Abstract
BACKGROUND
Thirty years after the origin of the field of psycho-oncology, limited data exist about the work practices of professionals providing psychosocial care to children with cancer and their families.
METHOD
A survey was designed to assess training, work environment, theoretical orientation, services provided, sub-specialty areas or areas of special interest, satisfactions, challenges and continuing education needs of pediatric psycho-oncologists. Members of national and international psycho-oncology organizations were invited to participate in the web-based survey.
RESULTS
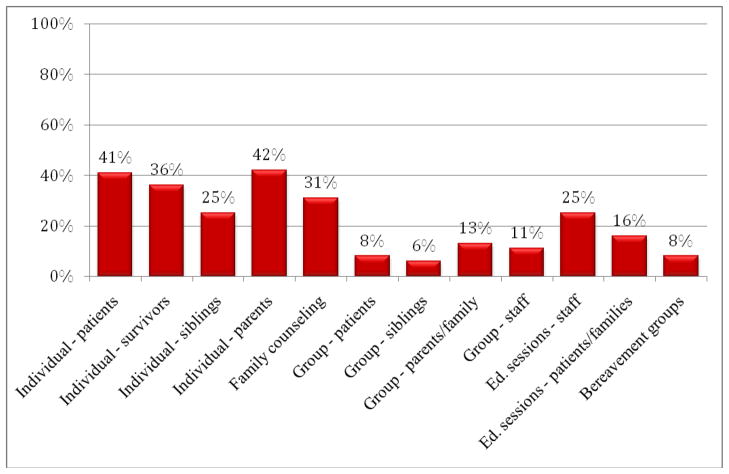
786 professionals from 63 countries responded. The sample consisted mostly of psychologists (41%), physicians (20%), and social workers (14%). Approximately half of the participants worked in a designated psycho-oncology unit. Psychologists and social workers provided the majority of psychosocial services. Individual sessions with parents were most common (42%), followed by sessions with children (41%), survivors (36%), families (31%) and siblings (25%). Therapies provided include CBT (50%), relaxation (43%), psychodynamic psychotherapy (27%), play therapy (26%), and imagery (23%). Two-thirds report having appropriate supervision; 37% conduct research; only half feel their salary is appropriate. Differences in therapeutic modalities were found by country. Clinicians desire training on clinical interventions, improving communication with medical staff, research and ethics.
CONCLUSIONS
An international cohort of clinicians providing pediatric psycho-oncology services perform a wide variety of tasks, use a range of therapeutic approaches and report considerable work satisfaction. Problem areas include professional inter-relations, inadequate supervision and needs for additional, specialized training. Opportunity exists for global collaboration in pediatric psycho-oncology research and practices to enhance clinical effectiveness and reduce professional isolation.
Keywords: Pediatric, Psycho-oncology, Childhood Cancer, Training, Professional rewards, Clinical Challenges
Background
Pediatric psychosocial oncology is a relatively young, multidisciplinary specialty concerned with the emotional and behavioral aspects of childhood cancer. Pediatric psycho-oncologists treat children and adolescents with cancer through the child’s diagnosis, treatment, re-entry to school and community, end-of-life care or survivorship after cancer. They also treat the distress of cancer caregivers and siblings of children with cancer. The beginnings of psychosocial oncology date to the 1970’s, when pediatric cancer survival increased and the stigma surrounding cancer diminished so that patients were informed about their diagnosis and could talk with mental health professionals about their illness [1]. Until this period, 42% of children still died within five years after diagnosis [2]. Many professionals remained hesitant about discussing cancer diagnosis and prognosis with children. There were few opportunities for children with cancer to talk about their feelings and fears; even parents whose child was diagnosed with cancer were advised not to communicate the diagnosis or prognosis to their child. If a psychiatrist, psychologist or social worker was available at the medical center, their work focused mainly on preparing the family for the child’s death.
