Abstract
Introduction
Medical error is often a traumatic experience not only for patients but also for doctors. However, patients as victims get much more publicity than those responsible for actual errors. The authors of the study conducted research to learn about Polish doctors' opinions on and reactions to medical errors and how they affect their further professional activity and psychological status. The aim of this study was to evaluate the impact of involvement in medical errors of doctors of different specialties and different age.
Material and methods
The research was conducted in a group of 100 doctors of different specialties. Respondents anonymously completed an experimental survey comprising 6 groups of multiple choice questions concerning such issues as awareness of the nature of medical error, legal liability of the perpetrator, consequences of medical error for further professional activity, the function of the Patients' Rights Representative and consequences of publishing the problem.
Results
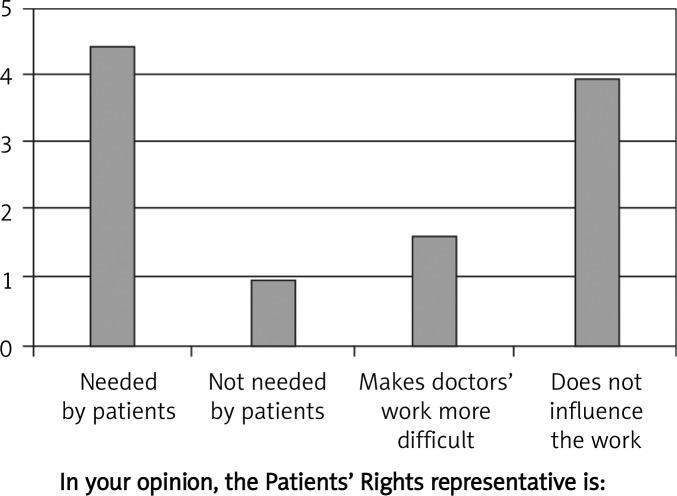
The results indicate many negative effects of medical errors on physicians, such as common fear of making an error (82%), increased caution (52%), disadvantageous security measures while performing one's duties (57%), worsening of doctor-patient relations (67%), loss of social trust (62%) and increased treatment costs (40%). Forty five percent of the surveyed doctors declared that patients need the Patients' Rights Representative and 39% claimed it does not affect their work.
Conclusions
Given the significant burden on physicians' health, well-being and performance associated with medical errors, health care institutions should take this into account and provide physicians with formal systems of support.
Keywords: medical error, physicians, emotional distress, professional support
Introduction
Medical errors are distressing for both patients and doctors alike. There are various effective tools introduced in the healthcare system for their prevention. Some medical protocols and pathways incorporated into medical practice may help in avoiding medical errors [1]. Furthermore, it has been proven that they may act as reminders to reduce distractions in the treatment process [2]. Unfortunately, sometimes the guidance of the protocol is not enough, and an error occurs. Victims’ families point the finger at themselves for not having provided their relatives with enough attention and care, and sufferers consider themselves as an undefined mistake source and think it is them to blame for recklessness. Doctors, just like patients, feel guilty, anxious, hurt, and lonely. Surveys performed on an American population show that medical error perpetrators, once they have committed an error, apart from talking about a sense of loss of reputation and patients’ confidence, and professional satisfaction, also mention continuous fear of committing yet another error and report some symptoms of distress, e.g. sleep disorders [3]. According to Dr Mamta Gautam [4], perpetrators always suffer no matter how serious the error. What is more, doctors compared with other professional groups are by far more burdened with responsibility for someone else's life and health. It is doctors who are most likely to suffer professional burnout resulting in decreased efficiency, exhaustion, depersonalization of relations with colleagues and patients. They often face chronic sleeplessness, headaches, tiredness, anxiety and fear, depression or escape behaviours that all lead to addictions. Professional burnout symptoms may favour medical errors that in turn may increase burnout. Growing awareness of the emotional and professional costs of burnout, as well as costs of medical errors, indicate a necessity to activate medical circles to continuously analyse the above-mentioned occurrences and to develop preventive and remedial programmes. Modern literature focuses more and more often and in greater detail on those who fall victim to medical errors. Yet, it seems that perpetrators-turned-victims of these errors also deserve some attention. To lessen the likelihood of patients falling victims of medical errors it is doctors who should be focused on, helped to tackle the emotional results of errors and face the consequences thereof, be enabled to continue and lead a fully-fledged professional life. Doctors should also be given a chance to freely express their opinions on this sensitive issue.
