) | Obs. BAC | cBAC Model | BACest Model |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Young Male x̄ (± SD) | 21.9 (1.1) | 179.6 (5.7) | 80.9 (11.3) | 18.8 (5.1) | 58.3 (3.6) | 47.0 (5.6) | .378 (.054) | .646 (.076) | .0581 (.014) | .0451 (.004) | .0440 (.007) |
| Middle-Age Male x̄ (± SD) | 42.5 (3.7) | 180.8 (6.6) | 93.1 (15.1) | 25.3 (5.4) | 53.9 (4.0) | 49.7 (5.9) | .330 (.049) | .612 (.075) | .0585 (.014) | .0417 (.005) | .0370 (.007) |
| Older Male x̄ (± SD) | 66.4 (5.0) | 177.7 (5.6) | 88.6 (12.6) | 29.4 (5.0) | 50.9 (3.6) | 44.6 (3.3) | .344 (.047) | .675 (.050) | .0604 (.007) | .0462 (.005) | .0400 (.007) |
| Young Female x̄ (± SD) | 21.7 (1.1) | 163.6 (7.4) | 60.9 (10.8) | 29.9 (6.5) | 51.3 (4.6) | 30.8 (3.0) | .506 (.081) | .982 (.096) | .0811 (.012) | .0719 (.007) | .0745 (.013) |
| Middle-Age Female x̄ (± SD) | 42.3 (3.4) | 163.3 (6.6) | 67.9 (14.0) | 35.5 (6.8) | 47.3 (4.9) | 31.5 (4.0) | .460 (.095) | .967 (.125) | .0818 (.016) | .0680 (.009) | .0670 (.015) |
| Older Female x̄ (± SD) | 68.9 (7.9) | 162.6 (3.9) | 70.7 (13.8) | 37.5 (6.7) | 45.0 (4.9) | 31.2 (3.1) | .440 (.088) | .970 (.094) | .0975 (.018) | .0666 (.008) | .0637 (.016) |
The administration of equal amounts of alcohol to each subject in the present study made it possible to compare the average dose received by each group in terms of grams of alcohol per kilogram of body weight (g/kg) and grams of alcohol per liter of body water (g/L). As one can see in Table 1, the older males received a slightly smaller dose of alcohol per kilogram of body weight, and a slightly larger dose per liter of body water compared to the younger males. However, the observed BACs for these groups did not differ significantly (.0604 and .0581, respectively). In contrast, the older females received smaller doses of alcohol based on both kilograms of body weight and liters of body water compared with the younger females; and the observed BACs for these groups were significantly different (.0811 compared with .0975, p<.05).
Overall, these results indicate that the changes in body weight and body water across the life span are different for males and females. Moreover, the relationships between these variables and the BACs observed for persons of different ages and gender are likely much more complex than previously proposed [Watson, Watson & Batt, 1981].
DISCUSSION
Our ability to accurately measure BAC and express the concentration of alcohol present in a person’s blood or breath forms the scientific basis for per se laws and legally accepted evidence in drinking and driving cases. However, the accuracy with which a person’s BAC can be measured has not been paralleled by the ability to accurately predict the BAC an individual will attain upon ingesting a given amount of alcohol. According to Arstein-Kerslake (1986), government agencies charged with enforcing per se laws relating to alcohol-impaired driving have a legal imperative to make available to the driving public information concerning the BACs that result from the consumption of alcoholic beverages. This information is typically provided in the form of alcohol charts or nomograms that may be used to estimate a person’s BAC [Werch, 1988].
More recently, computer models have been developed to assist researchers, educators, and law enforcement officials with prediction of the BAC that will likely be attained by an individual of a given height, weight, age, and gender [Addiction Research Foundation, 1991; National Highway Traffic Safety Administration, 1994]. To the extent that these devices may be considered useful, they should neither overestimate nor underestimate the BACs that are likely to be observed in the general population. However, as demonstrated above, both the cBAC and BACest models seriously underestimated the BACs that were observed in these subjects.
One factor that may have impacted the results obtained in the present study was the 4-hour fasting condition imposed on the subjects. Neither of the computer models tested in the present study made specific recommendations for dealing with the presence or absence of food in the stomach at the time of BAC estimation. However, the cBAC model was based on the mathematical equations developed by Widmark, who used a fasting condition for his subjects [Kapur, 1991]. Similarly, the BACest program assumes instaneous absorption and distribution of alcohol throughout the body. This condition is most likely to occur when there is no food in the stomach to delay absorption. Therefore, it appears that the fasting condition adopted in the present study did not violate the underlying assumptions of either computer model.