Early pediatric research in psycho-oncology suggested that terminally ill children knew much more than adults thought they did about their diagnosis and impending death [3]. Children’s fears and “melancholia” often went unattended because of the prohibition against talking about dying [4]. Patient isolation was further fueled by the belief, held by many, that the disease was contagious. Gradually there was recognition of the developmental stages in children’s understanding of death, which helped to guide the content of conversations professionals and parents had with children about illness and death [5]. The treatment of childhood cancer has made significant medical advances in recent decades and today more than 75 percent of children diagnosed with cancer are expected to survive [2]. With expected survival, the focus of care has evolved to focus more on the psychological and social needs of children living with cancer and, especially, the lifelong emotional and behavioral outcomes for survivors who experience late effects or other sequelae of their cancer treatment. In high-resource Western countries, integration of psychological and social services within pediatric oncology care has become routine, though services vary considerably between and within countries. There has also been tremendous growth of research on questions concerning the behavioral, psychosocial, neurocognitive and familial outcomes for children whose lives have been affected by cancer [6]. The Institute of Medicine (IOM) mandate for psychosocial support to be integrated into routine pediatric cancer care for the whole family [7] requires translating such research results into clinical care. This, in turn, requires understanding how psycho-oncologists function in pediatric oncology settings. This information could also help target appropriate professional recruitment, and development of multi-site, cooperative training programs. Because only about 10,000 children per year are diagnosed in the U.S. (globally, an estimated 175,300 new cancer cases occurred among children aged 0–14 in 2008) [8] many centers treat small numbers of children with cancer. Thus, it would make for efficiency if multi-site or web-based trainings could be developed to enhance local training opportunities.
While the current literature addresses the psychosocial needs and concerns of children, siblings and families affected by childhood cancer, little is known about the professional backgrounds and work experiences of pediatric psycho-oncology clinicians working in pediatric centers around the world. What training do most people have who work in this field? Which disciplines provide the majority of psychosocial care to children receiving cancer treatment? Are consistent clinical services being provided to children with cancer? Which psychosocial or behavioral interventions are most commonly used with children with cancer or with survivors or family members? Does the pediatric psycho-oncologist have appropriate supervision? Do they participate in research? What are their training needs? Do they feel isolated in their work? Would they like to work with a collaborative group? Do they feel their salary is commensurate with their work? What do they find most rewarding about working in pediatric psycho-oncology and what are the greatest challenges of the work? What do they perceive would help them to be more successful at their job?
This paper, which describes results of an international survey of pediatric psycho-oncologists, provides at least initial answers to many of these questions. The study goals were to, 1) gain information about the type of services being provided to children with cancer, and 2) describe the needs, interests and experiences of psycho-oncologists providing these services to children with cancer worldwide. Understanding the basic and continuing educational needs of this professional group will allow academic centers and professional organizations to effectively focus training and continuing education efforts for providers of psychosocial care to children with cancer. An additional goal was to determine whether a worldwide group of pediatric psycho-oncologists would identify a need to improve professional interaction and cohesion within the field. In this regard, we sought to learn whether providers of pediatric psychosocial oncologic services have an interest in sharing clinical methods, therapeutic tools, clinical insights and research findings and if they share a common interest in fostering research collaborations as a means to improve professional growth and satisfaction.
Methods
In order to obtain a comprehensive view of the clinical, research and administrative responsibilities, service provision and training needs of pediatric psycho-oncologists, the authors created a survey that evaluated respondents’: 1) demographic characteristics, 2) work setting, 3) services provided, 4) distribution of work responsibilities, 5) treatment approaches, 6) self-reported adequacy of supervision, 7) areas of specific sub-specialty interest (e.g. interventions, neurocognitive, death and dying), 8) research experience, 9) professional activities, 10) future training interests, and 11) the rewards and challenges of working in the field of pediatric psycho-oncology. Three oncology organizations, the International Psycho-Oncology Society (IPOS), the International Society of Paediatric Oncology (SIOP) and the Canadian Association of Psychosocial Oncology (CAPO) invited their members who provide pediatric psycho-oncology services to participate in this online survey. For survey purposes, youth with cancer was defined as including children, adolescents, and young adults up to the age of 25. Each group of professionals was sent 2 reminder emails approximately 3 weeks apart.