Cooperating teams of the Department of Endocrinology, Metabolism and Internal Diseases and the Faculty of Health Sciences launched research to learn about Polish doctors’ opinions on and reactions to medical errors and how they affect their further professional activity and psychological status.
Material and methods
A hundred doctors of different specialities, 25-56 years of age with different job seniorities (0-40 years) were asked to anonymously complete an experimental survey comprising 6 groups of multiple choice questions. The questions concerned such issues as awareness of the nature of medical error, legal liability of the perpetrator, consequences of medical error for further professional activity, the function of the Patients’ Rights Representative and consequences of publicising the problem.
Seventy women and 30 men at 29-60 years of age comprised the researched cohort. Job seniority was divided according to 5 time ranges into groups of which each included an approximately similar number of doctors. The smallest group was the one comprising doctors with the longest job seniority, 31-40 years (Table I).
Table I.
Characteristics of the research cohort of doctors
| Sex | Age [years] | Job seniority | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| F | M | 18-30 | 31-40 | 41-50 | 51-60 | 0-5 | 6-10 | 11-20 | 21-30 | 31-40 |
| 70 | 30 | 18 | 40 | 22 | 20 | 24 | 18 | 20 | 28 | 10 |
Results
The results depicted in percentages indicate a high level of agreement in doctors’ opinions on medical errors and social consequences thereof.
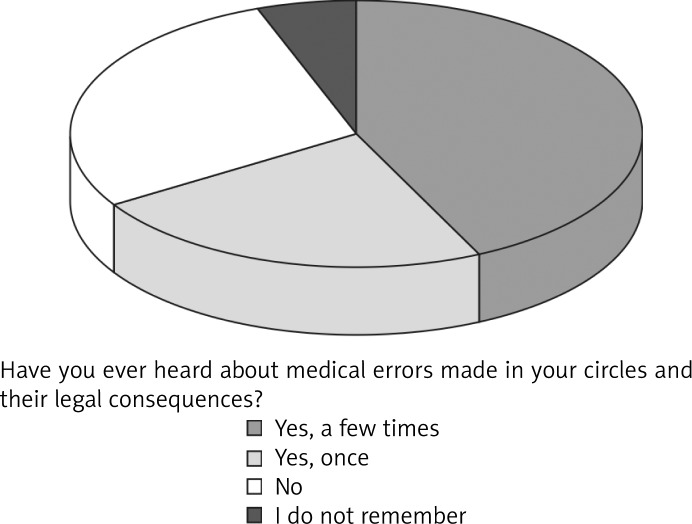
Admittedly, 1/3 of the surveyed doctors had not heard of medical error cases that might have occurred in their circles and legal consequences thereof. Yet, far more of them (64%) had personally come across the phenomenon and only 7% could recall the fact (Figure 1).
Figure 1.
The knowledge of doctors about medical errors made in their circles and their legal consequences
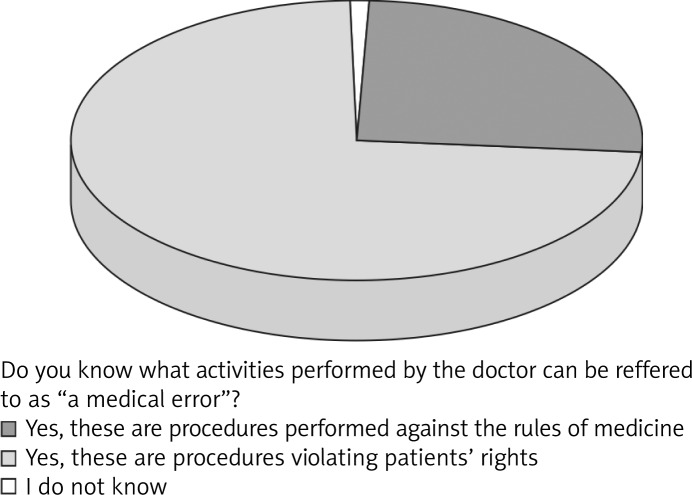
A majority of the study group (78%) unanimously defined a medical error as resulting from a procedure managed not according to the rules of medical conduct. A minority, i.e. 20%, opined that not only is the performance of such errors against the rules of medical conduct but it also impinges the patient's rights (Figure 2).
