Abstract
Background
Reduced heart rate variability (HRV) in older patients with heart failure (HF) is common and indicates poor prognosis. Exercise training (ET) has been shown to improve HRV in younger patients with HF. However the effect of ET on HRV in older patients with HF is not known.
Methods and Results
Sixty-six participants (36% males), age 69±5 years, with HF and both preserved ejection fraction (HFPEF) and reduced ejection fraction (HFREF), were randomly assigned to 16 weeks of supervised ET (ET group) versus attention-control (AC group). Two HRV parameters (the standard deviation of all normal RR intervals (SDNN) and the root mean square of successive differences in normal RR intervals (RMSSD)) were measured at baseline and after completion of the study. When compared with the AC group, the ET group had a significantly greater increase in both SDNN (15.46 ± 5.02 ms in ET versus 2.37 ± 2.13 ms in AC, P = 0.016), and RMSSD (17.53 ± 7.83 ms in ET versus 1.69 ± 2.63 ms in AC, P = 0.003). This increase was seen in both genders and HF categories.
Conclusion
ET improves HRV in older patients with both HFREF and HFPEF.
Introduction
Heart failure (HF) is a highly prevalent disease afflicting 5.8 million adults in the United States, with 600,000 new cases diagnosed each year 1. HF has become a disorder of the elderly with more than 80% of those afflicted above the age of 65 1. The majority of older patients with HF have a preserved ejection fraction (HFPEF) 2. Older patients with HF, especially those with HFPEF, have not been well represented in clinical trials which constitute a major clinical challenge since it has been shown that these patients respond differently to novel therapies than younger patients with HF, especially those with reduced ejection fraction (HFREF) 3.
Heart rate variability (HRV) is defined as beat-to-beat variations in heart rate of individuals in sinus rhythm. HRV is a noninvasive, reproducible, and easy-to-obtain measurement of cardiac autonomic nervous system function and its response to environmental changes 4, 5. Reduced HRV generally indicates either attenuation in the autonomic regulation of the sinoatrial node or failure of the sinoatrial node to respond to such regulation 4. Since first described by Hon and Lee in 1965 6, reduced HRV has been seen with normal aging 7, sedentary lifestyle 8, and in a number of neurological, metabolic, inflammatory, and cardiovascular disorders 4. In most of these disorders, reduced HRV has been shown to be an independent predictor of death 4, 9. Patients with HF in particular often have markedly reduced HRV 4, 10-12. Reduced HRV in patients with HF predicts poor prognosis 13. Specifically, impairment in one or more HRV parameter has been found to be a significant predictor of sudden cardiac death 14-16, progression of HF and HF death 17, and total mortality 13, 18-21.
Physical exercise and endurance exercise training (ET) have been shown to improve HRV in various populations, including healthy athletes 8, individuals with sedentary lifestyle 22, survivors of acute myocardial infarction 23, and patients with coronary artery disease who have undergone coronary artery bypass grafting surgery or percutaneous coronary intervention 24. Several studies have examined the impact of ET on HRV in patients with HF showing mostly favorable results 25-30. These studies, however, included only patients who are relatively young (age range: 55-67) and have exclusively HFREF (mean left ventricular ejection fraction range: 29-36%). The ET applied to the intervention groups in these studies varied in mode, intensity, and duration. Some of these studies did not use control groups, only one study used randomization, and none used any method of blinding. Therefore, the objective of the present study was to examine the effect of supervised endurance exercise training (ET) on HRV in older patients with both HFPEF and HFREF in a randomized, controlled, and single-blinded design.
Methods
Study Population and Design
Our subjects were participants in a National Institute of Health-funded clinical trial of ET in patients 65 years or older with both HFPEF and HFREF. The primary outcomes of this trial, exercise capacity and quality-of-life, have been previously reported 31, 32. Neurohormonal activation and autonomic function were among the secondary outcomes of this trial. In this study we will report the impact of ET on HRV as a measure of autonomic function in older patients with HF. All participants who had HRV measured at entry and exit of the trial were included in this study.
The protocol was approved by the Wake Forest University Baptist Medical Center Institutional Review Board. During a screening visit, subjects were familiarized with the testing environment and procedures and written informed consents were obtained. During a subsequent baseline visit, the outcome measures, including HRV measurements, were obtained. All tests, including HRV, were performed in the morning before participants had any oral intake since midnight including medications, except for water. After obtaining baseline measurements participants were randomized to either 16 weeks of aerobic exercise training group (ET) or attention control group (AC). Measurements of HRV were repeated after 16 weeks of ET. All testing was performed and analyzed by individuals blinded to participant’s group allocation.
