Abstract
Purpose
The role of serum AMH levels in prediction of ovarian response in idiopathic hypogonadotropic hypogonadism (IHH) was evaluated.
Material method(s)
Twelve patients with IHH underwent controlled ovarian hyperstimulation (COH) for IVF were enrolled in this prospective study. Serum AMH levels were studied on the 2nd or 3rd day of an induced menstrual cycle by a preceding low-dose oral contraceptive pill treatment. A fixed dose (150–300 IU/day) of hMG was given in all COH cycles. Correlations between serum AMH levels, COH outcomes and embryological data were investigated.
Results
Mean serum AMH levels was 3.47 ± 2.15 ng/mL and mean serum peak estradiol was 2196 ± 1705 pg/mL. Mean number of follicles >14 mm, >17 mm on hCG day and MII oocytes were 4.14 ± 3.2, 4 ± 2.5 and 7.28 ± 3.5, respectively. Mean number of grade A embryos and transferred embryos were 3.28 ± 2.4 and 2.5 ± 0.7, respectively. The clinical pregnancy rate per patient was 41.6 % (5/12). Positive correlations were observed between serum AMH levels and MII oocytes (r = 0.84), grade A embryos (r = 0.85), serum peak estradiol levels (r = 0.87), and number of follicles >14 mm (r = 0.83) and >17 mm (r = 0.81) on hCG day, respectively.
Conclusion
AMH appears as a promising marker of ovarian response in patients with IHH undergoing IVF.
Keywords: Anti-Mullerian hormone, Hypogonadotropic hypogonadism, Ovarian reserve, Ovarian response, IVF outcome
Introduction
Idiopathic hypogonadotropic hypogonadism (IHH) is the most common cause of hypogonadism that mainly refer to congenital deficiency of GnRH secretion or abnormal function of the hypothalamic-pituitary-ovarian axis [17]. The clinical presentation of IHH could either be related with primary amenorrhea or with delayed puberty in association with small ovaries comprising a large cohort of arrested follicles. Gonadotropin levels may be undetectable or apparently normal; however serum gonadotropin levels are generally below physiologic levels [4]. Anosmia, cleft lip/cleft palate and/or syndactyly are other findings that may accompany IHH. Patients with this disorder, defined also as Group I according to World Health Organization (WHO Group I), are apparently the exact candidates for ovulation induction with exogenous gonadotropins [23, 25]. Ovulation can be successfully induced with small doses of menotropins. The conventional procedure is to start ovulation induction with lower daily doses of human menopausal gonadotropins (hMG), while defining the effective threshold of ovarian response in order to prevent the complications associated with COH ([19, 20]). Alternatively, use of GnRH agonists in a pulsatile manner can also induce ovulation in such patients.
There has been an increasing interest in minimal or mild ovarian stimulation protocols in recent years. Accordingly, determining ovarian response or ovarian reserve is crucial in modern reproductive medicine in order to achieve acceptable pregnancy rates with minimal side effects. However, assessment of ovarian response in patients with IHH is challenging as these patients frequently have amenorrhea or irregular menstrual cycles with small ovaries making most of the classical ovarian reserve markers unreliable. Antral follicle count (AFC), basal serum FSH, LH or estradiol and ovarian response to previous COH are common parameters guiding clinicians in planning or controlling a COH cycle. In this unique patient population AFC is technically subjective due to non-ovulation or disrupted gametogenesis, and assessment of serum FSH and/or estradiol is unreliable. Despite the well-known concept that most of these patients respond well to menotropins, predicting ovarian response is still crucial to avoid ovarian hyperstimulation in a high responder patient or to achieve a favorable COH outcome in a poor responder patient [9]
AMH is mainly expressed by granulosa cells of early antral and pre-antral follicles [2, 26], where its expression is already initiated by the smallest growing follicles. Over the last decade, many prospective studies have been evaluated the plausible role of AMH in predicting both quantitative and qualitative ovarian response in assisted reproductive technologies (ART) [8]. Consequently, several groups have addressed serum levels of AMH as a novel and superior clinical marker of ovarian reserve and/or ovarian response compared with conventional markers [13]. Owing to the unique advantages of AMH, the primary objective of this preliminary study is to investigate the accuracy of serum AMH levels in predicting ovarian response prior to COH in IVF cycles, and as a secondary outcome to assess the correlation between serum AMH levels and COH outcomes including embryological data in a cohort of IHH patients.
