Abstract
Physicians in community-based practice rarely have the time, nor the inclination, to participate in formal, controlled clinical research. While few would question the importance of statistically valid clinical trials focused on establishing the safety and efficacy of new pharmaceuticals and medical devices, most busy practitioners recognize that formal clinical research can't be approached casually. Beyond the operational infrastructure typically required to execute medical research, the imposition of fundamentally experimental research is such that it is not easily accommodated in day-to-day medical practice. Indeed, the often artificial nature of controlled clinical research is, in many ways, incompatible with actual practice conditions. However, the characteristics and, more importantly, the outcomes of “real world” medical practice are becoming of increasing scientific and practical importance. Underscored by recent post-approval drug recalls, the “real world” practice environment can be an invaluable source of information on the actual effectiveness of treatment regimens, drugs, and devices. Inasmuch as clinical trials tend to exclude noncompliant patients and those with comorbid conditions, a new paradigm is appropriate for capturing the outcomes of actual practice. While not without statistical and analytical limitation, the brand of “naturalistic” research undertaken in observational patient registries is becoming rapidly accepted by both the scientific and practitioner communities.
THE REALITY (?) OF CLINICAL RESEARCH
To definitively establish the efficacy of a new drug, a controlled experiment must be performed. In order to eliminate the “noise” of confounding variables, the framework of a clinical trial must feature rigid inclusion/exclusion criteria, statistical validity, a formal protocol, and precise endpoints. As a result, the scientific community can generally place great reliance on the findings from studies in which all extraneous factors have been ruled out, leaving only the magnitude of a difference between arm A and arm B to definitely establish a drug's relative efficacy.
Few can challenge the merits of well-executed clinical research for establishing the safety and efficacy of drugs, devices, diagnostic tools, or treatment regimens. The reality of clinical research, however, is that in the very controls necessary to support a valid experiment lie aspects that are often artificial relative to the conditions found in actual medical practice. While a new statin may prove to reliably control hypercholesterolemia in a clinical trial, in the “real world” patients are often noncompliant with therapy and present with comorbid conditions that have to be addressed coincident with a primary disease. Clinical research may provide all the proof necessary to allow the FDA to approve a new H2-antagonist; however, rarely in actual practice are the same endoscopic assessments undertaken to uncover asymptomatic gastric lesions. Given the differences between the environment underlying clinical research and the conditions reflective of actual community-based medical practice, recent drug recalls due to safety concerns come as less of a surprise. What is surprising, perhaps, is that there is no formal regulatory structure mandating the compilation of data more reflective of the conditions in which a drug is actually utilized!
Community-based practitioners even remotely interested in participating in traditional controlled clinical research must, therefore, recognize that many trials impose conditions that may not be compatible with day-to-day medical practice. Even notwithstanding these potentially unnatural procedures, practitioners often overlook the operational and infrastructural requirements basic to clinical research: that is, patients must be enrolled and data must be captured. Most academic research centers have come to grips with the resource requirements for clinical trials, typically employing study nurses to coordinate enrollment and often utilizing medical students to complete case report forms. Few community-based practices have the luxury of additional resources to purchase new magazines for the waiting room, let alone complete detailed case reports.
There is certainly a place for controlled clinical research, but that place may not be in the community setting. The reality of clinical research also underscores the gap between the information emanating from controlled trials and the patient outcomes attainable in the “real world.” This is not in the least to suggest that findings from clinical trials are invalid, but rather to emphasize the relative paucity of data on outcomes of actual practice.
THE VALUE OF OBSERVATIONAL RESEARCH
Information derived through relatively uncontrolled research has considerable value, provided the context within which data are compiled is valid and data collection processes are designed to minimize inaccuracies. The Framingham Heart Study, in operation since 1948, is one notable example of an observational research initiative that, through its extensiveness and comprehensiveness, provides the medical community an outstanding source of information on trends associated with treatment for cardiovascular and other conditions (1). The National Registry of Myocardial Infarction, an industry-sponsored initiative, has, since 1990, been the foundation underlying many important treatment guidelines for the management of heart attacks (2). This latter program underscores the growing interest in observational programs sponsored by pharmaceutical and device manufacturers, and increasingly mandated by the FDA, as a condition of market approval. Indeed, research reflecting actual practice conditions is becoming of increasing importance to product manufacturers, both as a vehicle for understanding “real world” drug or device safety and effectiveness and, candidly, as a mechanism for achieving widespread practitioner exposure to a new product or indication.
In years past, manufacturers seeking to accelerate market exposure for their medical products would often sponsor so-called clinical trials that were in fact thinly veiled sampling or “seeding” programs. Rarely were these initiatives designed with any true analytical goals. In return for their participation in the trial, physicians were essentially compensated simply for utilizing the sponsor's product, and the sponsor was able to “jump start” its sales efforts. Medicare Fraud and Abuse legislation, however, effectively and appropriately curtailed these programs.
