Abstract
Objective
To identify high-performance work practices (HPWP) associated with high frontline health care worker (FLW) job satisfaction and perceived quality of care.
Methods
Cross-sectional survey data from 661 FLWs in 13 large health care employers were collected between 2007 and 2008 and analyzed using both regression and fuzzy-set qualitative comparative analysis.
Principal Findings
Supervisor support and team-based work practices were identified as necessary for high job satisfaction and high quality of care but not sufficient to achieve these outcomes unless implemented in tandem with other HPWP. Several configurations of HPWP were associated with either high job satisfaction or high quality of care. However, only one configuration of HPWP was sufficient for both: the combination of supervisor support, performance-based incentives, team-based work, and flexible work. These findings were consistent even after controlling for FLW demographics and employer type. Additional research is needed to clarify whether HPWP have differential effects on quality of care in direct care versus administrative workers.
Conclusions
High-performance work practices that integrate FLWs in health care teams and provide FLWs with opportunities for participative decision making can positively influence job satisfaction and perceived quality of care, but only when implemented as bundles of complementary policies and practices.
Keywords: High-performance work practices, frontline health care workers, job satisfaction, perceived quality of care
Frontline health care workers (FLWs), ranging from nursing assistants and patient care technicians to mental health counselors and respiratory therapy technicians, comprise over 50 percent of the health care workforce and provide a wide range of direct patient care and supportive services across health care settings (Schindel et al. 2006). Traditionally, health care organizations have seen investment in FLWs as less worthwhile because the low threshold to entry means these workers can be easily replaced (Lepak and Snell 2002). However, as the U.S. population ages and demand for health care continues to rise, organizations are increasingly relying on FLWs as a more cost-effective method of meeting basic service demands and expanding primary care services (Brownstein et al. 2011). Consequently, workforce management and work redesign strategies have increasingly emerged as critical to health care organizations’ efforts to recruit and retain skilled workers and improve service quality without raising costs (e.g., Standing and Chowdhury 2008).
High-performance work practices (HPWP), also referred to as high involvement or high commitment work systems, seek to increase worker satisfaction and improve organizational performance through investment in human capital (Pfeffer 1996; Burke 2006). HPWP are typically implemented as synergistic “bundles” of policies and practices that emphasize worker training, socialization, and rewards such as team-building, performance-based incentives, job rotation or multiskilling, and participative decision making (Appelbaum et al. 2001; Sullivan 2004). In the health care sector, the effects of HPWP have primarily been studied among physicians or nurses and have been broadly associated with increased worker commitment and reduced health care errors (Harmon et al. 2003; Gowen, McFadden, and Tallon 2006; West et al. 2006). Specific HPWP such as team-based work practices and pay-for-performance have also received considerable attention as strategies for engaging staff and improving quality of care (Fried, Topping, and Rundall 2000; Pearson et al. 2008).
However, although research suggests that FLWs’ response to workforce management and redesign efforts can significantly impact the success of these strategies (Dickson et al. 2009; Petrova et al. 2010), few studies have examined the effects of HPWP on this group of workers. In addition, although HPWP are conceptualized as most effective when implemented as “bundles” of policies and practices (McAlearney et al. 2011), few studies have tested this assumption or assessed the relative effectiveness of different combinations of HPWP. Current research on HPWP has tended to either operationalize HPWP as a single-factor construct or examine the isolated net effect of individual practices on outcomes. Except for a single qualitative study on nursing homes conducted by Eaton (2000) that highlighted the need for a configurational approach to this type of research, the few studies that have examined additive or interactive effects of HPWP on outcomes have not been conducted in the health care sector (MacDuffie 1995; Barnard and Rodgers 2000; Macky and Boxall 2007).
The current study contributes to the literature by applying both multivariate regression and fuzzy-set qualitative comparative analysis (QCA) techniques to identify different configurations or “bundles” of HPWP associated with high job satisfaction and perceived quality of care among FLWs. Data for this study are drawn from a sample of 661 FLWs located within 13 large health care employers within the United States. The framework for this study is based on a conceptual model developed by Garman et al. (2011) following an extensive review of the literature, and it focuses specifically on HPWP policies and practices designed to engage and empower frontline staff as a means of improving worker satisfaction and quality of care.
Background
High-performance work practices originated in the manufacturing sector in the early 1990s but have since spread to the health care and service sectors (Appelbaum, Bailey, and Kalleberg 2000; Preuss 2003; Harley, Allen, and Sargent 2007). HPWP emphasize investment in human capital as a strategy for improving organizational performance. While definitions vary, HPWP are generally conceptualized as “bundles” of mutually reinforcing and complementary human resource policies and practices that promote rigorous worker selection practices, increased career and skill development opportunities, and the use of performance-based incentives, team-based work practices, and participatory decision making (Huselid 1995; Godard and Delaney 2000). A core assumption is that the cumulative effects of HPWP will be greater than the sum of their individual parts (Boxall and Macky 2009). However, while MacDuffie (1995) found significant interactive effects between different types of human resource practices in a sample of 62 automotive assembly plants surveyed in the late 1980s, this assumption has not been explicitly tested in the health care sector.
Research on HPWP in the health care sector is also fairly limited. To the best of our knowledge, only three studies have examined the effect of HPWP on FLWs: Eaton (2000) conducted a qualitative study of the association between work structures and patient care quality in 14 skill nursing facilities in California and Pennsylvania and found that “high-quality” facilities consistently promoted teamwork and the sharing patient information with nurse aides, whereas “low-quality” facilities did not engage in these practices. Appelbaum, Berg, Frost, and Preuss (2003) examined a sample of nurse aides and housekeepers in 12 U.S. hospitals and found that workers in positions that provided more autonomy and opportunities for team-based work were less likely to quit their jobs. Finally, Harley, Allen, and Sargent (2007) found that HPWP positively influenced job satisfaction and reduced turnover intention among 1,318 aged care workers in the Australian service sector. The authors also found that HPWP had slightly different effects on FLWs than on nurses, demonstrating the applicability of HPWP to FLWs as well as the need for additional research on this group of workers.
Conceptual Framework
The conceptual framework for this study is based on an evidence-informed model developed by Garman et al. (2011) after reviewing 114 peer-reviewed articles on HPWP, 10 of which were specific to health care. In this model, the authors identified four “subsystems” of HPWP as critical for achieving positive worker- and organization-level outcomes: staff motivation, frontline empowerment, talent acquisition, and leadership support.
