Abstract
Socioeconomic status, though a robust and strong predictor of health, has generally been unable to fully explain the health gap between blacks and whites in the United States. However, at both the individual and neighborhood levels, socioeconomic status is often treated as a static factor with only single-point-in-time measurements. These cross-sectional measures fail to account for possible heterogeneous histories within groups who may share similar characteristics at a given point in time. As such, ignoring the dynamic nature of socioeconomic status may lead to the underestimation of its importance in explaining health and racial health disparities.
In this study, I use national longitudinal data to investigate the relationship between neighborhood poverty and respondent-rated health, focusing on whether the addition of a temporal dimension reveals a stronger relationship between neighborhood poverty and health, and a greater explanatory power for the health gap between blacks and whites. Results indicate that long-term neighborhood measures are stronger predictors of health outcomes and explain a greater amount of the black/white health gap than single-point measures.
Keywords: racial health disparities, neighborhood effects, USA, socioeconomic status (SES), longtitudinal
Introduction
Prior investigations have consistently shown that socioeconomic status and its differential distributions across race are key determinants of health and racial health disparity (Haan & Kaplan, 1986; Adler, Boyce, Chesney, Folkman & Syme, 1993; Adler, Boyce, Chesney, Cohen, Folkman, Kahn, et al. 1994). However, adjusting for demographic and socioeconomic characteristics has generally been unable to fully account for the health disparity between non-Hispanic blacks and non-Hispanic whites (henceforth referred to as blacks and whites, respectively) in the United States (Williams & Collins, 1995, 2001). The persistence of this unexplained gap has led to an increased attention to differences in residential living conditions as a contributing factor to the health disparities between blacks and whites (House & Williams, 2000).
Blacks, contrasted with other minority groups such as Asians and to a lesser extent Hispanics, are least likely to be able to translate socioeconomic success into residential mobility to more affluent neighborhoods (Alba & Logan, 1993; Rosenbaum & Friedman, 2001). As a consequence of discrimination, equitable access to residential neighborhoods has been denied to blacks, restricting their choices of neighborhoods to those that are often less desirable and divergent from their socioeconomic attainment (Alba, Logan & Bellair, 1994; Logan & Alba, 1995). That is, blacks are disproportionately exposed to areas of concentrated poverty characterized by diminished quality of the social and economic environments, high rates of neighborhood turnover and mobility, crime, and social disorder (Sampson, Raudenbush & Earls, 1997). Residing in disadvantaged socioeconomic neighborhoods, in turn, has been consistently shown to be associated with adverse health outcomes including mortality, low birthweight, and infant mortality (Morenoff & Lynch, 2004; Yen & Kaplan, 1999; Yen & Syme, 1999; Kawachi & Bekrman, 2003; Pickett & Pearl, 2001; Robert, 1999).
However, socioeconomic status, at both the individual and neighborhood levels, is often treated as a static factor with only single-point-in-time measurements. These cross-sectional measures fail to account for possible heterogeneous histories within groups who may share similar characteristics at a single-point-in-time. Given that long exposures to poverty have been found to have more profound impacts than short exposures (Malat, Oh & Hamilton, 2005; McDonough, Sacker & Wiggins, 2005) and that the duration of exposure greatly differs between blacks and whites (McDonough, et al. 2005; Quillian, 2003), ignoring the dynamic nature of these factors may lead to the underestimation of the importance of both in explaining health and racial health disparities. In this paper, I use longitudinal data to investigate the relationship between individual and neighborhood poverty on health, focusing on whether the addition of a temporal dimension reveals a stronger relationship between neighborhood poverty and health and whether it provides a greater explanatory power for the health gap between blacks and whites over adjustments of single-point measures of socioeconomic status.
The Dynamic Nature of Individual and Neighborhood Characteristics
The importance of the temporal dimension over a life-course is especially salient if one considers the dynamic nature of financial resources. Although one’s real income is expected to rise with accumulation of experience and expertise in the workforce, there may be considerable volatility over a lifetime (Duncan, 1988; Solon, 1992; Zimmerman, 1992). Rank & Hirschl (2001) estimate that half of Americans will experience either poverty or affluence at least one year between the ages of twenty-five & seventy-five while only 20 percent will experience neither end of the economic spectrum. Temporary or short-term fluctuations may be a consequence of job loss or exit from the labor force for various reasons, such as returning to school. Similarly, income spikes may reflect a transition into a different field, re-entry into the labor force after a spell of unemployment, or initial employment upon completion of school. Cross-sectional data are ill-equipped to adjust for these life-course changes.
Within a lifetime, drops in income may cause some to fall into poverty. However, the condition of poverty is not an absorbing state. To the extent that income fluctuates, individuals may also cross the threshold into and out of the dichotomous classification of poverty multiple times over the life-course (Stevens, 1994). For example, thirty-five percent of those who were poor in 1996 were above the poverty threshold the next year and almost half climbed out of poverty after three years (Iceland, 2003). Thus, a single-point-in-time measurement of even an extremely coarse category such as poverty status may not accurately reflect an individual’s long-term condition.
As individual-level characteristics may change, so may the context of neighborhoods where one resides. This may be due to a slow process of neighborhood gentrification or deterioration over time or a more abrupt change when individuals move residential locations. Evidence with respect to the stability of individuals’ neighborhood environments over time is mixed. Kunz, Page & Solon (2003) estimate that childhood neighborhood characteristics exhibit high consistency over the five-year timeframe observed. The correlation between the five-year averages of log mean neighborhood income and single-year values is between 0.83 and 0.96, depending on the restriction of the sample to only movers versus all children, respectively. The high correlations suggest that a snap shot of an individual’s neighborhood context may not be such an inaccurate reflection of his long-term neighborhood environment. In contrast, several other investigations into neighborhood stability, using longer time frames suggest a different conclusion (Quillian, 2003; Timberlake, 2003; Massey, Gross & Shibuya,. 1994; Gramlich, Laren & Sealand, 1992). Gramlich and collegues (1992) find a great deal of neighborhood heterogeneity even in poor adults, with a quarter of them entering and leaving extremely poor urban neighborhoods (defined as Census tracts with poverty rate greater than 30%) in a year. However, using a dichotomous measure of neighborhood poverty may give a misleading picture if individuals who cross over the poverty threshold into or out of poor neighborhoods experience only a marginal change in neighborhood circumstance. This does not seem to be the case. Quillian (2003) estimates that among individuals who move into or out of poor neighborhoods (defined as Census tracts with poverty rate greater than 20%), the difference in neighborhood poverty rates is substantial. For those moving into or out of poor neighborhoods, the average change in neighborhood poverty rate is approximately 18 percent; changes among non-movers are smaller, from 0.6 to 2 percent. However, Quillian (2003) notes that these minor single year changes usually represented a progression towards neighborhood gentrification or deterioration that required several years to complete.
