Abstract
Study objective
We sought to determine, using video review, the frequencies of first attempt success and adverse effects during rapid sequence intubation (RSI) in a large, tertiary care pediatric emergency department (ED).
Methods
We conducted a retrospective study of children undergoing RSI in the ED of a pediatric institution. Data were collected from pre-existing video and written records of care provided. The primary outcome was successful intubation on the first attempt at laryngoscopy. The secondary outcome was the occurrence of any adverse effect during RSI, including episodes of physiologic deterioration. We collected time data from the RSI process using video review. We explored the association between physician type and first attempt success.
Results
We obtained complete records for 114 of 123 (93%) children who underwent RSI in the ED over 12 months. Median age was 2.4 years and 89 (78%) were medical resuscitations. Of the 114 subjects, 59 (52%) were successfully intubated on the first attempt. Seventy subjects (61%) had one or more adverse effects during RSI; 38 (33%) suffered oxyhemoglobin desaturation and two required cardiopulmonary resuscitation after physiologic deterioration. Fewer adverse effects were documented in the written records than were noted on video review. The median time from induction through final endotracheal tube placement was 3 minutes. After adjusting for patient characteristics and illness severity, attending level providers were 10 times more likely to be successful on the first attempt than all trainees combined.
Conclusions
Video review of RSI revealed that first attempt failure and adverse effects were much more common than previously reported for children in an ED.
INTRODUCTION
Background
Rapid sequence intubation (RSI) is the standard for definitive airway management in emergency medicine.1–4 The administration, in rapid succession, of sedative and neuromuscular blocking medications is designed to optimize conditions for emergent intubation while limiting the risk of patient harm. RSI is reported to be a highly successful and safe procedure among adult emergency department (ED) patients,1,2,4 with one multicenter study reporting success on the first attempt for 85% of these patients.2 Children are thought to be at greater risk during emergent intubation, for both failed attempts and adverse effects.1 To our knowledge, there are few studies that report pediatric-specific data for RSI in an ED, all of which have important limitations.3,5–9
In a report from the National Emergency Airway Registry (NEAR), 156 children (18 years or younger) had intubation attempted in an ED setting, including one dedicated pediatric ED. For the 127 children who underwent RSI, 78% were successfully intubated on the first attempt and 16% had at least one adverse effect (including 2% with desaturation, 7% with mainstem intubation, and 4% with esophageal intubation).3 In a separate retrospective study of 143 children intubated in a pediatric ED, bradycardia was reported in 4% of patients and hypoxemia in 22%.5 These studies likely under-report the frequency of both first attempt failure and adverse effects, due to voluntary self-reporting or the limitations of chart review. Our clinical experience and quality assurance efforts suggested failed first attempts and adverse effects occur more commonly than reported for pediatric emergency patients undergoing RSI.
Importance
RSI is among the most common critical procedures performed for pediatric emergency patients and should be a high priority for quality assurance efforts.9–11 First attempt success is used as a measure of the quality of the RSI process and the ease of intubation.2,3 The failure of early attempts at intubation may deplete a patient’s oxygen reserve, leading to physiologic deterioration of an already critically ill or injured child. An accurate description of the frequency of first attempt success and adverse effects of RSI for children in an ED setting will allow a better risk assessment and inform targeted interventions to reduce that risk.
Goals of This Investigation
The goal of our study was to accurately and thoroughly describe the process, success, and safety of RSI for patients in a busy pediatric ED. Using video review, we specifically sought to determine the frequencies of first attempt success and adverse effects for patients undergoing RSI in a pediatric ED.
METHODS
Study design
We performed a retrospective, observational study using video-review as the primary method of data collection. Our institutional review board approved our protocol prior to study commencement.
Setting
We conducted our study in the ED of a tertiary-care children’s hospital, which is the major regional provider of emergency care to children and has approximately 90,000 annual visits. In this ED, critically ill or injured patients are managed in one of four resuscitation bays by a designated team, which includes ED physician and nurse team leaders, a pediatric or emergency medicine resident, several bedside nurses, and a respiratory therapist. The physician team leader is either board-certified in Pediatric Emergency Medicine (PEM) or a second or third-year fellow in PEM. For critically injured patients, the team also includes a general surgery resident, a surgical fellow or attending surgeon, and providers from Anesthesiology and Critical Care. During the study period, no standard protocol for the practice of RSI was in place and video-assisted laryngoscopy was not routinely performed.
Since 2000, each of the ED resuscitation bays has had a ceiling-mounted digital camera, which records audio and video continuously. Video recording was instituted for peer review and quality assurance activities, and consent to review these videos is included in our ED’s general consent for care. These cameras give a fixed view, from above the foot of the patient’s bed, of the entire care area (Figure 1). Digital videos were automatically stored on a secure drive and deleted 60 days after the patient’s visit.
Figure 1.

View from Ceiling Mounted Video Camera
Selection of subjects
All children undergoing RSI in our ED between April 1, 2009 and March 31, 2010 were eligible for inclusion. We defined RSI as the administration, in rapid succession, of sedative and neuromuscular blocking medications to facilitate endotracheal intubation.1 We excluded children intubated using non-RSI methods (sedative only or no medications due to cardiac arrest) and any who arrived intubated and did not require re-intubation in the ED. If a patient was intubated using RSI during separate ED visits, each visit was included as a unique encounter if it occurred during the study period.
