1. DISEASE CHARACTERISTICS
1.1 Name of the disease (synonyms)
Familial hypobetalipoproteinaemia.
1.2 OMIM# of the disease
107730.
1.3 Name of the analysed genes or DNA/chromosome segments
APOB.
1.4 OMIM# of the gene(s)
107730.
1.5 Mutational spectrum
Over 60 mutations have been reported, mostly nonsense and frameshift, occurring throughout the 29 exons of APOB.1, 2, 3 Missense mutations affecting the amino terminal region of the protein have also been described in hypobetalipoproteinemia.4
1.6 Analytical methods
DNA sequencing of genomic-exonic DNA with at least 20-bp of flanking intronic sequence. Western blotting can be used to detect truncated apoB species that are >30% of full-length protein size, to estimate where the mutation occurs within APOB. If Western blotting is negative, sequencing of the 5′ 30% of the gene (exons 1 through 25) is recommended. Where homozygous familial hypobetalipoproteinaemia is suspected and a mutation(s) in APOB cannot be found, consider MTTP sequencing.
1.7 Analytical validation
Where a mutation is identified using bi-directional DNA sequencing, the test is repeated from a fresh dilution of DNA for confirmation. For homozygous familial hypobetalipoproteinaemia, testing of the patient's parents is recommended, to confirm that the two mutations are present in trans (ie, on opposite chromosomes).
1.8 Estimated frequency of the disease
(Incidence at birth (‘birth prevalence') or population prevalence)
1 in 3000 are estimated to carry apoB truncations (heterozygous familial hypobetalipoproteinaemia).5
1.9 If applicable, prevalence in the ethnic group of investigated person
Not applicable.
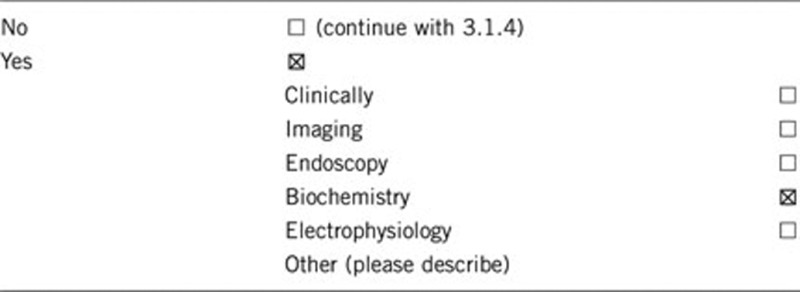
1.10 Diagnostic Setting

Comment: Familial hypobetalipoproteinaemia is primarily a biochemical diagnosis; heterozygotes have apoB levels one-quarter to one-third of normal, whilst in homozygotes apoB is very low or undetectable.
2. Test characteristics
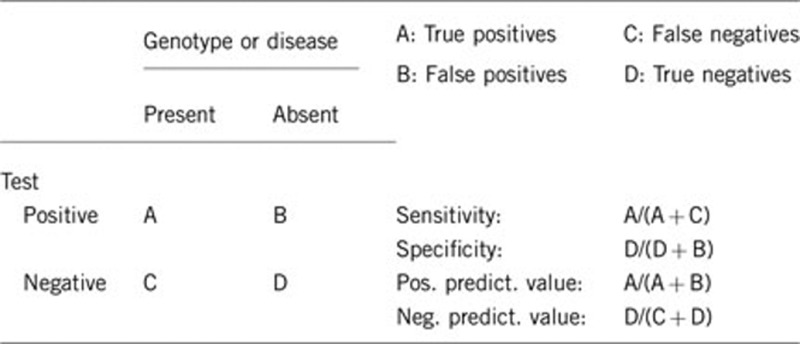
2.1 Analytical sensitivity
(proportion of positive tests if the genotype is present)
Approximately 100%.
2.2 Analytical specificity
(proportion of negative tests if the genotype is not present)
Approximately 100%.
