Abstract
Despite great potential benefits, there are concerns about the possible harm from medical imaging including the risk of radiation-related cancer. There are particular concerns about computed tomography (CT) scans in children because both radiation dose and sensitivity to radiation for children are typically higher than for adults undergoing equivalent procedures. As direct empirical data on the cancer risks from CT scans are lacking, the authors are conducting a retrospective cohort study of over 240 000 children in the UK who underwent CT scans. The main objective of the study is to quantify the magnitude of the cancer risk in relation to the radiation dose from CT scans. In this paper, the methods used to estimate typical organ-specific doses delivered by CT scans to children are described. An organ dose database from Monte Carlo radiation transport-based computer simulations using a series of computational human phantoms from newborn to adults for both male and female was established. Organ doses vary with patient size and sex, examination types and CT technical settings. Therefore, information on patient age, sex and examination type from electronic radiology information systems and technical settings obtained from two national surveys in the UK were used to estimate radiation dose. Absorbed doses to the brain, thyroid, breast and red bone marrow were calculated for reference male and female individuals with the ages of newborns, 1, 5, 10, 15 and 20 y for a total of 17 different scan types in the pre- and post-2001 time periods. In general, estimated organ doses were slightly higher for females than males which might be attributed to the smaller body size of the females. The younger children received higher doses in pre-2001 period when adult CT settings were typically used for children. Paediatric-specific adjustments were assumed to be used more frequently after 2001, since then radiation doses to children have often been smaller than those to adults. The database here is the first detailed organ-specific paediatric CT scan database for the UK. As well as forming the basis for the UK study, the results and description of the methods will also serve as a key resource for paediatric CT scan studies currently underway in other countries.
INTRODUCTION
Since its introduction in the early 1970s the number of computed tomography (CT) scans performed annually has increased rapidly in developed countries, with the greatest increases occurring since the widespread introduction of multi-detector CT in the late 1990s(1). In 2008 there were 3.4 million CT scans performed in England, an increase of 140 % since 1997(2). The increase in the USA was 280 % over the same period(3) and this pattern is repeated across other developed countries(4). For children, there is less published evidence of an increase in the use of CT scans. However, in a study of usage in young people in the north of England between 1993 and 2002, the number of scans and scanned patients rose significantly over the study period(5).
Despite the great potential benefits, there are concerns about the possible harms from the rise in medical imaging including the risk of radiation-related cancer. Studies of the atomic bomb survivors, as well as studies of medically exposed populations have demonstrated that radiation is carcinogenic to most human tissues and organs(6). Based on these data a recent modelling study suggested that about 29 000 (95 % uncertainty interval: 15 000–45 000) future cancers could be related to the number of CT scans performed in 2007 in the USA including about 4500 cancers from exposures in childhood(7). There are particular concerns about CT scans in children for two reasons. Firstly, the radiation risk per unit dose for many cancers is higher for children than for adults and they have longer remaining life expectancy to demonstrate radiation-related effects(6). Secondly, the radiation doses that children receive from these exposures can be higher than those that adults receive because of smaller body size and attenuation, especially if the technical parameters are not adjusted for the patient size(8).
As direct empirical data on the cancer risks from CT scans are lacking, the authors are conducting a retrospective cohort study in the UK to determine whether the risk of developing cancer is increased in children who underwent CT scans(5). So far, a cohort of 246 000 children and young adults (all under 22 y of age) who received over 400 000 CT scans during 1985–2002 from the electronic radiology information systems (RIS) held by radiology departments in Great Britain has been assembled. Cancer incidence is being ascertained through the National Health Service Central Register and regional cancer registries. Analyses will be focused on leukaemia and, depending on sample size, other known radiogenic cancers that occur at relatively young ages (brain, thyroid and breast). A key objective of the study is to quantify the magnitude of the cancer risk in relation to the radiation dose from CT scans. In order to achieve this goal, individual-level organ dose estimates for each exposed patient are required. In this paper, the methods used to estimate typical organ-specific doses delivered by CT scans to children during the study period 1985–2002 are described.
MATERIALS AND METHODS
The objective of radiation dosimetry in the cohort study was to estimate radiation doses to specific organs on an age- and sex-dependent basis for any given CT examination by calendar year. Specific organs of interest for the radiation dosimetry included the red bone marrow (RBM), brain, thyroid and breast. Firstly, an organ dose database using a series of computational human phantoms (newborns, 1, 5, 10, 15 y and adults for both males and females) was established. Secondly, available data for the radiation dosimetry, including electronic data on CT scans for the cohort members and CT scan practice in the UK from surveys conducted during the study time period were collected. Finally, the established organ dose database collected cohort CT scan information and the CT scan practice in the UK surveys were combined to estimate typical organ-specific doses to the cohort by patient age, sex, examination type and calendar year.
Calculation of organ dose database
Two comprehensive organ dose databases for CT scans in adults are available that were developed by two independent organisations using Monte Carlo simulations: National Radiation Protection Board (NRPB) in the UK (now part of the Health Protection Agency)(9, 10) and the National Research Centre for Environment and Health (GSF) in Germany(11, 12). However, the NRPB data are limited only to adults and the GSF data are limited to only two paediatric ages: 2 months and 7 y, neither of which were standardised to the reference dimensions of body and organs suggested by the International Commission on Radiological Protection (ICRP)(13, 14).
More recently, a new class of computational human phantoms, called hybrid phantoms, was introduced by researchers at the University of Florida and the National Cancer Institute(15). The hybrid phantoms combine the flexibility and the realism which are the major advantages of the previous stylised(16) and voxel(17) phantoms, respectively. The hybrid phantoms are based on reference body dimensions and anatomy of paediatric and adult individuals in compliance with the recommended organ and body dimensions from the ICRP(14). The hybrid phantom series includes newborn, 1, 5, 10, 15 y and adult male and female reference individuals which provide higher age resolution than those adopted in the GSF database. In the current study, a new organ dose database for paediatric and adult males and females was established using the hybrid phantom series coupled with Monte Carlo simulation of the X-ray beam in a CT scanner(18, 19).
