Abstract
Background
Self-care training can reduce hospitalization for heart failure (HF), and more intensive intervention may benefit more vulnerable patients, including those with low literacy.
Methods and Results
A 1-year, multisite, randomized controlled comparative effectiveness trial with 605 patients with HF. Those randomized to single session received a 40-minute in-person, literacy-sensitive training; the multisession group received the same initial training and then ongoing telephone-based support. The primary outcome was combined incidence of all-cause hospitalization or death; secondary outcomes included HF-related hospitalization and HF-related quality of life (HFQOL) with pre-specified stratification by literacy. Overall, the incidence of all-cause hospitalization and death did not differ between intervention groups (incidence rate ratio (IRR)=1.01 (95% Confidence Interval (CI): 0.83, 1.22). The effect of multisession training compared with single session training differed by literacy group: among low literacy, multisession yielded lower incidence of all-cause hospitalization and death: IRR=0.75 (0.45,1.25); and among higher literacy, multisession yielded higher incidence: IRR=1.22 (0.99,1.50) (interaction p=0.048). For HF-related hospitalization: among low literacy, multisession yielded lower incidence: IRR=0.53 (95% CI: 0.25,1.12); and among higher literacy, multisession yielded higher incidence: IRR=1.32 (95% CI: 0.92,1.88) (interaction p=0.005). HFQOL improved more for patients receiving multisession compared with single session at 1 and 6 months, but the difference at 12 months was smaller. Effects on HFQOL did not differ by literacy.
Conclusions
Overall, an intensive multisession intervention did not change clinical outcomes compared with a single session intervention. People with low literacy appear to benefit more from multisession than people with higher literacy.
Clinical Trial Registration Information
ClinicalTrials.gov; Identifier: NCT00378950.
Keywords: heart failure, self-management, literacy
Introduction
Heart failure (HF) self-care training can decrease hospitalizations, delay mortality, and improve HF-related quality of life (HFQOL). 1, 2 Although self-care training appears to have important benefits for patients, the optimal design remains unclear. Previously effective trials have tested interventions that range from one session to several sessions, and generally compare with usual care. 1-4 We do not know the optimal amount of training, whether ongoing support is needed, the best mode of administration, the setting, or the target populations. 5 Some evidence suggests that training may be particularly beneficial for vulnerable patients, including those with lower socioeconomic status (SES) and/or low literacy skills. 3, 6
Low literacy is a risk factor for several adverse outcomes including all-cause mortality, 7-9 all-cause hospitalization, 10, 11 and HF-related hospitalization. 12 Literacy appears to be an independent predictor of outcomes distinct from educational attainment and other measures of SES. 13 Previous studies, including our own single-center trial, have demonstrated that self-care training or intensive care management programs improve outcomes when compared with less intensive interventions or usual care, and that these effects are equal or greater among patients with low literacy skills. 3, 12, 14, 15 This suggests that the level of support required to optimize health outcomes may vary according to literacy level.
Because patients with low literacy often have knowledge deficits and may need more intensive instruction to master HF self-care, we developed a program that tailors instruction to need and seeks to create sustained mastery. We were interested in whether the effects of this more intensive, multisession intervention offered more benefit than a single session of training, and whether more intensive training would have a differential effect based on literacy level. Thus, we conducted a randomized, controlled trial to compare the effects of two different amounts of self-care training on the incidence of all-cause hospitalization and death. Our secondary outcomes were incidence of HF-related hospitalizations and HFQOL.
Methods
We conducted a randomized trial (ClinicalTrials.gov NCT00378950) comparing the effectiveness of a single session versus a more intensive multisession education program. Details regarding study participant eligibility, recruitment procedures, and data collection processes have been previously described and are summarized here. 16 The study protocol was approved by the Institutional Review Board Human Subjects Committees at all sites.
Setting and Participants
Study participants were enrolled from 2007 to 2009 from General Internal Medicine and Cardiology clinics at four sites: University of North Carolina at Chapel Hill; Feinberg School of Medicine, Northwestern University; University of California, San Francisco-San Francisco General Hospital; and Olive View-UCLA Medical Center. To be included in the study, each participant required a clinical diagnosis of HF, New York Heart Association (NYHA) class II-IV symptoms in the past 6 months, current use of a loop diuretic, fluency in English or Spanish, and adequate cognitive functioning based on the Mini-Cog screener.17 A clinical diagnosis of heart failure required the patient’s physician to diagnose heart failure and one of the following test results: 1) left ventricular hypertrophy on electrocardiogram or echocardiogram, 2) ejection fraction less than 50%, 3) pulmonary edema on chest x-ray, or 4) elevated b-type natriuretic peptide.