The Temporal Dimension of Individual and Neighborhood Poverty and Its Association with Health
The dynamic nature of both individual and neighborhood socioeconomic levels may be a crucial component to understanding health, neighborhood context, and their intersection. An extensive line of research has documented a strong association between individual-level socioeconomic status and health outcomes (Haan & Kaplan, 1986; Adler et al., 1993, 1994; Pappas, Queen, Hadden & Fisher, 1993). Those with less education and financial resources exhibit disproportionately worse health outcomes across all levels of the socioeconomic gradient, not just at the lower end of the distribution (Adler et al., 1993). However, relatively few studies have distinguished between chronic and transient spells of poverty and their association with health. The handful of studies that have investigated the impact of varying durations of income level or poverty on individuals’ well-being consistently find that longer term spells of financial hardship have a greater negative impact on health than shorter term spells (Malat et al., 2005; McDonough et al., 2005; McDonough & Berglund, 2003; Duncan, Brooks-Gunn & Klebanov, 1994; Korenman, Miller & Sjaastad, 1995). Equally important, current economic circumstances do not erase the impact of earlier poverty experiences on health (Malat et al., 2005; McDonough & Berglund, 2003) and estimates based on long-term poverty are greater than those based on single-year measures (Korenman et al., 1995). These findings suggest that long-term measures of financial resources may be better predictors of health than single-year measures (Benzeval & Judge, 2001; Korenman et al., 1995; but see McDonough, Duncan, Williams & House, 1997).
Though there has been less work on whether varying durations of neighborhood poverty exposure differentially affect health, findings from the few studies that have done so suggest that the impact of neighborhood context increases with duration of exposure (Turley 2003; Ross, Reynolds & Geiss 2000). For example, Ross et al. (2000) find that the length of time in a poor neighborhood is positively related with increased depression and anxiety of residents. Their findings suggest that the effects of risk exposure on health, whether they exist at the individual or neighborhood level, are cumulative. That is, a superficial exposure to neighborhood poverty would exert minimal effects on health while a persistent, life-long exposure may exert significant detrimental health effects that have been compounded over time. Cross-sectional measures that fail to distinguish between exposure lengths may lead to noisy proxies for long-term neighborhood conditions and consequently, attenuated estimates of neighborhood effects.
Race, Duration of Exposure to Poverty, and Racial Health Disparity
The temporal dimension of individual and neighborhood poverty is closely intertwined with race and by extension, racial health disparity. Research consistently finds that blacks are more likely to experience chronic poverty, with significantly longer spells, lower exit rates, and higher re-entry rates than whites (Iceland, 2003; Stevens, 1999; McDonough et al., 2005). The longitudinal pattern of neighborhood poverty exposure across racial groups parallels that for individual-level poverty duration. That is to say, not only do blacks have longer durations of poverty spells, they also spend a disproportionate time in poorer neighborhoods than comparable whites (Quillian, 2003; Timberlake, 2003; Sharkey, 2008).
Using the Panel Study of Income Dynamics (PSID), Quillian (2003) estimates the average tenure for those who enter poor neighborhoods (defined as Census tracts with poverty rate greater than 20%) is 8.5 years for whites and 11.8 years for blacks. The exit rate after one year is 30 percent for whites and only 18 percent for blacks. South and Crowder (1997), using a shorter time frame of the PSID, also find a differential entry and exit rate between blacks and whites. The rate of entry into poor neighborhoods for blacks residing in non-poor tracts in any given year is 11 percent, compared to 1.4 percent for whites. Exit rates are 6.7 percent and 16.7 percent for blacks and whites, respectively.
The notions that both individual and neighborhood poverty may exert their effects on health through duration of exposure and that there are differences in length of exposure across race, suggest a potential explanation for why a significant portion of black/white health disparities, net of single-point measures of socioeconomic differences, remains unexplained. If we interpret the race residual as the racial disparity in health that cannot be accounted for by differences in socioeoconomic status, then we can view the point estimate for race as a potentially biased estimation of that disparity. That is, given that the length of poverty exposure (at both the individual and neighborhood levels) is positively correlated to both poor health and being black, the level of racial disparities that cannot be accounted for by socioeconomic circumstances may have been overestimated. Accounting for the temporal dimension in both individual and neighborhood factors may provide an additional explanation to the black/white health disparity that has been thus far largely ignored.
RESEARCH OBJECTIVES
This paper has several objectives:
To examine whether multiple-year measures of neighborhood context are stronger predictors of health than single-year measures.
To examine whether longer durations of neighborhood poverty exposure have a larger association with health than shorter exposures.
To examine whether the black/white health gap, net of single-point-in-time measures of SES, is further explained with the inclusion of multiple-year measures of individual income and neighborhood context
Analytical Strategy
Using longitudinal data, I begin with a simple descriptive analysis that examines whether single-point measures of income and neighborhood poverty are suitable proxies for long-term conditions. I then estimate a series of multivariate regression models that explore the associations between family income, neighborhood poverty, and health. The base model adjusts for only single-point measures of individual-level SES. Subsequent models add on multiple-year measures of income, then single-point measures of neighborhood poverty, then multiple-year measures of neighborhood poverty. The race residuals and point estimates of neighborhood poverty, when applicable, are compared across the models.
DATA AND MEASURES
Analyses are based on data from the years 1980–1996 of the Panel Study of Income Dynamics (PSID). The PSID is a longitudinal study of a nationally representative sample of the non-immigrant U.S. population, annually collecting an extensive list of socioeconomic information as well as some health measures.
I use a restricted version of the PSID that includes respondents’ census tracts of residence, employed as rough proxies of neighborhoods in this study, during the time of interview. (Although I use the term “neighborhood” in referring to census tracts because it has been extensively used in the neighborhood-health literature, it is not without the recognition that the designation of census tracts as neighborhoods is not ideal and may not adequately capture respondents’ notion of their neighborhood or account for the differential spatial distribution of residents within census tracts.) Census tract poverty measures were extracted from the Geolytics’ Neighborhood Change Database (NCDB) which contains decennial census tract level measures for years 1980, 1990, and 2000 and linked to each respondent-year observation via 2000 tract identifiers. A unique feature of the NCDB is that it offers tract level information for all three decades normalized to 2000 tract boundaries. Because tract boundaries change across decennial census, variations in tract demographics due to boundary adjustments may be spuriously attributed to compositional changes. Consequently, normalization of tract boundaries is a critical adjustment to increase the measurement accuracy of neighborhood trends by minimizing the noise produced by boundary changes. I estimate neighborhood conditions between decennial census years by linearly interpolating across decennial tract measures.
Health Measure
I use respondent-rated health, as measured in 1996, as the health outcome. Respondent-rated health, collected only for heads and spouses of heads in the PSID, was measured on a five-point scale: fair, poor, good, very good, and excellent. I dichotomize the measure to poor health (fair/poor=1) and good health (good/very good/excellent=0). Although not an objective measure, respondent-rated health has been shown to be a strong predictor of mortality, net of adjustments for clinical measures of health status (Benyamini and Idler, 1999; Idler and Benyamini, 1997). Moreover, this association is similar for blacks and whites (McGee, Liao, Cao, & Cooper 1999).
Socio-economic Measures
Individual-level socioeconomic and demographics adjustments, as measured in 1996, include marital status, education, labor force status, race, gender, and age. Marital status is divided into three categories: single, married, and other (divorced, separated, widowed). Educational attainment represents the years of schooling attended (fewer than 12, 12, 13–15, 16, and 17+). Labor force categories include the employed, the unemployed, and the labor force non-participants. Age is measured continuously. Family poverty income ratio and neighborhood poverty levels are derived from 1996 single-point observations and 1980–1996 multiple-year observations. The family poverty income measure is grouped into four categories: family poverty income ratio less than 1, family poverty income ratio between 1 and 2, family poverty income ratio between 2 and 3, and family poverty income ratio 3 or higher. Neighborhood poverty levels are classified into three categories: less than 10 percent poor (affluent), 10 to 20 percent poor (mixed), and 20 percent or more poor (poor). For multiple-year measures of family poverty income and neighborhood poverty levels, annual measures are averaged across the years and then classified into the appropriate levels. I also include wealth (net family assets) quintiles, as measured in 1994, as an additional adjustment for economic level.