Heart rate variability
To measure HRV, each participant was connected to a cardiac monitor and asked to lie down in a quiet room with dimmed lights for 15 minutes. Then, a supine, resting 10-minute ECG recording was obtained and used to calculate time-domain HRV parameters using commercially available software (PREDICT II HRVECG, Arrhythmia Research Technology, Inc., Austin, TX). The ECG recordings were examined by an electrophysiologist who was blinded to participant group allocation. Participants with non-sinus rhythm (including atrial fibrillation and paced rhythm) were excluded since HRV could not be measured in these individuals. ECG recordings with normal sinus rhythm were further examined for non-sinus ectopic beats. All ectopic beats and their subsequent sinus beats were filtered out prior to calculating HRV parameters. Because of the short duration of ECG recording, only the following two time-domain HRV parameters could be obtained and used in the analysis: the standard deviation of all normal RR intervals (SDNN), and the root mean square of successive differences in normal RR intervals (RMSSD).
Exercise Training
Participants randomized to ET exercised 3 times per week for 16 weeks for a total of 48 sessions in a dedicated facility under medical supervision 33. Each session lasted one hour and consisted of warm-up, stimulus, and cool-down phases. The stimulus phase consisted of walking on a track as well as lower extremity cycling on a Schwinn Air dyne. Data from the baseline exercise test were used to generate an individualized initial exercise prescription according to standard methods in HF patients. During the initial period of training, participants exercised at 40-50% of heart rate reserve (HRR) for the first two weeks while the duration of the exercise was gradually increased on each of the two modes of exercise (walking and cycling). Over the following several weeks, the intensity of exercise was gradually increased to 60-70 % HRR and the exercise duration was increased to 15-20 minutes on each training mode. The exercise prescription (intensity and duration) was adjusted as needed based on medical considerations and clinical responses 33, 34. Missed exercise sessions were made up so that each patient completed no less than 40 of the 48 (>80%) exercise training sessions.
Participants randomized to the AC group received phone calls every two weeks throughout the 16-week follow-up. This served to provide attention and interaction with the study staff. The telephone conversations focused on adherence with the study protocol, reminders and encouragement to keep upcoming study visits, and to ascertain whether there were any new medical events since the prior contact. The telephone conversations intentionally did not address exercise behaviors.
Statistical analysis
Baseline characteristics were compared between the two study groups using 2-sample t- test for continuous variables and Fisher’s exact test for categorical variables. The changes in HRV between baseline and follow-up were calculated for all participants. Comparisons of change in HRV between groups were made using analysis of covariance (ANCOVA) procedure. To maximize precision and control for random differences between study groups, we adjusted for baseline values of HRV, age, gender, pulse pressure, HF category (HFREF vs HFPEF), and baseline measures of exercise capacity and heart rate recovery. Both HRV parameters (SDNN and RMSSD) were non-normally distributed and logarithmic transformation was applied prior to analysis. In order to evaluate whether the effect of ET on HRV differs by age, gender, or HF category, we repeated the ANCOVA procedure while testing for interaction between ET and each one of these variables separately. Two-sided level of significance was set at p<0.05 for all analyses. SAS-enterprise 9.1 software (SAS institute, Cary, NC, USA) was used for all statistical analyses.
Results
Study population and baseline characteristics
There were 101 participants randomized into the study (50 AC and 51 ET). Of those, 21 participants (10 AC and 11 ET) missed either baseline or follow-up ECG recordings and were excluded from analysis. Among those who had both baseline and follow-up ECG recordings, 14 participants (6 AC and 8 ET) had non-sinus rhythm (atrial fibrillation or permanent pacemaker with paced rhythm) and were excluded from analysis. The remaining 66 participants (35 AC and 31 ET) were included in the analysis. Baseline characteristics of these participants are described in table 1 and were compared between the 2 study groups. Generally, these participants were elderly and representative of patients with HF in the community in age, sex distribution, and the proportion of HFPEF. These participants, however, had randomly higher than usual systolic blood pressure and pulse pressure, and lower than usual rates of usage of certain medications including beta blockers and angiotensin-converting enzyme (ACE) inhibitors. As evident from table 1, ET and AC groups did not differ across a broad range of demographics, comorbid conditions, heart failure characteristics, medications use, and measures of exercise capacity and HRV, all indicates an effective randomization. The only exception was the random difference in pulse pressure, which was higher in the AC group than in the ET group (Table 1).
Table 1.