2.3 Clinical sensitivity
(proportion of positive tests if the disease is present)
The clinical sensitivity can be dependent on variable factors such as age or family history. In such cases a general statement should be given, even if a quantification can only be made case by case.
Many factors, such as a strict vegan diet, illness, and high-dose statin therapy, can cause hypobetalipoproteinaemia. The more common secondary causes in the hospital setting include cachexia, malabsorption, malnutrition, severe liver disease and hyperthyroidism. Familial hypobetalipoproteinaemia is characterised by low levels (<5th percentile for age and sex) of plasma apoB-containing lipoproteins.1, 2 It has been suggested that familial hypobetalipoproteinaemia might represent a longevity syndrome and be associated with cardiovascular protection due to resistance to atherosclerosis. Heterozygotes are usually asymptomatic with LDL cholesterol and apolipoprotein (apo) B concentrations approximately one-third of those in normal plasma.
Homozygous famlial hypobetalipoproteinaemia is clinically characterised by the absence of apoB-containing lipoproteins and the clinical features resemble those of abetalipoproteinaemia; fat malabsorption, acanthocytosis, marked hypocholesterolaemia and deficiency of apoB. Most cases are complicated by retinitis pigmentosa, spinocerebellar ataxia and myopathy. Should this constellation of findings be present there are two possibilities, homozygous familial hypobetalipoproteinaemia or abetalipoproteinaemia caused by mutations in MTTP. Family screening is useful in delineating between these conditions, as while obligate heterozygote parents of abetalipoproteinaemia have normal plasma lipid profiles, obligate heterozygous parents of homozygous familial hypobetalipoproteinaemia have one-third plasma concentrations of LDL cholesterol and apoB.
The clinical sensitivity is also dependent on the type of mutation in APOB gene: (i) heterozygotes for apo B truncations shorter than apo B-48 may have fatty liver and a mild intestinal fat malabsorption following high fat intake; (ii) homozygotes for apo B truncations longer than apo B-48 may have a milder phenotype than homozygotes for shorter apo B truncations (whose clinical manifestations are similar to those of ABL); (iii) homozygotes for long truncations (eg, apo B-87) are asymptomatic or have fatty liver.
2.4 Clinical specificity
(proportion of negative tests if the disease is not present)
The clinical specificity can be dependent on variable factors such as age or family history. In such cases a general statement should be given, even if a quantification can only be made case by case.
Approximately 100%.
2.5 Positive clinical predictive value
(life time risk to develop the disease if the test is positive)
100%.
2.6 Negative clinical predictive value
(Probability not to develop the disease if the test is negative)
Assume an increased risk based on family history for a non-affected person. Allelic and locus heterogeneity may need to be considered.
Index case in that family had been tested:
100%.
Index case in that family had not been tested:
Should the constellation of clinical findings be present in an index case, it is possible that they might have abetalipoproteinaemia, rather than homozygous familial hypolipoproteinaemia. Abetalipoproteinaemia patients receive similar treatment advice as homozygous familial hypobetalipoproteinaemia patients. Should the constellation of clinical findings be present in an index case, it is possible that they might have homozygous familial hypobetalipoproteinaemia, rather than abetalipoproteinaemia. Homozygous familial hypobetalipoproteinaemia patients receive similar treatment advice as abetalipoproteinaemia patients. Also, there are even rarer conditions called homozygous proprotein convertase subtilisin/kexin type 9 (PCSK9) deficiency and familial combined hypolipidemia (due to homozygous mutations in angiopoietin-like protein 3, ANGPTL3) that present with extremely low (but not absent) levels of apoB-containing lipoproteins, but no systemic manifestations. To date, there are only a handful of families in the world reported with these latter two genetic conditions.