Recruitment, Baseline Interview, Initial Education, and Randomization
Potential participants were approached at regular outpatient appointments. Those agreeing to participate provided informed consent. Subsequently, the research assistant (RA) administered baseline questionnaires. At the end of the baseline assessment, all participants received the initial training session from the site’s health educator. The initial training session was approximately 40 minutes long and included review of daily self-assessment and action planning in case of exacerbation, salt avoidance, exercise, and medication adherence. Participants also received the Caring for Your Heart: Living Well with HF education manual (http://www.nchealthliteracy.org/hfselfmanage.html) and a new digital scale for weighing themselves. Our literacy-sensitive training materials were refined and expanded for this trial based on materials we previously developed and tested, and the training was grounded in social cognitive theory and learning theory.3, 18 The health educator at each site had a master’s degree in health education or related field and experience teaching patients in clinical settings. Prior to the start of enrollment, the educators participated in a 2-day training with the investigators that involved review of the intervention and role-play. Following that session, the educators met weekly with one of the investigators (D.A.D.) to continue role-play, discuss questions, and foster similar implementation of the interventions at each site. During the first 6 months of enrollment, educators recorded 2-3 telephone coaching sessions with patients (with permission) to facilitate training and quality assurance. These sessions were reviewed by a co-investigator (DAD) and the lead educator (VH) and discussed with the educators on group calls.
After the initial training session, participants were randomized to either the single session or multisession group, stratified by literacy and site. Randomization occurred in blocks of varying size (block sizes of 4, 6, and 8 for English speaking subjects, and 4 for Spanish speakers) that were unknown to the investigators, and group assignment was concealed in opaque consecutively numbered envelopes that were opened after the initial training session by the educator. RAs and investigators remained masked to study arm assignment.
Multisession Intervention Description
Those assigned to single session completed their session and continued with their usual care. Those assigned to multisession received the same initial session plus our more intensive education and self-care training intervention. 16, 19 The multisession intervention also included more specific instruction using daily weights to guide diuretic self-adjustment if the patient’s physician allowed it.
Over the next 4 weeks, the multisession participant was scheduled to receive 5-8 follow-up phone calls (approximately 10 minutes each) from the site’s health educator to reinforce the education and to guide the patient toward better self-care skills. During the first 2 calls, the health educator focused on reviewing the key behavior components of the program: performing and recording daily weights, assessing for symptoms, taking the proper dose of diuretic according to their weight (based on a plan developed with their provider), and calling the doctor when appropriate. This information continued to be reviewed at every call to assess adherence. Calls 3–8 focused on the other three elements of HF self-care: medication adherence, limiting salt, and exercise. The calls focused on reviewing the initial educational content, assessing the patient’s knowledge and behaviors, and providing additional information and motivation. After the first month, the educator initiated calls every 2 weeks until the patient demonstrated mastery for all content areas. The intent of the education sessions was to ensure mastery of the content, and to build self-efficacy toward carrying out the self-management activities. Once mastery was demonstrated, the educator called the patient monthly to check on their self-care and to encourage the patient to continue the program.
Importantly, all contact from the educator focused on self-care, and the educator did not serve as an advocate for the patient with the health care system or a conduit of information about patient status to the physician unless patient safety was at risk. The educator coached the patient on how to effectively contact the clinical practice and helped the patient understand important times when they should contact their healthcare providers. All education was delivered in the language preferred by the patient (English or Spanish) by a bilingual educator.
Study Measures
We abstracted age, gender, co-morbid conditions, prescribed medications, diagnostic lab tests, and echocardiogram results from the medical chart. All interviews were conducted verbally in the language of choice (English or Spanish) by a trained RA fluent in the language. During baseline interviews, we obtained race/ethnicity, insurance status, income, subjective SES, years of education, and medication use by self-report. HF severity was assessed by interview and categorized by NYHA class. Subjective SES was assessed using the MacArthur Scale of Subjective Social Status.20 All items that had not previously been administered in Spanish were translated by native Spanish speakers using forward and back translation.
Literacy was measured with the reading comprehension passages of the Short-Test of Functional Health Literacy in Adults (S-TOFHLA) in either English or Spanish. The S-TOFHLA is a 36-item, 7-minute timed test of reading comprehension, and is a reliable, validated measure of literacy in the health care context. 21 Each participant’s literacy level was categorized as either inadequate/marginal (0-22 correct answers), which we refer to as “low literacy,” or adequate literacy (23–36 correct). HFQOL was assessed at baseline using the validated Improving Chronic Illness Care Evaluation (ICICE) Heart Failure Symptom Scale (HFSS).22 The HFSS consists of 7 questions about health during the previous 4 weeks with a 5-point response scale; scores were transformed to a 100-point scale with 100 representing the least possible symptoms/best health. In our analyses, a difference of 14 points on the 0-100 scale is roughly equivalent to a difference in one level of NYHA classification.23
Outcome Assessment
Our primary outcome was combined incidence of all-cause hospitalization or death. Patients were interviewed at 6 and 12 months to determine if any hospitalizations had occurred in the previous time period, and if so, at which hospital(s) the event(s) took place. Following the interviews, we obtained the admission and discharge summaries for each hospitalization and also queried for any other hospitalizations occurring during the study at that site. At 12-month follow-up, we did an additional search for hospitalizations at the main clinical sites as well, regardless of whether the participant reported outcomes at that site. We confirmed deaths using a national death index which uses several databases, including the social security death index, and is updated monthly. 24 All assessors of outcome status were masked to study arm assignment. We used the medical record-confirmed events for analysis rather than self-reported counts.