Today, in part a reflection of more responsible promotional activities, but mostly in recognition of the need for post-approval data on utilization and outcomes, pharmaceutical and medical device companies have begun to create and implement observational trials, better known as “patient registries.” While these programs still benefit their sponsors in showcasing their products to practitioners, they have come a long way in their goals and methods. Indeed, findings from many patient registries today are published in first-tier medical journals and presented at medical meetings.
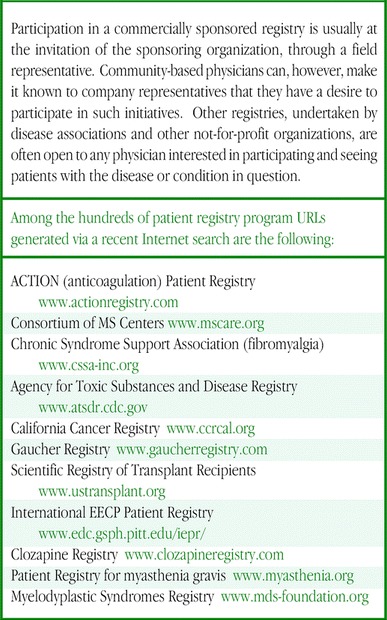
While there are numerous patient registries being run by not-for-profit associations (Table), today's commercially-sponsored patient registries are commonly run in an arm's-length fashion under the auspices of a Scientific Advisory Panel, in many cases comprised of leading clinicians in a particular field. Findings are derived through formal analysis plans often requiring sophisticated statistical methods (in many cases, to make sense of typically heterogeneous patient populations). Serious efforts are undertaken to compile meaningful data through case report forms. Physicians are compensated, but typically quite modestly, and only as reimbursement for time spent in completing forms. In some situations, providers participate primarily to gain access to detailed reports that may be useful in clinical quality improvement initiatives and, as such, participation may not be compensated at all.
If these programs are carefully and thoughtfully designed, the information captured from them reflects actual medical practice and can reveal issues that may not have been seen in preapproval clinical research. A drug's actual effectiveness — as contrasted with its efficacy — is only truly reflected in the “real world,” in which patients present with comorbidities that may have constituted an exclusion from clinical trials, or in which patients aren't as compliant with treatment as they are required to be in clinical research. These “real world” conditions may also reveal safety issues that, due to the to need eliminate confounding variables in preapproval studies, could never be expected to be uncovered. Physicians cautiously exploring the use of a newly approved product may be motivated to participate in a patient registry if only to gain early access to potentially impactful information that reflects general experience well beyond their practice. At present, this may be the only mechanism available for uncovering such information as, perhaps surprisingly, there is no specific legislated requirement to study patients in a postapproval setting (unless it was a condition of market approval or a requirement as a result of safety concerns compiled through general market experience).
The challenge — and it is no small one — is to capture data reflective of actual practice conditions without altering the very conditions being examined and the outcomes being sought! Data collection in a patient registry must be benign, not only to preserve the naturalistic environment, but also since there are generally few incremental staff resources available for compiling data. Indeed, a patient registry must fit elegantly into daily life in the busy medical practice setting. At the same time, it must be sufficiently rigorous to generate meaningful conclusions. Achieving this delicate balance is one of the greatest challenges associated with the design and implementation of observational research.
PATIENT REGISTRIES - PHYSICIAN BENEFITS
At some point in the future, the world of medical practice will be entirely electronic in terms of data transactions. Extracting “real world” data via electronic medical records holds considerable promise for the optimal level of efficiency and unobtrusiveness sought in observational research. Through a behind-the-scenes transfer of encrypted data to a secure central data repository, researchers will gain rapid and accurate access to aggregate data compiled in an elegant fashion. Those days are, however, still fairly far off for the majority of community-based physicians.
In the interim, the design and implementation of a patient registry must take into account the nature of daily medical practice while keeping in sight of its scientific goals. The program cannot be operationally obtrusive, yet it must capture sufficient data to support analyses. Until the world of medical practice is entirely electronic, incremental effort will generally be required to support these programs. Accordingly, the benefits of physician participation must at least match, if not exceed, the costs. And these benefits and costs are not always simply monetary in nature.
Classically, the benefits of participating in a patient registry from the perspective of a community-based physician include the following opportunities:
To add to the body of knowledge about a particular disease and its management
To contrast practice-specific findings with those from a larger, more representative database
To better understand patient perspectives relating to therapeutic approaches and outcomes
To gain access to “best practices” data
To undertake exploratory research utilizing the registry database, and to publish/present the findings
To connect with a community of like-minded physicians
To transition into clinical research by participating in a “lower stakes” initiative
Added to this list can also be a financial motivation. In all candor, however, honoraria from observational research is generally quite modest, and must really be considered reimbursement for time spent; which, if the registry is well designed, should be nominal. Participation in most registries sponsored by a noncommercial entity is almost always voluntary and uncompensated.