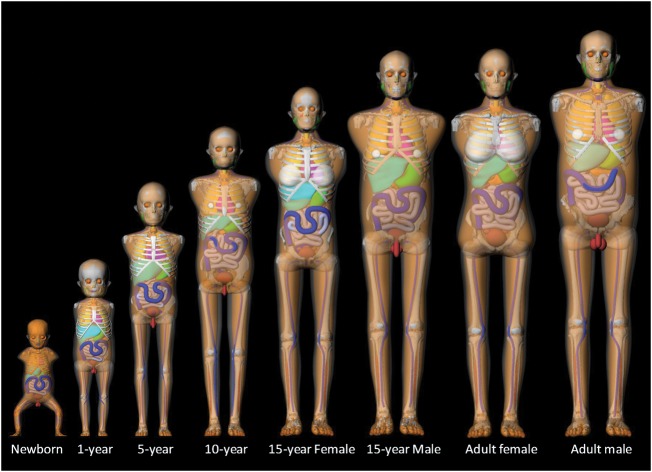
To simulate a CT scanner within the Monte Carlo calculations, detailed technical specifications of a SOMATOM Sensation 16-helical CT scanner were obtained from the manufacturer and simulated within a general purpose Monte Carlo radiation transport code, MCNPX2.6(20). MCNPX2.6 is designed to simulate the interaction of many types of radiation particle within a variety of materials over broad ranges of energies. The simulated CT scanner model was validated by comparing computed tomography dose index (CTDI) data measured from head and body CTDI phantoms with the values simulated using the Monte Carlo-based CT scanner model. The results agreed within 8 % which was similar to the results of comparisons from other investigators(21–23). A series of reference paediatric and adult hybrid phantoms were employed to establish the organ dose database: newborns, 1, 5, 10, 15 y and adult males and females(15). The phantoms are based on real-patient CT images of the head and torso at the given ages with body dimensions and organ masses matched to international reference data, including the reference organ masses in ICRP Publication 89(14), the reference gastro-intestinal dimensions in ICRP Publication 100(24) and the standard elemental composition of organs and tissues in ICRP Publication 89 and the International Commission on Radiation Units and Measurements Report 46(25). The arms were removed from each phantom to more realistically simulate typical arm-raised position in both head and torso CT scans, but right and left humeral heads were included to more accurately calculate their contribution to the active marrow dose. Figure 1 shows the three-dimensional frontal views of the hybrid phantom series ranging from newborn to adult male and female.
Figure 1.
Three-dimensional frontal views of the hybrid phantom series ranging from newborn to adult male and female used to generate an organ dose database.
Organ doses from helical scans with a given scan range were approximated by the summation of doses from multiple axial slices included in the scan range of interest, which is the approach also used in CT-expo(26), which is the software package based on the GSF organ dose database. This approach provides a great flexibility to the CT dosimetry calculations in which one can readily estimate organ doses for whatever CT scan coverage by using the pre-calculated organ dose database. Different sets of organ dose calculations were performed for a single axial scan which started from the top of head down to the bottom of the phantom with an interval of 1 cm. A total of 12 phantoms were generated and implemented into Monte Carlo calculations.
Accurate estimates of RBM dose are essential for the assessment of leukaemia risks. Absorbed doses to RBM in the organ dose database were calculated using a fluence-to-dose response function developed at the University of Florida(27) which is an updated version of the function developed at the Oak Ridge National Laboratory (ORNL)(16). The fluence-to-dose response functions were derived using fractional skeletal masses and associated electron absorbed fractions as reported for the University of Florida adult male phantom, which were based upon micro-CT images of trabecular spongiosa taken from a 40-year old male cadaver(28). The fluence-to-dose response functions relate the photon fluence in a skeletal source region and the absorbed dose in a skeleton target region. Photon fluence crossing the spongiosa region of each bone site was scored for 25 energy bins ranging from 0.01 to 10 MeV within the Monte Carlo simulation. RBM doses in each bone site were then calculated by multiplying the photon fluence by the fluence-to-dose response function. Total absorbed doses for RBM were calculated by weighting site-specific doses by the RBM distribution in reference individuals(18).
Available data for cohort dosimetry
The study cohort was identified from 72 NHS trusts in England and Wales (corresponding to 97 hospitals) and 6 NHS boards in Scotland (corresponding to 13 hospitals). Electronic data from RIS were obtained for all patients who had one or more CT scans before 22 y of age during 1985–2002. The retrieved data included patient identifiers, date of birth, sex and date and type of CT examination. Typical parameter settings were taken from two nationwide surveys of CT practice in the UK during the similar time period of this study(29–31). In 1989, a national survey was carried out by the NRPB in collaboration with the Institute of Physical Sciences in Medicine to estimate the frequency of use and estimate typical patient doses(30, 31). The information on technical factors (e.g. kVp, mA s, pitch, etc.) typically used for 18 types of CT examinations was collected in the survey for 83 % of NHS scanners. The survey did not differentiate between settings for adult and paediatric patients, most likely because they were assumed to be the same or very similar at that time. In 2003, a second national survey was performed by the NRPB in collaboration with the CT User Group and the CT evaluation facility, ImPACT, of the Medicines and Healthcare products Regulatory Agency to assess potential changes in CT practice resulting from the introduction of multi-slice CT. The survey collected CT practice data for paediatric patients with three age groups (0–1, 5 and 10 y) as well as for adult patients. Selected procedures included six common CT examinations (routine head, abdomen, abdomen/pelvis, chest/abdomen/pelvis, chest and high-resolution chest) for adults and two examinations (head and chest) for children. Technical setting data, including scan mode, tube voltage, tube current and rotation time and pitch were collected by questionnaire. For each examination, the values of CTDIw and CTDIvol per rotation, which represent X-ray output from a CT scanner, were calculated using the reported technical setting data. The two nationwide surveys are summarised in Table 1.
Table 1.
Summary of the 1989 and 2003 nationwide surveys of CT practice in the UK.
| Year | Patient age | Examination types | Collected technical settings |
|---|---|---|---|
| 1989 | Adult | 18 examinationsa | Tube potential (kVp) |
| Exposure setting (mA s) | |||
| Nominal slice width (mm) | |||
| Couch increment (mm) | |||
| 2003 | Adult | 6 examinationsb | Tube potential (kVp) |
| Pitch | |||
| Slice width (mm) | |||
| Childrenc | 2 examinationsd | Scan length (mm) | |
| CTDIw and CTDIvol |
aHead, posterior fossa, pituitary, internal auditory meatus, orbits, facial bone, routine chest, mediastinum, routine abdomen, liver, pancreas, kidney, adrenals, routine pelvis, cervical spine, thoracic spine and lumbar spine.
bHead, chest, high-resolution CT, abdomen, abdomen and pelvis and whole body.
c0–1, 5 and 10 y old.
dHead and chest.
Estimation of organ-specific doses for cohort
The numerous CT scan types in the cohort database were grouped into 17 different scan regions taking into account the specific organs of interest in this study (Table 2). For example, the scan region defined here as ‘brain CT’ in Table 2 included any type of CT in which the brain has likely been scanned. ‘Partial brain CT’ was a separate category for scans such as the orbit and internal auditory meatus, which would usually result in a lower brain dose. Since only the RBM receives a measurable dose in the extremity scan, CT scans on any region of upper and lower extremities were grouped together. For multiple region scans, the radiation dose was estimated by summing the individual scans defined in Table 2 (e.g. abdomen/pelvis scan dose=abdomen scan dose+pelvis scan dose). For the unknown (no information on CT scan region was given), average doses weighted by frequency of other CT scans were used for the dose estimates.
Table 2.