Data Collection
Using electronic tracking resources, we identified all patients evaluated in the resuscitation area during the study period. A study investigator then reviewed the medical records of these patients to determine if RSI was performed in the ED. We ascertained subject capture through a review of separate patient lists, including ED deaths and admissions to an Intensive Care Unit (ICU) or operating room (OR) within our institution. For patients who underwent RSI in the ED, the corresponding video was downloaded from the secure drive using a proprietary software program (VideoSphere, March Networks, Ottawa, Ontario, Canada). The software’s video display included a time readout in hours, minutes, and seconds. Videos were reviewed separately from patient care and deleted following data collection.
Our methods generally conformed to published guidelines for both observational and chart review studies.12,13 Three investigators (B.K., A.R., M.M.), all board-certified in Pediatric Emergency Medicine (PEM) and experienced with video review, selected the data elements of interest, which were defined through consensus and utilizing the relevant literature. We collectively reviewed the medical and video/audio records of the first 5 study subjects, in order to design and refine the data abstraction form. Each of three investigators (B.K., A.R., and M.M.) collected data on one-third of the remaining patients. When an investigator was involved in a subject’s clinical care, all data for that subject were collected by one of the other investigators.
Video review was the primary source for all study data; if a data point was unavailable or unclear from the video, it was obtained from the medical record or consensus review. If not recorded in the medical record, the data element was considered missing for that subject.
Inter-reviewer reliability
To allow an assessment of the reliability of video review, a second investigator (A.R. or M.M.) reviewed the video and collected data on 12% of subjects. For dichotomous data, we calculated both the percent agreement between reviewers and a corresponding Kappa statistic [95% confidence interval (CI)]. For continuous data elements, and discrete elements of sufficient range, we used Kendall’s tau to assess the correlation of paired observations.
Patient and RSI Process Characteristics
We collected data on patient characteristics, the RSI process, and the intubating providers. As a proxy for severity of illness, we obtained each patient’s 24-hour Pediatric Risk of Mortality score (PRISM II).14 PRISM II is routinely calculated on all patients admitted to our institution’s Pediatric ICU (PICU). For study patients not admitted to the PICU, we calculated the PRISM II score using standard methods.15 Diagnostic category was based on the primary diagnosis assigned to the subject upon discharge from the ED. Indication for intubation was defined by consensus review using a modification of a published scheme.16 We defined physician type for the provider performing the first attempt at intubation, using a combination of training level (postgraduate year) and discipline. Physician types were Pediatric Resident, Emergency Medicine Resident, PEM Fellow, PICU Fellow, PEM Attending, and Providers from Anesthesiology. Using video review, we collected various time data surrounding the RSI process, including the decision to perform RSI, the administration of RSI medications, and the initiation and duration of laryngoscopy.
Outcomes
Our primary outcome was first attempt success, measured as the number of patients with successful intubation on the first attempt at laryngoscopy. We defined an intubation attempt as a single insertion of a laryngoscope blade into a subject’s mouth with the intent of inserting an endotracheal tube (ETT) into the trachea, whether or not ETT placement was attempted.2–4,17–19 We defined successful intubation as the placement of an ETT distal to the glottis, which we judged to have occurred through a combination of video evidence of clinical confirmation, particularly end-tidal carbon dioxide measurement, and the patient’s clinical course after intubation.
Our secondary outcome was the occurrence of adverse effects, measured as the number of patients with video evidence of one or more adverse effects during RSI.2,20 An adverse effect was deemed to be associated with RSI if it occurred between administration of the first RSI sedative and the securing of the final ETT. We included among adverse effects episodes of physiologic deterioration, specifically oxyhemoglobin desaturation, bradycardia, hypotension, and the performance of cardiopulmonary resuscitation (CPR). Oxyhemoglobin desaturation, bradycardia, and hypotension were defined by video evidence of the resuscitating team recognizing or addressing the episode, as continuous vital sign data were unavailable. For desaturation, we required the team to verbalize a desaturation to less than 90% and, if the intubation attempt was unsuccessful, to stop the attempt and initiate bag-valve mask ventilation. For bradycardia and hypotension, the team needed to verbalize the onset of either during RSI. For primary data collection, we did not review the written record to identify additional episodes of physiologic deterioration not evident on video review.
We attempted to identify the following adverse effects using only video review: non-airway intubation, inadequate paralysis (vocalization, biting, and/or general movement at the first attempt), vomiting, and ETT obstruction. The following adverse effects were identified with the aid of the medical record: mainstem intubation (confirmatory chest radiograph), aspiration (foreign material visualized in the airway or a combination of vomiting and new infiltrate on chest radiograph), pneumomediastinum, pneumothorax, and dental/oral injury.
In order to determine the magnitude of potential discrepancies between video review and written documentation, a trained research assistant, blinded to all primary study data, collected data from the written record for three study outcomes: first attempt success, the occurrence of oxyhemoglobin desaturation, and the performance of CPR during RSI. Data sources for this review included the nursing record of the resuscitation and physician procedure notes.