Figure 2.
The knowledge of doctors about activities referred to as “a medical error”
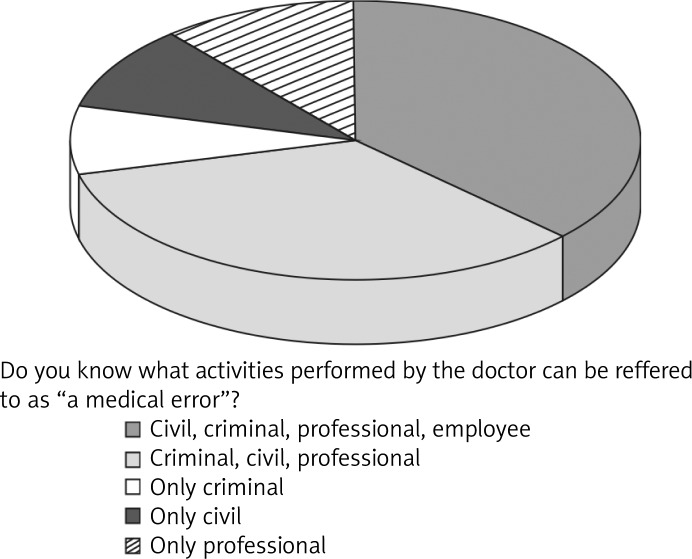
There were far more opinions among the surveyed doctors on legal liability taken on by error perpetrators. Thirty nine percent of the surveyed subjects thought that the doctor is to take on criminal, civil, disciplinary and professional liability; 31% thought that it should be criminal, civil and professional liability; and 10% each believed that doctors should face only criminal, professional, or civil liability (Figure 3).
Figure 3.
The knowledge of doctors about medical error legal liability
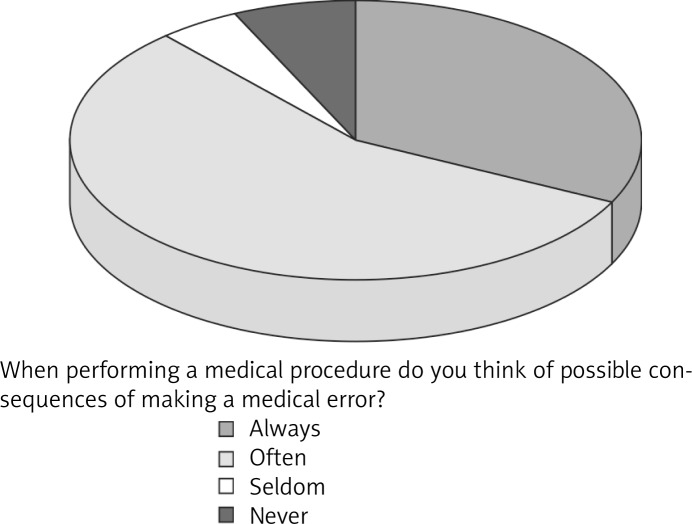
It was interesting to see how a threat of committing a medical error may influence one's professional work: a thought of possible consequences of a medical error accompanied half of the respondents (50%) while performing their duties, as many as 1/3 (32%) of the group had always been thinking about possible medical errors while performing their duties, and 10% could not interchangeably define the fact (Figure 4).
Figure 4.
Doctors’ opinions on awareness of legal liability impact of medical errors on being more cautious in the work
About half of the surveyed (52%) confirmed that being aware of legal liability for medical errors raises the level of caution at work. 1/3 (34%) admitted trying to avoid performing certain procedures, 1/3 (29%) far more often consulted taking any decisions with their colleagues, and 1/3 (28%) needed more time to ponder before arriving at a definite diagnosis or decision about a form of treatment. Only 9% of the surveyed doctors confirmed that being aware of legal liability for committing a medical error affected neither their emotions nor professional duties (Table II).