Materials and methods
Twelve patients diagnosed with IHH were enrolled to this study who were scheduled to undergo COH for IVF between 2007 and 2010 at the University of Ankara-Center for Research on Human Reproduction. IHH was diagnosed before the age of 18 by exclusion of other possible acquired etiologies along with low endogen gonadotropin levels (<4–5 IU/L) and low estradiol levels (<20 pg/mL or <73 pmol/L), [19, 20]. All patients had normal serum thyroid-stimulating hormone (TSH), prolactin and testosterone concentrations. A possible pituitary lesion was excluded either by sella MRI or by computerized tomography in all patients prior to study as a part of routine diagnostic work up. Relatively small sized ovaries and thin endometrium was confirmed with trans-vaginal ultrasound (TV-USG). Other developmental statuses were normal in all patients, except irregular menstruation or amenorrhea. At least 2 repeated unsuccessful intrauterine insemination attempts had been carried out previously in all patients before undergoing IVF. COH was initiated using human menopausal gonadotropins (hMG) (Menogon, Ferring Pharmaceuticals, Turkey) that have been applied on the 2nd or 3rd day of an induced menstrual cycle following a preceding low-dose oral contraceptive pill (OCP). Menotropin doses ranged between 150 and 300 IU/day according to the patient’s age, body mass index (BMI) and prior ovarian response to IUI/IVF cycles. Serum samples for AMH, FSH, LH and estradiol were collected on the 2nd or 3rd day of a low-dose OCP induced menstrual cycle. All collected serum samples were stored at −20 °C. Follicular response was followed with serial ultrasound examinations and serum estradiol assessments. Final oocyte maturation was induced by 10,000 IU human chorionic gonadotropin (hCG) when at least two follicles reached 18 mm in diameter and trans-vaginal ultrasound-guided oocyte retrieval was performed 36 h later. On days 3 or 5 after oocyte retrieval, depending on the number of good quality embryos, a total of 1–3 embryos were transferred into the uterine cavity under the ultrasound guidance with a flexible catheter (Wallace; Irvine Scientific, Santa Ana, CA). Embryo scoring was performed as described previously [5]. Total number of oocytes was defined as the total number of oocytes collected at oocyte pick-up. Metaphase II oocytes was defined as oocytes extruded its first polar body. Luteal phase support was achieved by using daily intra-muscular injections of micronized progesterone (100 mg) and estradiol hemihydrate (4 mg, d.i.b.) starting on the day after oocyte retrieval, and continued until pregnancy test. When pregnancy occurred vaginal micronized progesterone (Progestan, Kocak Farma, Turkey) 600 mg daily was continued until 12th week of gestation. Pregnancy was confirmed by a positive blood test for β-hCG assay 12 days after the embryo transfer.
Serum AMH levels were assessed using the Beckman Coulter enzyme-linked immune-sorbent assay (ELISA) kit according to the manufacturer manual [DSL Active® MIS/AMH ELISA kit, Ref. no DSL-10-14400, Webster-USA]. Detection range of the kit is between 0.05 and 15 ng/mL. All available data were transferred to SPSS (SPSS for Windows 9.0; SPSS Inc., Chicago, IL, USA). Pearson’s correlation coefficient was used to determine relationships between serum AMH levels, COH outcome and embryological data. All participants signed a written informed consent and the study was approved by the local ethical committee.
Results
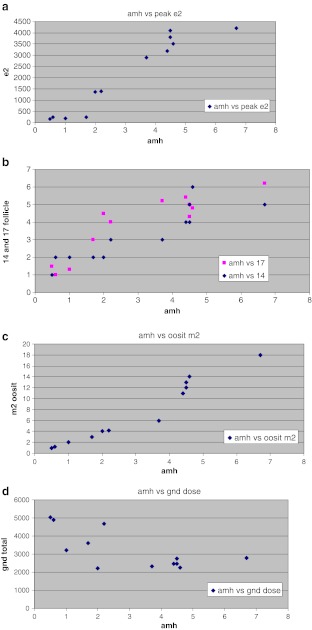
IVF cycle characteristics, outcome measures and AMH levels of 12 IHH patients were evaluated and demonstrated in the Table 1. Mean serum peak estradiol was 2196 ± 1705 pg/mL and serum AMH was 3.47 ± 2.15 ng/mL. There were strong positive correlations between serum AMH levels and serum peak estradiol levels (r = 0.87, p = 0.001), number of follicles >14 mm (r = 0.83, p = 0.003) and >17 mm (r = 0.81, p = 0.003) on hCG day, MII oocytes retrieved (r = 0.84, p = 0.002), and grade A embryos were generated (r = 0.85, p = 0.002) (Fig. 1a, b, c and Table 2). A weak negative correlation was detected between serum AMH levels and total gonadotropin dose (r = −0.69, p = 0.0506), (Fig. 1d and Table 1). In the majority of cases, antral follicle assessment was ineffective due to small ovaries and suboptimal assessment of ovarian follicles, so the correlation between serum AMH and AFC couldn’t have been evaluated in the study.