Practices in the staff motivation subsystem focus on increasing workers’ awareness of and personal stake in the organization's vision through strategies such as providing workers with opportunities to provide input on current work processes or providing performance-based incentives linked with objective criteria (Cappelli and Neumark 2001). In contrast, frontline empowerment practices affect care processes associated with safe, high-quality care by reducing status distinctions and providing an environment in which workers feel secure, for example, team-based work practices, decentralized decision making, or supportive practices such as job rotation or flexible scheduling that enable workers to seek additional learning opportunities or experience more autonomy in their positions (Cropanzano and Mitchell 2005; Farrar et al. 2011). Finally, practices in the talent acquisition emphasize rigorous recruitment and selection of staff as well as provision of career and skill development opportunities, whereas leadership support practices help make leaders aware of the strategic alignment between HPWP and desired outcomes at the worker and/or organizational level (Eaton 2000; Ramirez, Guy, and Beale 2007).
The current study focuses primarily on HPWP associated with worker and organization-level outcomes in the staff motivation and frontline empowerment subsystems. We emphasize these two subsystems because they contain the practices most readily reportable by FLWs and because they are the only subsystems within Garman et al.'s (2011) model hypothesized to have a direct effect on FLW and/or organizational outcomes (Figure 1). Talent acquisition practices related to the recruitment and hiring of staff influence the quality of hires brought into an organization, but their effect on frontline health care processes is indirect; similarly, leadership support practices influence the adoption, implementation, and sustainability of other HPWP subsystems, but they are not otherwise expected to influence FLWs’ daily work processes.
Figure 1.
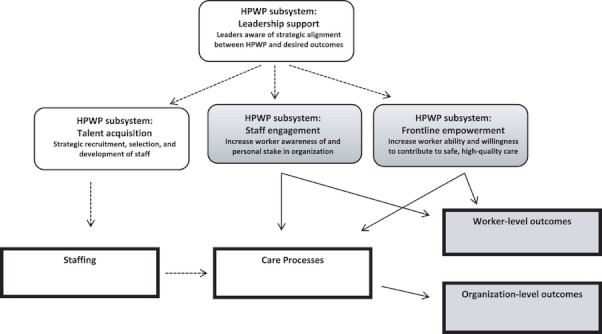
Conceptual Model of High Performance Work Practice (HPWP) Subsystems and Their Hypothesized Effect on Worker- and Organization-Level Outcomes
Note. This conceptual model is adapted from previous work by Garman et al. (2011). Shaded boxes and solid arrows indicate variables and hypothesized relationships included in the current analysis.
Study Hypotheses
Previous research has discussed the potential advantages of a configurational approach to analysis of constructs such as HPWP, which are conceptualized as most effective when “bundled” together as complementary sets of policies and practices (Meyer, Tsui, and Hinings 1993; Fiss 2011). This approach has not previously been taken in research on HPWP in health care, primarily because traditional regression techniques are limited in their ability to accommodate interactions between three or more variables. However, recent methodological advances in the use of fuzzy-set QCA have now made a configurational approach more feasible (Ragin 2008b).
In the current study, we apply both multivariate regression and fuzzy-set QCA to identify configurations of HPWP that are positively associated with worker and organizational outcomes, specifically FLWs’ job satisfaction and perceived quality of care. Job satisfaction is an important employee-level outcome associated with both worker commitment (Castle et al. 2007) and retention (Denton et al. 2007). Similarly, perceived quality of care is strongly correlated with patient satisfaction (e.g., Sikorska-Simmons 2006) and previous research has found that frontline worker assessments of patient health are as accurate as those of mid-level practitioners (Hartig, Engle, and Graney 1997; Engle, Graney, and Chan 2001).
Consistent with Garman et al.'s (2011) conceptual model, we hypothesize that configurations of HPWP, including practices from both the staff motivation and the frontline empowerment subsystems, will be associated with both high job satisfaction and high perceived quality of care. We also test the complementarity hypothesis, which suggests that HPWP are more effective when implemented in tandem than as isolated, individual practices.
Methods
Data and Sample
This study utilized baseline data collected between March 2007 and December 2008 as part of the national evaluation of the Robert Wood Johnson Foundation Jobs to Careers: Transforming the Frontline Lines of Health Care program. Our study sample consisted of FLWs and key informants located within 13 health care employers, comprised of 10 unique hospitals and/or health care systems and 3 community health centers. While geographically diverse, all of the health care employers in our sample shared a common expressed interest in investing in FLWs and had clear strategic reasons for doing so. In addition, all except two of the employers were private not-for-profit. Appendix SA2 provides a more detailed profile of the health care employers within our sample.
At baseline, that is, prior to implementation of the Jobs to Careers programs, FLWs in targeted occupations at each health care employer were surveyed about their demographic characteristics, job satisfaction, perceived quality of care, and policies and practices within the staff motivation and frontline empowerment subsystems. These survey measures were previously validated in a sample of frontline workers in long-term care and are described in detail elsewhere (Morgan 2005; Morgan and Konrad 2008). Surveys were distributed in person to FLWs by an evaluation liaison located within each health care employer, and returned directly to the evaluation team using business reply envelopes to ensure confidentiality. Information about the study protocol and FLW rights as human subjects was included with each survey. A total of 661 FLWs returned the questionnaire, for an overall response rate of 73.7 percent; response rates for individual health care employers varied from 57 to 100 percent. Key informants responsible for clinical operations and/or HR policies at each participating health care organization (e.g., CEO or high-level executive, HR personnel and managers) were also interviewed about each employer's history of investment in workforce development and the extent to which senior management supported the use of these policies and practices. Consent for these semi-structured interviews was obtained through formal written consent. The evaluation team staff also collected contextual data on county-level population and unemployment rates from the Census Bureau and the Bureau of Labor Statistics Local Area Unemployment Statistics.
Listwise deletion of missing data reduced the final analytic sample to 615 FLWs in the job satisfaction model and 588 in the model examining perceived quality of care. T-tests conducted to determine if data were missing at random indicated that FLWs in the final analytic sample did not differ significantly from those excluded due to missing data on any of the variables in this study.
Measures
Previous research suggests that there is significant variation in the extent to which policies and practices are consistently implemented across organizations (McGovern and Stiles 1997; Currie and Proctor 2001). Consequently, we gave preference to FLW assessments of enacted human resource policies within their immediate work environment (Callan et al. 2007), and we relied on key informants’ reports of formal HR policies only as needed to fill in missing data.