To assess the secondary outcome of incidence of HF-related hospitalization, one member of the 3-member adjudication committee, masked to study arm assignment, reviewed the admission and discharge summaries to determine if the hospitalization was HF-related. The investigator used a study protocol and their clinical judgment to determine whether uncontrolled HF was an important contributing factor to the admission. If the first assessor decided the admission was definitely HF-related or definitely not HF-related, no further assessment was done. For all others, another assessor conducted a second assessment. If there was disagreement between the first two assessors, a third assessor reviewed the admission, and the case was discussed by the full committee to resolve the difference. We also obtained all emergency department visit records from institutions that participants said they visited. We evaluated emergency department visits for whether they were HF-related in the same manner as hospitalizations.
HFQOL was measured by interviewer-administered questionnaire at baseline, 1-month, 6-months, and 12-months.
We tracked the number and content of calls in the multisession group as an indicator of dose.
We reviewed all hospitalizations, deaths, and emergency department visits for potential adverse events caused by the interventions. Specifically, we evaluated for the presence of hypokalemia, renal insufficiency, volume depletion, and syncope. 16
Sample Size
Our sample size calculation is discussed in detail elsewhere.16 Using data from our previous trial to estimate event rates (1.63 events/person/year in the control group and 1.14 events/person/year in the intervention group),3 we aimed to study 600 patients with HF to achieve power of 0.9 to detect an incidence rate ratio of 0.7.16
Statistical Analysis
We compared differences in the incidence rates of the primary and secondary outcomes between the two study groups using negative binomial regression. 25, 26 We first compared crude (unadjusted) differences. Next, we repeated the models adjusting for those variables that were statistically significantly different between arms at baseline. The rate of the primary outcome differed across sites, so we included a site-level fixed effect. The variance was adjusted for clustering of patients within sites, and we adjusted for varying exposure due to time on trial. The number of patients per physician was low, so we did not adjust for clustering at the physician level. In our protocol, we pre-specified that we would adjust for variables with baseline differences detected at the p<0.05 level, so we conducted both adjusted and unadjusted analyses.
Because one of our hypotheses was that the effect of the intervention was moderated by literacy status, we conducted pre-specified subgroup analyses by literacy level; this was performed by including an indicator variable for low literacy and interacting this indicator with the study arm; a Wald test on the coefficient of the interaction term was used to test the hypothesis that literacy modified multisession effectiveness relative to single session.
We used generalized estimating equations to determine the change in HFQOL associated with the intervention. We specified a model with HFQOL as the dependent variable and covariates for the study arm and follow up period, with interactions to allow for the possibility of changes in the net effect of the intervention over time. We also performed subgroup analyses by interacting literacy with the study arm and follow up period.
Missing data on adjustment variables was imputed using best subset regression for HFQOL if only one item was missing (n=8 imputed) and using hot deck procedures for subjective economic status based on categories for schooling, income, and age (n=18 imputed).27 Of the 605 study subjects, 4 were excluded from the adjusted models due to missing HFQOL values.
Results
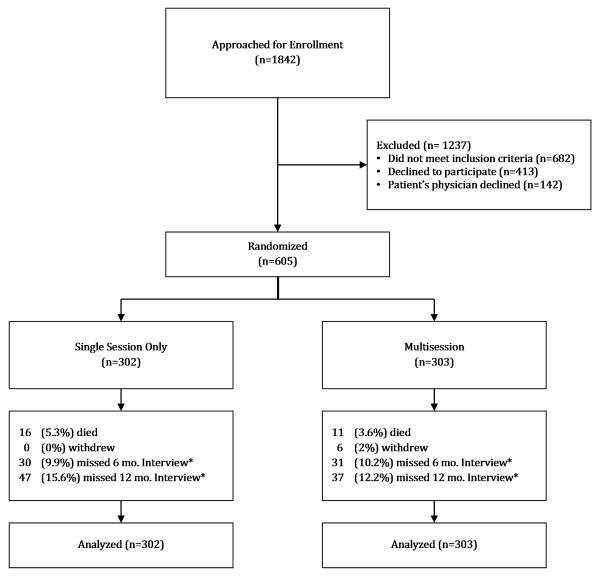
We approached 1842 patients for enrollment, 605 of whom were enrolled after meeting the inclusion criteria, agreeing to participate, and having their physician agree to allow participation (Figure 1).
Figure 1.
Flow diagram of progress through the study. Footnote at bottom of Figure 1:
*Response rates for the 6 and 12 month interviews differed by literacy group with lower literacy participants more likely to miss the interview (for example, at 12 months, response rate for low literacy was 80% and for higher literacy 90%). However, the difference in response rates by literacy was not different between the study groups.
Baseline demographic and clinical characteristics are shown in Table 1. The multisession and single session groups were statistically significantly different at baseline for HFQOL, use of angiotensin converting enzyme inhibitor or angiotensin receptor blocker (ACEI/ARB), and subjective SES (Table 1).
Table 1.