Table 1.
Characteristics and cycle outcomes of the patients
| Mean values | n = 12 patients |
|---|---|
| Age (years) | 28.18 ± 3.5 |
| BMI (kg/m2) | 26.3 ± 2.7 |
| FSH (IU/L) | 0.6 ± 0.3 |
| LH (IU/L) | 0.3 ± 0.2 |
| E2 (pg/mL) | 14 ± 4.9 |
| Peak E2 (pg/mL) | 2196 ± 1705 |
| AMH (ng/mL) | 3.47 ± 2.15 |
| Cumulative gonadotropin dose (IU) | 3227 ± 1069 |
| Follicles >14 mm on hCG day (#) | 4.14 ± 3.2 |
| Follicles >17 mm on hCG day (#) | 4 ± 2.5 |
| MII Oocytes retrieved (#) | 7.28 ± 3.5 |
| Grade A embryos (#) | 3.28 ± 2.4 |
| Embryos transferred (#) | 2.5 ± 0.7 |
| Clinical pregnancy rate % per patient | 41.6 |
Fig. 1.
a, b, c, d Correlation between serum AMH levels and peak serum estradiol, number of follicles >14–17 mm on hCG day, MII oocytes, and cumulative gonadotropin dose. a Serum AMH levels and peak serum estradiol levels. b Serum AMH levels and follicles >14–17 mm on hCG day. c Serum AMH levels and number of MII oocytes. d Serum AMH levels and cumulative gonadotropin dose
Table 2.
Correlations between serum AMH levels, and COH outcome parameters and embryologic data
| AMH | Serum Peak E2 | MII oocytes | hCG day | Total hMG Dose | Grade A embryos | |
|---|---|---|---|---|---|---|
| Follicle >14 mm | Follicle >17 mm | |||||
| r | 0,8766 | 0,8395 | 0,8287 | 0,8142 | −0,6918 | 0,8516 |
| p value | 0.001 | 0.002 | 0.003 | 0.003 | 0.0506 | 0.002 |
r, Pearson Correlation Efficient
p value, calculated by student T-test spearman’s rank correlation coefficient
A p value <0.05 was accepted as statistically important
E2, estradiol
hCG, Human Chorionic Gonadotropin
Discussion
The present study demonstrated that serum AMH may be a good predictor of ovarian response in IHH patients. Significant correlations were found between serum AMH and peak serum estradiol, number of follicles >14–17 mm on hCG day, number of MII oocytes, number of top quality embryos and cumulative gonadotropin dose used. Since IHH patients are potentially fertile and respond very well to exogenous gonadotropins, assessment of ovarian reserve or prediction of COH response is of outmost importance either to predict cycle outcomes or to prevent possible COH associated complications [25]. In this context, the results of the current study are important in two different aspects. First, to our knowledge, this is the first study that demonstrates the correlation between serum AMH levels and COH outcome in IHH patients. Second, serum AMH levels are not found to be totally suppressed in this group, supporting that AMH is secreted before the gonadotropin-dependent follicular stages and has a potential role in initial follicle recruitment serving as a paracrine regulator of early follicle growth.
Similar to IHH patients the endogenous serum gonadotropins are suppressed in patients receiving OCP, however many pre-antral and antral follicles are detectable in this group. In this respect, various results have been reported regarding the impact of steroid suppression on serum AMH levels. Some studies reported null effect of OCP treatment on serum AMH levels [18, 21, 22], whereas others revealed suppressed AMH levels in normal cycling women pretreated with OCP [1, 15]. In a recent case report it was demonstrated that during 16 week course of menotropin treatment both serum AMH and AFC increased in an IHH patient. Authors speculated that, the increase in serum AMH was due to stimulation and growth of FSH-dependent follicles [24]. Beyond conflicting reports, in the current study, serum AMH levels were found as not totally suppressed in IHH patients with a mean serum level of 3.03 ± 1.9 ng/ml and ranging between 0.5 and 7.0 ng/ml. Our result are in accordance with the previous data, which revealed that AMH is highly expressed and secreted by pre-antral and small antral follicles that are up to 2–4 mm of diameter which cannot be easily detected by ultrasound [26]. Neither primordial follicles nor the antral follicles that are greater than 8 mm diameter are believed to not express AMH.