Job satisfaction and perceived quality of care were based on FLW ratings on a scale of 1–10. Six measures of HPWP were utilized. Practices categorized as belonging to the staff motivation subsystem included (1) workers’ opportunities for creative input and innovation in their work (scaled 1–4); (2) supervisor support for FLW participation, operationalized as the extent to which supervisors treated FLWs as equal members of the health care team and listened to their observations (two items, scaled 0–2, α = 0.84); and (3) provision of incentive pay, such as pay for performance (Yes/No). Frontline empowerment practices included (4) team-based work practices, that is, the extent to which workers felt that they were part of the health care team and supported by co-workers (two items, scaled 1–4, α = 0.75); (5) flexible work arrangements such as self-scheduling or telework (Yes/No); and (6) job rotation or multiskilling, that is, rotating FLWs into different roles or departments to develop cross-functional skills (Yes/No). More detailed information on these study measures is provided in Appendix SA3.
We also included a number of FLW demographic and contextual characteristics as control variables. Demographic characteristics were based on FLW self-report and included gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other non-Hispanic minority), education (high school or less, greater than high school education), work status (full-time, part-time), and family status (single mother, other). FLWs were also classified into one of two categories: (1) workers providing direct patient care (e.g., medical assistants, patient care technicians, and certified nursing assistants), and (2) administrative and other support staff (e.g., clinical service representatives, medical receptionists, and monitor or laboratory technicians). Contextual characteristics included health care employer type (community health center, hospital or health care system), county population (per 100,000), and county unemployment (percent).
Analyses
Due to our interest in the impact of both individual and combined HPWP, analyses proceeded in three phases: (1) multivariate regression; (2) QCA; and (3) integration of QCA with regression.
In Phase I, all analyses were run as ordinary least-squares regression. Robust cluster variance estimators accounted for the clustering of FLWs within the 13 unique health care employers. Pearson and phi correlations as well as variance inflation factors (VIF) after each regression did not indicate problematic multicollinearity: Correlations were all <0.4 and VIF < 2. Analyses in this phase mirror previous HPWP research, which has examined associations between individual HPWP and the outcomes of interest, but not tested for synergistic rather than competing effects.
In Phase II, we re-analyzed our sample using a different technique, QCA. QCA is based on set-theoretic principles and differs from regression in several ways that make it better suited to examining combinatorial effects of HPWP on job satisfaction or quality of care. The most critical differences between regression and QCA relate to the assumptions made by each regarding associations between predictors and outcomes. In regression analysis, each independent variable is considered sufficient, by itself, to produce an incremental change in the outcome. The impact of a given predictor on the outcome is also generally assumed to be the same not only for all values of other predictors but across their different combinations as well. While regression models can accommodate two-way interaction terms, the interpretation of main and interaction effects is often challenged by the high degree of collinearity that usually exists between them (Jaccard, Wan, and Turrisi 1990) and models generally cannot feasibly be extended to examine more complex combinations, for example, three- or four-way interactions (Ragin 1987).
By contrast, a key assumption of QCA is that predictors exert their influence in combination with other variables to impact outcomes. QCA also assumes causal heterogeneity, that is, that different combinations of practices can lead to the same outcome (Rihoux and Ragin 2009) and is asymmetric, meaning factors that contribute to the presence of an outcome are analyzed separately from factors that contribute to the absence of that outcome (Ragin 1999). The assumptions of causal heterogeneity and asymmetry are both related to the underlying logic behind QCA, which is based on set–subset relationships (Fiss 2011) and better suited to examination of combinatorial effects of HPWP than regression.
In the current study, QCA was applied to identify configurations of HPWP associated with high job satisfaction and high perceived quality of care, adjusting for the clustering of FLWs within health care employers. This process was accomplished in five steps. First, QCA requires that all variables have values ranging from 0 to 1. With dichotomous variables, this process is straightforward, as all cases are already represented in this format. However, nondichotomous variables must be re-calibrated so that they range from 0 to 1 (Ragin 2008b). Multiple calibration techniques are available (Ragin 2008a). In our study, we chose to calibrate by rank ordering and then standardizing all nondichotomous variables to range from 0 to 1 (Longest and Vaisey 2008); in this calibration process, cases are defined relative to each other based on the observed distribution of scores.
Calibrated variables were then used to construct a data matrix known as a truth table (Fiss 2011). Truth tables are the primary analytic tool within QCA and effectively restructure the data to display all possible configurations of HPWP associated with the specified outcome (Ragin 2008b). A sample truth table displaying the 10 configurations of HPWP with the greatest empirical prevalence within our sample and their association with FLW high job satisfaction and perceived quality of care is provided in Appendix SA4.
Next, probabilistic criteria were applied to calculate the set-theoretic consistency and coverage for each row in the truth table. Consistency and coverage are the two main criteria for evaluating QCA results. Set-theoretic consistency measures the extent to which a given configuration of practices is always associated with the same outcome (Smithson and Verkuilen 2006). In order to be considered “sufficient” to produce an outcome, a configuration must meet a minimum consistency threshold of 0.80, or 80 percent (Ragin 2008b). Set-theoretic coverage, or the proportion of FLWs represented by a given configuration of HPWP, indicates the empirical prevalence of that configuration within the data.
Principles from Boolean algebra were then used to identify logically minimum combinations of HPWP sufficient to produce high job satisfaction and/or perceived quality of care in our sample. This minimization process was accomplished using computer algorithms and was not conducted by hand (Ragin 2008b). The purpose of this minimization process is to eliminate variables that do not contribute meaningfully to the outcome in question and to differentiate between necessary and sufficient variables. Evaluation of sufficiency and necessity is a critical component of QCA. Variables are considered necessary if they must be present in order for the outcome to occur; however, the presence of a necessary variable is not sufficient to guarantee that the outcome will occur. Sufficient variables are those that consistently produce a given outcome when they are present. In practice, variables or configurations of variables are considered sufficient when the minimum consistency threshold of 0.80 is met (Ragin 2008b).
Finally, in Phase III, configurational solutions identified through QCA were entered into regression models to identify configurations of HPWP that were associated with job satisfaction and perceived quality of care after controlling for FLW demographic and contextual characteristics.
All regression analyses were conducted in Stata 11.0. QCA was conducted using the FUZZY module in Stata 11.0 (Longest and Vaisey 2008).