Table II.
Influence of knowledge of legal liability for medical error on practice
| Does awareness of legal liability for medical error influence your professional practice? | % |
|---|---|
| Yes, I'm more careful | 52 |
| Yes, I avoid some actions | 34 |
| I often consult decisions with colleagues | 29 |
| I need more time to think before deciding on the diagnosis and therapy | 28 |
| Awareness of legal liability for medical errors has no effect on my actions | 9 |
According to a majority of respondents, publicity of medical errors committed by doctors has negative social consequences. Sixty seven percent claim this sort of publicity aggravates doctor–patient relations, 62% say this may lead to an increase in patients’ mistrust towards doctors, and 40% think it increases treatment costs since doctors are more willing to perform some extra, not always essential, preventive procedures. Smaller groups comprising 20% of respondents each pointed to the subsequent follow-ups of the issue publicity: encouragement of greater carefulness, being discouraged from choosing medicine as a career path, and restraining doctors from making risky decisions even if they are essential for the course of treatment. Twenty three percent of the surveyed doctors claimed that publicity about medical errors significantly decreases patients’ sense of safety and 11% pointed to a constructive effect of publicity on patients’ sense of safety (Table III).
Table III.
Doctors’ opinions on the effects of public information about medical errors they made
| Effects of public information about medical errors | % |
|---|---|
| Make relations between doctors and patients worse | 67 |
| Increases the mistrust between patients and doctors | 62 |
| Increases medical costs by taking not always necessary preventive procedures | 40 |
| Encourages doctors to take greater care | 21 |
| Discourages the selection of the medical profession | 19 |
| Discourages risky decisions despite importance for the effects of treatment | 20 |
| Reduces the sense of safety for patients | 23 |
| Has a positive effect on sense of safety for patients | 11 |
The Patients’ Rights Representative is an establishment that is very much occupied with proceedings against medical errors. According to half (45%) of the surveyed doctors, patients need the Patients’ Rights Representative, approximately the same number of doctors (39%) claimed it does not affect their work, and as many as 16% believe it makes it more difficult for the doctors to perform their duties (Figure 5).
Figure 5.
The opinion of doctors on Patients’ Rights Representative
Discussion
The professional responsibility that doctors face because of their daily duties places this professional group at the top of the hierarchy of professional and ethical requirements. Considering the above it is obvious that professional burnout poses a still existing threat for medical circles. It also directly relates to the phenomenon of medical errors. It has been scientifically proved that apart from situational determinants there exist certain personality traits that predispose an individual to suffer professional burnout. One such trait is obsessive-compulsive behaviour patterns that at first might be associated with being meticulous, which on the one hand might be an adaptive behaviour that may prove advantageous in the course of medical education, and yet on the other hand may interfere with private and professional life. Accompanying remorse, continuous doubts and over-responsibility may result in a chronic sense of not being engaged enough or lacking competence, or lacking skill to set limits, which altogether collide with professional satisfaction and ability to take care of one's own affairs. Discrepancies between being aware of one's own emotional and physical needs leads to a destructive effect of being overworked which in turn falls short of committing a medical error. Any medical malpractice may consequently result in distress-related serious health problems that hinder performing professional duties. Although many authors of medical studies have confirmed the importance of medical errors, they still first of all focus on the patient. The way medical errors affect doctors’ health and functioning is yet to have been researched and focused on. Nonetheless, seemingly it is doctors who should be looked after and their situation and problem that should be tackled when fighting the phenomenon. Although discussions about the importance of doctors being overworked and underslept have been unceasing, the medical professionals are always regarded as perpetrators. Luckily there have appeared some reports describing medical error perpetrators as ‘secondary victims’, which is to indicate not only the emotional damage they sustain but also the unintentional nature of the deed or even opposite, good intent thereof [5]. Having made an error a doctor may react with distress, self-doubt, a sense of loss of self, fear or depression and shame that linger for a long time, predisposing a doctor to professional burnout that in turn, following a vicious circle, promotes the foregoing.