Grouping categories of CT examinations and description of the anatomical coverage of CT scan regions used for organ dose estimates.
| Scan region | Anatomical coverage |
|---|---|
| Brain | Top of skull through skull base |
| Partial brain | Just above frontal sinus to end of maxillary sinus |
| Facial bone | Just above frontal sinus to below mandible |
| Neck | Mid-orbit to clavicle head |
| Chest | Just above lung apices to below the diaphragm |
| High-resolution CT | Just above lung apices to below the diaphragm |
| Abdomen | Diaphragm to iliac crest |
| Pelvis | Just above iliac crest to below symphysis pubis |
| Hip | Just above sacroiliac joint to approximately centimeter below lesser trochanters |
| Cervical spine | Skull base to the first thoracic vertebra |
| Thoracic spine | Just above the first thoracic vertebra to below the 12th thoracic vertebra |
| Lumbosacral spine | Just above the first lumbar vertebra to below coxxys |
| Shoulder | Just above acromioclavicular joint to just below scapular tip |
| Whole body | Just below mandible to below symphysis pubis |
| Extremity | Entire hand |
| Unknown | No information of CT scan region |
| Multiple regions | Scans that involved more than one scan regions |
For each category of scan region, the typical scan length was estimated from a literature review and expert consultation(29, 30, 32). The anatomical coverage of each scan category is also tabulated in Table 2. For extremity scans, CT scan of the hand was the most common extremity scan (>50 %). As RBM dose from other extremity scans resulted in a similar dose to the hand scan, the dose estimates for the hand scan to all the extremity CT scans in the cohort were applied.
Increased awareness of the radiation doses and risks from paediatric CT scans has resulted in increased use of paediatric specific CT scan settings depending on the age or preferably weight of the patient. Since 2001, a greater use of age-adjusted CT examination has been reported(29, 33–34). Arch and Frush(35) observed that tube potential and current settings had decreased significantly for paediatric CT since 2001 and concluded that it was a reasonable assumption that these changes were due to efforts to increase awareness about the risks of radiation. To assess the temporal trend of CT settings in the UK, data from the pilot study for the cohort were analysed in which detailed technical settings of CT scans were abstracted from CT films for 333 patients from three Newcastle hospitals, collectively known as the Newcastle NHS Foundation Trust. Linear regression models were used to analyse the temporal trend in the current–time product (mA s) for head, chest and abdomen CT scans by calendar year taking into account the age of the patient. There was a significant decreasing trend in mA s with increasing year (p < 0.05, which is defined as the probability of obtaining a test statistic at least as extreme as the one that was actually observed.) for each type of CT scan. Further examination of the data suggested that this was largely due to a step change around 2001 rather than a gradual decline over time. When the data were analysed before and after 2001 there was no clear evidence of a trend in mA s within each time period. This may correspond to the high level of attention that the problem received after the simultaneous publication of three papers on the topic in 2001(8, 36, 37). Therefore, technical settings in the study before 2001 were based on the 1989 NRPB survey and after 2001 they were based on the 2003 survey. It was also assumed that technical settings did not depend on age, or height and weight, before 2001. The national survey in 2003 collected technical settings for children in three age groups (0–1, 5 and 10 y). These age-specific settings for CT scans performed after 2001 were used and the survey data for adults were used for scans performed over the age of 15 y.
The organ dose database generated in this study was normalised by CTDI values and then multiplied by scan-specific CTDI to obtain organ doses for a given scan. Therefore, it was necessary to determine CTDI for each scan region. CTDIvol by patient ages from the 2003 survey data (Table 3) was used. Since CTDIvol values were not available in the 1989 survey, they were calculated using the scan settings (e.g. kVp kVp, mA s and pitch) for each CT scanner model from the survey data and CTDI coefficients published by ImPACT(30, 38). The 2003 CT practice survey in the UK included only head and chest CT examinations. For the other CT scans (e.g. abdomen scans) of paediatric patients, adult CTDIvol values by assuming the same child-to-adult ratio as for the chest scan were adjusted. The CTDIvol values used for organ dose estimates by time period, patient age and scan region are summarised in Table 3.
Table 3.
CTDIvol values used for organ dose estimates for different scan types, ages, sexes and time periods obtained from the NRPB reports.
| Scan region | CTDIvol valuesa |
||||
|---|---|---|---|---|---|
| Pre-2001b |
Post-2001b |
||||
| All ages | 0–1 y | 5 y | 10 y | 15 y to adults | |
| Brain | 51 | 25 | 34 | 44 | 56 |
| Partial brain | 62 | 25 | 34 | 44 | 56 |
| Facial bone | 55 | 25 | 34 | 44 | 56 |
| Neck | 32 | 12 | 12 | 15 | 11 |
| Shoulder | 32 | 12 | 12 | 15 | 11 |
| Chest | 17 | 11 | 11 | 14 | 10 |
| High resolution CT | 4 | 2 | 2 | 3 | 2 |
| Abdomen | 18 | 13 | 13 | 17 | 12 |
| Pelvis | 25 | 12 | 12 | 15 | 11 |
| Hip | 25 | 12 | 12 | 15 | 11 |
| Cervical spine | 32 | 17 | 17 | 22 | 15 |
| Thoracic spine | 33 | 17 | 17 | 22 | 15 |
| Lumbosacral spine | 34 | 17 | 17 | 22 | 15 |
| Whole body | 17 | 11 | 11 | 14 | 10 |
| Extremity | 32 | 17 | 17 | 22 | 15 |
aFor CT scans on the adult head and for all paediatric procedures, CTDIvol values relate to the 16-cm diameter CT dosimetry phantom (head phantom), while those on adult trunk relate to the 32-cm diameter CT phantom (body phantom).
bFor time period of <2001, CTDIvol values were calculated using CT setting parameters (e.g. kVp, mA s and pitch) in the 1989 CT practice survey data. For time period of 2001+, CTDIvol values in 2003 CT practice survey data were used.
RESULTS AND DISCUSSIONS
Organ dose matrix by examination type, age, sex and time periods
Absorbed doses (mGy) for brain, thyroid, breast and RBM were calculated for reference male and female individuals of ages 0, 1, 5, 10, 15 and 20 y for a total of 17 different scan types as tabulated in Table 2. One of the 17 scan types is ‘multiple regions’ which is subcategorised into a total of 53 scan types (e.g. abdomen and extremity). The organ doses were interpolated to obtain the values for in-between ages with the age resolution of 1 y and were calculated for the two time periods pre- and post-2001. Illustrative organ doses for the three most common types of CT scan: brain, chest and abdomen scans are shown in Tables 4–6, respectively, for different ages, sexes and time periods. A comprehensive spreadsheet containing organ doses for 69 scan types (16 individual scan and 53 multiple scans), 22 age groups from newborn to 22 y old, two sexes and two time periods (pre- and post-2001) was generated for use in the epidemiological analysis.
Table 5.