Before scheduling an IVF cycle in IHH patients, using classical markers of ovarian reserve are generally impractical to predict COH response, so novel markers are definitely required to prevent COH associated complications. Accumulated evidence showed that serum AMH levels reflect the size of the follicle cohort and well correlate with the number of oocytes retrieved, peak serum estradiol level and gonadotropin consumption [6, 12]. Nelson et al. demonstrated that circulating AMH can be used to individualize treatment strategies for COH which leads reduced clinical risk and optimized treatment burden [14]. In a donor study, measurement of AMH was found to be a strong predictor of gonadotropin sensitivity, which helps physicians to predict hyper-response that is associated with ovarian hyperstimulation [12]. Similarly, Riggs et al. [16] reported that AMH was found to be superior to other biomarkers of ovarian reserve to predict either low or high response among young women that were selected as oocyte donors. Authors also concluded that serum AMH levels well correlated with embryo morphology and pregnancy outcome in the recipient population [16]. Recently, Majumder et al. [11] found that both AMH levels and AFC were comparable predictors of the number of oocytes retrieved, number of oocytes fertilized, and the number of top quality embryos available for transfer or to be frozen. Furthermore, authors decided that AMH performed better than AFC with regard to live birth [11]. In another interesting study, AMH was found superior to basal FSH and AFC, and had the potential to predict patient’s ovarian response to COH while helping to reduce iatrogenic complications of COH [13]. In that study, AMH was also considered as a better predictor than FSH but not AFC especially for poor response. In a recent meta-analysis that assessed the accuracy of AMH and AFC as predictors of an excessive response in IVF/ICSI cycles, sensitivity and specificity rates for AMH were found as 82 and 76 %, and for AFC were 82 and 80 %, respectively. Investigators concluded that both AMH and AFC are accurate predictors of excessive response and both tests appear to have clinical value [3]. Luisi et al. [10] more recently showed that secretion of AMH is not influenced by the hypothalamic-ovarian axis activity and is not impaired in hypothalamic amenorrhea. These data also indirectly supports that AMH can also be an excellent marker of ovarian reserve in neuroendocrine forms of amenorrhea [10].
Even though both AMH and AFC appear as good predictors of ovarian reserve; AMH may be superior in this specific group of patients mainly due to 2 reasons: first, AMH seems superior compared to AFC in prediction of hyper response which is extremely important in WHO group I patients with a high ovarian reserve [13]; second, in case of poor ovarian reserve, which can also occur in IHH patients, relying on AFC assessment when scheduling a COH cycle can lead to diagnostic confusions due to long existing small ovaries that make AFC assessment technically impractical [7, 8].
In summary, as is well known, current study demonstrated that gonadotropin independent ovarian follicles up to 4 mm in diameter act as the main source of AMH, based on the finding that serum AMH levels are not totally suppressed in IHH patients. Moreover strong correlations between AMH and COH outcome were observed, and this may guide physicians in adjusting gonadotropin doses before scheduling a COH cycle to avoid associated complications. However, it should be underlined that the correlation between the numbers of top quality embryos and serum AMH levels can be due to the high number of MII oocytes retrieved in this young population. Despite the low number of the subjects enrolled could be a limitation, findings of the current study may be important since it is first to assess AMH among IHH patients. Furthermore designing a study consisting of a large number of patients having such a rare clinical condition is somehow challenging and obviously larger studies are required. As a conclusion, assessment of serum AMH level seems as a promising marker of ovarian response in IHH patients undergoing IVF/ICSI. Since response to gonadotropin stimulation could be either excessive or insufficient in such individuals, assessment of ovarian reserve and prediction of COH response is of outmost importance.
Acknowledgments
Disclosure statement
There are no financial or commercial interests to declare regarding the authors of the study.
Footnotes
Capsule
AMH correlates with ovarian response in patients with idiopathic hypogonadotropic hypogonadism.