Qualitative data about sources of professional satisfactions and frustrations were obtained through three open-ended questions at the end of the survey. Responses were then analyzed thematically using a grounded theory approach, an established qualitative research method in which concepts and themes which emerge from reviews of the qualitative data form the basis of the coding of the narratives [9–12]. In our study, two research assistants and a study investigator (LW) agreed upon the identification of themes, followed by the creation and identification of codes. A postdoctoral fellow (SZ) and study investigator (LW) independently coded the data. Discrepancies were reviewed and when appropriate, definitions were revised, until there was agreement on all items. This analysis allowed us to capture subjective qualities of the subjects’ professional experiences, satisfactions and training needs.
Quantitative data were analyzed using SPSS 12.0.1 [13]. Descriptive statistics were used, including frequencies and crosstabs. Categorical variables were analyzed with chi-square tests. While multiple comparisons are made, Bonferroni-type adjustments were not made to the p-value, as this is a descriptive study, designed to identify themes and areas for future research. The goal of adjustments for multiple comparisons is to reduce the likelihood of Type I error (finding significant relationships where there are none), but it also increases the likelihood of Type II error (ignoring relationships that, indeed, are real). Since this is an exploratory phase of work where our goals are identifying potential areas for future research, we opted to leave the p-value unadjusted, at p < .05.
Results
Demographics
Seven hundred and eighty-six pediatric psycho-oncology professionals from 63 countries responded to the survey request, with 40% from Europe, 44% from North America, 7% from Asia, 4% from South America, 4% from Australia, and 1% from Africa. Of the participants, 7% were in the 20–29 year old range, 25% between the ages of 30–39, 29% between the ages of 40–49, 29% between 50–59, and 10% age 60 or greater. Seventy-eight percent of the participants were female; the majority psychologists (20%), physicians (14%) and social workers (9%) (Table 1). Five hundred and eighty-five subjects completed all survey questions. There were no significant differences between survey completers and those who did not complete all the questions on any of the demographic or practice variables with the exception of work setting. Those who reported working in either inpatient or outpatient settings (as opposed to all other work settings) were more likely to complete the survey in its entirety (X2 (1) = 80.4, p < .001; X2 (1) = 89.1, p < .001, respectively). There were no differences for those who reported working in private practice versus those who did not. Data below are reported by question for those who answered each question.
Table 1.
Demographics (n=786)
| Demographic/Work Setting Variable | % (n) |
|---|---|
|
| |
| Gender | |
| Female | 78% (613) |
| Male | 22% (173) |
|
| |
| Age | |
| 20–29 | 1.3% (57) |
| 30–39 | 24.9% (196) |
| 40–49 | 28.6% (225) |
| 50–59 | 29.1% (229) |
| 60+ | 10.1% (79) |
|
| |
| Country/Continent | |
| Africa | 1.3% (10) |
| Australia | 3.8% (30) |
| North America | |
| Canada | 11.6% (91) |
| United States | 31.7% (249) |
| Other North America | 0.9% (7) |
| Europe | |
| France | 2.8% (22) |
| Germany | 2.6% (20) |
| Italy | 3.1% (24) |
| Netherlands | 3.7% (29) |
| Spain | 2.6% (20) |
| United Kingdom | 13.4% (105) |
| Other Europe | 11.7% (92) |
| Asia | |
| India | 3.2% (25) |
| Other Asia | 3.7% (29) |
| South America | 3.8% (30) |
|
| |
| Profession | |
| Psychology | 41% |
| Medicine | 20% |
| Social Work | 14% |
| Nursing | 9% |
| Counseling | 4% |
| Child Life/Recreational Therapist | 1% |
| Chaplaincy | 1% |
| Other | 10% |
|
| |
| Work Setting | |
| Inpatient | 62% |
| Outpatient | 69% |
| Private Practice | 12% |
| Academic/Research | 6% |
| Home Care/Hospice | 2% |
| Other | 14% |
Work Settings
The majority of participants reported that their primary work setting was either an outpatient (64%) and/or an inpatient (57%) medical setting. Eleven percent worked in private practice and 20% in other locations, including community organizations, camps, and advocacy groups. Fifty-one percent reported having a designated psycho-oncology unit in their work setting. Of those who knew how many psycho-oncology staff worked at their facility (n = 492), the majority (71%) reported that their worksite had 1–5 full time staff, 12% reported 6–10 full time staff members, and 8% had greater than 11 staff members. Ten percent of participants reported having no full time designated psycho-oncology provider at their work site.