Absorbed doses (mGy) to brain, thyroid, breast and RBM calculated for male and female reference individuals with the ages from 0 to 22 y who underwent chest CT scans for pre- and post-2001 time periods in the UK.
| Chest scan | Pre-2001 |
Post-2001 |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
Male |
Female |
|||||||||||||
| Age (y) | Brain | Thyroid | Breast | RBM | Brain | Thyroid | Breast | RBM | Brain | Thyroid | Breast | RBM | Brain | Thyroid | Breast | RBM |
| 0 | 1.3 | 27.7 | 36.9 | 13.0 | 1.3 | 27.7 | 36.9 | 13.0 | 0.4 | 8.9 | 11.9 | 4.2 | 0.4 | 8.9 | 11.9 | 4.2 |
| 1 | 0.9 | 27.4 | 29.3 | 12.1 | 0.9 | 27.4 | 29.3 | 12.1 | 0.3 | 8.8 | 9.4 | 3.9 | 0.3 | 8.8 | 9.4 | 3.9 |
| 2 | 0.9 | 27.1 | 28.8 | 11.0 | 0.9 | 27.1 | 28.8 | 11.0 | 0.3 | 8.7 | 9.3 | 3.6 | 0.3 | 8.7 | 9.3 | 3.6 |
| 3 | 0.9 | 26.7 | 28.4 | 9.9 | 0.9 | 26.7 | 28.4 | 9.9 | 0.3 | 8.6 | 9.2 | 3.2 | 0.3 | 8.6 | 9.2 | 3.2 |
| 4 | 0.8 | 26.3 | 28.0 | 8.8 | 0.8 | 26.3 | 28.0 | 8.8 | 0.3 | 8.5 | 9.0 | 2.9 | 0.3 | 8.5 | 9.0 | 2.9 |
| 5 | 0.8 | 26.0 | 27.6 | 7.7 | 0.8 | 26.0 | 27.6 | 7.7 | 0.3 | 8.4 | 8.9 | 2.5 | 0.3 | 8.4 | 8.9 | 2.5 |
| 6 | 0.8 | 25.5 | 27.1 | 7.8 | 0.8 | 25.5 | 27.1 | 7.8 | 0.3 | 8.6 | 9.2 | 2.7 | 0.3 | 8.6 | 9.2 | 2.7 |
| 7 | 0.8 | 25.0 | 26.7 | 7.9 | 0.8 | 25.0 | 26.7 | 7.9 | 0.3 | 8.9 | 9.5 | 2.8 | 0.3 | 8.9 | 9.5 | 2.8 |
| 8 | 0.8 | 24.5 | 26.3 | 7.9 | 0.8 | 24.5 | 26.3 | 7.9 | 0.3 | 9.1 | 9.8 | 3.0 | 0.3 | 9.1 | 9.8 | 3.0 |
| 9 | 0.8 | 24.0 | 25.9 | 8.0 | 0.8 | 24.0 | 25.9 | 8.0 | 0.3 | 9.4 | 10.1 | 3.1 | 0.3 | 9.4 | 10.1 | 3.1 |
| 10 | 0.7 | 23.4 | 25.4 | 8.0 | 0.7 | 23.4 | 25.4 | 8.0 | 0.3 | 9.6 | 10.4 | 3.3 | 0.3 | 9.6 | 10.4 | 3.3 |
| 11 | 0.7 | 22.9 | 25.0 | 7.8 | 0.7 | 23.3 | 24.9 | 7.8 | 0.3 | 10.1 | 11.0 | 3.4 | 0.3 | 10.3 | 11.0 | 3.5 |
| 12 | 0.6 | 22.4 | 24.5 | 7.5 | 0.6 | 23.1 | 24.4 | 7.6 | 0.3 | 10.6 | 11.6 | 3.5 | 0.3 | 11.0 | 11.5 | 3.6 |
| 13 | 0.5 | 21.8 | 24.0 | 7.3 | 0.6 | 23.0 | 23.9 | 7.4 | 0.3 | 11.0 | 12.1 | 3.7 | 0.3 | 11.7 | 12.0 | 3.8 |
| 14 | 0.5 | 21.3 | 23.5 | 7.0 | 0.5 | 22.8 | 23.3 | 7.3 | 0.2 | 11.5 | 12.7 | 3.8 | 0.3 | 12.3 | 12.6 | 3.9 |
| 15 | 0.4 | 20.8 | 23.0 | 6.8 | 0.5 | 22.6 | 22.8 | 7.1 | 0.2 | 11.9 | 13.3 | 3.9 | 0.3 | 13.0 | 13.1 | 4.1 |
| 16 | 0.4 | 20.5 | 22.9 | 6.8 | 0.5 | 22.3 | 22.2 | 7.1 | 0.2 | 11.8 | 13.1 | 3.9 | 0.3 | 12.8 | 12.7 | 4.1 |
| 17 | 0.3 | 20.1 | 22.7 | 6.8 | 0.5 | 22.0 | 21.5 | 7.1 | 0.2 | 11.6 | 13.0 | 3.9 | 0.3 | 12.7 | 12.4 | 4.1 |
| 18 | 0.3 | 19.8 | 22.5 | 6.9 | 0.4 | 21.7 | 20.9 | 7.1 | 0.2 | 11.4 | 12.9 | 3.9 | 0.3 | 12.5 | 12.0 | 4.1 |
| 19 | 0.3 | 19.5 | 22.3 | 6.9 | 0.4 | 21.4 | 20.3 | 7.1 | 0.2 | 11.2 | 12.8 | 4.0 | 0.3 | 12.3 | 11.6 | 4.1 |
| 20 | 0.3 | 19.2 | 22.1 | 6.9 | 0.4 | 21.1 | 19.6 | 7.1 | 0.2 | 11.1 | 12.7 | 4.0 | 0.3 | 12.1 | 11.3 | 4.1 |
| 21 | 0.3 | 19.2 | 22.1 | 6.9 | 0.4 | 21.1 | 19.6 | 7.1 | 0.2 | 11.1 | 12.7 | 4.0 | 0.3 | 12.1 | 11.3 | 4.1 |
| 22 | 0.3 | 19.2 | 22.1 | 6.9 | 0.4 | 21.1 | 19.6 | 7.1 | 0.2 | 11.1 | 12.7 | 4.0 | 0.3 | 12.1 | 11.3 | 4.1 |
Table 4.