Baseline characteristics of the 2 study groups:
| Characteristics at baseline | AC group (N= 35) | ET group (N=31) | P-Value |
|---|---|---|---|
| Age | 70.1 ± 5.6 | 68.0 ± 4.8 | 0.099 |
| Men | 13 (37.1) | 11 (35.5) | > 0.9 |
| Caucasians | 28 (80) | 27 (87) | 0.521 |
| Body Weight, kg | 77.7 ± 14.6 | 81.9 ± 14.7 | 0.242 |
| Body mass index, kg/m2, | 28.6± 6.1 | 29.4±5.4 | 0.555 |
| Body surface area, m2 | 1.87 ± 0.20 | 1.93 ± 0.19 | 0.231 |
| Heart Rate | 71.9 ± 10.5 | 76.7 ± 14.5 | 0.132 |
| Systolic Blood Pressure, mmHg | 150.6 ± 19.9 | 143.0 ± 18.3 | 0.116 |
| Diastolic blood pressure, mmHg | 78.7 ±8.3 | 81.5 ± 9.0 | 0.208 |
| Pulse pressure, mmHg | 71.9 ± 16.2 | 61.5 ± 16.2 | 0.013 |
| History of diabetes | 10 (28.6) | 5 (16.1) | 0.256 |
| History of pulmonary edema | 15 (42.9) | 8 (25.8) | 0.198 |
| Beta blockers use | 4 (11.4) | 6 (19.3) | 0.497 |
| Calcium channel blockers use | 12 (34.3) | 9 (29.0) | 0.792 |
| Digoxin use | 12 (34.3) | 9 (29.0) | 0.792 |
| ACE-inhibitors use | 17 (48.6) | 14 (45.2) | 0.810 |
| Exercise peak oxygen uptake, ml/kg/min | 12.9 ± 2.6 | 14.0 ± 2.7 | 0.11 |
| Exercise peak work load, watts | 47.9 ± 16.5 | 53.6 ± 18.6 | 0.189 |
| Exercise time, min | 6.3 ± 2.8 | 7.1 ± 3.2 | 0.172 |
| HRR at 1 minute, beat/min | 20.0 ± 11.8 | 26.3 ± 13.6 | 0.065 |
| SDNN, ms | 30.2 ± 17.7 | 31.6 ± 21.0 | 0.776 |
| RMSSD, ms | 20.4 ± 15.5 | 24.7 ± 24.7 | 0.406 |
| Left ventricular ejection fraction >40% | 20 (57.1) | 17 (54.8) | 1.0 |
| NYHA Class II | 21 (60) | 19 (61.3) | > 0.9 |
| NYHA Class III | 14 (37.1) | 12 (38.7) | > 0.9 |
Values are mean ± SD or number (%). AC =attention control; ET = exercise training; ACE = angiotensin converting enzyme; HRV = heart rate variability; SDNN = the standard deviation of all normal RR intervals; RMSSD = the root mean square of successive differences in normal RR intervals; NYHA = New York heart association.
Participants randomized to ET adhered well to the intervention with an average number of ET sessions attended being 44.2 ± 6.7, and a median compliance (number of sessions attented divided by number of sessions offered for each participant) being 89.1% (interquartile range: 84.6 – 93.3). Missed sessions were often due to acute illness or hospitalization.
Effect of ET on HRV
Following the 16 week intervention, ET group had a significantly greater increase in HRV compared to AC group (Table 2). The mean increase in SDNN was 15.46 ± 5.02 ms in ET group versus 2.37 ± 2.13 ms in AC group (P = 0.016), and the mean increase in RMSSD was 17.53 ± 7.83 ms in ET group versus 1.69 ± 2.63 ms in AC group (P = 0.003) (Figure 1). This effect of ET on HRV did not differ by gender, or HF category (all interaction p values > 0.05). There was, however, a trend toward greater improvement in SDNN in HFREF than in HFPEF (interaction p=0.06) (Figure 2). The increase in HRV measures did not significantly correlate with different measures of exercise capacity including peak exercise oxygen comsumption, peak exercise work load, or exercise time. There was, however, positive correlation between the increase in HRV and the number of ET sessions attended, although such correlation did not reach statistical significance (r = 0.23 (P = 0.22) for change in SDDN, and r = 0.25 (P = 0.16) for MSSD).
Table 2.