Data analysis
The unit of analysis was the patient visit, not the provider or attempt number. We included the first 5 subjects in the analysis, whose data was collected by consensus review. We tabulated all data and generated descriptive statistics for outcomes and data elements of interest.
We explored the association between physician type and first attempt success. For this analysis, PEM attending physicians and providers from Anesthesiology were combined into one physician type (Attending). We calculated the first attempt success of each physician type; we report first attempt success (as a percentage with 95% CI) for all trainees combined and the Attending type. We also report the unadjusted odd ratio (OR, 95% CI) for the first attempt success of the Attending type compared with all physician trainees.
We then used multivariable logistic regression to explore further the association between physician type (attending versus trainee) and first attempt success, adjusting for covariates with demonstrated or potential associations with success: patient age (years), type of resuscitation (medical versus trauma), PRISM II score, and the presence of inadequate paralysis at the first attempt. For this step in our analysis, we report an adjusted OR (95% CI) for first attempt success, again between the Attending type and all trainees.
SAS software version 9.2 was used for all calculations (Copyright © 2006, SAS Institute Inc., Cary, NC, USA.).
RESULTS
Study Subjects
We reviewed the medical records of 2,999 patients who were managed in the ED resuscitation area during the 12 month study period. We identified 145 who underwent intubation, 123 of whom met our definition of RSI (4% of all patients reviewed) and make up our study sample. Of these 123 patients, 122 were identified through the initial chart review and one from a list of PICU admissions. We obtained videos for 114 of 123 patients (93%); nine videos were unavailable for review due to automated deletion from the secured drive (Figure 2). Few data elements were missing for study subjects: presence of a cervical collar (1 subject), PRISM II score (3), any airway assessment (1), difficult airway exam (1), patient positioning for intubation (1), the performance of pre-oxygenation (3), and the time a clear decision to intubate was made (12) (for definitions of several data elements, please refer to Tables 3 and 4).
Figure 2. Study Subjects.
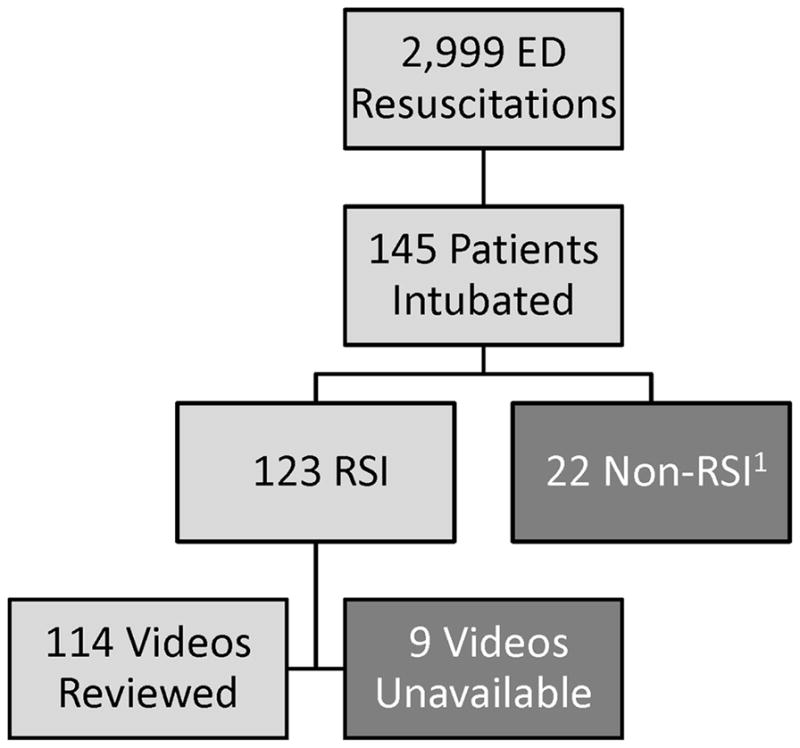
1For these 22 patient, twenty-one were in cardiopulmonary arrest and no meds were given for intubation and one patient received sedation only prior to intubation
Table 3. Characteristics of the RSI Process.
Number of patients (% of 114, unless indicated)
| Arrival Assessment | n (%) |
|---|---|
| Airway adjuncts utilized1 | 12 (11) |
| Airway assessed2 | 40 (35) |
| Difficult airway exam performed3 | 11 (10) |
|
| |
|
Preparation
| |
| Patient positioned for intubation4 | 80 (71) |
| Pre-oxygenation > 3 minutes5 | 86 (77) |
|
| |
|
RSI sedative
| |
| Etomidate | 104 (91) |
| Other6 | 10 (9) |
|
| |
|
RSI Paralytic
| |
| Succinylcholine | 87 (76) |
| Rocuronium | 18 (16) |
| Vecuronium | 9 (8) |
Oral or nasopharyngeal airway.
Any general airway exam as a part of the initial ABC assessment, including statement of “airway clear”, n = 113.
Any component of specific difficult airway exam, as described by Wall et al, n = 113.
Any positioning, including raising the bed, pulling the patient up in the bed, or placing a shoulder roll, n = 113.
Recommended minimum duration for adequate pre-oxygenation by Walls et al, n = 111.