References
- 1.Arbo E, Vetori DV, Jimenez MF, Freitas FM, Lemos N, Cunha-Filho JS. Serum anti-mullerian hormone levels and follicular cohort characteristics after pituitary suppression in the late luteal phase with oral contraceptive pills. Hum Reprod. 2007;22(12):3192–3196. doi: 10.1093/humrep/dem258. [DOI] [PubMed] [Google Scholar]
- 2.Baarends WM, Uilenbroek JT, Kramer P, Hoogerbrugge JW, Leeuwen EC, Themmen AP, et al. Anti-müllerian hormone and anti-müllerian hormone type II receptor messenger ribonucleic acid expression in rat ovaries during postnatal development, the estrous cycle, and gonadotropin-induced follicle growth. Endocrinology. 1995;136:4951–4962. doi: 10.1210/en.136.11.4951. [DOI] [PubMed] [Google Scholar]
- 3.Broer SL, Dolleman M, Opmeer BC, Fauser BC, Mol BW, Broekmans FJ. AMH and AFC as predictors of excessive response in controlled ovarian hyperstimulation: a meta analysis. Hum Reprod Update. 2011;17(1):46–54. doi: 10.1093/humupd/dmq034. [DOI] [PubMed] [Google Scholar]
- 4.Burgués S, Spanish Collaborative Group on Female Hypogonadotrophic Hypogonadism The effectiveness and safety of recombinant human LH to support follicular development induced by recombinant human FSH in WHO group I anovulation: evidence from a multicentre study in Spain. Hum Reprod. 2001;16(12):2525–2532. doi: 10.1093/humrep/16.12.2525. [DOI] [PubMed] [Google Scholar]
- 5.Fisch JD, Rodriguez H, Ross R, Overby G, Sher G. The Graduated Embryo Score (GES) predicts blastocyst formation and pregnancy rate from cleavage-stage embryos. Hum Reprod. 2001;16(9):1970–1975. doi: 10.1093/humrep/16.9.1970. [DOI] [PubMed] [Google Scholar]
- 6.Hehenkamp WJ, Looman CW, Themmen AP, Jong FH, Velde ER, Broekmans FJ. Anti-Mullerian hormone levels in the spontaneous menstrual cycle do not show substantial fluctuation. J Clin Endocrinol Metab. 2006;91:4057–4063. doi: 10.1210/jc.2006-0331. [DOI] [PubMed] [Google Scholar]
- 7.Marca A, Pati M, Orvieto R, Stabile G, Carducci Artenisio A, et al. Serum Anti-Mullerian Hormone levels in women with secondary amenorrhea. Fertil Steril. 2006;85:1547–1549. doi: 10.1016/j.fertnstert.2005.10.057. [DOI] [PubMed] [Google Scholar]
- 8.Marca A, Sighinolfi G, Radi D, Argento C, Baraldi E, Carducci A, et al. Anti-Müllerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART) Hum Reprod. 2009;16(2):113–130. doi: 10.1093/humupd/dmp036. [DOI] [PubMed] [Google Scholar]
- 9.Levy T, Orvieto R, Homburg R, Peleg D, Dekel A, Ben-Rafael Z. Severe ovarian hyperstimulation syndrome despite low plasma oestrogen concentrations in a hypogonadotrophic, hypogonadal patient. Hum Reprod. 1996;11(6):1177–1179. doi: 10.1093/oxfordjournals.humrep.a019350. [DOI] [PubMed] [Google Scholar]
- 10.Luisi S, Ciani V, Podfigurna-Stopa A, et al. Serum anti-Müllerian hormone, inhibin B, and total inhibin levels in women with hypothalamic amenorrhea and anorexia nervosa. Gynecol Endocrinol. 2012;28(1):34–38. doi: 10.3109/09513590.2011.579664. [DOI] [PubMed] [Google Scholar]
- 11.Majumder K, Gelbaya TA, Laing I, Nardo LG. The use of anti-Müllerian hormone and antral follicle count to predict the potential of oocytes and embryos. Eur J Obstet Gynecol Reprod Biol. 2010;150(2):166–170. doi: 10.1016/j.ejogrb.2010.02.029. [DOI] [PubMed] [Google Scholar]
- 12.Nakhuda GS, Douglas NC, Thornton MH, Guarnaccia MM, Lobo R, Sauer MV. Anti-Müllerian hormone testing is useful for individualization of stimulation protocols in oocyte donors. Reprod Biomed Online. 2010;20(1):42–47. doi: 10.1016/j.rbmo.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Nardo LG, Gelbaya TA, Wilkinson H, Roberts SA, Yates A, Pemberton P, et al. Circulating basal anti-Müllerian hormone levels as predictor of ovarian response in women undergoing ovarian stimulation for in vitro fertilization. Fertil Steril. 2009;92:1586–1593. doi: 10.1016/j.fertnstert.2008.08.127. [DOI] [PubMed] [Google Scholar]