The analysis sample is restricted to black and white respondents who are either the household head or spouse and at least 18 years of age in 1996 and have at least one year of nonmissing family poverty income ratio and tract-level poverty rate between 1980 and 1995. The resulting sample size is comprised of 10,013 individuals, with information on personal income and neighborhood context as far back as 1980. Table 1 provides descriptive statistics of the total sample and by race.
Table 1.
Descriptive Statistics of the PSID Sample (1980–1996)‡
| Characteristics | Full Sample | White | Black |
|---|---|---|---|
| N | 10,013 | 6,765 | 3,248 |
|
| |||
| % | % | % | |
| Gender | |||
| Female | 55.89 | 53.53 | 60.81 |
| Male | 44.11 | 46.47 | 39.19 |
| Mean Age | 46.56(14.35) | 47.06(14.64) | 45.52(13.69) |
| Race | |||
| White | 67.56 | ||
| Black | 32.44 | ||
| Family Poverty Income Ratio | |||
| 100% Or Less | 10.56 | 4.75 | 22.66 |
| 100% to 200% | 16.11 | 12.20 | 24.26 |
| 200% to 300% | 16.60 | 16.01 | 17.83 |
| Over 300% | 56.74 | 67.05 | 35.25 |
| Marital Status | |||
| Married | 70.82 | 79.14 | 53.48 |
| Single | 8.57 | 4.67 | 16.69 |
| Other | 20.61 | 16.19 | 29.83 |
| Education Level | |||
| <12 Years | 22.21 | 16.73 | 33.62 |
| 12 Years | 35.70 | 35.67 | 35.78 |
| 13 to 15 Years | 22.16 | 22.14 | 22.20 |
| 16 Years | 11.82 | 14.93 | 5.36 |
| 17+ Years | 8.10 | 10.52 | 3.05 |
| Labor Force Status | |||
| Employed | 67.47 | 69.83 | 62.56 |
| Unemployed | 3.87 | 2.35 | 7.05 |
| Not In The Labor Force | 28.65 | 27.82 | 30.39 |
| Tract Poverty | |||
| 1996 Tract <10% Poor | 46.00 | 58.94 | 19.06 |
| 1996 Tract 10%to20% Poor | 30.70 | 31.53 | 28.97 |
| 1996 Tract 20%+ Poor | 23.30 | 9.53 | 51.97 |
| Mean 1980–1996 Ave Tract Poverty Rate | 14.66 (10.77) | 10.15 (6.56) | 24.06 (11.71) |
| Mean 1980–1996 Percent Time in Poor Tract | 25.21 (36.73) | 10.32 (24.31) | 56.21 (38.80) |
| 1994 Average Wealth ($) | 141,822 (416,304) | 191,234 (495,299) | 38,906 (87,570) |
| Health Status | |||
| Poor Health | 17.02 | 12.77 | 25.86 |
| Good Health | 82.98 | 87.23 | 74.14 |
All characteristics, unless otherwise noted, are measured in 1996.
Note: Standard deviation in parenthesis
ANALYSIS
Descriptive Analyses
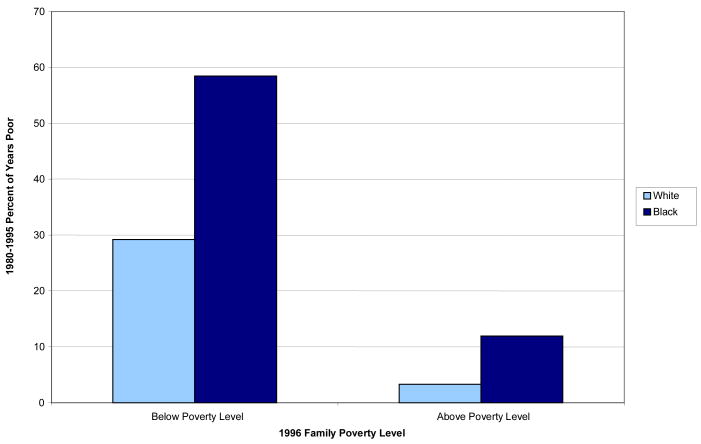
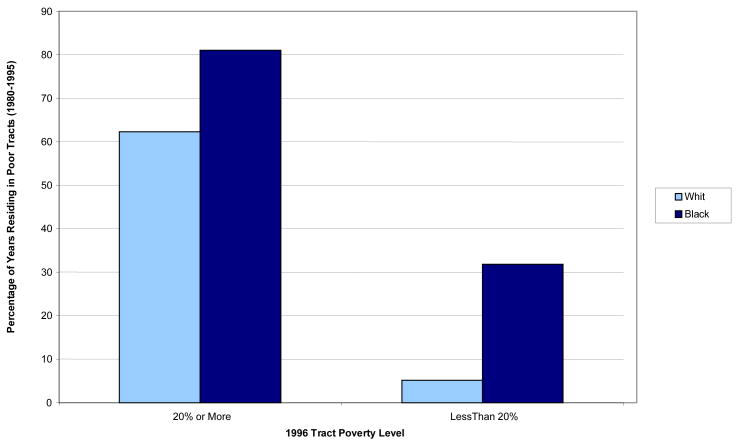
I begin with exploratory descriptive analyses investigating the relationship between race, duration of poverty, and duration of residing in poor neighborhoods. Simple bivariate analyses reveal that single-point adjustments for family income do not account for the very different economic histories between blacks and whites. Blacks who fell under the poverty threshold in 1996 had experienced durations of poverty that were twice as long as those experienced by comparable whites (Figure 1). This suggests that single-point measures of poverty status may be more accurate proxies for long-term conditions for blacks than for whites. A parallel analysis for neighborhood poverty rate shows a similar pattern. On average, black individuals who resided in a poor neighborhood in 1996 had spent approximately 80 percent of the years between 1980 and 1995 in poor neighborhoods (Figure 2). Comparable whites had spent approximately 63 percent of those years in poor neighborhoods. Moreover, blacks who resided in non-poor neighborhoods in 1996 had spent over 30 percent of their time in poor neighborhoods between 1980 and 1995, compared to approximately only 5 percent for whites.
Figure 1.
Bivariate Analysis of Percent of Years Poor between 1980–1995 by 1996 Family Poverty Status and Race in the PSID (1980–1996)
Note: Analysis restricted to respondents with at least six years of nonmissing family income values between 1980–1995.
Figure 2.
Bivariate Analysis of Proportions of Years Resided In a Poor Neighborhood between 1980–1995 by 1996 Neighborhood Poverty Level and Race in the PSID (1980–1996)
Note: Analysis restricted to respondents with at least six years of nonmissing tract poverty values between 1980–1995.