Results
Consistent with national trends (Schindel et al. 2006), the majority of FLWs in our sample were female (91 percent), had a high school education or less (61 percent), and nonwhite minorities (78 percent). On average, the mean income of these workers was $25,000 a year; only 4 percent of the workers reported an annual income of $40,000 or more. A total of 51 percent of these workers provided direct patient care; the remainder were administrative or other support staff. Approximately 29 percent of FLWs worked in community health centers; the remainder worked in hospital-based systems. A full table of descriptive statistics is provided in Appendix SA5.
Multivariate regression results indicate that three practices—supervisor support, team-based work practices, and flexible work arrangements—were positively associated with both job satisfaction and perceived quality of care (Table 1). Provision of incentive pay was significantly associated with perceived quality of care (β = 0.32, p < .01) but not with job satisfaction. By contrast, opportunities for creative input was associated with FLW job satisfaction (β = 0.59, p < .01) but not perceived quality of care. Job rotation was not significantly associated with either outcome.
Table 1.
Multivariate Regression: Individual HPWP Associated with FLW Job Satisfaction and Perceived Quality of Care†
| Job Satisfaction (N = 615, R2 = 0.35) | Perceived Quality of Care (N = 588, R2 = 0.27) | |||||||
|---|---|---|---|---|---|---|---|---|
| Coeff. | Robust SE | 95% | CI | Coeff. | Robust SE | 95% | CI | |
| High performance work practices | ||||||||
| Creative input | 0.59** | 0.08 | 0.42 | 0.76 | 0.18 | 0.13 | −0.10 | 0.47 |
| Supervisor support | 0.63** | 0.20 | 0.20 | 1.05 | 0.78** | 0.15 | 0.46 | 1.10 |
| Incentive pay | 0.01 | 0.12 | −0.25 | 0.28 | 0.22** | 0.06 | 0.10 | 0.34 |
| Team-based work | 0.81** | 0.17 | 0.44 | 0.19 | 0.43* | 0.17 | 0.06 | 0.80 |
| Flexible work | 0.40** | 0.10 | 0.18 | 0.63 | 0.27** | 0.06 | 0.13 | 0.41 |
| Job rotation | −0.11 | 0.12 | −0.38 | 0.16 | 0.14 | 0.12 | −0.12 | 0.41 |
| FLW characteristics | ||||||||
| Male | −0.56** | 0.15 | −0.89 | −0.23 | −0.01 | 0.19 | −0.42 | 0.40 |
| Race/ethnicity | ||||||||
| Black | 0.12 | 0.13 | −0.17 | 0.42 | 0.01 | 0.21 | −0.44 | 0.46 |
| Hispanic | 0.31* | 0.14 | 0.00 | 0.61 | 0.23* | 0.11 | 0.00 | 0.46 |
| Other minority | −0.35** | 0.10 | −0.57 | −0.12 | −0.48* | 0.22 | −0.96 | 0.00 |
| More than high school degree | −0.25 | 0.16 | −0.60 | 0.09 | 0.05 | 0.10 | −0.15 | 0.26 |
| Works part-time | −0.37* | 0.17 | −0.74 | −0.01 | −0.00 | 0.19 | −0.42 | 0.41 |
| Single mother | −0.14 | 0.23 | −0.63 | 0.36 | 0.11 | 0.12 | −0.18 | 0.36 |
| Administrative or nonclinical role | −0.07 | 0.08 | −0.25 | 0.11 | −0.16 | 0.11 | −0.39 | 0.07 |
| Contextual variables | ||||||||
| Community health l | 0.18 | 0.16 | −0.17 | 0.53 | −0.07 | 0.12 | −0.34 | 0.20 |
| County population (10,000) | −0.03* | 0.01 | −0.06 | −0.01 | −0.01 | 0.02 | −0.04 | 0.03 |
| County unemployment (%) | −0.15** | 0.04 | −0.23 | −0.07 | −0.13* | 0.05 | −0.24 | −0.01 |
| Constant | 1.69** | 0.51 | 0.58 | 2.81 | 4.43** | 0.47 | 3.40 | 5.46 |
Note. HPWP, high-performance work practices; FLW, frontline health care worker.
p < .05;
p < .01.
Results from Breusch–Pagan Lagrangian multiplier and Hausman specification tests indicated that OLS regression was the appropriate modeling approach.
Table 2 presents key results obtained when the study sample was re-analyzed using QCA. First and foremost, no single HPWP met the minimum consistency threshold of 0.80. These findings suggest that by themselves, individual HPWP are not sufficient to produce high job satisfaction or quality of care; to achieve maximum effect, HPWP must be implemented in tandem.
Table 2.
Fuzzy-Set Qualitative Comparative Analysis: High-Performance Work Practice Sufficient for High Job Satisfaction and Perceived Quality of Care
| Consistency* | Raw Coverage | |
|---|---|---|
| Job satisfaction, full sample | ||
| Creative input | 0.66 | 0.77 |
| Supervisor support | 0.64 | 0.87 |
| Incentive pay | 0.57 | 0.56 |
| Team-based work | 0.71 | 0.84 |
| Flexible work | 0.69 | 0.73 |
| Job rotation | 0.54 | 0.49 |
| Configuration: Supervisor support*Incentive pay*Team-based work*Flexible work | 0.84† | 0.34 |
| Configuration: Creative input*Supervisor support*Team-based work | 0.83† | 0.65 |
| Perceived quality of care, full sample | ||
| Creative input | 0.71 | 0.74 |
| Supervisor support | 0.65 | 0.86 |
| Incentive pay | 0.60 | 0.56 |
| Team-based work | 0.71 | 0.81 |
| Flexible work | 0.74 | 0.72 |
| Job rotation | 0.64 | 0.38 |
| Configuration: Creative input*Supervisor support*Team-based work*Flexible work | 0.86† | 0.53 |
| Configuration: Supervisor support*Incentive pay*Team-based work*Flexible work | 0.85† | 0.33 |
| Configuration: Creative input*Supervisor support*Team-based work*Job rotation | 0.84† | 0.32 |
| Configuration: Creative input*Supervisor support*Incentive pay*Job rotation | 0.81† | 0.21 |
To be considered “sufficient” to produce the outcome, must have a consistency value of 0.80 or higher.
Sufficiency criteria of 0.80 or higher are met.
Two configurations of HPWP were identified as sufficient for high job satisfaction. The first configuration of Supervisor support*Incentive pay*Team-based work*Flexible work accounted for 34 percent of FLWs highly satisfied with their jobs, whereas the second configuration of Creative input*Supervisor support*Team-based work practices accounted for 65 percent of highly satisfied FLWs. Examination of individual HPWP within these configurations revealed that supervisor support and team-based work practices were necessary but not sufficient for high FLW job satisfaction.