Changes in HRV parameters in the 2 study groups:
| HRV | AC group | ET group | P- Value | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Baseline | Follow-up | Change | Baseline | Follow-up | Change | ||
|
|
|
||||||
| SDNN | 30.2 ± 17.7 |
32.6 ± 15.4 |
2.4 ± 2.13 |
31.6 ± 21.0 |
47.0 ± 36.5 |
15.5 ± 5.02 |
0.016 |
|
|
|
||||||
| RMSSD | 20.4 ± 15.5 |
22.1 ± 15.9 |
1.7 ± 2.62 |
24.7 ± 24.7 |
42.3 ± 48.3 |
17.5 ± 7.85 |
0.003 |
Data represent means ± SD. P-Values represent comparison of least squared means of the change in HRV following adjustment for age, gender, heart rate, pulse pressure, beta blockers usage, baseline exercise capacity (peak exercise oxygen uptake, peak work load, exercise time, and heart rate recovery during baseline exercise stress testing) baseline HRV values, and heart failure category (preserved vs reduced ejection fraction). AC =attention control; ET = exercise training; SDNN- the standard deviation of all normal RR intervals; RMSSD- the root mean square of successive differences in normal RR intervals.
Figure 1.
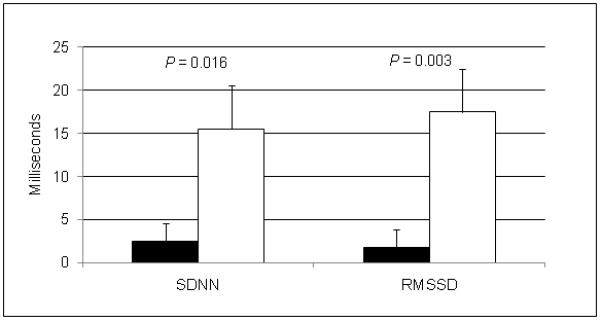
Raw, unadjusted mean changes (± SD) in heart rate variability (HRV) parameters in the two study groups. P values represent comparison of the transformed data after adjusting for age, gender, pulse pressure, heart failure category (preserved vs reduced ejection fraction), and baseline values of HRV and exercise capacity. Black boxes represent the attention control group; white boxes represent the exercise Training group; SDNN = the standard deviation of all normal RR intervals; RMSSD = the root mean square of successive differences in normal RR intervals.
Figure 2.
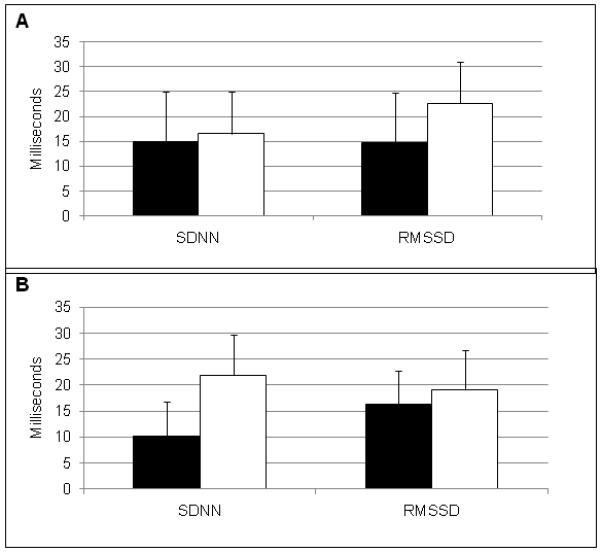
Raw, unadjusted mean changes (± SD) in heart rate variability parameters in the exercise training group stratified by gender (panel A: black boxes represent men; white boxes represent women), and by heart failure categories (panel B: black boxes represent heart failure and preserved ejection fraction; white boxes represent heart failure and reduced ejection fraction). SDNN = the standard deviation of all normal RR intervals; RMSSD = the root mean square of successive differences in normal RR intervals.
Discussion
In this study, we have shown that endurance ET significantly improved HRV in older patients with HF regardless of age, gender, or HF category (HFREF or HFPEF). This improvement in HRV is possibly dose-dependant, and did not correlate with measures of exercise capacity. To our knowledge, this is the first randomized, controlled, and single-blinded study to examine the impact of ET on HRV in older adults with both HFPEF and HFREF. In spite of the challenges in adherence that usually face outpatient exercise studies, we were able to achieve close to 90% compliance rate. Our findings are in agreement with those from earlier studies that have examined the impact of ET on HRV in relatively younger populations who had exclusively HFREF 25-30. Therefore, this study supports the contention that the favorable effect of ET on HRV is robust in a variety of HF populations, including the elderly and those with HFPEF who were not targeted in earlier studies.