These descriptive analyses suggest that: 1) the accuracy of single-point measures in capturing long-term individual-level poverty differs by racial group, with a larger proportion of transient poor whites being classified as chronically poor and 2) the accuracy of single-point measures in capturing long-term neighborhood conditions differs by racial group, with a larger proportion of whites residing in a poor neighborhood in a given year experiencing better neighborhood environments in the long run. This pattern, consistent with studies that found blacks were more likely to experience chronic poverty and long-term exposure to high neighborhood poverty compared to whites, supports the hypothesis that racial health disparities, independent of socioeconomic conditions may be overestimated when only single-point-in-time measures for individual and neighborhood economic conditions are used to account for the differences in socioeconomic characteristics between blacks and whites. However, these are only bivariate statistics and do not adjust for other socioeconomic characteristics (e.g., education, marital status, employment status) between blacks and whites that are associated with income and neighborhood socioeconomic level. The magnitude in the heterogeneity of the socioeconomic histories between blacks and whites may be attenuated once other single-point measures are accounted for.
Multivariate Analysis
In the following sections, I estimate a series of multivariate regression models to empirically examine whether the inclusion of a temporal dimension further accounts for the racial health gap, net of single-point measures of socioeconomic factors. For each of my analysis, I conduct a logistic regression model with a binary outcome measure of respondent reported poor health. Controls for gender, age, education, employment, and marital status, as previously defined, are included throughout. For models that include multiple-point measures of income or neighborhood poverty, I include a series of binary indicators that account for the number of years in which family income and neighborhood poverty is observed. All analyses adjust for clustering at the family level.
Single-Point versus Long-Term Measures of Family Income
To test whether adjusting for long-term economic measures account for a larger portion of the racial health disparity than single-point measures, I begin with a base model (Model 1) with only year 1996 single-point measures of socioeconomic and demographic conditions. In the next model (Model 2), I use 1980–1996 average family poverty income as a long-term measure of economic means and compare estimates of single-point versus long-term measures of income on health. Finally, I add wealth levels in Model 3 as an additional control for long-term economic means.
Single-point versus Long-Term Measures of Neighborhood Context
The modeling sequence to determine the impact of adjusting for long-term measures of neighborhood context versus single-point measures follows the same strategy used in the family income models. The base model accounts for only current family income and current neighborhood poverty level (Model 4A). To test the hypothesis that a multiple-year measure of neighborhood context is a stronger predictor of health than a single-year measure, I compare estimates of the impact of single-point measures of neighborhood poverty categories (Model 4A) to 1980–1996 average measures (Model 5A). Each primary model (e.g., Model 5A), is followed by a secondary model (e.g., Model 5B) which uses a longer-term measure for economic sufficiency. In the secondary models, single-point measures of family income are replaced with 1980–1996 averages and wealth is added as an additional control. Accounting for long-term economic conditions reduces the likelihood that the observed association between health and neighborhood context is due to poorly measured levels of economic sufficiency.
Transient versus Persistent Exposure to Neighborhood Poverty
Although long-term averages may better capture long-term conditions than single-point measures, averages may mask large variances in neighborhood context. For example, averaging may mask exposure to poor neighborhoods if residents also resided in middle-income neighborhoods for some time. Hence, averaging may not be the most appropriate strategy to summarize an individual’s exposure to neighborhood poverty. Consequently, I also employ two alternative specifications for neighborhood poverty: a continuous and discrete measurement for length of exposure to poor neighborhoods. The continuous measure is defined as the proportion of years the respondent resided in a poor neighborhood during the timeframe of observation and is entered into the model as a linear specification. The discrete measure is divided into three categories: never exposed transient exposure, and persistent exposure. The “never exposed” category is the reference category and is defined as never having been observed to reside in a poor neighborhood. Transient exposure to neighborhood poverty is defined as residing in a poor neighborhood for less than 50 percent of the time; conversely, residing in a poor neighborhood for over half of the time is considered to be a persistent exposure.
For both the continuous and discrete measures of exposure to poor neighborhoods, I estimate a logistic model that adjusts for the amount of exposure to poor neighborhoods between 1980 and 1996 while adjusting for single-point measures of family income (Model 6A & 7A). As in the previous section, each primary model is followed by a secondary model that replaces 1996 single-point measures of family income with 1980–1996 averages and adds wealth to the list of covariates.
RESULTS
Model results for family income reveal the expected negative association between income and poor health (Table 2). Moreover, long-term measures of income reveal a stronger association with health than single-year measures. These patterns are consistent with results from previous studies (Benzeval & Judge, 2001; Korenman et al., 1995).
Table 2.
Logistic Regression Results of Single and Multiple Year Measures of Family-level Poverty on 1996 Poor Health in the PSID, 1980–1996 ±
| Characteristics | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
|
|
|||
| OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| Race [Reference: White] | |||
| Black | 1.61** [1.39, 1.87] | 1.47** [1.26, 1.71] | 1.34** [1.15, 1.57] |
| 1996 Family Poverty Income Ratio [Reference: Over 300%] | |||
| 100% Or Less | 2.54** [2.05, 3.15] | ||
| 100%to200% | 2.23** [1.86, 2.67] | ||
| 200%to300% | 1.42** [1.17, 1.72] | ||
| 1980–1996 Ave Family Poverty Income Ratio [Reference: Over 300%] | |||
| 100% Or Less | 3.06** [2.35, 4.00] | 2.31** [1.73, 3.08] | |
| 100%to200% | 2.83** [2.35, 3.42] | 2.24** [1.83, 2.74] | |
| 200%to300% | 1.65** [1.38, 1.98] | 1.38** [1.14, 1.67] | |
| Wealth Quintiles [Reference: Quintile 5] | |||
| Quintile 1 | 2.30** [1.75, 3.03] | ||
| Quintile 2 | 1.99** [1.53, 2.58] | ||
| Quintile 3 | 1.57** [1.23, 2.02] | ||
| Quintile 4 | 1.36** [1.08, 1.70] | ||
**Statistically Significant at the 1% Level,
Statistically Significant at the 5% Level
Accounting for the economic history of individuals substantially reduced the unexplained racial health disparity observed in Model 1. The inclusion of long-term (1980–1996 average) income measures in Model 2 yielded statistically significant reductions in the black/white disparity estimates, from OR=1.61 to 1.47. The additional adjustment for wealth reduced the health gap further to OR=1.34. In the logit metric, this represents a 39 percent reduction in the unexplained disparity (from 0.48 to 0.29). The remaining racial health gap is still highly statistically significant, indicating that adjustments for long-term measures of individual socioeconomic factors still do not fully account for why blacks disproportionately experience poor health.
Results from the neighborhood poverty models yielded a similar pattern to the results from the family income models. The cross-sectional specification (Model 4A) showed a significant positive association between neighborhood poverty level and poor health; compared to individuals residing in affluent neighborhoods, individuals residing in mixed neighborhoods have a 24 percent greater odds of reporting poor health while those residing in poor neighborhoods have a 20 percent greater odds (though not statistically significant) of reporting poor health.. Comparing results from Model 1, the additional adjustment for neighborhood poverty does not provide any additional explanation for the black/white health gap. Notably, replacing single-point measures of family income with multiple-year averages and adding wealth eliminates any significant association for the single-point measure of poor neighborhood (Model 4B). This suggests that the significant neighborhood estimates based on cross-sectional data may be due to imperfect measures of individual-level attributes. However, single-point measures of neighborhood context may be poor proxies for long-term neighborhood environment, attenuating the association towards the null. Indeed, multiple-point measures of neighborhood poverty levels show a significant association with health that are larger in magnitude than the single-point measures (Model 5A) and were robust to the inclusion of long-term measures of personal income (Model 5B). In addition, accounting for long term conditions of both family income and neighborhood poverty reduced the unexplained racial health gap from OR=1.61 to OR=1.26. In the logit metric, this represents a 51 percent reduction in the unexplained disparity (from 0.48 to 0.23).