3. Clinical Utility
3.1 (Differential) diagnosis: The tested person is clinically affected
(To be answered if in 1.10 ‘A' was marked)
3.1.1 Can a diagnosis be made other than through a genetic test?
3.1.2 Describe the burden of alternative diagnostic methods to the patient
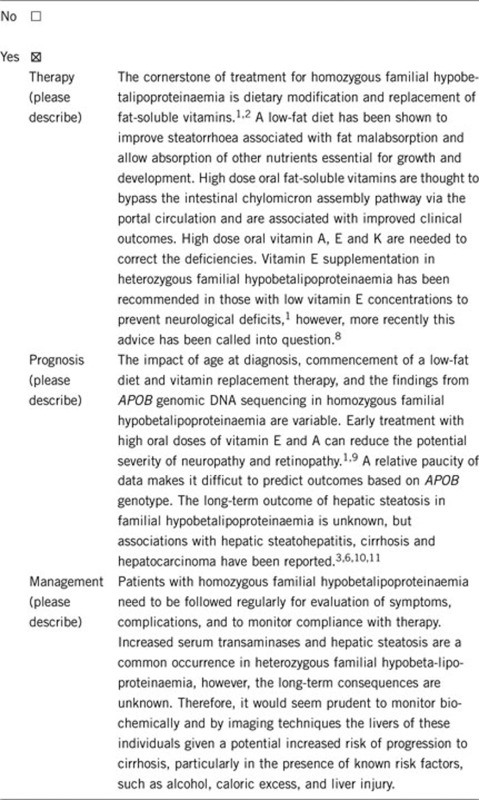
Heterozygotes for familial hypobetalipoproteinaemia are often asymptomatic, but have plasma LDL cholesterol and apoB concentrations that are one-third of normal. Most of them have increased serum transaminases due to hepatic steatosis and sometimes mild fat malabsorption.6, 7 Homozygous familial hypobetalipoproteinaemia is characterised by the absence of plasma apoB-containing lipoproteins with marked hypocholesterolaemia, absence of LDL cholesterol and apoB and low triglyceride concentrations. In addition, increased serum transaminases due to hepatic steatosis, acanthocytosis and fat-soluble vitamin deficiency are found. Homozygous familial hypobetalipoproteinaemia cannot be distinguished from abetalipoproteinaemia clinically.
3.1.3 How is the cost effectiveness of alternative diagnostic methods to be judged?
Not applicable.
3.1.4 Will disease management be influenced by the result of a genetic test?
3.2 Predictive setting: The tested person is clinically unaffected but carries an increased risk based on family history
(To be answered if in 1.10 ‘B' was marked)
3.2.1 Will the result of a genetic test influence lifestyle and prevention?
If the test result is positive (please describe).
If the test result is negative (please describe).
3.2.2 Which options in view of lifestyle and prevention does a person at-risk have if no genetic test has been done (please describe)?
Not applicable.
3.3 Genetic risk assessment in family members of a diseased person
(To be answered if in 1.10 ‘C' was marked)
3.3.1 Does the result of a genetic test resolve the genetic situation in that family?
Not applicable.
3.3.2 Can a genetic test in the index patient save genetic or other tests in family members?
Not applicable.
3.3.3 Does a positive genetic test result in the index patient enable a predictive test in a family member?
Not applicable.
3.4 Prenatal diagnosis
(To be answered if in 1.10 ‘D' was marked)
3.4.1 Does a positive genetic test result in the index patient enable a prenatal diagnosis?
Not applicable.
4. IF APPLICABLE, FURTHER CONSEQUENCES OF TESTING
Please assume that the result of a genetic test has no immediate medical consequences. Is there any evidence that a genetic test is nevertheless useful for the patient or his/her relatives? (Please describe)
Acknowledgments
This work was supported by EuroGentest2 (Unit 2: ‘Genetic testing as part of health care'), a Coordination Action under FP7 (Grant Agreement Number 261469) and the European Society of Human Genetics. RAH is supported by the Jacob J. Wolfe Distinguished Medical Research Chair at the University of Western Ontario, the Edith Schulich Vinet Canada Research Chair in Human Genetics (Tier I), the Martha G. Blackburn Chair in Cardiovascular Research, and operating grants from the CIHR (MOP-13430, MOP-79523, CTP-79853), the Heart and Stroke Foundation of Ontario (NA-6059, T-6018, PRG-4854), the Pfizer Jean Davignon Distinguished Cardiovascular and Metabolic Research Award, and Genome Canada through the Ontario Genomics Institute.