Demographic and clinical characteristics of the enrolled participants.
|
Overall Sample N(%) or Mean±SD |
Single Session Only N(%) or Mean±SD |
Multisession N(%) or Mean±SD |
P | |
|---|---|---|---|---|
| Size | 605 | 302 | 303 | |
| Demographics | ||||
| Literacy (TOFHLA) | 24.2±12.3 | 24.5±12.4 | 24.0±12.2 | 0.63 |
| Site | 1.00 | |||
| UNC | 216 (36) | 108 (36) | 108 (36) | |
| NU | 166 (27) | 83 (27) | 83 (27) | |
| UCSF | 148 (24) | 74 (25) | 74 (24) | |
| UCLA | 75 (12) | 37 (12) | 38 (13) | |
| Age | 60.7±13.1 | 60.3±12.3 | 61.1±13.8 | 0.49 |
| Race/Ethnicity | 0.73 | |||
| White, non-Hispanic | 233 (39) | 122 (40) | 111 (37) | |
| Hispanic | 97 (16) | 43 (14) | 54 (18) | |
| African American | 232 (38) | 114 (38) | 118 (39) | |
| Other | 41 (7) | 22 (7) | 19 (6) | |
| Missing | 2 (0) | 1 (0) | 1 (0) | |
| Gender: Male | 314 (52) | 156 (52) | 158 (52) | 0.90 |
| Language: English | 522 (87) | 261 (88) | 261 (87) | 0.67 |
| Income Level, $ | 0.91 | |||
| <15,000 | 305 (52) | 153 (52) | 152 (52) | |
| 15,000-24,999 | 92 (16) | 43 (15) | 49 (17) | |
| 25,000-40,000 | 67 (11) | 35 (12) | 32 (11) | |
| >40,000 | 125 (21) | 63 (21) | 62 (21) | |
| Education Level | 0.22 | |||
| <12th grade | 160 (26) | 78 (26) | 82 (27) | |
| High School | 177 (29) | 86 (28) | 91 (30) | |
| Some college | 140 (23) | 64 (21) | 76 (25) | |
| College graduate or greater |
128 (21) | 74 (25) | 54 (18) | |
| Subjective | 5 (3, 7) | 5 (3, 7) | 4 (2, 6) | 0.01* |
| Socioeconomic Status (median and interquartile range) |
||||
| Insurance | 0.76 | |||
| Medicare Only | 65 (11) | 28 (9) | 37 (12) | |
| Medicare & Medicaid | 104 (17) | 52 (17) | 52 (17) | |
| Medicare & Private | 129 (21) | 68 (23) | 61 (20) | |
| Medicaid | 151 (25) | 77 (25) | 74 (24) | |
| Private | 77 (13) | 35 (12) | 42 (14) | |
| Uninsured | 79 (13) | 42 (14) | 37 (12) | |
| Clinical Characteristics | ||||
| HFSS | 61±22 | 63±22 | 59±22 | 0.02 |
| NYHA Class at baseline | 0.556* | |||
| I | 114 (19) | 60 (20) | 54 (18) | |
| II | 304 (50) | 152 (50) | 152 (50) | |
| III | 118 (20) | 56 (19) | 62 (20) | |
| IV | 69 (11) | 34 (11) | 35 (12) | |
| Systolic Dysfunction: | 355 (59) | 186 (62) | 169 (56) | 0.15 |
| LV Ejection fraction <0.45 |
||||
| Systolic BP (mm/Hg) | 125±23 | 124±22 | 125±24 | 0.58 |
| Diastolic BP (mm/Hg) | 71±13 | 72±14 | 71±12 | 0.34 |
| Body Mass index | 33.1±8.9 | 33.8±9.0 | 32.5±8.7 | 0.09 |
| Creatinine level | 1.3±0.5 | 1.2±0.5 | 1.3±0.6 | 0.19 |
| Diabetes | 290 (48) | 140 (46) | 150 (50) | 0.44 |
| Hypertension | 513 (85) | 257 (85) | 256 (84) | 0.83 |
| Atrial Fibrillation | 288 (48) | 136 (45) | 152 (50) | 0.21 |
| Previous MI or angina | 230 (38) | 112 (37) | 118 (39) | 0.64 |
| PHQ Depression Score | 7.5±5.4 | 7.1±5.3 | 7.8±5.6 | 0.12 |
| Current smoker | 96 (16) | 50 (17) | 46 (15) | 0.64 |
| Medication History | ||||
| ACE-I | 391 (66) | 200 (67) | 191 (64) | 0.37 |
| ARB | 120 (20) | 64 (21) | 56 (18) | 0.39 |
| ACE-I or ARB | 497 (82) | 258 (85) | 239 (79) | 0.04 |
| Beta blocker | 492 (82) | 251 (84) | 241 (80) | 0.16 |
| Spironolactone | 166 (27) | 90 (30) | 76 (25) | 0.20 |
Abbreviations: TOFHLA=Test of Functional Health Literacy in Adults, HFSS=Heart Failure Symptom Scale, NYHA=New York Heart Association, LV=Left Ventricular, BP=Blood Pressure, MI=Myocardial Infarction, PHQ=Patient Health Questionnaire, ACE-I=Angiotensin Converting Enzyme Inhibitor, ARB=Angiotensin Receptor Blocker.