Patients with HF often have cardiac autonomic dysfunction manifested with reduced HRV 4, 10. This is thought to be related to neurohormonal activation and attenuation of cardiac vagal tone 11, 12. Elderly patients with HF have even more impaired HRV that is explained in part by age-related autonomic dysfunction 7, and in part by their associated comorbidities such as hypertension, diabetes mellitus, atherosclerotic heart disease, and inflammatory conditions 4. In addition, elderly patients with HF are more often women, have HFPEF, and have a higher burden of non-cardiac comorbidities. They have repeatedly shown to respond differently to various drug therapies and other interventions, including exercise training. Therefore, it was reasonable to expect that impaired HRV in older patients with HF, especially HFPEF, might respond differently to ET than in younger patients with HFREF. With the rising incidence of HF among the elderly, especially HFPEF, it was important to ascertain the benefit of ET on cardiac autonomic dysfunction in this patient population.
The mechanism by which ET improves HRV is not well understood. It is believed, however, that ET increases vagal tone and reduces sympathetic cardiac influence resulting in improvement in HRV 9, 35. At least 2 mediators are thought to play a role in increasing in cardiac vagal tone in response to ET, nitric oxide (NO) and angiotensin II. NO is thought to have a direct effect on cardiac vagal tone, and an indirect effect on sympathetic cardiac influence 36. ET has been shown to improve NO bioavailability and endothelial function 37. The second mediator, angiotensin II, is a known inhibitor of cardiac vagal activity 38. Athletes and physically trained individuals have been shown to have lower levels of plasma renin activity, and therefore lower angiotensin II levels, than non-athletes and untrained individuals 39. Nevertheless, determining the exact mechanism by which ET improves HRV and autonomic cardiac regulation requires additional research studies.
Although it is well-established that impaired HRV in patients with HF is a significant predictor of morbidity and mortality 13, 14, 17, 19, 20, the clinical implication, namely improving exercise capacity and survival, of improving HRV in this patient population is still not established. In this study, we did not find any significant correlation between improvement in HRV and changes in exercise capacity. Such a correlation was reported, however, by Ponikowski et al who demonstrated a significant correlation between improvement in HRV parameters and improvement in ventilatory response to ET 40. Therefore, it remains unclear whether improvement in autonomic dysfunction is a mediator to the improvement in exercise capacity in patients with HF. Our study was not designed to examine survival, so we were unable to examine the correlation between change in HRV and survival. However, survival benefit of improving HRV in response to ET was demonstrated in a small pilot study by Larsen et al 25 who reported a trend toward better survival in patients with HF who showed improvement in HRV in response to ET. Future studies are needed to determine if improvement in HRV indicates improvement in exercise capacity and survival. .
Study Limitations
Although our study participants resemble the general population with HF in several aspects including age, sex distribution, and proportion of HFPEF 1, because this study was conducted several years ago 31, 32, the rates of usage of certain medications including beta blockers and angiotensin-converting enzyme inhibitors (5% and 16% respectively) were lower than current rates. It is unknown whether greater use of these medications would modify the effect of ET on HRV. Considering the relatively small sample size and the low usage of these medications, we were unable to confidently test whether these medications altered the impact of ET on HRV. The high systolic blood pressure and pulse pressure in our study sample could also have altered their response to ET. These high values of systolic and pulse pressures could partially be explained by the high proportion of elderly women with HFPEF among our participants, and partially by the fact that these participants were recruited several years ago before the implementation on newer guidelines that advocate more aggressive management of hypertension. In addition, 2 patient groups were excluded from our study by design which may affect the generalizability of our results. The first group includes those with atrial fibrillation and permanent pacemaker with paced rhythm for whom HRV could not be measured. It is known that patients with atrial fibrillation often have significant autonomic dysfunction 41. However, it remains unknown how ET would impact autonomic dysfunction in these patients. The second group includes those who were unable to undergo exhaustive exercise testing and outpatient supervised ET (those who are non-ambulatory, residing in a nursing home, or recently hospitalized). Therefore it is not clear if lower intensity exercise or unsupervised home-based exercise tailored for these patients in particular would prove beneficial.
We used a relatively short-term recording of HRV (10 minutes). While this method of HRV measurement has been validated 4, long-term recording (24 hour) remains the gold-standard. Since these measurements were done in resting conditions during morning hours, we do not know if the improvement seen in HRV is sustained during adrenergic surges throughout the day. Lastly, in this study we only used time-domain parameters. While time-domain measurements correlate well with frequency-domain measurements of HRV, such correlation is weaker with shorter recording times4.