Model results for duration in poor neighborhoods show a marginally insignificant association (p-value=0.72) between duration in poor neighborhoods and likelihood of reporting poor health (Model 6A). A persistent residence in poor neighborhoods is associated with poor health while a transient residence showed no significant association (Model 7A). However, the association between persistent exposure to neighborhood poverty and poor health became insignificant once long-term measures of personal income were controlled for (Model 7B). With respect to the racial health disparity, duration in neighborhood poverty did not provide any further explanation to the black/white health gap (Model 3 vs 6B and 7B).
DISSCUSSION AND CONCLUSION
The results of the analyses using multiple-point measures of family income and neighborhood poverty suggest that cross-sectional analyses of neighborhood-effects are subject to two sources of bias that work in opposing directions. First, estimates of neighborhood-effects are inflated when single-point measures of income are used to adjust for financial viability. When long-term measures (multiple-year averages) and wealth were controlled for, the neighborhood estimates are significantly attenuated and the single-point estimates of neighborhood poverty become non-significant. The sensitivity of the neighborhood poverty estimates to the inclusion of longer term measures of personal attributes reflects the most often voiced concern regarding cross-sectional studies of neighborhood-effects. That is, neighborhood-level estimates may be reflections of omitted variable bias or measurement error at the individual-level rather than contextual influences. The inability of the single-point neighborhood poverty estimates to retain their statistical significance when wealth and longer-term measures of family income are included as additional adjustments for compositional heterogeneity across neighborhoods suggest that much of the so-called neighborhood effects found in previous cross-sectional studies that relied on only single-point measures of income may be more of an artifact of variable omission and measurement error at the individual level. At the same time, the consistent increase in the magnitude of neighborhood estimates when multiple-year measures of neighborhood poverty are used reveal that single-point measures of neighborhood poverty level are also noisy proxies for long-term neighborhood context that have led to downwardly biased estimates of neighborhood effects. For the general case, the net bias due to these two sources based on theoretical grounds may be impossible to determine. However, at least in this study, the association between long-term measures of neighborhood poverty and poor health were robust to the inclusion of wealth and long-term measures of income. Compared to studies using cross-sectional data, these results provide stronger evidence that neighborhood context does indeed impact health.
As opposed to single-point measures, long-term neighborhood measures of neighborhood poverty may better capture the cumulative wear and tear and “weathering” effects (Geronimus, 1992) experienced by residents chronically exposed to disadvantaged environments. These influences on health may be more independent of personal level of socioeconomic status. Less likely to reflect long-term conditions, single-point measures of neighborhood poverty, may be only able to capture the influences of neighborhood context that are quickly mutable, such as health behaviors (e.g., smoking, exercising, diet). The health impact of these may also take some time to manifest and may not be readily discernable in cross-sectional analyses.
The ambiguity regarding the net direction of bias of cross-sectional neighborhood estimates from these two sources reflect the enormous and possibly insurmountable complexity in recovering causal estimates of neighborhood context. In addition to issues regarding measurement error and omission of individual factors, analysts need to be concerned about the possible bias induced by adjusting for individual-level attributes routinely treated as confounders, such as income and education, that may have been influenced by past neighborhood conditions. These factors may arguably be also considered intermediate variables in the pathway between neighborhood context and health. Adjusting for such variables may lead to severely overly conservative estimates of neighborhood influences on health while omitting them would certainly lead to criticisms of under-adjustment of individual-level heterogeneity.
Adjusting for long-term measures of neighborhood poverty further explained over 20 percent of the remaining black/white health gap that remained unexplained after wealth and long-term measures of income were controlled for. In comparison, adjusting for single-point neighborhood poverty provided no further explanation. This suggests that there existed a great deal of heterogeneity in neighborhood context histories between blacks and whites that was not adequately captured by single-point adjustments and analyses using single point neighborhood data have considerably underestimated the degree of neighborhood disadvantage experienced by blacks, compared to whites. Further, the nontrivial reduction in the race residual indicates that chronic exposure to poor neighborhoods by blacks may be a significant determinant of the black/white health gap and suggests multi-level sources for the persistence of the health disadvantage shouldered by blacks.
From an even broader perspective, this study’s finding that chronic exposure to neighborhood poverty helps explain the black/white health disparity underscores the multi-dimensional and enduring consequences of racial segregation in America. Racial segregation, in spatially isolating blacks and creating areas of concentrated poverty, has disproportionately exposed blacks to distressed social, economic, and physical environments (Massey & Denton, 1993; Massey & Fischer, 2000) that cannot be explained away by differences in socioeconomic status (Alba & Logan, 1993; South & Crowder, 1997; Rosenbaum & Friedman, 2001; Acevedo-Garcia, Osypuk, McArdle & Williams, 2008; Sharkey, 2008). Given that segregation exposes blacks to areas of concentrated poverty, this study’s findings that chronic exposure to poor neighborhoods contributes to the black/white health gap is consistent with extant evidence that found segregation to be associated with detrimental health consequences for blacks, even after adjustments for individual-level controls (Subramanian, Acevedo-Garcia & Osypuk, 2005). The enduring effects of segregation and neighborhood poverty in perpetuating racial health disparities become even more salient when one considers the strong likelihood for black families of residing in impoverished neighborhoods across successive generations while persistent residence in poor neighborhoods across generations for white families is very uncommon (Sharkey, 2008).
In summary, results of this study are consistent with findings from others that have found blacks to be much more likely to have chronic exposure to poverty at both the individual and neighborhood levels while poverty exposure for whites are comparatively transient. Results also indicate that multiple-year measures of income and neighborhood poverty are stronger predictors of health outcomes and explain a greater amount of the black/white health gap than single-point measures. This suggests that ignoring the dynamic nature of individual socioeconomic status and neighborhood context has led to a significant underestimation of the importance of both in explaining health and racial health disparities. As such, racial health disparities studies that rely on only cross-sectional data may be missing a critical component that may undermine their ability to explain a sizable portion of the black/white health gap. The substantial reduction in the race residual after accounting for long term measures of socioeconomic status at both the individual and neighborhood level suggest that 1) better measures of socioeconomic status in a life-course framework may even further explain the health gap between blacks and whites and 2) segregation, to the extent that it chronically exposes blacks to areas of concentrated poverty, plays a substantial role in generating black/white health disparities.
Table 3.