For subjective socioeconomic status and NYHA class, we used the nonparametric Wilcoxon-Mann-Whitney rank-sum test. However, the conclusions remained the same regardless of statistical test used.
Over 12 months, patients in the TTG group received a mean of 14.2 calls (SD 4.8) with a mean duration of 12.0 minutes (SD 4.3) each.
Incidence of all-cause hospitalization and death
Overall, we found no difference between multisession and single session groups for the incidence of all-cause hospitalization or death over 12 months. The unadjusted incidence rate ratio (IRR) was 1.01 (95% Confidence Interval (CI): 0.83, 1.22) and adjusted IRR was 0.96 (95% CI: 0.70, 1.31) (adjusting for site, HFQOL, ACEI/ARB use, and subjective SES) for the multisession group compared with the single session group (Table 2).
Table 2.
All-cause and heart failure related hospitalization.
| Single Session Only | Multisession | ||||
|---|---|---|---|---|---|
| N | Incidence Rate/ Year |
Incidence Rate/ Year |
Unadjusted Incidence Rate Ratio |
Adjusted Incidence Rate Ratio* |
|
| All-cause Hospitalization or death |
|||||
| All | 605 | 0.73 | 0.75 | 1.01 (0.83,1.22) | 0.96 (0.70,1.31) |
| Inadequate Literacy | 225 | 0.90 | 0.73 | 0.75 (0.45,1.25) | 0.73 (0.39,1.36) |
| Adequate Literacy | 380 | 0.63 | 0.76 | 1.22 (0.99,1.50) | 1.16 (0.87,1.55) |
| HF-Related Hospitalization | |||||
| All | 605 | 0.30 | 0.27 | 0.92 (0.77,1.11) | 0.90 (0.70,1.15) |
| Inadequate Literacy | 225 | 0.40 | 0.22 | 0.53 (0.25,1.12) | 0.48† (0.24,0.92) |
| Adequate Literacy | 380 | 0.24 | 0.30 | 1.32 (0.92,1.88) | 1.34 (0.87,2.07) |
HF=heart failure
An incidence rate ratio less than 1.0 favors the multisession group over the single session group.
Adjusted for site, HFQOL, ACE/ARB use, and subjective SES.
Confidence intervals for unadjusted difference in medians use bootstrapping
p<0.05
We conducted a pre-specified subgroup analysis by literacy and found that for patients with low literacy, the IRR was 0.75 (95% CI: 0.45,1.25) and adjusted IRR was 0.73 (95% CI: 0.39,1.36) favoring the multisession group vs. the single session group. Among patients with higher literacy, the unadjusted IRR was 1.22 (95% CI: 0.99,1.50), and adjusted IRR was 1.16 (95% CI: 0.86,1.55) favoring the single session group. The effect of multisession differed by literacy level with an interaction p value of 0.048.
Secondary Outcomes
HF-related hospitalization
The unadjusted IRR was 0.92 (95% CI: 0.77, 1.11) and the adjusted IRR was 0.90 (95% CI: 0.70,1.15) favoring the multisession group vs. the single session group. Among patients with lower literacy the unadjusted IRR was 0.53 (95% CI: 0.25,1.12) and the adjusted IRR was 0.48 (95% CI: 0.24, 0.92) favoring the multisession group, and for those with higher literacy, the unadjusted IRR was 1.32 (95% CI: 0.92,1.88) and the adjusted IRR was 1.34 (95% CI: 0.87, 2.07) favoring the single session group. Again, the effect of multisession differed by literacy level with an interaction p value of 0.005.
Emergency Department Visits
Emergency department visits that did not result in hospitalization were not different between the multisession and single session group: unadjusted IRR was 0.82 (95% CI: 0.42, 1.64) and adjusted IRR was 0.79 (95% CI: 0.47, 1.31). The point estimate was not different by literacy and the interaction p value was not statistically significant: 0.85.