Although this study was completed a number of years ago 31, 32, its findings are still significant. It fills a critical gap in our knowledge about the impact of ET on HRV in a growing population of older patients with HF, especially those with HFPEF. It shows that autonomic dysfunction in older patients with HF can be safely improved by ET.
Conclusion
ET improves HRV in older patients with HF. This effect is equally significant in men and in women, and may be greater in patients with HFREF than in HFPEF. Further studies are needed to determine the clinical implication of these findings.
Acknowledgments
Acknowledgement of grants and other support: N.I.H. R37AG18915 and RO1AG12257; The Claude D. Pepper Older Americans Independence Center of Wake Forest University
N.I.H. P30AG21332 and N.I.H. MO1RR07122; General Clinical Research Center of the Wake Forest University School of Medicine
N.I.H. 5T32HL087730-02. Training Grant in Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke
The sponsor had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Financial Disclosures:
Khalil Murad, MD: None
Peter H. Brubaker, PhD: Boston Scientific CRM > 10K
David M Fitzgerald, MD: None
Timothy M Morgan, PhD: None
David C. Goff, Jr., MD, PhD: He has served as a consultant for (< $ 10K) and received grant support from Merck (< $10K), and as a DSMB member for a trial funded by Takeda (< $10K).
Elsayed Z Soliman, MD, MS, MSc: None
Joel D Eggebeen, MS: None
Dalane W Kitzman, MD: Has served as consultant for and/or received grant support from Synvista (> $10K), Bristol-Meyers-Squibb (> $10K), Novartis (> $10K), Boston Scientific (> $10K), Relypsa (> $10K), Forest Laboratories, and Medtronic.
References
- 1.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009 Jan 27;119(3):480–486. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- 2.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006 Jul 20;355(3):251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 3.Yusuf S, Pfeffer MA, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003 Sep 6;362(9386):777–781. doi: 10.1016/S0140-6736(03)14285-7. [DOI] [PubMed] [Google Scholar]
- 4.Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996 Mar 1;93(5):1043–1065. [PubMed] [Google Scholar]
- 5.Kleiger RE, Stein PK, Bigger JT., Jr Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol. 2005 Jan;10(1):88–101. doi: 10.1111/j.1542-474X.2005.10101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hon EH, Lee ST. The Fetal Electrocardiogram. 3. Display Techniques. Am J Obstet Gynecol. 1965 Jan 1;91:56–60. doi: 10.1016/0002-9378(65)90586-7. [DOI] [PubMed] [Google Scholar]
- 7.Reardon M, Malik M. Changes in heart rate variability with age. Pacing Clin Electrophysiol. 1996 Nov;19(11 Pt 2):1863–1866. doi: 10.1111/j.1540-8159.1996.tb03241.x. [DOI] [PubMed] [Google Scholar]
- 8.Dixon EM, Kamath MV, McCartney N, Fallen EL. Neural regulation of heart rate variability in endurance athletes and sedentary controls. Cardiovasc Res. 1992 Jul;26(7):713–719. doi: 10.1093/cvr/26.7.713. [DOI] [PubMed] [Google Scholar]
- 9.Routledge FS, Campbell TS, McFetridge-Durdle JA, Bacon SL. Improvements in heart rate variability with exercise therapy. Can J Cardiol. Jun;26(6):303–312. doi: 10.1016/s0828-282x(10)70395-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Casolo G, Balli E, Taddei T, Amuhasi J, Gori C. Decreased spontaneous heart rate variability in congestive heart failure. Am J Cardiol. 1989 Nov 15;64(18):1162–1167. doi: 10.1016/0002-9149(89)90871-0. [DOI] [PubMed] [Google Scholar]
- 11.Nolan J, Flapan AD, Capewell S, MacDonald TM, Neilson JM, Ewing DJ. Decreased cardiac parasympathetic activity in chronic heart failure and its relation to left ventricular function. Br Heart J. 1992 Jun;67(6):482–485. doi: 10.1136/hrt.67.6.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kienzle MG, Ferguson DW, Birkett CL, Myers GA, Berg WJ, Mariano DJ. Clinical, hemodynamic and sympathetic neural correlates of heart rate variability in congestive heart failure. Am J Cardiol. 1992 Mar 15;69(8):761–767. doi: 10.1016/0002-9149(92)90502-p. [DOI] [PubMed] [Google Scholar]