It was also necessary to explore the possibility that the errors in BAC prediction generated by the two computer models may have resulted from reduced reliability of these BAC estimation programs for overweight persons (> 15% above ideal body weight). However, there were several overweight subjects in each of the age/gender groups, and further examination of the BAC data obtained for the overweight subjects failed to reveal bias or limitation in BAC prediction for these persons. In fact, the computer-generated BAC estimations for these subjects were actually closer to the observed BACs. This might indicate that too much importance is being placed on body weight as the best estimator of BAC.
Indeed, the cBAC program claims that body weight is the most important factor in determining BAC, since an increase in body weight results in an increase in body water [Kapur, 1991]. However, the relationship between body weight, body water, and BAC is much more complex than this statement reflects. Body water estimates are thought to provide the best estimation of the volume of distribution for ethanol in the body [York & Hirsch, 1997]. However, since fat tissue contains relatively little water, each kilogram of excess body weight (fat tissue) results in very little additional body water volume to dilute the alcohol [Devgun & Dunbar, 1990]. Thus, the most likely explanation for the discrepancies between the observed and predicted BACs in the present study lies in the complex relationship between body weight, body water, and BAC.
Since Widmark’s original work (1932), there have been several revisions of the equations used to predict BAC. Most notably, Watson et al. (1981) updated Widmark’s work and provided equations derived for expressing the relationship between the amount of alcohol ingested and BAC in terms of total body water and the blood water fraction, rather than body weight alone. Both of the computer models emphasize the importance of estimating body water when calculating and predicting BAC. Thus, further scrutiny of the methods used to estimate body water is warranted.
Bioelectrical impedance was used to determine body water in the present study because we suspected that accurate body water estimation might be the biggest obstacle to reliable BAC prediction. The body water volume obtained with BIA was compared to that obtained with the cBAC program, which uses the Watson et al. (1980) anthropometric equations to estimate body water. Regression of the cBAC-estimated body water values on the TBW values estimated with bioelectrical impedance indicated that the two estimates of body water volume were highly comparable (r > .90). Thus, the discrepancies between observed BAC and the cBAC predictions do not appear to have resulted from differences in the reliability of the two methods of obtaining each subject’s total body water volume.
The BACest model, by comparison, relies on population averages to estimate body water as a percentage of body weight. This model assumes that body water is approximately 58% of the body weight for males, and 49% for females. However, body water percentages do not provide reliable estimates of body water volume. Two examples from the present study serve to further illustrate the complexity of the relationship between body weight, percent body water, and body water volume.
In the first example, the body weights for two of the male subjects in the study differed by less than 2 kilograms. However, their corresponding percentages of body water determined with BIA were 48% and 61%, and their TBW volumes were 36.3 and 46.7 liters, respectively. Had we used the 58% average assumed in the BACest model, the TBW volume for one of these males would have been significantly overestimated. In the second example, two of the female subjects in the study differed in body water volume by less than 3 liters. However, these subjects differed in body weight by more than 30 kg, and their body water percentages were 37% and 55%. It is evident from these examples that the relationship between body weight and body water is far more complex than the population averages adopted in the BACest program would suggest.
The narrow (conventional) treatment of body water as a percentage of body weight is likely the primary source of the limitations observed with the BACest model. On the other hand, the discrepancies between the observed BACs and those predicted by the cBAC model in the present study are most likely rooted in the algorithm utilized by the cBAC model to predict BAC from body water volume.
One of the more notable shortcomings of both computer models lies in estimating BACs in older females. Additional studies currently underway in our laboratory suggest that older females reach higher BACs in spite of body water volumes that are equivalent to that found in younger females [Davies & Bowen, in press]. A similar finding was recently reported by other investigators [Lucey, Hill, Young et al., 1999]. The reason(s) for this apparent anomaly remain to be determined, making the serious underestimation of BACs for older females in this study understandable. Collectively, the findings presented above suggest that additional studies are necessary to better define the relationship between body weight, body water, and the resultant BAC. In addition, future validation studies must include heterogeneous subject groups (e.g., males and females; obese and normal weight individuals; young and older subjects) to ensure that BAC prediction models are appropriate for a wide range of individuals.