Logistic Regression Results of Single and Multiple-Year Measures of Neighborhood Poverty on 1996 Poor Health in the PSID, 1980–1996 ±
| Characteristics | Model 4A | Model 4B | Model 5A | Model 5B |
|---|---|---|---|---|
|
|
||||
| OR | OR | OR | OR | |
| Race [Reference: White] | ||||
| Black | 1.54** [1.31, 1.81] | 1.34** [1.13, 1.58] | 1.40** [1.18, 1.67] | 1.26** [1.05, 1.51] |
| 1996 Family Poverty Income Ratio [Reference: Over 300%] | ||||
| 100% Or Less | 2.43** [1.95, 3.02] | 2.33** [1.87, 2.90] | ||
| 100%to200% | 2.14** [1.78, 2.57] | 2.09** [1.74, 2.52] | ||
| 200%to300% | 1.37** [1.12, 1.67] | 1.35** [1.11, 1.65] | ||
| 1980–1996 Ave Family Poverty Income Ratio [Reference: Over 300%] | ||||
| 100% Or Less | 2.27** [1.70, 3.04] | 2.14** [1.60, 2.88] | ||
| 100%to200% | 2.20** [1.79, 2.70] | 2.14** [1.74, 2.64] | ||
| 200%to300% | 1.36** [1.12, 1.65] | 1.35** [1.11, 1.64] | ||
| Wealth Quintiles [Reference: Quintile 5] | ||||
| Quintile 1 | 2.28** [1.72, 3.00] | 2.26** [1.71, 3.00] | ||
| Quintile 2 | 1.96** [1.51, 2.54] | 1.93** [1.48, 2.51] | ||
| Quintile 3 | 1.55** [1.21, 2.00] | 1.55** [1.21, 1.99] | ||
| Quintile 4 | 1.34* [1.07, 1.69] | 1.34* [1.07, 1.69] | ||
| 1996 Tract Poverty Level [Reference: 10% Or Less] | ||||
| 10%to20% | 1.24** [1.06, 1.46] | 1.13 [0.96, 1.33] | ||
| 20% Or More | 1.20 [0.99, 1.45] | 1.05 [0.86, 1.28] | ||
| 1980–1996 Ave Tract Poverty Level [Reference: 10% Or Less] | ||||
| 10%to20% | 1.26** [1.06, 1.50] | 1.11 [0.93, 1.33] | ||
| 20% Or More | 1.45** [1.18, 1.79] | 1.24* [1.00, 1.54] | ||
**Statistically Significant at the 1% Level,
Statistically Significant at the 5% Level
Table 4.
Logistic Regression Results of Duration in Neighborhood Poverty on Poor Health in the PSID (1980–1996)±
| Characteristics | Model 6A | Model 6B | Model 7A | Model 7B |
|---|---|---|---|---|
| OR | OR | OR | OR | |
| Race [Reference: White] | ||||
| Black | 1.51** [1.27, 1.80] | 1.33** [1.11, 1.59] | 1.48** [1.25, 1.77] | 1.32** [1.10, 1.58] |
| 1996 Family Poverty Income Ratio [Reference: Over 300%] | ||||
| 100% Or Less | 2.42** [1.95, 3.02] | 2.42** [1.95, 3.02] | ||
| 100%to200% | 2.17** [1.81, 2.60] | 2.16** [1.80, 2.60] | ||
| 200%to300% | 1.40** [1.15, 1.70] | 1.39** [1.14, 1.69] | ||
| 1980–1996 Ave Family Poverty Income Ratio [Reference: Over 300%] | ||||
| 100% Or Less | 2.21** [1.65, 2.96] | 2.22** [1.65, 2.97] | ||
| 100%to200% | 2.20** [1.79, 2.70] | 2.20** [1.79, 2.71] | ||
| 200%to300% | 1.37** [1.13, 1.66] | 1.37** [1.13, 1.66] | ||
| Wealth Quintiles [Reference: Quintile 5] | ||||
| Quintile 1 | 2.32** [1.75, 3.06] | 2.31** [1.75, 3.06] | ||
| Quintile 2 | 1.97** [1.52, 2.56] | 1.97** [1.52, 2.56] | ||
| Quintile 3 | 1.58** [1.23, 2.03] | 1.58** [1.23, 2.02] | ||
| Quintile 4 | 1.36** [1.09, 1.71] | 1.36** [1.09, 1.71] | ||
| 1980–1996 Duration in Poor Tract [Reference: Never] | ||||
| Transient | 1.15 [0.94, 1.40] | 1.05 [0.85, 1.28] | ||
| Persistent | 1.23* [1.03, 1.49] | 1.09 [0.91, 1.32] | ||
| 1980–1996 Proportion Years In Poor Tract | 1.02 [1.00, 1.04] | 1.01 [0.99, 1.03] | ||
**Statistically Significant at the 1% Level,
Statistically Significant at the 5% Level, Odds Ratio’s for Proportion Years in Poor Tract represent a hypothetical 10% point change.
Acknowledgments
This research was supported by the Kellogg Foundation’s Health Scholar Multidisciplinary Track Fellowship at the University of Michigan and the NIH Predoctoral Ruth L. Kirschstein National Research Service Award (Grant #1-F31-HD051032-01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acevedo-Garcia D, Lochner KA. Residential Segregation and Health. In: Kawachi I, Berkman L, editors. Neighborhoods and health. Oxford: Oxford University Press; 2003. pp. 265–287. [Google Scholar]
- Acevedo-Garcia D, Osypuk TL, McArdle N, Williams DR. Toward a Policy-Relevant Analysis of Geographic and Racial/Ethnic Disparities in Child Health. Health Affairs. 2008;27(2):321–333. doi: 10.1377/hlthaff.27.2.321. [DOI] [PubMed] [Google Scholar]
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, Syme SL. Socioeconomic Status and Health. The Challenge of the Gradient. Am Psychol. 1994;49(1):15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL. Socioeconomic Inequalities in Health. No easy solution. Jama. 1993;269(24):3140–3145. [PubMed] [Google Scholar]
- Alba RD, Logan JR. Minority Proximity to Whites in Suburbs: An Individual-Level Analysis of Segregation. American Journal of Sociology. 1993;98(6):1388–1427. [Google Scholar]
- Alba RD, Logan JR, Bellair PE. Living with Crime: The Implications of Racial/Ethnic Differences in Suburban Location. Social Forces. 1994;73(2):395–434. [Google Scholar]
- Alba RD, Logan RJ, Stults BJ. How Segregated are Middle-class African Americans. Social Problems. 2000;47:543–558. [Google Scholar]
- Benyamini Y, Idler EL. Community Studies Reporting Association between Self-Rated Health and Mortality: Additional Studies, 1995 to 1998. Research on Aging. 1999;21(3):392–401. [Google Scholar]
- Benzeval M, Judge K. Income and Health: The Time Dimension. Soc Sci Med. 2001;52:1371–1390. doi: 10.1016/s0277-9536(00)00244-6. [DOI] [PubMed] [Google Scholar]
- Collins CA. Racism and Health: Segregation and Causes of Death Amenable to Medical Intervention in Major U.S. Cities. Ann N Y Acad Sci. 1999;896:396–398. doi: 10.1111/j.1749-6632.1999.tb08152.x. [DOI] [PubMed] [Google Scholar]
- Collins CA, Williams DR. Segregation and Mortality: The Deadly Effects of Racism? Sociological Forum. 1999;14(3):495–523. [Google Scholar]
- Denton NA, Massey DS. Residential Segregation of Blacks, Hispanics, and Asians by Socioeconomic-Status and Generation. Social Science Quarterly. 1988;69(4):797–817. [Google Scholar]
- Diez-Roux AV. Investigating Neighborhood and Area Effects on Health. American Journal of Public Health. 2001;91:1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV. Places, People, and Health. American Journal of Epidemiology. 2002;155:516–519. doi: 10.1093/aje/155.6.516. [DOI] [PubMed] [Google Scholar]
- Duncan GJ. The Volatility of Family Income over the Life Course. In: Baltes P, Featherman D, Lerner RM, editors. Life-span Development and Behavior. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. pp. 317–358. [Google Scholar]
- Duncan GJ, Brooks-Gunn J, Klebanov PK. Economic Deprivation and Early Childhood Development. Child Development. 1994;65(2):296–318. [PubMed] [Google Scholar]
- Duncan GJ, Connell JP, Klebanov PK. Conceptual and Methodological Issues in Estimating Causal Effects of Neighborhoods and Family Conditions on Individual Development. In: Brooks-Gunn J, Duncan G, Aber J, editors. Neighborhood Poverty. Context and Consequences for Children. I. New York: Russell Sage; 1997. [Google Scholar]