- 13.Bilchick KC, Fetics B, Djoukeng R, et al. Prognostic value of heart rate variability in chronic congestive heart failure (Veterans Affairs’ Survival Trial of Antiarrhythmic Therapy in Congestive Heart Failure) Am J Cardiol. 2002 Jul 1;90(1):24–28. doi: 10.1016/s0002-9149(02)02380-9. [DOI] [PubMed] [Google Scholar]
- 14.La Rovere MT, Pinna GD, Maestri R, et al. Short-term heart rate variability strongly predicts sudden cardiac death in chronic heart failure patients. Circulation. 2003 Feb 4;107(4):565–570. doi: 10.1161/01.cir.0000047275.25795.17. [DOI] [PubMed] [Google Scholar]
- 15.Anastasiou-Nana MI, Terrovitis JV, Athanasoulis T, et al. Prognostic value of iodine-123-metaiodobenzylguanidine myocardial uptake and heart rate variability in chronic congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 2005 Aug 1;96(3):427–431. doi: 10.1016/j.amjcard.2005.03.093. [DOI] [PubMed] [Google Scholar]
- 16.Makikallio TH, Huikuri HV, Makikallio A, et al. Prediction of sudden cardiac death by fractal analysis of heart rate variability in elderly subjects. J Am Coll Cardiol. 2001 Apr;37(5):1395–1402. doi: 10.1016/s0735-1097(01)01171-8. [DOI] [PubMed] [Google Scholar]
- 17.Galinier M, Pathak A, Fourcade J, et al. Depressed low frequency power of heart rate variability as an independent predictor of sudden death in chronic heart failure. Eur Heart J. 2000 Mar;21(6):475–482. doi: 10.1053/euhj.1999.1875. [DOI] [PubMed] [Google Scholar]
- 18.Boveda S, Galinier M, Pathak A, et al. Prognostic value of heart rate variability in time domain analysis in congestive heart failure. J Interv Card Electrophysiol. 2001 Jun;5(2):181–187. doi: 10.1023/a:1011485609838. [DOI] [PubMed] [Google Scholar]
- 19.Villareal RP, Liu BC, Massumi A. Heart rate variability and cardiovascular mortality. Curr Atheroscler Rep. 2002 Mar;4(2):120–127. doi: 10.1007/s11883-002-0035-1. [DOI] [PubMed] [Google Scholar]
- 20.Aronson D, Mittleman MA, Burger AJ. Measures of heart period variability as predictors of mortality in hospitalized patients with decompensated congestive heart failure. Am J Cardiol. 2004 Jan 1;93(1):59–63. doi: 10.1016/j.amjcard.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 21.Makikallio TH, Huikuri HV, Hintze U, et al. Fractal analysis and time- and frequency-domain measures of heart rate variability as predictors of mortality in patients with heart failure. Am J Cardiol. 2001 Jan 15;87(2):178–182. doi: 10.1016/s0002-9149(00)01312-6. [DOI] [PubMed] [Google Scholar]
- 22.Furlan R, Piazza S, Dell’Orto S, et al. Early and late effects of exercise and athletic training on neural mechanisms controlling heart rate. Cardiovasc Res. 1993 Mar;27(3):482–488. doi: 10.1093/cvr/27.3.482. [DOI] [PubMed] [Google Scholar]
- 23.Sandercock GR, Grocott-Mason R, Brodie DA. Changes in short-term measures of heart rate variability after eight weeks of cardiac rehabilitation. Clin Auton Res. 2007 Feb;17(1):39–45. doi: 10.1007/s10286-007-0392-5. [DOI] [PubMed] [Google Scholar]
- 24.Takeyama J, Itoh H, Kato M, et al. Effects of physical training on the recovery of the autonomic nervous activity during exercise after coronary artery bypass grafting: effects of physical training after CABG. Jpn Circ J. 2000 Nov;64(11):809–813. doi: 10.1253/jcj.64.809. [DOI] [PubMed] [Google Scholar]
- 25.Larsen AI, Gjesdal K, Hall C, Aukrust P, Aarsland T, Dickstein K. Effect of exercise training in patients with heart failure: a pilot study on autonomic balance assessed by heart rate variability. Eur J Cardiovasc Prev Rehabil. 2004 Apr;11(2):162–167. doi: 10.1097/01.hjr.0000124214.21584.bb. [DOI] [PubMed] [Google Scholar]