The continued reliance upon per se legislation for enforcement of drunken driving laws, and the call for lowering the legal limit for intoxication to 0.08 percent BAC, make it imperative that we provide valid and reliable information to the public concerning the factors likely to impact blood alcohol concentration.
REFERENCES
- Addiction Research Foundation. Computerized Blood Alcohol Calculator; 1991.
- Arstein-Kerslake GW. A confidence interval approach to the development of blood alcohol concentration charts. Alc. Drugs Driving. 1986.;2:9–15. [Google Scholar]
- Borkenstein RF, Crowther RF, Shumate RP, Zeil WB, Zylman R. The Role of the Drinking Driver in Traffic Accidents. Bloomington, IN: Department of Police Administration, Indiana University; 1964. [Google Scholar]
- Breslin FC, Kapur BM, Sobell MB, Cappell H. Gender and alcohol dosing: A procedure for producing comparable breath alcohol curves for men and women. Alcohol Clin. Exp. Res. 1997.;21:928–930. doi: 10.1111/j.1530-0277.1997.tb03860.x. [DOI] [PubMed] [Google Scholar]
- Davies BT, Bowen CK. Total body water and peak alcohol concentration: A comparative study of young, middle-age, and older females. Alcohol Clin Exp Res. In press. [PubMed] [Google Scholar]
- Devgun MS, Dunbar JA. Alcohol consumption, blood alcohol level and the relevance of body weight in experimental design and analysis. J. Stud. Alc. 1990.;51:24–28. doi: 10.15288/jsa.1990.51.24. [DOI] [PubMed] [Google Scholar]
- Goist KC, Sutker PB. Acute alcohol intoxication and body composition in women and men. Pharmacol. Biochem. Behav. 1985.;22:811–814. doi: 10.1016/0091-3057(85)90532-5. [DOI] [PubMed] [Google Scholar]
- House EG, Waller PF, Stewart JR. Blood alcohol level and injury in traffic crashes. 26th Annual Proceedings of the American Association for Automotive Medicine. 1982:349–373. [Google Scholar]
- Hurst PM. Epidemiological aspects of alcohol in driver crashes and citations. J. Safety Res. 1973.;5:130–148. [Google Scholar]
- Kapur BM. CBAC: Computerized blood alcohol concentration. A computer model as a clinical and educational tool. Ann. Biochim. Clin. 1991.;30:36–39. [Google Scholar]
- Khavari KA, Farber PD. A profile instrument for the quantification and assessment of alcohol consumption: The Khavari alcohol test. J. Stud. Alc. 1978.;39:1525–1539. doi: 10.15288/jsa.1978.39.1525. [DOI] [PubMed] [Google Scholar]
- Kushner RF, Schoeller DA, Fjeld CR, Danford L. Is the impedance index (ht2/R) significant in predicting total body water? Am. J. Clin. Nutr. 1992.;56:835–839. doi: 10.1093/ajcn/56.5.835. [DOI] [PubMed] [Google Scholar]
- Lawrence NW, Herbert MA, Jeffcoate WJ. Circadian variation in effects of ethanol in man. Pharmacol. Biochem. Behav. 1983.;18:555–558. doi: 10.1016/0091-3057(83)90235-6. [DOI] [PubMed] [Google Scholar]
- Lucey MR, Hill EM, Young JP, Demo-Danenberg L, Beresford TP. The influences of age and gender on blood ethanol concentrations in healthy humans. J. Stud. Alc. 1999.;60:103–110. doi: 10.15288/jsa.1999.60.103. [DOI] [PubMed] [Google Scholar]
- Lukaski HC. Methods for the assessment of human body composition: Traditional and new. Am. J. Clin. Nutr. 1987.;46:537–556. doi: 10.1093/ajcn/46.4.537. [DOI] [PubMed] [Google Scholar]
- Matthews DB, Miller WR. Estimating blood alcohol concentration: Two computer programs and their applications in therapy and research. Add. Behav. 1979.;4:55–60. doi: 10.1016/0306-4603(79)90021-2. [DOI] [PubMed] [Google Scholar]
- Miller WR, Munoz RF. How to control your drinking. Englewood Califfs, NJ: Prentice-Hall; 1976. [Google Scholar]