A total of four different configurations of HPWP were identified as sufficient for high perceived quality of care. Of these four configurations, the configuration with the highest consistency and coverage scores was Creative input*Supervisor support*Team-based work*Flexible work. The consistency of this configuration was 0.86, meaning it was associated with high perceived quality of care 86 percent of the time, and the raw coverage was 0.53, meaning this configuration accounted for 53 percent of the workers in our sample. However, only the configuration of Supervisor support*Incentive pay*Team-based work*Flexible work was also associated with high job satisfaction (consistency 0.85, coverage 0.33). Examination of HPWP within the four configurations indicated that supervisor support was also necessary for high perceived quality of care, although again, not sufficient to achieve this outcome unless implemented in tandem with other practices.
Table 3 presents multivariate regression results for associations between HPWP configurations and FLW job satisfaction and perceived quality of care. Both configurations of HPWP identified as sufficient for high job satisfaction in FLWs were significant in regression analyses, even after controlling for demographic and contextual characteristics. In particular, the configuration of Creative input*Supervisor support*Team-based work was associated with almost a three-point increase in frontline workers’ job satisfaction ratings (β = 2.89, p < .01). However, after controlling for FLW demographic and contextual characteristics, only three configurations of HPWP were significantly associated with perceived quality of care. Regression analyses indicated that the configuration of Creative input*Supervisor support*Team-based work*Flexible work was the most strongly associated with perceived quality of care (β = 1.82, p < .01); however, two other configurations of practices involving supervisor support and team-based work practices also emerged as significant.
Table 3.
Multivariate Regression and Fuzzy-Set Qualitative Comparative Analysis: Configurations of High-Performance Work Practices (HPWP) Associated with Frontline Health Care Worker Job Satisfaction and Perceived Quality of Care
| Job Satisfaction (N = 615, R2 = 0.25) | Perceived Quality of Care (N = 588, R2 = 0.19) | |||||||
|---|---|---|---|---|---|---|---|---|
| Coeff. | Robust SE | 95% CI | Coeff. | Robust SE | 95% CI | |||
| HPWP† | ||||||||
| Supervisor*Pay*Team*Flex | 0.54* | 0.22 | 0.07 | 1.01 | 0.54** | 0.14 | 0.23 | 0.85 |
| Input*Supervisor*Team | 2.89** | 0.22 | 2.42 | 3.37 | N/A | N/A | N/A | N/A |
| Input*Supervisor*Team*Flex | N/A | N/A | N/A | N/A | 1.82** | 0.38 | 0.98 | 2.65 |
| Input*Supervisor*Team*Rotate | N/A | N/A | N/A | N/A | 0.75* | 0.30 | 0.10 | 1.41 |
| Input*Supervisor*Pay*Rotate | N/A | N/A | N/A | N/A | −0.15 | 0.24 | −0.67 | 0.37 |
| Frontline worker characteristics | ||||||||
| Male | −0.58* | 0.18 | −0.98 | −0.17 | −0.10 | 0.19 | −0.53 | 0.32 |
| Race/ethnicity | ||||||||
| Black | 0.01 | 0.15 | −0.32 | 0.35 | −0.03 | 0.20 | −0.46 | 0.39 |
| Hispanic | 0.36* | 0.15 | 0.03 | 0.68 | 0.34* | 0.14 | 0.04 | 0.64 |
| Other minority | −0.27* | 0.11 | −0.51 | −0.03 | −0.52* | 0.22 | −0.99 | −0.05 |
| More than high school degree | −0.24 | 0.17 | −0.62 | 0.14 | 0.07 | 0.11 | −0.16 | 0.31 |
| Works part-time | −0.35 | 0.19 | −0.76 | 0.06 | 0.05 | 0.18 | −0.35 | 0.45 |
| Single mother | −0.32 | 0.25 | −0.87 | 0.23 | −0.03 | 0.11 | −0.27 | 0.21 |
| Administrative or nonclinical role | −0.07 | 0.09 | −0.26 | 0.12 | −0.20 | 0.12 | −0.46 | 0.06 |
| Contextual variables | ||||||||
| Community health center | 0.13 | 0.21 | −0.32 | 0.58 | −0.18 | 0.12 | −0.45 | 0.09 |
| County population (10,000) | −0.02 | 0.02 | −0.06 | 0.02 | 0.00 | 0.02 | −0.03 | 0.04 |
| County unemployment (%) | −0.09* | 0.04 | −0.17 | −0.00 | −0.09 | −0.05 | −0.20 | 0.01 |
| Constant | 6.61** | 0.28 | 6.00 | 7.23 | 7.62** | 0.32 | 6.93 | 8.32 |
Note.
p < .05.
p < .01.
Creative input (Input), Supervisor support (Supervisor), Incentive pay (Pay), Team-based work (Team), Flexible work (Flex), Job rotation (Rotate).
We also conducted additional, post hoc analyses to test for the possibility of differential HPWP effects based on health care employer type or FLW job role. Results (not shown) did not differ by employer type (i.e., no difference between hospital-based systems or community health centers). However, as shown in Table 4, while there were also no differences in job satisfaction between direct care and administrative workers, results indicate differential effects of HPWP on perceived quality of care: For direct care workers, both team-based work and flexible work were identified as necessary but not sufficient for high perceived quality of care. By contrast, a single configuration of HPWP including all practices except job rotation emerged as both necessary and sufficient to high perceived quality of care in administrative workers. The small sample sizes mean these findings must be interpreted with caution; however, results indicate the need for additional research examining the impact of HPWP on care processes in these two groups of workers.
Table 4.
Fuzzy-Set Qualitative Comparative Analysis: Configurations of High-Performance Work Practices Sufficient for High Job Satisfaction and Perceived Quality of Care by Frontline Health Care Worker Job Type
| Consistency* | Raw Coverage | |
|---|---|---|
| Job satisfaction, direct care workers | ||
| Supervisor support*Incentive pay*Team-based work*Flexible scheduling | 0.85 | 0.57 |
| Creative input*Supervisor support*Team-based work | 0.84 | 0.65 |
| Job satisfaction, administrative or other support workers | ||
| Supervisor support*Incentive pay*Team-based work*Flexible scheduling | 0.81 | 0.62 |
| Creative input*Supervisor support*Team-based work | 0.80 | 0.65 |
| Perceived quality of care, direct care workers | ||
| Creative input*Supervisor support*Team-based work*Flexible scheduling | 0.88 | 0.50 |
| Creative input*Incentive pay*Team-based work*Flexible scheduling | 0.87 | 0.28 |
| Supervisor support*Incentive pay*Team-based work*Flexible scheduling | 0.82 | 0.38 |
| Perceived quality of care, administrative or other support workers | ||
| Creative input*Supervisor support*Incentive pay*Team-based work*Flexible scheduling | 0.81 | 0.29 |
To be considered “sufficient” to produce the outcome, must have a consistency value of 0.80 or higher.