Ketamine (3), midazolam (2), lorazepam (2), thiopental (2), and fentanyl (1).
Table 4. Timing of the RSI Process.
median time in minutes or seconds, n = 114 unless indicated
| Interval | Median (IQR) |
|---|---|
| Arrival to decision1 (min) | 15.7 (6.3, 32.6) |
| Decision to sedative2 (min) | 7.4 (3.8, 10.7) |
| Sedative to final ETT placement (min) | 3.2 (1.9, 7.5) |
| - sedative to laryngoscopy3 (sec) | 90 (66, 132) |
| - laryngoscopy to final ETT (sec) | 72 (30, 246) |
| Final ETT placement to securement4 (min) | 3.6 (2.9, 4.3) |
| Duration of 1st attempt5 (sec) | 36 (24, 54) |
Verbalized decision to intubate, n = 102 for time of decision. Results shown only for 102 subjects with full data.
First sedative medication used for RSI. Visual evidence of administration was used if no clear statement of administration was made. Results shown for the 102 subjects with full data.
First insertion of the laryngoscope blade following administration of the RSI paralytic medication.
Represents the time required for clinical confirmation, including auscultation and ETCO2 monitoring, and taping or otherwise securing the final ETT.
Insertion of the laryngoscope blade to removal.
Characteristics of the study sample are summarized in Table 1. Only two patients were older than 18 years of age: a 48 kilogram 23 year old with special health care needs and a 22 year old patient with alcohol intoxication. A third of subjects were less than 12 months of age, and a third weighed less than 10 kg. Two subjects had a syndrome with associated craniofacial abnormalities; no other child had a known anatomical abnormality of the mouth, throat, larynx, or trachea. The leading indications for intubation were a failure of oxygenation (22 subjects) or ventilation (20), followed by head injury (17), seizure (16), apnea due to infection (12), and altered mental status (11). None of the 114 subjects died in the ED; five died during the corresponding hospitalization.
Table 1. Demographic and Health Characteristics.
Number of patients (% of 114, unless indicated) or median (IQR) shown
| Demographics | |
|---|---|
| Age in years | 2.4 (0.4, 10.1) |
| Weight in kg | 13 (5.7, 38) |
| Gender, female | 54 (47) |
|
| |
|
Presenting Characteristics
| |
| Medical resuscitation (non-trauma) | 89 (78) |
| Cervical collar (n = 113) | 21 (19) |
| Hypoxemic or supplemental oxygen1 (n = 108) | 52 (48) |
| Vital signs on arrival2 | |
| Normal HR and BP | 66 (58) |
| Abnormal HR | 42 (37) |
| Hypotension | 14 (12) |
| Abnormal HR and hypotension | 8 (7) |
|
| |
|
Clinical Characteristics
| |
| PRISM II (n=111) | 6 (2, 12) |
| Diagnostic category3 | |
| Neurologic | 39 (34) |
| Respiratory (lower tract) | 29 (26) |
| Trauma4 | 21 (18) |
| Shock | 13 (11) |
| Other | 12 (11) |
|
| |
|
Disposition from the ED
| |
| ICU | |
| Pediatric | 90 (79) |
| Neonatal | 13 (11) |
| Cardiac | 2 (2) |
| Operating room5 | 6 (5) |
| Transfer to outside facility6 | 3 (3) |
First oxyhemoglobin saturation < 90% (written record) or receiving supplemental oxygen on arrival (video review).
Based on first recorded vital signs and age-based normals (Pediatric Advanced Life Support).
“Neurologic” included seizures and altered mental status. “Respiratory - lower tract” included asthma, pneumonia, and bronchiolitis. “Trauma” included head injuries. “Shock” included any form of shock, including metabolic, septic, cardiogenic, and hypovolemic. “Other” included upper airway obstruction (3), burns/asphyxia (4), intoxication (4), and intra-abdominal process (1).
Seven traumatically injured patients had a diagnostic category other than “Trauma”
One subject discharged to the floor following post-operative extubation and the other five to the PICU.
One subject, a 22 year old girl intubated for alcohol intoxication, was transferred to the nearest adult facilty and two to the local burn center.
Reliability of video review
A second reviewer collected data for 14 subjects (12% of the sample). For first attempt success, our primary outcome, agreement between reviewers was 100% and the kappa statistic 1.0.
Reviewer agreement was 93%, with a kappa of 0.85 (0.57, 1.0), for both the occurrence of desaturation and for episodes of bradycardia during RSI. Agreement was 100% and the kappa statistic1.0 for the identification of the provider performing the first attempt. For most time points, including the times of first sedative administration, first laryngoscopy, and the final securement of the ETT, Kendall’s tau was at least 0.97.
Primary outcome
Intubation was successful on the first attempt for 59 of 114 study subjects (52%; 95% CI 43%, 61%). Twenty-five subjects (22%) were intubated on the second attempt, and 30 (26%) required three or more attempts. All but one subject was intubated by the 5th attempt (one required 9 attempts); all were successfully intubated in the ED. Direct laryngoscopy was used for all but one subject, who was successfully intubated on the first attempt with a video laryngoscope, used during a brief trial of the equipment in the ED. No rescue methods, e.g., laryngeal mask airways, were used for any subject and no surgical airways were performed.