Although, increasingly, patient registries are being undertaken via the Internet, paper-based programs are still prevalent. But while Internet-based registries may present data entry efficiencies, like paper-based programs, data still must be collected to reflect patient demographics, the relevant disease history, treatments, outcomes, and, in many cases, patient quality of life. There is no avoiding the requirement to record the facts of the case, nor the reality that the accuracy of the registry is entirely in the hands of its physician participants: unlike clinical trials, registries rarely feature the added rigor (and expense) of site monitoring or source data validation.
Patient registries do, however, have certain elements that are based on the Good Clinical Practices intrinsic to traditional controlled clinical trials. In most cases, the objectives and procedures underlying a patient registry will be reviewed and approved by either a centralized institutional review board (IRB) or by the IRBs of each participating site. Since the registry is nonexperimental in nature, the IRB will generally focus its attention on the merits of the program and on protecting the privacy of patients involved. As such, patient consent is often a requirement for these initiatives as well. Similarly, consent generally serves to establish the limits of uses of patient data, and informs the patient that only unidentified, aggregate data will be used to support analyses.
Patient registries require, of course, that patients be enrolled. “Enrollment,” however, connotes a somewhat imprecise characterization of the patient's experience. From the patient's point of view, participation in a registry might feature only the knowledge that his or her deidentified case information is going to be used analytically. Indeed, participation in an observational program differs dramatically from enrollment into a double-blind, placebo-controlled clinical trial. In essence, after consenting to participate in an observational research program, the patient can expect to be managed as under normal practice conditions. While some programs may require the patient to return to the office or to complete a quality of life questionnaire on a fixed time interval, these activities generally reflect the extent of patient effort required. And in many cases, patients have appreciated the opportunity to express their opinions, and to know that their participation has, in some small way, contributed to knowledge about managing their disease.
While there is generally no “protocol” guiding the conduct of an experiment, “procedures” typically exist to guide the physician in enrolling patients into the registry, and in capturing and submitting patient data. Thus, the day-to-day experience for physicians (and their staffs) participating in a patient registry involves capturing and submitting patient data, responding to relatively benign data queries, and accessing periodic reports profiling the physician's experience against the aggregate. In short, minimal effort is generally required to contribute patient data to the central database. While the immediate feedback through comparative reports is usually seen as “payback,” perhaps the greatest benefit to the participating physician is the knowledge that his or her contribution of data is supporting a much larger aggregate effort, a level at which potentially valuable insights are being obtained.
LIMITATIONS
Important contrasts exist between formal clinical trials and patient registries that are intrinsic to their unique goals. Importantly, the clinical trial is statistically powered based upon a hypothesized difference between treatment arms. As such, randomization is required to ensure that the treatment arms are comparable, such that actual differences are due as much as possible to the treatment being studied. A patient registry may be built upon issues to be explored, but inasmuch as the program is not based on an a priori hypothesis, rarely can findings be characterized as definitive. An important attribute of most patient registries is, however, their size and variability, which is critical to the attainment of relevant findings. Many patient registries enroll thousands of patients, often far more than in a formal clinical trial. While “apples to apples” comparisons cannot be guaranteed in programs of this size, matched cohorts can be constructed and important trends examined. A registry more commonly aims to be hypothesis generating rather than hypothesis testing.
The individual physician's participation in a registry can rarely be seen as statistically valid — similar to the individual investigator's experience as one of many researchers participating in a trial. However, the composite of the physician's enrolled patients can be insightful, particularly in contrast to the overall aggregate from the registry database. Thus, the physician's experience in a registry lies somewhere between the anecdotal “n of 1” sample and the power of the aggregate database.
CONCLUSION
Formal clinical research is of vital importance to the advancement of medicine, and participation in formal clinical research can be quite rewarding to the individual practitioner. The imposition and infrastructure necessary to support clinical research, however, is such that it may be more compatible with academic medical practice. Community-based practitioners can, however, whet their appetite for research by participating in observational trials. These research initiatives, while not as far-reaching and definitive as controlled clinical trials, can reveal important trends in the “real world” practice of medicine. As such, they represent a valuable complement to trials aimed at drug approval. Indeed, patient registries can provide a structured glimpse into the uncontrolled nature of postapproval medical practice. Participation in these benign, naturalistic programs may be much more satisfying and considerably less obtrusive to the community-based physician.
Jeffrey P. Trotter, MM, is President of Ovation Research Group, an independent health economics and outcomes research group based in suburban Chicago. Mr. Trotter and his colleagues provide consulting and contract research services to medical device and pharmaceutical companies seeking to objectively examine the clinical and economic value of their products. Ovation currently supports the operations for several large-scale patient registries in a broad spectrum of diseases and conditions.
Table. Patient registry resources for physicians
REFERENCES
- National Heart, Lung and Blood Institute. The Framingham Heart Study. ( www.framingham.com/heart) [Google Scholar]
- The National Registry of Myocardial Infarction (NRMI) ( www.nrmi.org) [Google Scholar]