Discussion
Frontline health care workers play a critical role in the delivery of basic health care services and have an important impact on patient satisfaction and other health care outcomes (Schindel et al. 2006; Collins et al. 2008). Currently, FLW occupations are among the fastest growing in the United States; collectively, their projected growth rate is higher than the growth rate of all health and health care occupations in the U.S. workforce (Bureau of Labor Statistics 2004). Health care organizations are increasingly responding to quality, cost, and safety pressures by implementing bundles of HPWP designed to improve both worker commitment and health care outcomes. However, given that strategies such as HPWP require significant investment of resources on the part of health care employers, the limited evidence regarding their relative effectiveness in the health care sector provides a meaningful opportunity for more focused studies in this area. Furthermore, there is little research indicating which bundles of HPWP might be usefully combined to improve key worker and health care outcomes. This study sought to achieve two objectives: First, to identify individual or configurations of HPWP positively associated with both worker and organizational outcomes and, second, to test the hypothesis that HPWP are more effective when implemented in tandem than as isolated, individual practices.
Regression analysis identified supervisor support for FLW participation in care processes, team-based work practices, and flexible work as positively associated with FLW outcomes; these findings are consistent with previous research on FLW job satisfaction and commitment in long-term care (Bishop et al. 2008; Howe 2008; Decker, Harris-Kojetin, and Bercovitz 2009; Donoghue and Castle 2009). QCA expanded on these results by demonstrating that individually, none of the HPWP examined in this study were sufficient for high FLW job satisfaction or perceived quality of care. Instead, as suggested by the complementarity hypothesis, HPWP such as supervisor support and team-based work practices consistently produced high job satisfaction and perceived quality of care only when implemented in tandem with other practices. Configurational solutions identified using QCA remained significant even after controlling for FLW demographic and contextual characteristics. These results confirm the utility of a configurational approach to research on organizations and management in the health care sector (Meyer, Tsui, and Hinings 1993) and suggest the value of applying QCA as an alternative or complement to multiple regression in situations where combinatorial effects and/or causal heterogeneity of solutions are expected.
Study findings also provided preliminary confirmation of the hypothesis that a “bundled” approach to HPWP incorporating practices from multiple HPWP subsystems might be more effective than focusing on practices from just one HPWP subsystem: In the current study, the only configuration of HPWP sufficient for both high job satisfaction and quality of care included practices from both the staff motivation and frontline empowerment subsystems. This finding suggests that implementing policies from different HPWP subsystems may be more effective than focusing on a single subsystem or particular policy. Given that we only examined HPWP from two of the four HPWP subsystems within the Garman et al.'s (2011) framework, additional research is needed to determine the relative importance of a “bundled” approach involving practices from all four subsystems.
This study had several limitations that must be considered in the interpretation of the results. First, our sample included primarily not-for-profit hospitals and community health centers with an expressed commitment to investing in FLWs. Consequently, the prevalence of HPWP and FLW job satisfaction is likely to be higher in our sample than nationally. Study findings may also not be generalizable to for-profit or publicly owned health care organizations, which might have organizational priorities or personnel policies that do not support implementation of HPWP.
Another limitation of the study is the use of perceived quality of care rather than observed clinical measures of quality of care. Although previous literature has demonstrated that staff and patient perceptions of quality of care are often highly correlated (Hartig, Engle, and Graney 1997; Sikorska-Simmons 2006), we were only able to examine associations between HPWP and staff perceptions of care quality. Finally, we did not have a large number of organizations in our sample, which limited our ability to make valid inferences in subgroup analyses based on health care employer type and FLW job role.
Future research could address these limitations by replicating analyses in a nationally representative sample of hospitals, community health centers, or other health care organizations; by examining the impact of HPWP on observable behavioral worker-level outcomes such as absenteeism or turnover; or by linking findings to objective quality of care measures such as patient safety errors or patient satisfaction.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by grant 59245 from the Robert Wood Johnson Foundation with supplemental support from the Hitachi Foundation and the U.S. Department of Labor to evaluate the “Jobs to Careers: Transforming the Front Lines of Health Care” program. The authors would like to thank Brandy Farrar and Kendra Jason for assistance with data collection; Ashley Rice, Melissa Mann, and Jennifer Curasi for administrative support in the data collection process; and HSR referees who provided feedback on earlier drafts of the manuscript.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Overview of Health Care Employers.
Appendix SA3: Description of Key Study Variables.
Appendix SA4: Truth Table of the Most Frequent Configurations of High Performance Work Practices Associated with Each Outcome.
Appendix SA5: Descriptive Statistics (N = 661).