Absorbed doses (mGy) to brain, thyroid, breast and RBM calculated for male and female reference individuals with the ages from 0 to 22 y who underwent brain CT scans for pre- and post-2001 time periods in the UK.
| Brain Scan | Pre-2001 |
Post-2001 |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
Male |
Female |
|||||||||||||
| Age (y) | Brain | Thyroid | Breast | RBM | Brain | Thyroid | Breast | RBM | Brain | Thyroid | Breast | RBM | Brain | Thyroid | Breast | RBM |
| 0 | 56.0 | 9.2 | 1.1 | 16.3 | 56.0 | 9.2 | 1.1 | 16.3 | 27.5 | 4.5 | 0.5 | 8.0 | 27.5 | 4.5 | 0.5 | 8.0 |
| 1 | 47.4 | 4.0 | 0.4 | 17.1 | 47.4 | 4.0 | 0.4 | 17.1 | 23.2 | 1.9 | 0.2 | 8.4 | 23.2 | 1.9 | 0.2 | 8.4 |
| 2 | 46.0 | 3.5 | 0.4 | 16.1 | 46.0 | 3.5 | 0.4 | 16.1 | 24.4 | 1.8 | 0.2 | 8.5 | 24.4 | 1.8 | 0.2 | 8.5 |
| 3 | 44.6 | 3.0 | 0.3 | 15.0 | 44.6 | 3.0 | 0.3 | 15.0 | 25.6 | 1.6 | 0.2 | 8.5 | 25.6 | 1.6 | 0.2 | 8.5 |
| 4 | 43.3 | 2.5 | 0.3 | 14.0 | 43.3 | 2.5 | 0.3 | 14.0 | 26.7 | 1.5 | 0.2 | 8.6 | 26.7 | 1.5 | 0.2 | 8.6 |
| 5 | 41.9 | 2.0 | 0.3 | 13.0 | 41.9 | 2.0 | 0.3 | 13.0 | 27.9 | 1.3 | 0.2 | 8.6 | 27.9 | 1.3 | 0.2 | 8.6 |
| 6 | 41.7 | 1.9 | 0.2 | 11.8 | 41.7 | 1.9 | 0.2 | 11.8 | 29.4 | 1.3 | 0.2 | 8.1 | 29.4 | 1.3 | 0.2 | 8.1 |
| 7 | 41.4 | 1.9 | 0.2 | 10.5 | 41.4 | 1.9 | 0.2 | 10.5 | 30.8 | 1.4 | 0.2 | 7.6 | 30.8 | 1.4 | 0.2 | 7.6 |
| 8 | 41.2 | 1.8 | 0.2 | 9.3 | 41.2 | 1.8 | 0.2 | 9.3 | 32.3 | 1.4 | 0.2 | 7.0 | 32.3 | 1.4 | 0.2 | 7.0 |
| 9 | 41.0 | 1.7 | 0.2 | 8.1 | 41.0 | 1.7 | 0.2 | 8.1 | 33.7 | 1.4 | 0.2 | 6.5 | 33.7 | 1.4 | 0.2 | 6.5 |
| 10 | 40.8 | 1.7 | 0.2 | 6.9 | 40.8 | 1.7 | 0.2 | 6.9 | 35.2 | 1.5 | 0.2 | 6.0 | 35.2 | 1.5 | 0.2 | 6.0 |
| 11 | 40.4 | 1.6 | 0.2 | 6.3 | 40.7 | 1.6 | 0.2 | 6.5 | 36.7 | 1.4 | 0.1 | 5.6 | 37.0 | 1.4 | 0.1 | 5.9 |
| 12 | 40.0 | 1.4 | 0.1 | 5.8 | 40.6 | 1.4 | 0.1 | 6.1 | 38.1 | 1.3 | 0.1 | 5.3 | 38.8 | 1.3 | 0.1 | 5.8 |
| 13 | 39.6 | 1.3 | 0.1 | 5.2 | 40.5 | 1.3 | 0.1 | 5.8 | 39.6 | 1.3 | 0.1 | 5.0 | 40.6 | 1.3 | 0.1 | 5.7 |
| 14 | 39.2 | 1.2 | 0.1 | 4.6 | 40.4 | 1.2 | 0.1 | 5.4 | 41.1 | 1.2 | 0.1 | 4.7 | 42.4 | 1.2 | 0.1 | 5.6 |
| 15 | 38.7 | 1.0 | 0.1 | 4.0 | 40.3 | 1.1 | 0.1 | 5.0 | 42.5 | 1.1 | 0.1 | 4.4 | 44.2 | 1.2 | 0.1 | 5.5 |
| 16 | 37.4 | 1.1 | 0.1 | 3.5 | 39.8 | 1.1 | 0.1 | 4.4 | 41.1 | 1.2 | 0.1 | 3.8 | 43.7 | 1.2 | 0.1 | 4.8 |
| 17 | 36.1 | 1.1 | 0.1 | 3.0 | 39.4 | 1.1 | 0.1 | 3.7 | 39.6 | 1.2 | 0.1 | 3.2 | 43.3 | 1.2 | 0.1 | 4.1 |
| 18 | 34.7 | 1.2 | 0.1 | 2.4 | 39.0 | 1.1 | 0.1 | 3.1 | 38.1 | 1.3 | 0.1 | 2.7 | 42.8 | 1.2 | 0.1 | 3.4 |
| 19 | 33.4 | 1.2 | 0.1 | 1.9 | 38.5 | 1.1 | 0.1 | 2.5 | 36.7 | 1.3 | 0.1 | 2.1 | 42.3 | 1.2 | 0.1 | 2.7 |
| 20 | 32.1 | 1.2 | 0.1 | 1.3 | 38.1 | 1.1 | 0.1 | 1.8 | 35.2 | 1.4 | 0.1 | 1.5 | 41.8 | 1.2 | 0.1 | 2.0 |
| 21 | 32.1 | 1.2 | 0.1 | 1.3 | 38.1 | 1.1 | 0.1 | 1.8 | 35.2 | 1.4 | 0.1 | 1.5 | 41.8 | 1.2 | 0.1 | 2.0 |
| 22 | 32.1 | 1.2 | 0.1 | 1.3 | 38.1 | 1.1 | 0.1 | 1.8 | 35.2 | 1.4 | 0.1 | 1.5 | 41.8 | 1.2 | 0.1 | 2.0 |
Table 6.
Absorbed doses (mGy) to brain, thyroid, breast and RBM calculated for male and female reference individuals with the ages from 0 to 22 y who underwent abdomen CT scans for pre- and post-2001 time periods in the UK.