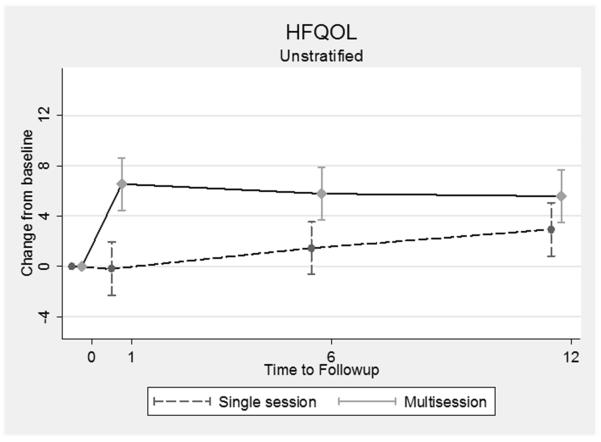
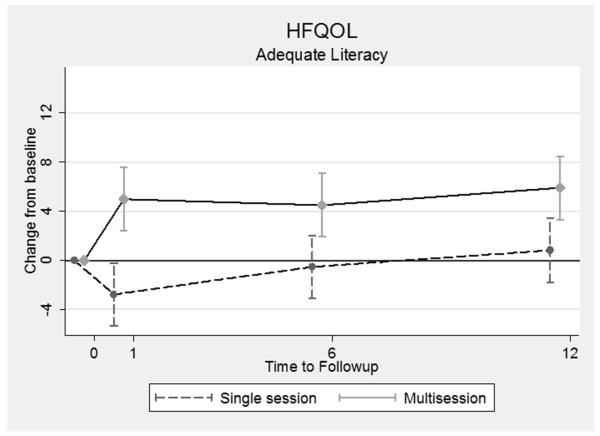
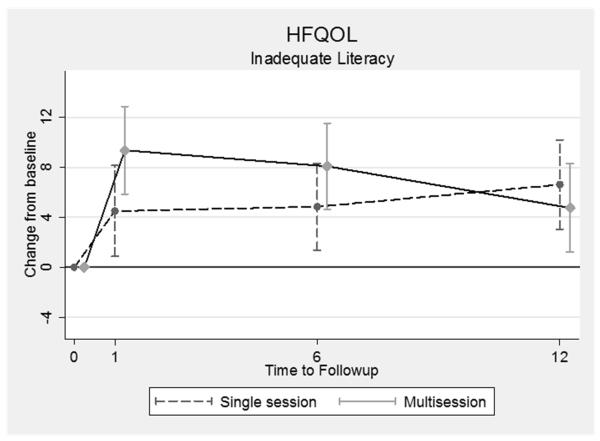
HFQOL
Patients in the multisession group had greater improvement in HFQOL from baseline at 1-month (as described previously28) and 6-month assessments (p <0.001 and p=0.003, respectively), but the differences between the groups waned over time (Figure 2). After 12 months, the differences between the groups was no longer statistically significant (2.62 points better for multisession, p=0.082). The greater improvement in HFQOL in the multisession group appears more sustained in the higher literacy subgroup than the lower literacy subgroup, but the interaction was not statistically significant (p=0.41) (Figure 2).
Figure 2.
Change in HFQOL from baseline at 1, 6, and 12 months. (a) all study patients, (b) only those with adequate literacy, and (c) only those with lower (inadequte) literacy.
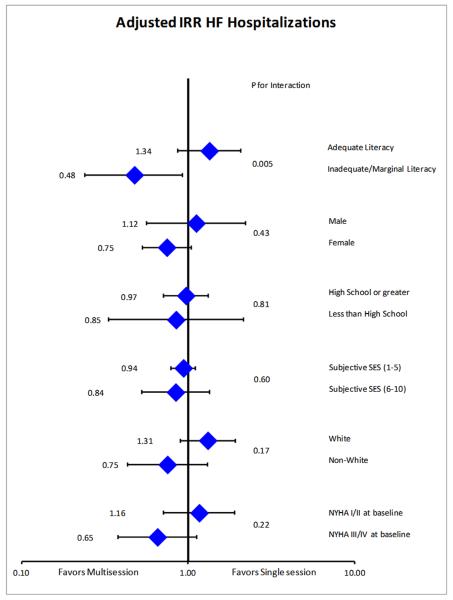
Subgroup Analyses
We evaluated the relative effects of multisession versus single session for several subgroups other than literacy. Among the subgroups tested (sex, education, SES, race, and NYHA class), none of them modified the effect of multisession as much as literacy (Figure 3).
Figure 3.
Subgroup analysis for differences in heart failure related hospitalization for the multisession group compared to the single session group. (Adjusted for site, HFQOL, ACE/ARB use, and subjective SES.)
Adverse Events
Episodes of hypokalemia, renal insufficiency, volume depletion, and syncope were similar between the groups and no events were attributable to the single session or the multisession intervention.
Discussion
In this comparative effectiveness research study, ambulatory patients with HF who received the multisession intervention did not have a lower incidence of all-cause hospitalizations or death compared with those who received a single session. Intensive, longitudinal teaching did not seem to offer additional benefit over a single intensive educational session for the population as a whole. However, the multisession intervention may have been more effective than a single session for those with low literacy, particularly for HF-related hospitalizations. HFQOL improved more for multisession patients at 6 months, but not at 12 months, and this effect did not differ according to literacy. Our study was designed with limited exclusion criteria and enrolled an economically, ethnically, racially, and geographically diverse group of patients from outpatient settings at 4 university health centers. As such, our results represent a broad segment of HF patients.
We hypothesized that patients with lower literacy would derive more benefit from the more intensive multisession intervention. The complexity and scope of information required for optimal HF self-care is probably not adequately covered in one education session. People with low literacy skills may have difficulty with review and self-study of educational materials and consequently have more difficulty reaching mastery after one session than people with higher literacy skills. The multisession strategy should have “leveled the playing field” enabling patients with low literacy to receive adequate instruction and achieve outcomes similar to patients with higher literacy.