Secondary outcome
Seventy subjects (61%, 95% CI 52%, 70%) experienced at least one adverse effect during RSI and thirty-five (31%, 95% CI 23%, 40%) suffered more than one. The most common adverse effects were physiologic deterioration (primarily oxyhemoglobin desaturation), right mainstem intubation, and non-airway intubation (Table 2). The depth of desaturation was available for 29 of the thirty-eight subjects with an episode identified during RSI. Among these twenty-nine subjects, 22 (76%) had desaturation to below 80% and 10 (29%) to less than 60%. Two subjects with a perfusing rhythm became pulseless following physiologic deterioration during RSI; each received chest compressions and intravenous epinephrine. Both children were successfully intubated on the third attempt, had a subsequent return of spontaneous circulation, and survived to hospital discharge. We did not identify any occurrences of aspiration, pneumothorax, or pneumomediastinum for any subject.
Table 2.
Adverse Effects during RSI
| Physiologic Deterioration | n (% of 114) |
|---|---|
| Any episode | 45 (39) |
| one episode | 23 (20) |
| two or more episodes | 22 (19) |
| Desaturation | 38 (33) |
| Bradycardia | 5 (4) |
| Hypotension | 4 (4) |
| CPR1 | 2 (2) |
|
| |
|
Other Adverse Effects
| |
| Right mainstem intubation2 | 34 (30) |
| left hemi-thorax opacification3 | 5 (4) |
| Non-airway intubation4 | |
| detected | 20 (18) |
| undetected | 1 (1) |
| Inadequate paralysis (first attempt) | 11 (10) |
| Vomiting | 8 (7) |
| Dental/oral injury | 1 (1) |
Patients with a perfusing rhythm who became pulseless and required chest compressions during RSI.
Final radiologist impression of the confirmatory radiograph.
On confirmatory chest radiograph. Presumes complete atelectasis of the left lung in association with right mainstem intubation.
An ETT placed outside the airway. “Detected” indicates misplacement identified by clinical confirmation. “Undetected” indicates misplacement not immediately recognized- this patient was successfully re-intubated after the secured ETT was found to be supraglottic on the confirmatory radiograph.
Discrepancies between video and written records
Focused review of the written record revealed marked variation in the documentation of important aspects of the RSI process as well as notable discrepancies with findings from video review. The nursing record of the resuscitation (n = 83) and the physician procedure note (n = 67) were the sources that most frequently contained documentation of the number of attempts. In the nursing record, first attempt success was 64% (53 of 83) and in the procedure note 58% (39 of 67), representing absolute differences from video review of 12% and 6%, respectively. The written records of 108 subjects either referenced or specifically included physiologic data collected during RSI. Oxyhemoglobin desaturation during RSI was documented for 20 (19%) of these subjects, a difference of 21% compared with video review. Of the 38 subjects noted on video review to experience desaturation during RSI, 20 (53%) had no corresponding documentation in the written record. Only one of the two subjects who underwent CPR during RSI had documentation in the written record that CPR was performed.
Description of the RSI process and time intervals
Characteristics of the RSI process are reported in Table 3 and important time intervals in Table 4. Nearly one quarter of subjects received less than 3 minutes of pre-oxygenation. The median time from a verbalized decision to intubate to final ETT insertion was 11.8 minutes (IQR 8.3, 17.6). In almost 25% of subjects, the duration of laryngoscopy on the first attempt, during which the patient was apneic and not receiving oxygen or ventilation, was over 1 minute.
Analyses of physician type and first attempt success
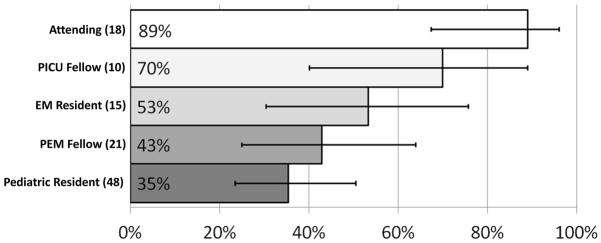
A physician trainee (resident or fellow) performed the first attempt for 84% (96 of 114) of the sample and was in the first 3 years of post-graduate training for 46%. First attempt success varied by physician type (Figure 3). A physician trainee successfully intubated 43 of 96 subjects (45%, 95% CI 35%, 55%) on the first attempt; attending providers were successful on the first attempt for 16 of the remaining 18 subjects (89%, 95% CI 67%, 97%). The unadjusted odds ratio for first attempt success by an attending compared with a trainee was 9.9 (95% CI 2.2, 45.3). After adjusting for patient age, resuscitation type, PRISM II, and inadequate paralysis, attending providers were still ten times more likely to be successful on the first attempt (adjusted odds ratio 10.2, 95% CI 2.1, 50.9).
Figure 3. First Attempt Success by Physician Type (n = subjects per type).
“Attending” is comprised of both attending physicians from Pediatric Emergency Medicine and providers from Anesthesiology. First attempt success was 88% (6 of 7 subjects) for PEM attendings and 91% (10 of 11 subjects) for providers from Anesthesiology. Two study subjects, whose first attempts were performed by a neonatology fellow and an otolaryngology resident, respectively, are not included in this figure. 95% confidence intervals for the first attempt success of each physician type are indicated by the “error” lines: Attending (67%, 97%), PICU Fellow (40%, 89%), EM Resident (30%, 75%), PEM Fellow (25%, 64%), and Pediatric Resident (23%, 50%).