| Abdomen scan | Pre-2001 |
Post-2001 |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
Male |
Female |
|||||||||||||
| Age (y) | Brain | Thyroid | Breast | RBM | Brain | Thyroid | Breast | RBM | Brain | Thyroid | Breast | RBM | Brain | Thyroid | Breast | RBM |
| 0 | 0.4 | 2.2 | 14.0 | 7.6 | 0.4 | 2.2 | 14.0 | 7.6 | 0.2 | 0.8 | 5.1 | 2.8 | 0.2 | 0.8 | 5.1 | 2.8 |
| 1 | 0.2 | 2.2 | 11.0 | 6.9 | 0.2 | 2.2 | 11.0 | 6.9 | 0.1 | 0.8 | 4.0 | 2.5 | 0.1 | 0.8 | 4.0 | 2.5 |
| 2 | 0.2 | 1.9 | 10.8 | 6.3 | 0.2 | 1.9 | 10.8 | 6.3 | 0.1 | 0.7 | 4.0 | 2.3 | 0.1 | 0.7 | 4.0 | 2.3 |
| 3 | 0.2 | 1.7 | 10.6 | 5.6 | 0.2 | 1.7 | 10.6 | 5.6 | 0.1 | 0.6 | 3.9 | 2.1 | 0.1 | 0.6 | 3.9 | 2.1 |
| 4 | 0.2 | 1.4 | 10.4 | 5.0 | 0.2 | 1.4 | 10.4 | 5.0 | 0.1 | 0.5 | 3.8 | 1.8 | 0.1 | 0.5 | 3.8 | 1.8 |
| 5 | 0.1 | 1.1 | 10.2 | 4.4 | 0.1 | 1.1 | 10.2 | 4.4 | 0.1 | 0.4 | 3.8 | 1.6 | 0.1 | 0.4 | 3.8 | 1.6 |
| 6 | 0.1 | 1.1 | 10.0 | 4.7 | 0.1 | 1.1 | 10.0 | 4.7 | 0.1 | 0.4 | 3.9 | 1.8 | 0.1 | 0.4 | 3.9 | 1.8 |
| 7 | 0.1 | 1.0 | 9.8 | 5.0 | 0.1 | 1.0 | 9.8 | 5.0 | 0.1 | 0.4 | 4.0 | 2.1 | 0.1 | 0.4 | 4.0 | 2.1 |
| 8 | 0.1 | 1.0 | 9.6 | 5.4 | 0.1 | 1.0 | 9.6 | 5.4 | 0.1 | 0.4 | 4.1 | 2.3 | 0.1 | 0.4 | 4.1 | 2.3 |
| 9 | 0.1 | 1.0 | 9.5 | 5.7 | 0.1 | 1.0 | 9.5 | 5.7 | 0.1 | 0.4 | 4.2 | 2.6 | 0.1 | 0.4 | 4.2 | 2.6 |
| 10 | 0.1 | 1.0 | 9.3 | 6.0 | 0.1 | 1.0 | 9.3 | 6.0 | 0.1 | 0.5 | 4.3 | 2.8 | 0.1 | 0.5 | 4.3 | 2.8 |
| 11 | 0.1 | 0.9 | 9.1 | 5.7 | 0.1 | 0.9 | 9.1 | 5.8 | 0.0 | 0.4 | 4.6 | 2.8 | 0.0 | 0.4 | 4.6 | 2.9 |
| 12 | 0.1 | 0.7 | 8.9 | 5.3 | 0.1 | 0.8 | 8.9 | 5.6 | 0.0 | 0.4 | 4.8 | 2.8 | 0.0 | 0.4 | 4.8 | 3.0 |
| 13 | 0.1 | 0.6 | 8.7 | 5.0 | 0.1 | 0.7 | 8.7 | 5.4 | 0.0 | 0.3 | 5.0 | 2.8 | 0.0 | 0.4 | 5.0 | 3.1 |
| 14 | 0.1 | 0.5 | 8.6 | 4.6 | 0.1 | 0.6 | 8.5 | 5.1 | 0.0 | 0.3 | 5.3 | 2.8 | 0.0 | 0.4 | 5.2 | 3.1 |
| 15 | 0.0 | 0.4 | 8.4 | 4.3 | 0.0 | 0.5 | 8.3 | 4.9 | 0.0 | 0.3 | 5.5 | 2.8 | 0.0 | 0.4 | 5.4 | 3.2 |
| 16 | 0.0 | 0.4 | 8.3 | 4.3 | 0.0 | 0.6 | 8.1 | 5.0 | 0.0 | 0.3 | 5.4 | 2.8 | 0.0 | 0.4 | 5.3 | 3.3 |
| 17 | 0.0 | 0.4 | 8.2 | 4.3 | 0.0 | 0.6 | 7.9 | 5.2 | 0.0 | 0.3 | 5.4 | 2.8 | 0.0 | 0.4 | 5.2 | 3.4 |
| 18 | 0.0 | 0.4 | 8.1 | 4.3 | 0.0 | 0.6 | 7.7 | 5.4 | 0.0 | 0.2 | 5.3 | 2.8 | 0.0 | 0.4 | 5.0 | 3.5 |
| 19 | 0.0 | 0.4 | 8.1 | 4.3 | 0.0 | 0.7 | 7.4 | 5.5 | 0.0 | 0.2 | 5.3 | 2.8 | 0.0 | 0.4 | 4.9 | 3.6 |
| 20 | 0.0 | 0.3 | 8.0 | 4.3 | 0.0 | 0.7 | 7.2 | 5.7 | 0.0 | 0.2 | 5.2 | 2.8 | 0.0 | 0.5 | 4.7 | 3.7 |
| 21 | 0.0 | 0.3 | 8.0 | 4.3 | 0.0 | 0.7 | 7.2 | 5.7 | 0.0 | 0.2 | 5.2 | 2.8 | 0.0 | 0.5 | 4.7 | 3.7 |
| 22 | 0.0 | 0.3 | 8.0 | 4.3 | 0.0 | 0.7 | 7.2 | 5.7 | 0.0 | 0.2 | 5.2 | 2.8 | 0.0 | 0.5 | 4.7 | 3.7 |
Illustrative organ doses for brain, chest and abdomen scans
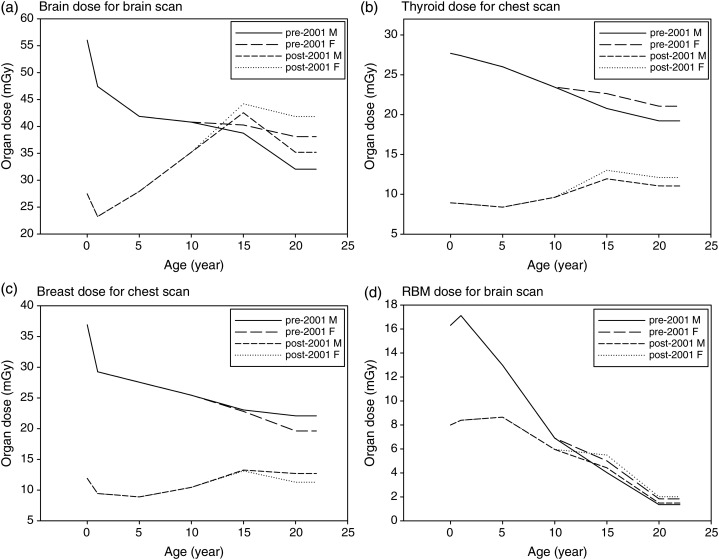
Illustrative doses for the four organs of interest in this study are depicted in Figure 2a–d for different ages, sexes and the two time periods. The organ doses vary depending on two parameters: body dimension represented by age in this study and CTDIvol (Table 3) multiplied to the normalised organ dose database. Firstly, adults overall receive lower doses compared with children which might be caused by the greater attenuation of the X-ray due to their larger body dimensions than children. Secondly, in case of pre-2001 scans where identical CTDIvol was assumed for children and adults, the decreasing trend of organ doses caused by the body size is clear. However, as for post-2001, an overall greater CTDIvol was assumed for adults than for children and it results in a diminished trend in organ doses across age.