We also hypothesized that patients with higher literacy would derive benefit from the more intensive training. In this study, however, the single session intervention was as good as the multisession, and perhaps even better, for patients with higher literacy with respect to hospitalizations. We are unsure why the multisession program may lead to more hospitalizations. Perhaps the effect of the multisession is to increase self-care and activation and to increase attention to symptoms. Patients with higher literacy may need less assistance with improving self-care and activation. But, the additional phone calls may have led to closer attention to symptoms and subsequently more admissions, similar to effects seen in other studies.29
One of our secondary outcomes, HFQOL, followed a different pattern. In the case of HFQOL, the multisession group had greater improvement, but the difference between the multisession and single session groups waned over time. In contrast to the hospitalization findings, the effects of multisession on HFQOL were equal or greater among participants with higher literacy compared to those with lower literacy. This difference in findings suggests that different elements of self-care may affect hospitalization and HFQOL differently. For example, earlier activation of the care system may help to avoid hospitalizations, but increasing exercise may play a larger role in improving HFQOL. 30 Such distinctions in HF self-care effects may be useful in the design of self-care training programs.
Other trials of self-care training have been mixed with regard to effect modification by literacy or similar variables. We previously performed a single site trial of 126 patients that compared a similarly intensive multisession intervention vs. usual care.3 That trial demonstrated improvements for both low and higher literacy patients who received the more intensive intervention, with somewhat stronger effects among patients with low literacy, but the study was not powered to detect effect modification.3 A recent comparative effectiveness research study evaluated HF self-management training versus general HF education and demonstrated effect modification by income.6 Conversely, studies that incorporate more aspects of patient navigation and disease management, and compare with usual care have not shown effect modification.4, 14, 15 For example, a study of nurse management versus usual care did not show effect modification by literacy.14, 15
Our study had some limitations. Our multisession intervention, like self-care training and/or disease management, combined several elements based on the theory that their individual effects would be difficult to detect if tested independently. We cannot attribute effects to any single element of the intervention. Additionally, we did not collect information on the dose of medications or the number of outpatient visits in each group. It is possible that some effect of the multisession intervention was to increase care-seeking behavior. Another limitation was that the randomization did not evenly distribute HFQOL between the groups. Because HFQOL is such a powerful predictor of hospitalization, we felt that this uneven distribution could influence our results and inferences. The point estimates of effect remained similar regardless of adjustment. Lastly, our study was conducted at 4 academic centers, which may limit generalizability to unaffiliated health care systems.
Conclusions
A more intensive multisession intervention for patients with HF did not decrease the incidence of hospitalizations compared with single session only. However, effect modification by literacy suggests that more intensive interventions may hold benefit for specific subgroups. The design of self-care interventions should take into account the needs of the patient in regard to prior knowledge and skills, the design of the educational materials, and the delivery and reinforcement of information provided.
Clinical Impact.
This manuscript describes the comparative effectiveness of two types of a heart failure self-care training program: single session training versus multisession training. In a diverse population across 4 clinical sites, there was no difference in rate of hospitalization or death between the interventions. However, patient literacy was an important factor in the effect of the intervention. Patients with low literacy appeared to benefit from the multisession intervention compared with the single session intervention, but patients with higher literacy did not benefit. Although self-care training for heart failure is an important component of guideline-based care for all patients, it may be important to focus our most intensive resources via ongoing training for patients with low literacy skills.
Acknowledgements
We are indebted to several research team members who helped to ensure the rigorous and timely completion of this study: Sara Glass, RD, Adriana Hernandez, Aurora Hernandez, James Joyner, Zenelia Roman, and Adam Williams.
Funding Sources: We are grateful to the National Heart Lung and Blood Institute (NHLBI) for supporting this work (R01HL081257). NHLBI had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Conflict of Interest Disclosures: None
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission a systematic review of randomized trials. J Am Coll Cardiol. 2004;44:810–819. doi: 10.1016/j.jacc.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 2.Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D, Stewart S, Cleland JG. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD007228.pub2. CD007228. [DOI] [PubMed] [Google Scholar]