- Ellen IG. Is Segregation Bad for Your Health? The Case of Low Birth Weight. Brookings-Wharton Papers on Urban Affairs 2000. 2000;1:203–238. [Google Scholar]
- Elliott M, Finch BK, Klein D, Do DP, Ma S, Lurie N. Methods to Increase Effective Sample Size for Small Racial and Ethnic Minority Sub-Groups in National Health Surveys. Working Paper 2006 [Google Scholar]
- Fitzpatrick KM, LaGory M. Unhealthy Places: The Ecology of Risk in the Urban Landscape. New York, NY: Routledge; 2000. [Google Scholar]
- Fitzpatrick KM, LaGory M. “Placing” Health in an Urban Sociology: Cities as Mosaics of Risk and Protection. City and Community. 2003;2(1):33–46. [Google Scholar]
- Geronimus AT. The Weathering Hypothesis and the Health of African-American Women and Infants: Evidence and Speculations. Ethnicity and Disease. 1992;2 (3):207–221. [PubMed] [Google Scholar]
- Goldberg P, Gueguen A, Schmaus A, Nakache JP, Goldberg M. Longitudinal study of associations between perceived health status and self reported diseases in the French Gazel cohort. J Epidemiol Community Health. 2001;55(4):233–238. doi: 10.1136/jech.55.4.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg M. American Cities: Good and Bad News about Public Health. Bulletin of the New York Academy of Medicine. 1991;67:17–21. [PMC free article] [PubMed] [Google Scholar]
- Guest AM, Almgren G, Hussey JM. The Ecology of Race and Socioeconomic Distress: Infant and Working-Age Mortality in Chicago. Demography. 1998;35(1):23–34. [PubMed] [Google Scholar]
- Gramlich E, Laren D, Sealand N. Moving into and out of Poor Urban Areas. Journal of Policy Analysis and Management. 1992;11(2):273–287. [Google Scholar]
- Haan M, Kaplan GA. The Contributions of Socioeconomic Position to Minority Health; Report of the Secretary’s Task Force on Black and Minority Health; Washington D.C. 1986. [Google Scholar]
- House JS, Williams DR. Promoting health. Intervention strategies from social and behavioral research. Washington DC: National Academy Press; 2000. Understanding and Reducing Socioeconomic and Racial/Ethnic Disparities in Health; pp. 81–124. [Google Scholar]
- Hummer RA, Rogers RG, Eberstein IW. Sociodemographic Differentials in Adult Mortality: A Review of Analytic Approaches. Population and Development Review. 1998;24:553–578. [Google Scholar]
- Iceland J. Current Population Reports. Washington, DC: U.S. Census Bureau; 2003. Dynamics of Economic Well-Being, Poverty 1996–1999; pp. 70–91. [Google Scholar]
- Iceland J, Weinberg D, Steinmetz E. US Government Printing Office. Washington, D.C: U.S. Census Bureau; 2002. Racial and Ethnic Residential Segregation in the United States: 1980–2000. [Google Scholar]
- Iceland J, Wilkes RAUoM University of British C. Does Socioeconomic Status Matter? Race, Class, and Residential Segregation. Social Problems. 2006;53(2):248–273. [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Jargowsky PA. Poverty and Place: Ghettos, Barrios, and the American City. Russell Sage Foundation; New York: 1997. [Google Scholar]
- Jarowsky PA. Stunning Progress, Hidden Problems: The dramatic decline of concentrated poverty in the 1990s. The Livings Cities Census Series. The Brookings Institution 2003 [Google Scholar]
- Kawachi I, Berkman L. Neighborhoods and Health. Oxford University Press; 2003. [Google Scholar]
- Kling JR, Liebman JB, Katz LF. NBER Working Papers. National Bureau of Economic Research, Inc; 2005. Experimental Analysis of Neighborhood Effects. [Google Scholar]
- Korenman S, Miller J, Sjaastad J. Long-term Poverty and Child Development in the United States: Results from the NLSY. Children and Youth Services Review. 1995;17:127–155. [Google Scholar]
- Kunz Page, Solon Are Point-in-Time Measures of Neighborhood Characteristics Useful Proxies for Children’s Long-Run Neighborhood Environment? Economics Letters. 2003;79:231–237. [Google Scholar]
- LaVeist TA. Linking Residential Segregation and the Infant Mortality Race Disparity. Sociology and Social Research. 1989;73(2):90–94. [Google Scholar]
- LeClere FB, Rogers RG, Peters KD. Ethnicity and Mortality in the United States: Individual and Community Correlates. Social Forces. 1997;76(1):169–198. [Google Scholar]
- Link BG, Phelan J. Social Conditions As Fundamental Causes of Disease. Journal of Health and Social Behavior. 1995;35(Extra Issue: Forty Years of Medical Sociology: The State of the Art and Directions for the Future):80–94. [PubMed] [Google Scholar]
- Lobmayer P, Wilkinson RG. Inequality, Residential Segregation by Income, and Mortality in US Cities. J Epidemiol Community Health. 2002;56(3):183–187. doi: 10.1136/jech.56.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan JR, Alba RD. Who Lives in Affluent Suburbs? Racial Differences in Eleven Metropolitan Regions. 1995;28:353–364. [Google Scholar]
- Macintyre S, Ellaway A, Cummins S. Place Effects on Health: How Can We Conseptualize, Operationalise and Measure Them? Social Science & Medicine. 2002;55:125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Malat J, Oh HJ, Hamilton MA. Poverty Experience, Race, and Child Heal. Public Health Reports. 2005;120(4):442–447. doi: 10.1177/003335490512000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey DS. American Apartheid: Segregation and the Making of the Underclass. The American Journal of Sociology. 1990;96(2):329–357. [Google Scholar]
- Massey DS, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Harvard University Press; 1993. [Google Scholar]
- Massey D, Eggers M. The Spatial Concentration of Affluence, and Poverty during the 1970s. Urban Affairs Quarterly. 1993;29:299–315. [Google Scholar]
- Massey D, Fischer M. How Segregation Concentrates Poverty. Ethnic and Racial Studies. 2000;23(4):670–691. [Google Scholar]
- Massey DS, Gross AB, Shibuya K. Migration, Segregation, and the Geographic Concentration of Poverty. American Sociological Review. 1994;59(3):425–445. [Google Scholar]
- McDonough P, Berglund P. Histories of Poverty and Self-Rated Health Trajectories. Journal of Health and Social Behavior. 2003;44(2):198–214. [PubMed] [Google Scholar]
- McDonough P, Duncan GJ, Williams DR, House JS. Income Dynamics and Adult Mortality in the United States, 1972 through 1989. American Journal of Public Health. 1997;87(9):1476–1483. doi: 10.2105/ajph.87.9.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonough P, Sacker A, Wiggins RD. Time on my side? Life Course Trajectories of Poverty and Health. Social Science and Medicine. 2005;61:1795–1808. doi: 10.1016/j.socscimed.2005.03.021. [DOI] [PubMed] [Google Scholar]