Missing Subjects
For the nine eligible subjects whose videos were unavailable for review, we performed a sensitivity analysis for our main outcomes, using the written record for a select number of data elements. For these subjects, the median age was 4.3 years and seven (78%) were medical resuscitations. Seven of nine subjects were intubated on the first attempt (78%), with attempt number unclear for one patient. Four patients had documentation of an adverse effect in association with RSI: three with right mainstem intubation by confirmatory radiograph and one with an episode of oxyhemoglobin desaturation. None of the nine patients had documentation of pulseless arrest in the ED and all survived to hospital discharge. Based on findings from the written record, the inclusion of these subjects in our study sample would not have meaningfully changed the results for the primary or secondary outcomes.
LIMITATIONS
Our study has several limitations. First, the investigators who reviewed videos for data collection were not blinded to the study’s objectives, which could have biased our determination of adverse effects especially. However, we used standard definitions from the relevant literature and both measures of inter-reviewer agreement were high for adverse effects. Second, we relied on previously recorded videos from the resuscitation area and could not confirm clinical findings with direct observation, which also could have affected our determination of adverse effects. As our definition of physiologic deterioration required verbalization and/or action by the care team, we assume that we still underreport the occurrence of these episodes. Third, we were unable to completely quantify the severity and duration of physiologic deterioration. We report the depth of oxyhemoglobin desaturation for subjects with data available, and for three-quarters of those measured saturation dropped to below 80%. Moreover, even “mild” or brief episodes put a critically ill patient at risk for further deterioration. Fourth, data collection was limited to the ED. We did not attempt to assess whether an episode of deterioration complicated a patient’s subsequent course. Fifth, in a few cases, data were missing or unclear from the video record, as we relied on an unobstructed view and verbalization by the care team. Lastly, our study was conducted at a single, academic pediatric center, which limits generalizability of our findings to other ED settings.
DISCUSSION
RSI is a critical and often lifesaving procedure that, although infrequently performed in the pediatric ED, all emergency physicians must be able to perform successfully and safely. We present data from the first detailed, video-based evaluation of pediatric RSI in the ED. For patients in a pediatric ED, we found a higher frequency of both failed first attempts and adverse effects than previously reported in association with RSI. Importantly, two children had physiologic deterioration during RSI severe enough to require CPR.
There are several potential reasons why we found a lower frequency of first attempt success than previous studies. First, we strictly defined an intubation attempt, thereby capturing brief attempts that might otherwise have been unreported, e.g., those quickly aborted due to inadequate paralysis. We chose to count even brief attempts because any laryngoscopy can increase vagal tone and lead to bradycardia, laryngospasm, vomiting, and oral trauma. In addition, every attempt contributes to the total duration of laryngoscopy, during which the patient is apneic and not being oxygenated or ventilated. Second, our use of video review revealed more frequent first attempt failure and episodes of physiologic deterioration, including the performance of CPR, than was documented in the written record. The discrepancies between video review and written records in our study highlight the limitations of the methodologies employed by previous studies, which almost certainly underestimated the above outcomes. Third, a higher proportion of first attempts in our study were performed by pediatric trainees, who have been reported to be less proficient with intubation than counterparts in other disciplines.3,21 Physician trainee experience with critical procedures such as intubation, especially for pediatric trainees, has declined dramatically in the last 15 years.11,18 In the NEAR study, only 10% of intubations were attempted by pediatric residents, which may partially explain their higher percentage of first attempt success.3
We found a higher frequency of adverse effects than reported in either the NEAR study on pediatric intubations in EDs or, to a lesser extent, in the retrospective study by Fastle et al. In the NEAR study, the combination of self-reporting and convenience sampling likely resulted in falsely low estimates of both attempt failure and adverse effects. Capture rate was not reported and the outcomes for missed patients may have differed considerably. In Fastle et al, the detection of adverse effects depended on accurate recording in the written record. As noted above, we believe that differences in methodology explain most of the observed differences between our study and the existing literature and that the true frequencies of first attempt failure and adverse effects for children undergoing RSI in an ED are closer to our findings.10,22–25
Our study is the first to report a detailed description of the timing of the RSI process for ED patients, making possible an objective evaluation of published recommendations for the duration of various RSI intervals. The Manual of Emergency Airway Management,1 a standard reference for airway management in Emergency Medicine, suggests that once the decision to perform RSI has been made, the entire process should take approximately 11 minutes, from preparation to final placement of the ETT. An evidence basis for this recommendation is not provided. In our study, the time from the decision to intubate to final ETT insertion was 11 minutes or less for 45% of patients and was longer than 20 minutes for 16%. The suggested duration from the administration of sedative and paralytic medications through confirmation of ETT position is approximately 60 seconds.1 For a similar time interval (administration of RSI sedative through final ETT placement) this mark was achieved for three study subjects; the median for this time interval was 3 minutes and for twenty subjects was 10 minutes or more. Although Neonatal Resuscitation Program guidelines were developed for the resuscitation of neonates in a delivery room and not for children in an ED, they provide a published recommendation for the duration of laryngoscopy during emergent intubation, suggesting the “intubation procedure” should be completed within 30 seconds.26 The majority of our subjects had laryngoscopy times, on the first attempt alone, of longer than 30 seconds, with nearly 20% of first attempts lasting over a minute.