- 26.Selig SE, Carey MF, Menzies DG, et al. Moderate-intensity resistance exercise training in patients with chronic heart failure improves strength, endurance, heart rate variability, and forearm blood flow. J Card Fail. 2004 Feb;10(1):21–30. doi: 10.1016/s1071-9164(03)00583-9. [DOI] [PubMed] [Google Scholar]
- 27.Malfatto G, Branzi G, Riva B, Sala L, Leonetti G, Facchini M. Recovery of cardiac autonomic responsiveness with low-intensity physical training in patients with chronic heart failure. Eur J Heart Fail. 2002 Mar;4(2):159–166. doi: 10.1016/s1388-9842(01)00221-5. [DOI] [PubMed] [Google Scholar]
- 28.Kubinyi A, Bacior B, Szot W, Klecha A, Kawecka-Jaszcz K. [Cardiopulmonary exercise test and heart rate variability in patients with congestive heart failure who underwent physical rehabilitation] Przegl Lek. 2003;60(11):732–736. [PubMed] [Google Scholar]
- 29.Pietila M, Malminiemi K, Vesalainen R, et al. Exercise training in chronic heart failure: beneficial effects on cardiac (11)C-hydroxyephedrine PET, autonomic nervous control, and ventricular repolarization. J Nucl Med. 2002 Jun;43(6):773–779. [PubMed] [Google Scholar]
- 30.Kiilavuori K, Toivonen L, Naveri H, Leinonen H. Reversal of autonomic derangements by physical training in chronic heart failure assessed by heart rate variability. Eur Heart J. 1995 Apr;16(4):490–495. doi: 10.1093/oxfordjournals.eurheartj.a060941. [DOI] [PubMed] [Google Scholar]
- 31.Brubaker PH, Moore JB, Stewart KP, Wesley DJ, Kitzman DW. Endurance exercise training in older patients with heart failure: results from a randomized, controlled, single-blind trial. J Am Geriatr Soc. 2009 Nov;57(11):1982–1989. doi: 10.1111/j.1532-5415.2009.02499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kitzman DW, Brubaker P, Morgan TM, Stewart KP, Little WC. Exercise Training in Older Patients with Heart Failure and Preserved Ejection Fraction: A Randomized, Controlled, Single-Blind Trial. Circ Heart Fail. Sep 17; doi: 10.1161/CIRCHEARTFAILURE.110.958785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Franklin B. WMHE. ACSM’s Guidelines for Exercise Testing and Prescription. Lippincott Williams & Wilkins; Philadelphia: 2000. [Google Scholar]
- 34.Myers J. Principles of exercise prescription for patients with chronic heart failure. Heart Fail Rev. 2008 Feb;13(1):61–68. doi: 10.1007/s10741-007-9051-0. [DOI] [PubMed] [Google Scholar]
- 35.Carter JB, Banister EW, Blaber AP. The effect of age and gender on heart rate variability after endurance training. Med Sci Sports Exerc. 2003 Aug;35(8):1333–1340. doi: 10.1249/01.MSS.0000079046.01763.8F. [DOI] [PubMed] [Google Scholar]
- 36.Chowdhary S, Townend JN. Role of nitric oxide in the regulation of cardiovascular autonomic control. Clin Sci (Lond) 1999 Jul;97(1):5–17. [PubMed] [Google Scholar]
- 37.Kingwell BA. Nitric oxide as a metabolic regulator during exercise: effects of training in health and disease. Clin Exp Pharmacol Physiol. 2000 Apr;27(4):239–250. doi: 10.1046/j.1440-1681.2000.03232.x. [DOI] [PubMed] [Google Scholar]
- 38.Townend JN, al-Ani M, West JN, Littler WA, Coote JH. Modulation of cardiac autonomic control in humans by angiotensin II. Hypertension. 1995 Jun;25(6):1270–1275. doi: 10.1161/01.hyp.25.6.1270. [DOI] [PubMed] [Google Scholar]
- 39.Fagard R, Grauwels R, Groeseneken D, et al. Plasma levels of renin, angiotensin II, and 6-ketoprostaglandin F1 alpha in endurance athletes. J Appl Physiol. 1985 Sep;59(3):947–952. doi: 10.1152/jappl.1985.59.3.947. [DOI] [PubMed] [Google Scholar]
- 40.Ponikowski P, Chua TP, Piepoli M, et al. Ventilatory response to exercise correlates with impaired heart rate variability in patients with chronic congestive heart failure. Am J Cardiol. 1998 Aug 1;82(3):338–344. doi: 10.1016/s0002-9149(98)00303-8. [DOI] [PubMed] [Google Scholar]
- 41.Workman AJ. Cardiac adrenergic control and atrial fibrillation. Naunyn Schmiedebergs Arch Pharmacol. Mar;381(3):235–249. doi: 10.1007/s00210-009-0474-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