The authors declare no conflict of interest.
References
- Kane JP, Havel RJ.Disorders of the biogenesis and secretion of lipoproteins containing the B apolipoproteinsin Scriver CR, Beaudet AL, Sly WS (eds): The Metabolic and Molecular Bases of Inherited Disease New York: McGraw-Hill; 2001. 8th edn2717–2752. [Google Scholar]
- Hooper AJ, van Bockxmeer FM, Burnett JR. Monogenic hypocholesterolaemic lipid disorders and apolipoprotein B metabolism. Crit Rev Clin Lab Sci. 2005;42:515–545. doi: 10.1080/10408360500295113. [DOI] [PubMed] [Google Scholar]
- Tarugi P, Averna M. Hypobetalipoproteinemia: genetics, biochemistry, and clinical spectrum. Adv Clin Chem. 2011;54:81–107. [PubMed] [Google Scholar]
- Burnett JR, Zhong S, Jiang ZG, et al. Missense mutations in APOB within the betaalpha1 domain of human APOB-100 result in impaired secretion of ApoB and ApoB-containing lipoproteins in familial hypobetalipoproteinemia. J Biol Chem. 2007;282:24270–24283. doi: 10.1074/jbc.M702442200. [DOI] [PubMed] [Google Scholar]
- Welty FK, Lahoz C, Tucker KL, Ordovas JM, Wilson PW, Schaefer EJ. Frequency of apoB and apoE gene mutations as causes of hypobetalipoproteinemia in the Framingham offspring population. Arterioscler Thromb Vasc Biol. 1998;18:1745–1751. doi: 10.1161/01.atv.18.11.1745. [DOI] [PubMed] [Google Scholar]
- Hooper AJ, Adams LA, Burnett JR. Genetic determinants of hepatic steatosis in man. J Lipid Res. 2011;52:593–617. doi: 10.1194/jlr.R008896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonfeld G, Patterson BW, Yablonskiy DA, et al. Fatty liver in familial hypobetalipoproteinemia: triglyceride assembly into VLDL particles is affected by the extent of hepatic steatosis. J Lipid Res. 2003;44:470–478. doi: 10.1194/jlr.M200342-JLR200. [DOI] [PubMed] [Google Scholar]
- Clarke MW, Hooper AJ, Headlam HA, et al. Assessment of tocopherol metabolism and oxidative stress in familial hypobetalipoproteinemia. Clin Chem. 2006;52:1339–1345. doi: 10.1373/clinchem.2006.068692. [DOI] [PubMed] [Google Scholar]
- Chowers I, Banin E, Merin S, et al. Long-term assessment of combined vitamin A and E treatment for the prevention of retinal degeneration in abetalipoproteinaemia and hypobetalipoproteinaemia patients. Eye. 2001;15:525–530. doi: 10.1038/eye.2001.167. [DOI] [PubMed] [Google Scholar]
- Tarugi P, Lonardo A, Ballarini G, et al. A study of fatty liver disease and plasma lipoproteins in a kindred with familial hypobetalipoproteinemia due to a novel truncated form of apolipoprotein B (APO B-54.5) J Hepatol. 2000;33:361–370. doi: 10.1016/s0168-8278(00)80270-6. [DOI] [PubMed] [Google Scholar]
- Lonardo A, Tarugi P, Ballarini G, Bagni A. Familial heterozygous hypobetalipoproteinemia, extrahepatic primary malignancy, and hepatocellular carcinoma. Dig Dis Sci. 1998;43:2489–2492. doi: 10.1023/a:1026646618643. [DOI] [PubMed] [Google Scholar]