- McGee DL, Liao Y, Cao G, Cooper RS. Self-reported Health Status and Mortality in a Multiethnic US Cohort. Am J Epidemiol. 1999;149(1):41–46. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- Morenoff JD, Lynch JW. What makes a place healthy? Neighborhood influences on racial/ethnic disparities in health over the life course. In: Anderson NB, Rodolfo AB, Cohen B, editors. Critical Perspectives on Racial and Ethnic Difference in Health in Late Life. Washington, DC: Natl. Acad. Press; 2004. pp. 406–49. [Google Scholar]
- Pappas G, Queen S, Hadden W, Fisher G. The Increasing Disparity in Mortality between Social Groups in the United States 1960 and 1986. New England Journal of Medicine. 1993;329(2):103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- Pattillo-McCoy M. The Limits of Out-Migration for the Black Middle Class. Journal of Urban Affairs. 2000;22(3):225–241. [Google Scholar]
- Pickett KE, Pearl M. Multilevel Analyses of Neighbourhood Socioeconomic Context and Health Outcomes: A Critical Review. J Epidemiol Community Health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polednak AP. Segregation, Discrimination and Mortality in U.S. Blacks. Ethnicity & Disease. 1996;6:99–108. [PubMed] [Google Scholar]
- Quillian L. Migration Patterns and the Growth of High-Poverty Neighborhoods, 1970–1990. American Journal of Sociology. 1999;105(1):1–37. [Google Scholar]
- Quillian L. How Long are Exposures to Poor Neighborhoods? The Long-Term Dynamics of Entry and Exit from Poor Neighborhoods. Population Research and Policy Review. 2003;22(3):221–249. [Google Scholar]
- Rank MR, Hirschl TA. Rags or Riches: Estimating the Probabilities of Poverty and Affluence Across the Adult American Life Span. Social Science Quarterly. 2001;82:651–669. [Google Scholar]
- Reijneveld S, Schene A. Higher Prevalence of Mental Disorders in Socioeconomically Deprived Urban Areas in The Netherlands: Community or Personal Disadvantage? J Epidemiol Community Health. 1998;52(1):2–7. doi: 10.1136/jech.52.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert SA. Socioeconomic Position and Health: The Independent Contribution of Community Socioeconomic Context. Annual Review of Sociology. 1999;25:489–516. [Google Scholar]
- Rosenbaum E, Friedman S. Differences in the Locational Attainment of Immigrant and Native-Born Households with Children in New York City. Demography. 2001;38(3):337–348. doi: 10.1353/dem.2001.0030. [DOI] [PubMed] [Google Scholar]
- Ross CE, Reynolds JR, Geis KJ. The Contingent Meaning of Neighborhood Stability for Residents’ Psychological Well-Being. American Sociological Review. 2000;65(4):581–597. [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and Violent Crime: A Multilevel Study of Collective Efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Wilson WJ. Towards a Theory of Race, Crime and Urban Inequality. In: Hagan J, Peterson R, editors. Crime and Inequality. Stanford, CA: Stanford Univ Press; 1995. [Google Scholar]
- Sharkey P. The Intergenerational Transmission of Context. AJS. 2008;113(4):931–969. [Google Scholar]
- Sloggett A, Joshi H. Higher Mortality in Deprived Areas: Community or Personal Disadvantage? BMJ. 1994;309(6967):1470–1474. doi: 10.1136/bmj.309.6967.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solon G. Intergenerational Income Mobility in the United States. The American Economic Review. 1992;82(3):393–408. [Google Scholar]
- Schulz AJ, Williams DR, Israel BA, Lempert LB. Racial and Spatial Relations as Fundamental Determinants of Health in Detroit. The Milbank Quarterly. 2002;80(4):677–707. doi: 10.1111/1468-0009.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South SJ, Crowder KD. Escaping Distressed Neighborhoods: Individual, Community, and Metropolitan Influences. American Journal of Sociology. 1997;102(4):1040–1084. [Google Scholar]
- South SJ, Crowder KD. Leaving the ‘hood: Residential mobility between black, white, and integrated neighborhoods. American Sociological Review. 1998;63(1):17–26. [Google Scholar]
- Stevens AH. The Dynamics of Poverty Spells: Updating Bane and Ellwood. The American Economic Review; Papers and Proceedings of the Hundred and Sixth Annual Meeting of the American Economic Association; 1994. pp. 34–37. [Google Scholar]
- Stevens AH. Climbing out of Poverty, Falling Back in: Measuring the Persistence of Poverty Over Multiple Spells. Journal of Human Resources. 1999;34(3):557–588. [Google Scholar]
- Subramanian SV, Acevedo-Garcia D, Osypuk TL. Racial Residential Segregation and Geographic Heterogeneity in Black/White Disparity in Poor Self-Rated health in the US: A Multilevel Statistical Analysis. Social Science & Medicine. 2005;60(8):1667–1679. doi: 10.1016/j.socscimed.2004.08.040. [DOI] [PubMed] [Google Scholar]
- Timberlake JM. Racial and Ethnic Inequality in Childhood Exposure to Neighborhood Poverty and Affluence; Population Research Center Discussion Paper; University of Chicago. 2003. [Google Scholar]
- Turley RNL. When Do Neighborhoods Matter? The Role of Race and Neighborhood Peers. Social Science Research. 2003;32(1):61–79. [Google Scholar]
- Waitzman NJ, Smith KR. Separate but Lethal: The Effects of Economic Segregation on Mortality in Metropolitan America. The Milbank Quarterly. 1998;76(3, Socioecomic Differences in Health):341–373. doi: 10.1111/1468-0009.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR. Racism and Health: A Research Agenda. Ethnicity and Disease. 1996;6(1,2):1–6. [PubMed] [Google Scholar]
- Williams DR, Collins C. US Socioeconomic and Racial Differences in Health: Patterns and Explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Williams DR, Collins C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson WJ. The Truly Disadvantaged: the Inner City, the Underclass, and Public Policy. Chicago, Il: The University of Chicago Press; 1987. [Google Scholar]
- Yen Irene H, George A Kaplan. Neighborhood Social Environment and Risk of Death: Multilevel Evidence from the Alameda County Study. American Journal of Epidemiology. 1999;149:898–907. doi: 10.1093/oxfordjournals.aje.a009733. [DOI] [PubMed] [Google Scholar]
- Yen IH, Syme SL. The Social Environment and Health: A Discussion of the Epidemiologic Literature. Annual Review of Public Health. 1999;20(1):287–308. doi: 10.1146/annurev.publhealth.20.1.287. [DOI] [PubMed] [Google Scholar]
- Zimmerman DJ. Regression Toward Mediocrity in Economic Stature. The American Economic Review. 1992;82(3):409–429. [Google Scholar]