Clinical Services Provided
Forty-two percent of participants reported conducting individual treatment sessions with parents, 41% with children with cancer, 36% with survivors of pediatric cancers, and 25% held individual sessions with patients’ siblings. Thirty-one percent of the participants conducted family counseling sessions and 25% held educational sessions for staff.
It was reported that 22% of patients and 30% of parents are “usually” or “always” seen by a mental health provider during their routine visits. Fewer participants report that survivors of childhood cancer are “usually” or “always” seen by a mental health provider (18%) when they come for follow-up clinics. Thirty-five percent of participants reported that pediatric cancer patients are “usually” or “always” referred to a mental health provider after diagnosis. The participating psycho-oncologists stated that they “usually” or “always” work closely with the medical team (74%) in coordinating the patients’ care; 27% reported “usually” or “always” meeting together with the patient and the medical team.
Thirty-one percent of the participants reported providing clinical services to over 20 patients in a typical week, with the average hours worked per week (for pay) being 39. Almost all (92%) consult with medical staff, 83% provide clinical services, 80% have administrative duties, 79% teach/train/advise students, and 71% participate in research. Less than half (47%) provide consultation to school teachers of children with cancer, 27% conduct support groups for medical staff and 27% conduct psychological and/or neuropsychological testing. Very few providers conduct only one activity in their jobs.
Professional Disciplines
Participants were also asked which discipline provides psycho-oncology services to children with cancer, the child’s parents, and to survivors of childhood cancer at their institution. Response categories, for each discipline, included “Rarely/never”, “Sometimes”, “Frequently”, and “Most/all”. Providers report that at their work setting, psychologists and social workers frequently provide “most/all” of the psycho-oncology services to children with cancer (63% and 63%, respectively), followed closely by child life therapists (52%) and nurses (48%). Social workers were the professionals most likely to provide psychosocial services to parents of children with cancer (66%).
The most commonly utilized therapies included cognitive behavioral therapy (CBT) (50%), relaxation training (43%), psychodynamic psychotherapy (27%), play therapy (26%) and imagery (23%). Some differences in approach were found by geographic location. For example, CBT was most often reported by those who live in the United States (45%), Germany (40%), Australia (40%) and Africa (40%). The lowest use of CBT by professionals was reported in France (0%), Italy (21%), UK (16%) and countries in South America (17%). Psychodynamic psychotherapy was most frequently utilized in France (55%) and Africa (50%). Relaxation training was most commonly utilized in Africa (60%), United States (40%), Mexico/Central America (43%) and Spain (50%) and play therapy was most common in Africa (40%), Mexico/Central America (43%), South America (39%) and Spain (30%).
Sixty-five percent of participants reported having appropriate supervision and over half 54%) felt their salary was appropriate. Forty-nine percent indicated they supervise other staff and 62% supervise students.
Research
Fifty-four percent of participants reported conducting psychosocial research; of these, 78% said they have been involved in designing research studies, 76% in collecting data, 63% in analyzing data, and 69% in writing study reports and journal articles. Interest in further training in qualitative and quantitative research designs was endorsed by over a third of the total group of participants.
Professional Activities and Interests
The survey asked participants to describe subspecialty areas they worked in or were strongly interested in. The most frequently endorsed areas were clinical work with child and adolescent patients (47%), survivorship (45%), clinical work with parents/family (46%), treatment of siblings (29%), dying and death (40%), bereavement (30%), neurocognitive/school testing (16%), screening (38%), and ‘other’ (5%). Responses in the ‘other’ category included interests in reintegrating survivors into the school system, improving academic and cognitive function of pediatric survivors, and work in adolescent sexual health/functioning. Participants reported that they would benefit most from additional training in the areas of clinical interventions (73%), improving communication with medical staff (65%), ethics (55%), sharpening diagnostic skills (55%), qualitative research methods (47%), supervision training (44%), quantitative research methods (44%), and learning how to publish in the professional literature (33%).