Figure 2.
Organ-specific radiation dose by patient age and sex for the two time periods, pre- and post-2001 in the UK: (a) brain dose for brain CT scan; (b) thyroid dose for chest CT scan; (c) breast dose for chest CT scan and (d) RBM dose for brain CT scan.
Brain doses for the brain scan for male and female in pre- and post-2001 time periods are presented for the ages 0, 1, 5, 10, 15 and 20 y in Figure 2a. In case of the pre-2001 where identical CTDIvol, 51 mGy (Table 3), was assumed for children and adults, the brain doses decrease as the age increases due to the increasing body dimensions. For post-2001, 25, 34, 44 and 56 mGy were assumed for ages 0, 1, 5, 10, 15 y, and adults, respectively, which results in an overall increase in brain doses for older individuals. In both time periods, females receive greater brain doses than males after the age of 10 years which might be caused by their smaller head dimension compared with that of males. Similar trends in dose with age and time period are observed for thyroid and breast doses as shown in Figure 2b and c, although the differences in the thyroid and breast doses between the two time periods are greater for adults compared with those of the brain dose as shown in Figure 2a. As for the pre-2001 period when the scan protocol for adults was applied to children, the newborn receives 1.7-fold greater brain dose than the adult male in the brain scan. The thyroid and breast in the newborn undergoing chest scan receive 1.4- and 1.7-fold greater doses, respectively, than those in the adult male.
Figure 2d shows the RBM doses in the male and female exposed to the brain CT scan for the two time periods. The RBM dose significantly decreases with increasing age at exposure. Before 2001 the newborn receives about an 8-fold greater RBM dose than the 20-year old individual. The RBM dose for the brain examination is mostly dependent on the distribution of the RBM in the cranium and mandible, which is significantly lower in the older individuals than in younger ones(39). The difference in the RBM doses between newborn and adult is substantially decreased after 2001 since approximately half of the CTDIvol value, 25 mGy, is used for the newborn compared with 56 mGy for adults. Females receive slightly greater RBM doses compared with males which might be attributed to the smaller head size.
CONCLUSION
State-of-the-art paediatric phantoms combined with detailed national survey data to estimate typical organ-specific doses delivered by CT scans to children for a retrospective cohort study in the UK were used. Absorbed doses to brain, thyroid, breast and RBM were calculated for reference male and female individuals of ages 0, 1, 5, 10, 15 and 20 y for a total of 17 different scan types for the two time periods ≤2001 and >2001.
To the authors' knowledge, the organ dose database established in this study provides the only detailed and comprehensive estimates of typical organ doses by patient age, sex and time period for various types of CT scans. Although some dose estimates from CT scans were reported based on national survey data or literature review(29, 30, 34, 40, 41), they typically provided effective dose rather than organ doses, which are necessary for epidemiological studies. Also, the data were generally limited to adults. A key strength of this study was the use of a series of phantoms with a higher age resolution from newborn to adults for both males and females and with more realistic anatomy compared with the existing computational phantoms used in CT dosimetry. In addition, the latest bone marrow dosimetry models considering more realistic bone marrow fraction and dose response function by patient age was used. These advanced features have the ability to result in more accurate organ-specific dose estimates for epidemiological analysis.
Nevertheless, there are a couple of important assumptions involved in dose estimates where practical data were not available. Average CT scan setting data from national surveys rather than data from individual patients were used because these could not be obtained for the full cohort. The authors also assumed no technical adjustment depending on age before 2001. It will be necessary to perform an uncertainty analysis of dose estimates in the cohort study to assess the impact of the dose uncertainty on the epidemiological risk analysis.
The database here is the first detailed organ-specific paediatric CT scan database for the UK. It will be used to quantify the magnitude of the cancer risk in relation to the radiation dose from CT scans in this cohort study. The results and description of the methods are also an essential resource for other paediatric CT scan studies currently underway in other countries.
ACKNOWLEDGEMENTS
Dr. Elaine Ron died of cancer on 20 November 2010. The authors greatly appreciate her contributions, support and devotion to this study and to the field of radiation epidemiology.
FUNDING
This study was supported by contract NO2-CP-75501 from the US National Cancer Institute and through funding from the Radiation Research Programme of the UK Department of Health (Grant RRX 119). This research was supported in part by the Intramural Research Program of the National Institutes of Health and the National Cancer Institute.
REFERENCES
- 1.NCRP. National Council on Radiation Protection and Measurement; 2009. Ionizing radiation exposure of the population of the United States. [Google Scholar]
- 2.HPA. Health Protection Agency; 2010. Frequency and collective dose for medical and dental X-ray examinations in the UK, 2008 HPA-CRCE-012. [Google Scholar]
- 3.Mettler F. A., Jr, Thomadsen B. R., Bhargavan M., Gilley D. B., Gray J. E., Lipoti J. A., McCrohan J., Yoshizumi T. T., Mahesh M. Medical radiation exposure in the US in 2006: preliminary results. Health Phys. 2008;95:502. doi: 10.1097/01.HP.0000326333.42287.a2. [DOI] [PubMed] [Google Scholar]
- 4.Mettler F. A., Jr. Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources. Radiology. 2009;253:520–531. doi: 10.1148/radiol.2532082010. [DOI] [PubMed] [Google Scholar]
- 5.Pearce M. S., Salotti J. A., McHugh K., Metcalf W., Kim K. P., Craft A. W., Parker L., Ron E. CT scans in young people in Northern England: trends and patterns 1993–2002. Pediatr. Radiol. 2011;1:832–838. doi: 10.1007/s00247-011-2110-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NAS. National Academy of Sciences; 2005. Health risks from exposure to low levels of ionizing radiation: BEIR VII phase 2. [PubMed] [Google Scholar]
- 7.Berrington de Gonzalez A., Mahesh M., Kim K. P., Bhargavan M., Lewis R., Mettler F., Land C. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch. Intern. Med. 2009;169:2071–2077. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brenner D. J., Elliston C. D., Hall E. J., Berdon W. E. Estimated risks of radiation-induced fatal cancer from pediatric CT. Am. J. Roentgenol. 2001;176:289–296. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 9.NRPB. National Radiological Protection Board; 1991. Survey of CT practice in the UK. Part 3—normalized organ doses calculated using Monte Carlo techniques. NRPB-R250. [Google Scholar]