- 3.Dewalt DA, Malone RM, Bryant ME, Kosnar MC, Corr KE, Rothman RL, Sueta CA, Pignone MP. A heart failure self-management program for patients of all literacy levels: A randomized, controlled trial [isrctn11535170] BMC Health Serv Res. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Randomised trial of telephone intervention in chronic heart failure: Dial trial. BMJ. 2005;331:425. doi: 10.1136/bmj.38516.398067.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan DC, Heidenreich PA, Weinstein MC, Fonarow GC. Heart failure disease management programs: A cost-effectiveness analysis. Am Heart J. 2008;155:332–338. doi: 10.1016/j.ahj.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Powell LH, Calvin JE, Richardson D, Janssen I, Mendes de Leon CF, Flynn KJ, Grady KL, Rucker-Whitaker CS, Eaton C, Avery E. Self-management counseling in patients with heart failure. JAMA. 2010;304:1331–1338. doi: 10.1001/jama.2010.1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167:1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 8.Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, Newman AB, Rosano C, Rooks R, Rubin SM, Ayonayon HN, Schillinger D. Limited literacy is associated with mortality in the elderly: The health, aging, and body composition study. J Gen Intern Med. 2006;21:806–812. doi: 10.1111/j.1525-1497.2006.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, Matlock DD, Magid DJ, Masoudi FA. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305:1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13:791–798. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, Ren J, Peel J. Functional health literacy and the risk of hospital admission among medicare managed care enrollees. Am J Public Health. 2002;92:1278–1283. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther. 2009;85:651–658. doi: 10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: A systematic review of the literature. J Gen Intern Med. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sisk JE, Hebert PL, Horowitz CR, McLaughlin MA, Wang JJ, Chassin MR. Effects of nurse management on the quality of heart failure care in minority communities: A randomized trial. Ann Intern Med. 2006;145:273–283. doi: 10.7326/0003-4819-145-4-200608150-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hebert PL, Sisk JE. Health literacy and heart failure care in minority communities. Ann Intern Med. 2007;146:312. doi: 10.7326/0003-4819-146-4-200702200-00014. [DOI] [PubMed] [Google Scholar]
- 16.DeWalt DA, Broucksou KA, Hawk V, Baker DW, Schillinger D, Ruo B, Bibbins-Domingo K, Holmes M, Weinberger M, Macabasco-O’Connell A, Pignone M. Comparison of a one-time educational intervention to a teach-to-goal educational intervention for self-management of heart failure: Design of a randomized controlled trial. BMC Health Serv Res. 2009;9:99. doi: 10.1186/1472-6963-9-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: A cognitive ’vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15:1021–1027. doi: 10.1002/1099-1166(200011)15:11<1021::aid-gps234>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 18.DeWalt DA, Pignone M, Malone R, Rawls C, Kosnar MC, George G, Bryant B, Rothman RL, Angel B. Development and pilot testing of a disease management program for low literacy patients with heart failure. Patient Educ Couns. 2004;55:78–86. doi: 10.1016/j.pec.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Baker DW, DeWalt DA, Schillinger D, Hawk V, Ruo B, Bibbins-Domingo K, Weinberger M, Macabasco-O’Connell A, Pignone M. “Teach to goal”: Theory and design principles of an intervention to improve heart failure self-management skills of patients with low health literacy. J Health Communication. 2011;16:73–88. doi: 10.1080/10810730.2011.604379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychol. 2000;19:586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- 21.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 22.Baker DW, Brown J, Chan KS, Dracup KA, Keeler EB. A telephone survey to measure communication, education, self-management, and health status for patients with heart failure: The improving chronic illness care evaluation (icice) J Card Fail. 2005;11:36–42. doi: 10.1016/j.cardfail.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Macabasco-O’Connell A, Dewalt DA, Broucksou KA, Hawk V, Baker DW, Schillinger D, Ruo B, Bibbins-Domingo K, Holmes GM, Erman B, Weinberger M, Pignone M. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med. 2011;26:979–986. doi: 10.1007/s11606-011-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. [Accessed 2011];Archives. http://www.archives.com/
- 25.Lindsey JK. Modeling frequency and count data. Oxford University Press; Oxford: 1995. [Google Scholar]
- 26.Anand IS, Carson P, Galle E, Song R, Boehmer J, Ghali JK, Jaski B, Lindenfeld J, O’Connor C, Steinberg JS, Leigh J, Yong P, Kosorok MR, Feldman AM, DeMets D, Bristow MR. Cardiac resynchronization therapy reduces the risk of hospitalizations in patients with advanced heart failure: Results from the comparison of medical therapy, pacing and defibrillation in heart failure (companion) trial. Circulation. 2009;119:969–977. doi: 10.1161/CIRCULATIONAHA.108.793273. [DOI] [PubMed] [Google Scholar]
- 27.Pérez A, Dennis RJ, Gil JFA, Rondón MA, López A. Use of the mean, hot deck and multiple imputation techniques to predict outcome in intensive care unit patients in colombia. Stat Med. 2002;21:3885–3896. doi: 10.1002/sim.1391. [DOI] [PubMed] [Google Scholar]
- 28.Baker DW, DeWalt DA, Schillinger D, Hawk V, Ruo B, Bibbins-Domingo K, Weinberger M, Macabasco-O’Connell A, Grady K, Holmes GM, Erman B, Broucksou K, Pignone M. The effect of progressive, reinforcing telephone education and counseling vs. Brief educational intervention on knowledge, self-care behaviors and heart failure symptoms. J Card Fail. 2011;17:789–796. doi: 10.1016/j.cardfail.2011.06.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans affairs cooperative study group on primary care and hospital readmission. N Engl J Med. 1996;334:1441–1447. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 30.Flynn KE, Pina IL, Whellan DJ, Lin L, Blumenthal JA, Ellis SJ, Fine LJ, Howlett JG, Keteyian SJ, Kitzman DW, Kraus WE, Miller NH, Schulman KA, Spertus JA, O’Connor CM, Weinfurt KP. Effects of exercise training on health status in patients with chronic heart failure: Hf-action randomized controlled trial. JAMA. 2009;301:1451–1459. doi: 10.1001/jama.2009.457. [DOI] [PMC free article] [PubMed] [Google Scholar]