No-harm policy is another aspect of discussing medical errors. It should be considered that beside direct negative effects on the patient's health, unreasonable restriction and punishment of doctors may have effects against the patient's welfare. Decreased doctors' self-efficacy results in reducing their competency in treating health problems and negatively affects their decisions. Thus, it seems that a doctor's mistake and its further consequences harm not only the patient, but also the physician.
Therefore it is high time to consider structured and institutionalised support for doctors as a professional group often stigmatised by the media. Not only should they receive legal support but they should also be provided with professional support similar to that experienced by those who participate in various critical situations, clearly defined procedures of handling wronged patients so that they could carry on their professional existence. It is very important that doctors themselves feel motivated to accept this sort of help and could recognise its value and usefulness. According to studies carried out by Waterman, only 18% of doctors out of 86% interested ones decided to take part in training courses on the issue of medical errors. There exist barriers formed by doctors being able neither to acknowledge professional handicap nor to cross the border of social shame [6]. The required repair and preventive programmes should be devised by specialists, e.g. doctors of different specialities, psychologists, managers, lawyers, or even priests, to counteract the results of medical errors and to support ‘secondary victims’ thereof. To tailor programmes best matching doctors’ needs such undertakings should be supported by some scientific research [7]. Analyses of an American population provided very important information on local doctors’ point of view. Seventy seven percent of American doctors thought that lack of dialogue is a vital traumatic factor of committing medical errors, 56% claimed that a possibility to discuss an error with co-workers would improve the doctors’ comfort, and 70% said that apologising to the patient would not mean facing and handling responsibility. To devise preventive programmes based on some anonymous surveys on doctors’ opinions on the issue it is also worth considering medical errors committed by Polish doctors and their opinions on the problem. Our surveys revealed that doctors show no unanimous understanding of ‘medical error’. It has been proved that although the phenomenon of medical malpractice is encountered quite often in medical circles (70% of doctors), there are numerous discrepancies as to its exact definition. Although everyone considers it a practice against all rules of medical conduct there is only a very small group that views it as impinging on some patients’ rights, e.g. the right to receive medical services in accordance with current medical knowledge. Lack of unanimity is also apparent as far as perpetrators’ legal liability is concerned and gives evidence of not being properly informed or not being either willing or motivated to acknowledge the fact.
It is in doctors’ interests to acknowledge that making a medical error may result in various legal liabilities; this sort of awareness should be based on specific and useful information. The type of liability will always depend on the nature of the legal relation on the basis of which the work contract has been concluded. If the patient has been awarded any legal compensation or redress in the course of a suit, doctors working under a contract of employment are accountable for inflicted damage according to the rules of reciprocal responsibility between employer and employee. In accordance with the above the employer (a health service institution) may reimburse their employee (a doctor) for the costs they have incurred because of the medical error; the reimbursement, however, cannot exceed three monthly salaries. Only if a mistake has been made purposefully is the employer entitled to complete reimbursement. If a doctor is employed under civil law or as an individual or group practice, it is the doctor personally who is responsible. Furthermore, should the deed be indicative of crime, the doctor is to face criminal responsibility. Doctors should bear in mind that if the procedures were made against medical and ethical conduct, and regardless of suits in common plea courts, they may also be punished by medical courts. Familiarity with possibilities and rules of legal suits brought against doctors may raise awareness and care of performed procedures that in turn may lead to diminished levels of stress and fewer doubts, resulting in fewer medical errors.
Still, doctors are unanimous as to the negative influence of medical errors on the psychology of perpetrators thereof, work comfort and quality, as well as the devastating effects of the publicity these errors receive. All these doubtlessly confirm the traumatic effects that these phenomena have on doctors’ overall professional efficiency and patients’ safety.