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Appelbaum E, Bailey T, Kalleberg AL. Manufacturing Advantage: Why High-Performance Work Systems Pay Off. Ithaca, NY: Cornell University Press; 2000. [Google Scholar]
- Appelbaum E, Bailey T, Berg P, Kalleberg AL. “Do High Performance Work Systems Pay Off?”. Research in the Sociology of Work. 2001;10:85–107. [Google Scholar]
- Appelbaum E, Berg P, Frost A, Preuss G. “The Effect of WorkRe-Structuring on Low-Wage Low-Skilled Workers in U.S. Hospitals”. In: Appelbaum E, Bernhardt A, Murnane R, editors. Low-Wage America: How Workers Are Resharing Opportunity in the Workplace. New York: Russell Sage Foundation; 2003. pp. 33–76. [Google Scholar]
- Barnard ME, Rodgers RA. “How Are Internally Oriented HRM Policies Related to High Performance Work Practices? Evidence from Singapore”. International Journal of Human Resource Management. 2000;11(6):1017–46. [Google Scholar]
- Bishop C, Weinberg D, Leutz W, Dossa A, Pfefferle S, Zincavage R. “Nursing Assistants’ Job Commitment: Effect of Nursing Home Organizational Factors and Impact on Resident Well-Being”. Gerontologist. 2008;48(Special Issue):36–45. doi: 10.1093/geront/48.supplement_1.36. [DOI] [PubMed] [Google Scholar]
- Boxall P, Macky K. “Research and Theory on High-Performance Work Systems: Progressing the High-Involvement Stream”. Human Resource Management Journal. 2009;19(1):3–23. [Google Scholar]
- Brownstein J, Hirsch G, Rosenthal E, Rush C. “Community Health Workers ‘101’ for Primary Care Providers and Other Stakeholders in Health Care Systems”. Journal of Ambulatory Care Management. 2011;34(3):210–20. doi: 10.1097/JAC.0b013e31821c645d. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. Occupational Projects and Training Data 2003-2004: Supplement to the Occupational Outlook Handbook 2004-2005. Washington, DC: U.S. Department of Labor; 2004. [Google Scholar]
- Burke R. “The Human Resources Revolution”. In: Burke RJ, Cooper CL, editors. The Human Resources Revolution: Why Putting People First Matters. Oxford, UK: Elsevier Ltd; 2006. pp. 3–11. [Google Scholar]
- Callan V, Gallois C, Mayhew M, Grice T, Tluchowska M, Boyce R. “Restructuring the Multi-Professional Organization: Professional Identity and Adjustment to Change in a Public Hospital”. Journal of Health and Human Services Administration. 2007;29(4):449–77. [PubMed] [Google Scholar]
- Cappelli P, Neumark D. “Do High-Performance Work Practices Improve Establishment-Level Outcomes?”. Industrial and Labor Relations Review. 2001;54(4):737–75. [Google Scholar]
- Castle N, Engberg J, Anderson R, Men A. “Job Satisfaction of Nurse Aides in Nursing Homes: Intent to Leave and Turnover”. Gerontologist. 2007;47(2):193–204. doi: 10.1093/geront/47.2.193. [DOI] [PubMed] [Google Scholar]
- Collins K, Collins S, McKinnies R, Jensen S. “Employee Satisfaction and Employee Retention: Catalysts to Patient Satisfaction”. Health Care Manager. 2008;27(3):245–51. doi: 10.1097/01.HCM.0000318755.24332.4b. [DOI] [PubMed] [Google Scholar]
- Cropanzano R, Mitchell M. “Social Exchange Theory”. Journal of Management. 2005;31:874–900. [Google Scholar]
- Currie G, Proctor S. “Exploring the Relationship between HR and Middle Managers”. Human Resource Management Journal. 2001;11(7):53–69. [Google Scholar]
- Decker F, Harris-Kojetin L, Bercovitz A. “Intrinsic Job Satisfaction, Overall Satisfaction, and Intention to Leave the Job among Nursing Assistants in Nursing Homes”. Gerontologist. 2009;49(5):596–610. doi: 10.1093/geront/gnp051. [DOI] [PubMed] [Google Scholar]
- Denton M, Zeytinoglu I, Kusch K, Davies S. “Market Modeled Home Care: Impact on Job Satisfaction and Propensity to Leave”. Canadian Public Policy. 2007;33:S81–99. [Google Scholar]
- Dickson E, Anguelov Z, Vetterick D, Eller A, Singh S. “Use of Lean in the Emergency Department: A Case Series of Four Hospitals”. Annals of Emergency Medicine. 2009;54(4):504–10. doi: 10.1016/j.annemergmed.2009.03.024. [DOI] [PubMed] [Google Scholar]
- Donoghue C, Castle N. “Leadership Styles of Nursing Home Administrators and Their Association with Staff Turnover”. Gerontologist. 2009;49(2):166–74. doi: 10.1093/geront/gnp021. [DOI] [PubMed] [Google Scholar]
- Eaton S. “Beyond ‘Unloving Care’: Linking Human Resource Management and Patient Care Quality in Nursing Homes”. International Journal of Human Resource Management. 2000;11(3):591–616. [Google Scholar]
- Engle V, Graney M, Chan A. “Accuracy and Bias of Licensed Practical Nurse and Nursing Assistant Ratings of Nursing Home Residents’ Pain”. Journal of Gerontology: Series A Biological and Medical Sciences. 2001;56(7):M405–11. doi: 10.1093/gerona/56.7.m405. [DOI] [PubMed] [Google Scholar]
- Farrar B, Morgan J, Chuang E, Konrad TR. “Growing Your Own: Community Health Workers and Jobs to Careers”. Journal of Ambulatory Care Management. 2011;34(3):234–46. doi: 10.1097/JAC.0b013e31821c6408. [DOI] [PubMed] [Google Scholar]
- Fiss P. “Building Better Causal Theories: A Fuzzy Set Approach to Typologies in Organization Research”. Academy of Management Journal. 2011;54(2):393–420. [Google Scholar]
- Fried BJ, Topping S, Rundall T. “Groups and Teams in Organizations”. In: Shortell S, Kaluzny A, editors. Health Care Management: Organization Design and Behavior. Albany, NY: Delmar Publishers; 2000. pp. 154–90. [Google Scholar]
- Garman A, McAlearney A, Harrison M, Song P, McHugh M. “High-Performance Work Systems in Health Care Management, Part 1: Development of an Evidence-Informed Model”. Health Care Management Review. 2011;36(3):201–13. doi: 10.1097/HMR.0b013e318201d1bf. [DOI] [PubMed] [Google Scholar]
- Godard J, Delaney J. “Reflections on the High Performance Paradigm's Implications for Industrial Relations as a Field”. Industrial and Labor Relations Review. 2000;53(3):482–502. [Google Scholar]
- Gowen CR, McFadden KL, Tallon WJ. “On the Centrality of Strategic Human Resource Management for Healthcare Quality Results and Competitive Advantage”. Journal of Management Development. 2006;25(8):806–26. [Google Scholar]
- Harley B, Allen BC, Sargent LD. “High Performance Work Systems and Employee Experience of Work in the Service Sector: The Case of Aged Care”. British Journal of Industrial Relations. 2007;45(3):607–33. [Google Scholar]