Our findings suggest that there may be considerable room for improvement in the practice of RSI for children in pediatric EDs, although additional studies with similar methodology need to be performed to determine the generalizability of our findings. We continue to study RSI in our ED to identify those aspects of the RSI process that are both modifiable and associated with physiologic deterioration. Results of these additional investigations will inform targeted improvement efforts to improve the efficacy and safety of this lifesaving procedure for our patients. The low success rate of trainees, and in particular, pediatric residents, raises the question of whether they should be performing this procedure in the ED. The answer to this question depends on whether physiologic deterioration is related to the failure of early attempts, but the data and analyses presented in this report do not address this question. In the short term, we are attempting to standardize the RSI process at our institution through the development of a formal protocol, which will include data-driven recommendations for the timing of the RSI process. Video laryngoscopy is now used in our ED, and its routine application may improve rates of first attempt success, especially those of trainees.
Our study is the first to utilize video review to study pediatric RSI in the ED setting. Although video review was time consuming, this method allowed a more objective review of ED care, often repeatedly and in slower than real time, offering significant advantages over operator self-report.22–24,27–29 Other authors have noted the value of video review for quality assurance and peer review, specifically for resuscitations.28
In summary, video review of RSI uniquely allowed a detailed description of the success, safety, and timing of this procedure. More importantly, it revealed that first attempt failure and adverse effects were much more common than previously reported for pediatric emergency patients, despite being cared for in a high volume, tertiary care pediatric ED. This is concerning given that RSI is an often lifesaving procedure performed for critically ill patients, who cannot afford the potentially serious consequences of failed attempts and further deterioration. Our findings ought to motivate every institution who cares for pediatric emergency patients both to review the efficacy and safety of the RSI process for their patients.
Acknowledgments
Grants or other financial support: None
The study authors would like to acknowledge Dr. Linda Levin, Shu Zheng, and the Center for Clinical and Translational Science and Training of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center for their time and statistical support for this study.
Footnotes
Presentation Information: Poster presentation at the annual meeting of the Pediatric Academic Societies, Denver, CO, May, 2011.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Walls RM, Murphy MF, editors. Manual of Emergency Airway Management. 3. Lipincott, Williams, and Wilkins; 2008. [Google Scholar]
- 2.Sagarin MJ, Barton ED, Chng YM, et al. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med. 2005 Oct;46(4):328–336. doi: 10.1016/j.annemergmed.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Sagarin MJ, Chiang V, Sakles JC, et al. Rapid sequence intubation for pediatric emergency airway management. Pediatr Emerg Care. 2002 Dec;18(6):417–423. doi: 10.1097/00006565-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Sakles JC, Laurin EG, Rantapaa AA, et al. Airway management in the emergency department: a one-year study of 610 tracheal intubations. Ann Emerg Med. 1998 Mar;31(3):325–332. doi: 10.1016/s0196-0644(98)70342-7. [DOI] [PubMed] [Google Scholar]
- 5.Fastle R, Roback M. Pediatric rapid sequence intubation: incidence of reflex bradycardia and effects of pretreatment with atropine. Pediatr Emerg Care. 2004 Oct;20(10):651–655. doi: 10.1097/01.pec.0000142947.35394.81. [DOI] [PubMed] [Google Scholar]
- 6.Gnauck K, Lungo JB, Scalzo A, et al. Emergency intubation of the pediatric medical patient: use of anesthetic agents in the emergency department. Ann Emerg Med. 1994 Jun;23(6):1242–1247. doi: 10.1016/s0196-0644(94)70348-5. [DOI] [PubMed] [Google Scholar]
- 7.Marvez-Valls E, Houry D, Ernst AA, et al. Protocol for rapid sequence intubation in pediatric patients -- a four-year study. Med Sci Monit. 2002 Apr;8(4):CR229–234. [PubMed] [Google Scholar]
- 8.Sukys GA, Schvartsman C, Reis AG. Evaluation of rapid sequence intubation in the pediatric emergency department. J Pediatr (Rio J) 2011 Jul-Aug;87(4):343–349. doi: 10.2223/JPED.2113. [DOI] [PubMed] [Google Scholar]
- 9.Guilfoyle FJ, Milner R, Kissoon N. Resuscitation interventions in a tertiary level pediatric emergency department: implications for maintenance of skills. CJEM. 2011 Mar;13(2):90–95. doi: 10.2310/8000.2011.110230. [DOI] [PubMed] [Google Scholar]