How to tackle such a sensitive issue if at the same time legal requirements have to be considered, ethical standards have to be met, quality of medical services should remain the same, and doctors’ health and work comfort should be protected? One suggestion put forward is to focus on promoting health and comfort at all levels – physical, emotional, and spiritual – starting at the very beginning of medical studies and finishing with retirement. This is a challenge to be met not only by doctors themselves but also by related professionals and organisations that in one way or another influence doctors in performing their duties. To be safe for patients, doctors themselves must feel safe performing their duties and in the environment they find themselves. Social and environmental support and professional support as well as excellent training, good working conditions and security in case of failure or error that are very likely to be faced or committed by such a complicated creature as a human being are all indispensable conditions to be met and to become thoroughly and precisely prepared for. Development of tools for error prevention and forming a culture that accepts the imperfection of human performance should be important aims for healthcare [8].
Doctors do require actual assistance to deal with a threat of possible error. They need training in the area of dealing with stress once an error has been made, and they also have to learn how to react to an error committed by themselves or their colleagues and where to seek help and support when confronted with an error and a victim thereof, the patient. There still exist gaps in the literature on the subject of effective doctor-patient communication in the difficult circumstances of medical errors. Although since 2001 it has been a common practice accepted by the accreditation committee for health care to inform the patient about anticipated and unforeseen results of a procedure, it has been applied in very few cases. The reason behind this is related not only to doctors’ responsibility but also their fear resulting from patients’ and their families’ reaction and no ability to communicate with them properly [9]. Providing crucial information, e.g. on the subject of medical error victims’ needs and expectations, may allow doctors to develop and cultivate good relations with their patients as well as ensure a sense of security and professional competence and thus make it possible to launch any repair activities. Health care institutions and managers thereof are the ones to get to grips with the task. Their main assumption should be to devise research and educational programmes aiming at arranging formal and professional support for the doctors. Numerous publications containing research results will be exceptionally informative as well as educational and thus may decrease existing tension in medical circles, and among doctors it may raise the level of awareness, knowledge and a sense of confidence in undertaking any actions.
In conclusion, results of anonymous surveys on medical errors carried out among doctors indicate the following: ambiguous understanding of medical error entity, very little awareness of liability for medical error, common and destructive presence of fear of making an error while at work, effect of fear of making an error on increased caution and disadvantageous security measures undertaken while performing one's duties, no sense of support provided by legal or social institutions, harmful influence of medical error publicity resulting in worsening of doctor–patient relations, loss of social trust and increased treatment costs. Because of one-sidedly destructive effect of medical errors on doctors’ psyche and professional capability it is advisable to take probable perpetrators into institutionalised and professional care. Creating an organizational culture that beside development of the tools for error prevention accepts the imperfection of human performance seems to be crucial for both patients’ and doctors’ welfare.
References
- 1.Cox PM, Jr, D'Amato S, Tillotson DJ. Reducing medication errors. Am J Med Qual. 2001;16:81–6. doi: 10.1177/106286060101600302. [DOI] [PubMed] [Google Scholar]
- 2.Pape TM, Guerra DM, Muzquiz M, et al. Innovative approaches to reducing nurses' distractions during medication administration. J Contin Educ Nurs. 2005;36:108–16. doi: 10.3928/0022-0124-20050501-08. [DOI] [PubMed] [Google Scholar]
- 3.Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33:467–76. doi: 10.1016/s1553-7250(07)33050-x. [DOI] [PubMed] [Google Scholar]
- 4.Spickard A, Gabbe SG, Christensen JF. Before burnout: how physicians can defuse stress. JAMA. 2002;288:1447–50. doi: 10.1001/jama.288.12.1447. [DOI] [PubMed] [Google Scholar]
- 5.Waterman A. Impact of medical errors on physicians by Christopher Guadagnino. 2007. Oct, available at: www.physiciansnews.com.
- 6.Gallaugher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients’ and physicians’ attitudes regarding the disclosure of medical errors. JAMA. 2003;289:1001–7. doi: 10.1001/jama.289.8.1001. [DOI] [PubMed] [Google Scholar]
- 7.Pennachio, Dorothy L. To err is human: How to prevent medical errors. Patient Care. 2001;35:95. [Google Scholar]
- 8.Dennison RD. Creating an organizational culture for medication safety. Nurs Clin North Am. 2005;40:1–23. doi: 10.1016/j.cnur.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Gallagner TH, Hardy LM. Should we disclose harmful medical errors to patients? If so how? J Com. 2005;5:253–9. [Google Scholar]