- 14.Nelson SM, Yates RW, Lyall H, Jamieson M, Traynor I, Gaudoin M, et al. Anti-Müllerian hormone-based approach to controlled ovarian stimulation for assisted conception. Hum Reprod. 2009;24(4):867–875. doi: 10.1093/humrep/den480. [DOI] [PubMed] [Google Scholar]
- 15.Panidis D, Georgopoulos NA, Piouka A, Katsikis I, Saltamavros AD, Decavalas G, et al. The impact of oral contraceptives and metformin on anti-Müllerian hormone serum levels in women with polycystic ovary syndrome and biochemical hyperandrogenemia. Gynecol Endocrinol. 2010 Sep 14, [Epub ahead of print]. [DOI] [PubMed]
- 16.Riggs R, Kimble T, Oehninger S, Bocca S, Zhao Y, Leader B, et al. Anti-Müllerian hormone serum levels predict response to controlled ovarian hyperstimulation but not embryo quality or pregnancy outcome in oocyte donation. Fertil Steril. 2011;95:410–412. doi: 10.1016/j.fertnstert.2010.07.1042. [DOI] [PubMed] [Google Scholar]
- 17.Rothman MS, Wierman ME. Female hypogonadism: evaluation of the hypothalamic-pituitary-ovarian axis. Pituitary. 2008;11:163–169. doi: 10.1007/s11102-008-0109-3. [DOI] [PubMed] [Google Scholar]
- 18.Somunkiran A, Yavuz T, Yucel O, Ozdemir I. Anti-Müllerian hormone levels during hormonal contraception in women with polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol. 2007;134:196–201. doi: 10.1016/j.ejogrb.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 19.Speroff L, Fritz MA. Chapter 32, induction of ovulation. In: Speroff L, Fritz MA, editors. Clinical gynecologic endocrinology and infertility. 7. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 1293–1331. [Google Scholar]
- 20.Speroff L, Fritz MA. Chapter 11, amenorrhea. In: Speroff L, Fritz MA, editors. Clinical gynecologic endocrinology and infertility. 8. Philadelphia: Lippincott Williams & Wilkins; 2011. p. 443. [Google Scholar]
- 21.Steiner AZ, Stanczyk FZ, Patel S, Edelman A. Antimullerian hormone and obesity: insights in oral contraceptive users. Contraception. 2010;81(3):245–248. doi: 10.1016/j.contraception.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Streuli I, Fraisse T, Pillet C, Ibecheole V, Bischof P, Ziegler D. Serum antimüllerian hormone levels remain stable throughout the menstrual cycle and after oral or vaginal administration of synthetic sex steroids. Fertil Steril. 2008;90(2):395–400. doi: 10.1016/j.fertnstert.2007.06.023. [DOI] [PubMed] [Google Scholar]
- 23.Sungurtekin U, Fraser IS, Shearman RP. Pregnancy in women with Kallmann’s Syndrome. Fertil Steril. 1995;63(3):494–499. doi: 10.1016/s0015-0282(16)57415-9. [DOI] [PubMed] [Google Scholar]
- 24.Tran ND, Cedars MI, Rosen MP. The role of anti-müllerian hormone (AMH) in assessing ovarian reserve. J Clin Endocrinol Metab. 2011;96(12):3609–3614. doi: 10.1210/jc.2011-0368. [DOI] [PubMed] [Google Scholar]
- 25.Ulug U, Ben-Shlomo I, Tosun S, Erden HF, Akman MA, Bahceci M. The reproductive performance of women with hypo-gonadotropic hypogonadism in an in- vitro fertilization and embryo transfer program. J Assist Reprod Genet. 2005;22(4):167–171. doi: 10.1007/s10815-005-4914-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weenen C, Laven JS, Bergh AR, Cranfield M, Groom NP, Visser JA, et al. Anti-Müllerian hormone expression pattern in the human ovary: potential implications for initial and cyclic follicle recruitment. Mol Hum Reprod. 2004;10(2):77–83. doi: 10.1093/molehr/gah015. [DOI] [PubMed] [Google Scholar]