- 10.NRPB. National Radiological Protection Board; 1993. Normalized organ doses for x-ray computed tomography calculated using Monte Carlo techniques. NRPB-SR250. [Google Scholar]
- 11.Zankl M., Panzer W., Drexler G. The Calculation of Dose from External Photon Exposures Using Reference Human Phantoms and Monte Carlo Methods, Part VI: Organ Doses from Computed Tomographic Examinations. GSF, Gesellschaft für Strahlen und Umweltforschung mbH; 1991. [Google Scholar]
- 12.Zankl M., Panzer W., Drexler G. Tomographic Anthropomorphic Models, Part II: Organ Doses from Computed Tomographic Examinations in Paediatric Radiology. Gesellschaft für Strahlen und Umweltforschung mbH; 1993. [Google Scholar]
- 13.ICRP. International Commission on Radiological Protection; 1975. Report on the task group on reference man. ICRP Publication 23. [Google Scholar]
- 14.ICRP. International Commission on Radiological Protection; 2003. Basic anatomical and physiological data for use in radiological protection: reference values. ICRP Publication 89. [Google Scholar]
- 15.Lee C., Lodwick D., Hurtado J., Pafundi D., Williams J. L., Bolch W. E. The UF family of reference hybrid phantoms for computational radiation dosimetry. Phys. Med. Biol. 2010;55:339–363. doi: 10.1088/0031-9155/55/2/002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cristy, M., Eckerman, K. F. Oak Ridge National Laboratory; 1987. Specific absorbed fractions of energy at various ages from internal photon sources. ORNL/TM-8381, vol 1–7. [Google Scholar]
- 17.Zaidi H., Xu X. G. Computational anthropomorphic models of the human anatomy: the path to realistic Monte Carlo modeling in radiological sciences. Ann. Rev. Biomed. Eng. 2007;9:471–500. doi: 10.1146/annurev.bioeng.9.060906.151934. [DOI] [PubMed] [Google Scholar]
- 18.Lee C., Kim K., Long D., Fisher R., Tien C., Simon S., Bouville A., Bolch W. Organ doses for reference adult male and female undergoing computed tomography estimated by Monte Carlo simulations. Med. Phys. 2011;38:1196–1206. doi: 10.1118/1.3544658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee C., Long D., Simon S. L., Bolch W. E. Estimation of organ doses in reference pediatric individuals undergoing computed tomography using monte carlo simulations. Fifty-third Annual Meeting of the American Association of Physicists in Medicine; 2011. p. 3876. July 31–August 4. [Google Scholar]
- 20.Pelowitz D. B. Los Alamos National Laboratory; 2008. MCNPX User's Manual Version 2.6.0. LA-CP-05-0369. [Google Scholar]
- 21.Jarry G., DeMarco J. J., Beifuss U., Cagnon C. H., McNitt-Gray M. F. A Monte Carlo-based method to estimate radiation dose from spiral CT: from phantom testing to patient-specific models. Phys. Med. Biol. 2003;48:2645–2663. doi: 10.1088/0031-9155/48/16/306. [DOI] [PubMed] [Google Scholar]
- 22.Chang K. H., Lee W., Choo D. M., Lee C. S., Kim Y. Dose reduction in CT using bismuth shielding: measurements and Monte Carlo simulations. Radiat. Prot. Dosim. 2010;138:382–388. doi: 10.1093/rpd/ncp278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li X., Samei E., Segars W. P., Sturgeon G. M., Colsher J. G., Toncheva G., Yoshizumi T. T., Frush D. P. Patient-specific radiation dose and cancer risk estimation in CT: Part I. Development and validation of a Monte Carlo program. Med. Phys. 2011;38:397. doi: 10.1118/1.3515839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ICRP. International Commission on Radiological Protection; 2006. Human alimentary tract model for radiological protection. ICRP Publication 100. [DOI] [PubMed] [Google Scholar]
- 25.ICRU. Photon, Electron, Proton and Neutron Interaction Data for Body Tissues. 1992. International Commission on Radiation Units and Measurements.
- 26.Stamm G., Nagel H. D. CT-expo—novel program for dose evaluation in CT. RöFo: Fortschritte auf dem Gebiete der Röntgenstrahlen und der Nuklearmedizin. 2002;174:1570. doi: 10.1055/s-2002-35937. [DOI] [PubMed] [Google Scholar]
- 27.Johnson P. B., Bahadori A. A., Eckerman K. F., Lee C., Bolch W. E. Response functions for computing absorbed dose to skeletal tissues from photon irradiation—an update. Phys. Med. Biol. 2011;56:2347. doi: 10.1088/0031-9155/56/8/002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hough M., Johnson P., Rajon D., Jokisch D., Lee C., Bolch W. An image-based skeletal dosimetry model for the ICRP reference adult male—internal electron sources. Phys. Med. Biol. 2011;56:2309. doi: 10.1088/0031-9155/56/8/001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.NRPB. National Radiological Protection Board; 2005. Doses from computed tomography (CT) examinations in the UK—2003 Review. NRPB-W67. [Google Scholar]
- 30.NRPB. National Radiological Protection Board; 1991. Survey of CT practice in the UK. Part 2—dosimetric aspects. NRPB-R249. [Google Scholar]
- 31.NRPB-R248. National Radiological Protection Board; 1991. Survey of CT practice in the UK. Part 1—aspects of examination frequency and quality assurance. [Google Scholar]
- 32.Romans L. E. Computed Tomography for Technologists: A Comprehensive Test. Lippincott Williams and Wilkins; 2011. [Google Scholar]
- 33.Hollingsworth C., Frush D. P., Cross M., Lucaya J. Helical CT of the body: a survey of techniques used for pediatric patients. AJR Am. J. Roentgenol. 2003;180:401–406. doi: 10.2214/ajr.180.2.1800401. [DOI] [PubMed] [Google Scholar]
- 34.Galanski M., Nagel H. D., Stamm G. Paediatric CT Exposure Practice in the Federal Republic of Germany—Results of a Nationwide Survey in 2005/2006. Hannover Medical School; 2006. [Google Scholar]
- 35.Arch M. E., Frush D. P. Pediatric body MDCT: a 5-year follow-up survey of scanning parameters used by pediatric radiologists. Am. J. Roentgenol. 2008;191:611. doi: 10.2214/AJR.07.2989. [DOI] [PubMed] [Google Scholar]
- 36.Paterson A., Frush D. P., Donnelly L. F. Helical CT of the body: are settings adjusted for pediatric patients? Am. J. Roentgenol. 2001;176:297–301. doi: 10.2214/ajr.176.2.1760297. [DOI] [PubMed] [Google Scholar]
- 37.Rogers L. F. Taking care of children: check out the parameters used for helical CT. Am. J. Roentgenol. 2001;176:287. doi: 10.2214/ajr.176.2.1760287. [DOI] [PubMed] [Google Scholar]
- 38.ImPACT. ImPACT CT Patient Dosimetry Calculator. 2008. http://www.impactscan.org/ctdosimetry.htm . [Google Scholar]
- 39.ICRP. International Commission on Radiological Protection; 1996. Basic anatomical and physiological data: the skeleton. ICRP Publication 70. [PubMed] [Google Scholar]
- 40.CRCPD. Conference of Radiation Control Program Directors; 2007. Nationwide evaluation of x-ray trends (NEXT): tabulation and graphical summary of 2000 survey of computed tomography. CRCPD Publication E-07-2. [Google Scholar]
- 41.Mettler F. A., Huda W., Yoshizumi T. T., Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008;248:254–263. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]