- 10.Wang HE, Yealy DM. The challenge of defining the “science” of airway management--what is the right outcome measure? Acad Emerg Med. 2003 Jun;10(6):644–645. doi: 10.1111/j.1553-2712.2003.tb00049.x. [DOI] [PubMed] [Google Scholar]
- 11.Green SM, Ruben J. Emergency department children are not as sick as adults: implications for critical care skills retention in an exclusively pediatric emergency medicine practice. J Emerg Med. 2009 Nov;37(4):359–368. doi: 10.1016/j.jemermed.2007.05.048. [DOI] [PubMed] [Google Scholar]
- 12.Gilbert EH, Lowenstein SR, Koziol-McLain J, et al. Chart reviews in emergency medicine research: Where are the methods? Ann Emerg Med. 1996 Mar;27(3):305–308. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- 13.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007 Nov;18(6):800–804. doi: 10.1097/EDE.0b013e3181577654. [DOI] [PubMed] [Google Scholar]
- 14.Pollack MM, Ruttimann UE, Getson PR. Pediatric risk of mortality (PRISM) score. Crit Care Med. 1988 Nov;16(11):1110–1116. doi: 10.1097/00003246-198811000-00006. [DOI] [PubMed] [Google Scholar]
- 15.SFAR. Societe Francaise d’Anesthesie et de Reanimation Web site. [Accessed November 1, 2010]. Scoring systems for ICU and surgical patients: PRISM (Pediatric RIsk of Mortality) [Google Scholar]
- 16.Nishisaki A, Donoghue A, Colborn S, et al. Effect of just-in-time simulation training on tracheal intubation procedure safety in the pediatric intensive care unit. Anesthesiology. 2010 Jul;113(1):214–223. doi: 10.1097/ALN.0b013e3181e19bf2. [DOI] [PubMed] [Google Scholar]
- 17.Lane B, Finer N, Rich W. Duration of intubation attempts during neonatal resuscitation. J Pediatr. 2004 Jul;145(1):67–70. doi: 10.1016/j.jpeds.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Leone T, Rich W, Finer N. Neonatal intubation: success of pediatric trainees. J Pediatr. 2005 May;146(5):638–641. doi: 10.1016/j.jpeds.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 19.Levitan RM, Rosenblatt B, Meiner EM, et al. Alternating day emergency medicine and anesthesia resident responsibility for management of the trauma airway: a study of laryngoscopy performance and intubation success. Ann Emerg Med. 2004 Jan;43(1):48–53. doi: 10.1016/s0196-0644(03)00638-3. [DOI] [PubMed] [Google Scholar]
- 20.Nishisaki A, Donoghue A, Colborn S, et al. Effect of just-in-time simulation training on tracheal intubation procedure safety in the pediatric intensive care unit. Anesthesiology. 2010 Jul;113(1):214–223. doi: 10.1097/ALN.0b013e3181e19bf2. [DOI] [PubMed] [Google Scholar]
- 21.Falck AJ, Escobedo MB, Baillargeon JG, et al. Proficiency of pediatric residents in performing neonatal endotracheal intubation. Pediatrics. 2003 Dec;112(6 Pt 1):1242–1247. doi: 10.1542/peds.112.6.1242. [DOI] [PubMed] [Google Scholar]
- 22.Olsen J, Gurr D, Hughes M. Video analysis of emergency medicine residents performing rapid-sequence intubations. J Emerg Med. 2000 May;18(4):469–472. doi: 10.1016/s0736-4679(00)00168-2. [DOI] [PubMed] [Google Scholar]
- 23.Oakley E, Stocker S, Staubli G, et al. Using video recording to identify management errors in pediatric trauma resuscitation. Pediatrics. 2006 Mar;117(3):658–664. doi: 10.1542/peds.2004-1803. [DOI] [PubMed] [Google Scholar]
- 24.Mackenzie CF, Jefferies NJ, Hunter WA, et al. Comparison of self-reporting of deficiencies in airway management with video analyses of actual performance. LOTAS Group. Level One Trauma Anesthesia Simulation. Hum Factors. 1996 Dec;38(4):623–635. doi: 10.1518/001872096778827297. [DOI] [PubMed] [Google Scholar]
- 25.Nishisaki A, Marwaha N, Kasinathan V, et al. Airway management in pediatric patients at referring hospitals compared to a receiving tertiary pediatric ICU. Resuscitation. 2011 Apr;82(4):386–390. doi: 10.1016/j.resuscitation.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 26.Zaichkin J, Weiner GM. Neonatal Resuscitation Program (NRP) 2011: new science, new strategies. Neonatal Netw. 2011 Jan-Feb;30(1):5–13. doi: 10.1891/0730-0832.30.1.5. [DOI] [PubMed] [Google Scholar]
- 27.O’Donnell CP, Kamlin CO, Davis PG, et al. Endotracheal intubation attempts during neonatal resuscitation: success rates, duration, and adverse effects. Pediatrics. 2006 Jan;117(1):e16–21. doi: 10.1542/peds.2005-0901. [DOI] [PubMed] [Google Scholar]
- 28.Carbine D, Finer N, Knodel E, et al. Video recording as a means of evaluating neonatal resuscitation performance. Pediatrics. 2000 Oct;106(4):654–658. doi: 10.1542/peds.106.4.654. [DOI] [PubMed] [Google Scholar]
- 29.Ritchie PD, Cameron PA. An evaluation of trauma team leader performance by video recording. Aust N Z J Surg. 1999 Mar;69(3):183–186. doi: 10.1046/j.1440-1622.1999.01519.x. [DOI] [PubMed] [Google Scholar]