- Moskowitz H, Burns M, Williams AF. Skills performance at low blood alcohol levels. J. Stud. Alc. 1985.;46:482–485. doi: 10.15288/jsa.1985.46.482. [DOI] [PubMed] [Google Scholar]
- National Highway Traffic Safety Administration. Blood Alcohol Content Estimator. U.S. Department of Transportation; Washington, D.C.: 1994. [Google Scholar]
- National Highway Traffic Safety Administration. Setting Limits, Saving Lives: The case for .08 BAC laws. U.S. Department of Transportation; Washington, D.C.: 1997. [Google Scholar]
- O’Neill B, Williams AF, Dubowski KM. Variability in blood alcohol concentrations: Implications for estimating individual results. J. Stud. Alc. 1983.;44:222–230. doi: 10.15288/jsa.1983.44.222. [DOI] [PubMed] [Google Scholar]
- Radlow R, Hurst PM. Temporal relations between blood alcohol concentration and alcohol effect: An experiment with human subjects. Psychopharmacol. 1985.;85:260–266. doi: 10.1007/BF00428184. [DOI] [PubMed] [Google Scholar]
- Rimm DC, Sininger RA, Faherty JD, Whitley MD, Perl MB. A balanced placebo investigation of the effects of alcohol vs. alcohol expectancy on simulated driving behavior. Add. Behav. 1982.;7:27–32. doi: 10.1016/0306-4603(82)90021-1. [DOI] [PubMed] [Google Scholar]
- Rutgers University Center of Alcohol Studies. Alco-Calculator: An Educational Instrument. New Brunswick, NJ: Author; 1972. [Google Scholar]
- Savoie TM, Emory EK, Moody-Thomas S. Acute alcohol intoxication in socially drinking female and male offspring of alcoholic fathers. J. Stud. Alc. 1988.;49:430–435. doi: 10.15288/jsa.1988.49.430. [DOI] [PubMed] [Google Scholar]
- Sidell FR, Pless JE. Ethyl alcohol: Blood levels and performance decrements after oral administration to man. Psychopharmacol. 1971.;19:246–261. doi: 10.1007/BF00401941. [DOI] [PubMed] [Google Scholar]
- Sutker PB, Tabakoff B, Goist KC, Randall CL. Acute alcohol intoxication, mood states and alcohol metabolism in women and men. Pharmacol. Biochem. Behav. 1983.;18:349–354. doi: 10.1016/0091-3057(83)90198-3. [DOI] [PubMed] [Google Scholar]
- Watson PE, Watson ID, Batt RD. Total body water volumes for adult males and females estimated from simple anthropometric measurements. Am. J. Clin. Nutr. 1980.;33:27–39. doi: 10.1093/ajcn/33.1.27. [DOI] [PubMed] [Google Scholar]
- Watson PE, Watson ID, Batt RD. Prediction of blood alcohol concentrations in human subjects: Updating the Widmark equation. J. Stud. Alc. 1981.;42:547–556. doi: 10.15288/jsa.1981.42.547. [DOI] [PubMed] [Google Scholar]
- Werch CE. Paraphernalia for teaching, training, and research on blood alcohol concentration. Int. J. Addict. 1987.;22:1213–1234. doi: 10.3109/10826088709027482. [DOI] [PubMed] [Google Scholar]
- Werch CE. Information on blood alcohol concentration: Evaluation of two alcohol nomograms. J. Drug. Ed. 1988.;18:81–92. doi: 10.2190/28QH-DLWM-DAQW-YDY9. [DOI] [PubMed] [Google Scholar]
- Widmark EMP. Die theoretischen Grundlagen und die praktische Verwendbarkeit der gerichlich-medizinischen Alkoholbestimmung. Berlin: Urban & Schwarzenberg; 1932. [Google Scholar]
- York JL, Hirsch JA. Association between blood pressure and lifetime drinking patterns in moderate drinkers. J. Stud. Alc. 1997.;58:480–485. doi: 10.15288/jsa.1997.58.480. [DOI] [PubMed] [Google Scholar]
- York JL, Pendergast DE. Body composition in detoxified alcoholics. Alcohol Clin. Exp. Res. 1990.;14:180–183. doi: 10.1111/j.1530-0277.1990.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Zador PL. Alcohol-related relative risk of fatal driver injuries in relation to driver age and sex. Arlington, VA: Insurance Institute for Highway Safety; 1989. [DOI] [PubMed] [Google Scholar]