- Harmon J, Scotti DJ, Behson S, Farias G, Petzel R, Neuman JH, Keashly L. “Effects of High-Involvement Work Systems on Employee Satisfaction and Service Costs in Veterans Healthcare”. Journal of Healthcare Management. 2003;48(6):393–406. [PubMed] [Google Scholar]
- Hartig M, Engle V, Graney M. “Accuracy of Nurse Aides’ Functional Health Assessments of Nursing Home Residents”. Journals of Gerontology Series A. 1997;52(3):M142–8. doi: 10.1093/gerona/52a.3.m142. [DOI] [PubMed] [Google Scholar]
- Howe C. “Love, Money, or Flexibility: What Motivates People to Work in Consumer-Directed Home Care?”. Gerontologist. 2008;48(suppl. 1):46–60. doi: 10.1093/geront/48.supplement_1.46. [DOI] [PubMed] [Google Scholar]
- Huselid M. “The Impact of Human Resource Management Practices on Turnover, Producitivity, and Corporate Financial Performance”. Academy of Management Journal. 1995;38:635–72. [Google Scholar]
- Jaccard J, Wan C, Turrisi R. “The Detection and Interpretation of Interaction Effects between Continuous Variables in Multiple Regression”. Multivariate Behavioral Research. 1990;25(4):467–78. doi: 10.1207/s15327906mbr2504_4. [DOI] [PubMed] [Google Scholar]
- Lepak DP, Snell S. “Examining the Human Resource Architecture: The Relationships among Human Capital, Employment, and Human Resource Configurations”. Journal of Management. 2002;28(4):517–43. [Google Scholar]
- Longest K, Vaisey S. “Fuzzy: A Program for Performing Qualitative Comparative Analyses (QCA) in Stata”. Stata Journal. 2008;8(1):79–104. [Google Scholar]
- MacDuffie J. “Human Resource Bundles and Manufacturing Performance: Organizational Logic and Flexible Production Systems in the World Auto Industry”. Industrial and Labor Relations Review. 1995;48(2):197–221. [Google Scholar]
- Macky K, Boxall P. “The Relationship between High-Performance Work Practices and Employee Attitudes: An Investigation of Additive and Interaction Effects”. International Journal of Human Resource Management. 2007;18(4):537–67. [Google Scholar]
- McAlearney A, Garman A, Song P, McHugh M, Robbins J, Harrison M. “High-Performance Work Systems in Health Care Management, Part 2: Qualitative Evidence from Five Studies”. Health Care Management Review. 2011;36(3):214–26. doi: 10.1097/HMR.0b013e3182100dc4. [DOI] [PubMed] [Google Scholar]
- McGovern P, Stiles P. “Human Resource Management on the Line”. Human Resource Management Journal. 1997;7(4):12–29. [Google Scholar]
- Meyer A, Tsui A, Hinings C. “Configurational Approaches to Organizational Analysis”. Academy of Management Journal. 1993;36(6):1175–95. [Google Scholar]
- Morgan J. “Just a Job? A Mixed Method Analysis of the Work Situation of Direct Care Workers in Long-Term Care Settings”. Dissertation Abstracts International. 2005;66:09A. [Google Scholar]
- Morgan J, Konrad T. “A Mixed-Method Evaluation of a Workforce Development Intervention for Nursing Assistants in Nursing Homes: The Case of WIN A STEP UP”. Gerontologist. 2008;48(1):71–9. doi: 10.1093/geront/48.supplement_1.71. [DOI] [PubMed] [Google Scholar]
- Pearson S, Schneider E, Kleinman K, Coltin K, Singer J. “The Impact of Pay-for-Performance on Health Care Quality in Massachusetts, 2001-2003”. Health Affairs. 2008;27(4):1167–76. doi: 10.1377/hlthaff.27.4.1167. [DOI] [PubMed] [Google Scholar]
- Petrova M, Vail L, Bosley S, Dale J. “Benefits and Challenges of Employing Health Care Assistants in General Practice: A Qualitative Study of GP and Practice Nurses Perspectives”. Family Practice. 2010;27(3):303–11. doi: 10.1093/fampra/cmq011. [DOI] [PubMed] [Google Scholar]
- Pfeffer J. Competitive Advantage through People: Unleashing the Power of the Workforce. Cambridge, MA: Harvard Business School Press; 1996. [Google Scholar]
- Preuss G. “High Performance Work Systems and Organizational Outcomes: The Mediating Role of Information Quality”. Industrial and Labor Relations Review. 2003;56(4):590–605. [Google Scholar]
- Ragin C. The Comparative Method: Moving Beyond Qualitative and Quantitative Strategies. Berkeley, CA: University of California Press; 1987. [Google Scholar]
- Ragin C. “The Distinctiveness of Case-Oriented Research”. Health Services Research. 1999;34(5):1137–51. [PMC free article] [PubMed] [Google Scholar]
- Ragin C. “Measurement versus Calibration: A Set-Theoretic Approach”. In: Box-Steffensmeier J, Brady H, Collier D, editors. Oxford Handbook of Political Methodology. Oxford, UK: Oxford University Press; 2008a. pp. 174–98. [Google Scholar]
- Ragin CC. Redesigning Social Inquiry: Fuzzy Sets and Beyond. Chicago, IL: University of Chicago Press; 2008b. [Google Scholar]
- Ramirez M, Guy F, Beale D. “Contested Resources: Unions, Employers, and the Adoption of New Work Practices in U.S. and U.K. Telecommunications”. British Journal of Industrial Relations. 2007;45:497–517. [Google Scholar]
- Rihoux B, Ragin C. Configurational Comparative Methods: Qualitative Comparative Analysis (QCA) and Related Techniques. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- Schindel J, Cherner D, O'Neil E, Solomon K, Immartino B, Santimauro J. Workers Who Care: A Graphical Profile of the Frontline Health and Health Care Workforce. San Francisco, CA: Health Workforce Solutions; 2006. [Google Scholar]
- Sikorska-Simmons E. “Linking Resident Satisfaction to Staff Perceptions of the Work Environment in Assisted Living: A Multilevel Analysis”. Gerontologist. 2006;46(5):590–8. doi: 10.1093/geront/46.5.590. [DOI] [PubMed] [Google Scholar]
- Smithson M, Verkuilen J. Fuzzy Set Theory: Applications in the Social Sciences. Thousand Oaks, CA: Sage Publications; 2006. [Google Scholar]
- Standing H, Chowdhury A. “Producing Effective Knowledge Agents in a Pluralistic Environment: What Future for Community Health Workers?”. Social Science and Medicine. 2008;66:2096–107. doi: 10.1016/j.socscimed.2008.01.046. [DOI] [PubMed] [Google Scholar]
- Sullivan J. Rethinking Strategic HR: HR's Role in Building a Performance Culture. Chicago, IL: CCH Incorporated; 2004. [Google Scholar]
- West MA, Guthrie JP, Dawson J, Borrill C, Carter M. “Reducing Patient Mortality in Hospitals: The Role of Human Resource Management”. Journal of Organizational Behavior. 2006;27(7):983–1002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