Age and Work Experiences
We examined differences in work experiences based on age of the participants in order to better understand the educational needs of both junior and senior professionals. Trends were found in the number of weekly treatment sessions provided and in the theoretical orientations of the subjects by age. Older professionals (ages 50+) conducted significantly fewer treatment sessions overall, with those aged 30–39 providing more individual sessions with children (51% versus less than 40% for other age groups, X2 (4) = 11.9, p < .05), more individual sessions with parents (51% versus less than 41% for other age groups, X2 (4) = 10.1, p < .05). Younger professionals (20–29 years) were more likely to conduct group sessions with siblings (14% vs. 7% or less for older age groups, X2 (4) = 11.5, p < .05). Professionals aged 30–39 were significantly more likely to provide CBT than those in other age groups (42% vs. less than 36% for other age groups, X2 = 12.8 (4), p < .05).
The number of participants who reported providing supervision to staff increased significantly with age (5% for those ages 20–29 vs. 34% or more for older professionals, X2 = 29 (8), p < .001), but supervision to students was similar across the age groups. Older professionals were significantly more likely to work with cancer survivors (21% for those ages 20–29, vs. 46% or more for older groups, X2 = 14.5 (4), p < .01).
Younger participants reported being less likely to participate in scientific, academic or professional associations (26% vs. over 54% for older groups, X2 = 31.0 (8), p < .01). No age differences were found for participation in cross-national workgroups and consortia or for involvement in research.
Gender and Work Experiences
Female participants reported providing more group therapeutic sessions to children than male participants (9% vs. 4%, X2 = 4.0 (1), p < .05), and there was a trend towards females providing more group sessions with siblings (7% vs. 3%, X2 = 3.1 (1), p = .08). Females also provided more educational sessions for staff (27% vs. 19%, X2 = 4.2 (1), p < .05) and used play therapy (19% vs. 12%, X2 = 3.7 (1), p = .05), art therapy (11% vs. 5%, X2 = 4.8, p < .05), and relaxation training at a higher rate than males; male professionals used hypnosis more than females participants and showed a trend toward providing more music therapy (5% vs. 2%, X2 = 3.4 (1), p = .06). Male professionals were more likely to conduct hypnosis sessions than females (7% vs. 3%, X2 = 4.4 (1), p < .05). More men reported supervising staff (42% vs. 32%, X2 = 6.5 (2), p < .05) than women, but there was no significant gender difference in supervision of students. There were no gender differences in professionals’ areas of interest and no age or gender differences in participants’ involvement in research. Of those who answered the question (n = 495), men were more likely to be satisfied with their salary than women (63% vs. 50%, X2 = 5.7 (1), p < .05); there was no age difference in satisfaction with salary.
The Rewards and Challenges of Pediatric Psycho-Oncology
Four hundred and twenty-nine participants responded to the question about the most rewarding aspects of working in the field of psycho-oncology. Coding revealed the most commonly reported rewards were providing support across the cancer trajectory (mentioned by 44%) and finding the work to be meaningful work (32%). Additional factors contributing to professional satisfaction included patient/family strengths (8%), personal growth (6%), and positive interactions with colleagues (7%). Narratives that illustrate each of the themes are provided in Table 3.
Table 3.
The most rewarding aspects of working in the field of pediatric psycho-oncology
| Theme/Examples | N = 429 |
|---|---|
| Providing Support Across the Cancer Trajectory | 44% |
| |
| Meaningful Work | 32% |
| |
| Patient/Family Strengths | 8% |
| |
| Personal Growth | 6% |
| |
| Positive interactions with Colleagues | 7% |
| |
Three hundred and eighty participants provided a response to an open-ended question about the challenges they faced in their work. The themes that emerged reflected subjects’ perceptions of the work as highly emotionally taxing (28%) and often conducted without adequate supervisory and administrative resources (21%). Other challenges included interdisciplinary difficulties (18%), clinical challenges (untreated mental health problems, significant family conflict, non-adherent adolescents and families) (17%), inadequate training (8%), and inadequate time to timely address all patient needs and documentation requirements (8%). Narratives illustrating these themes are provided in Table 4.
Table 4.
The most challenging aspects of working in the field of pediatric psycho-oncology
| Theme/Examples | N = 380 |
|---|---|
| Emotionally Taxing | 28% |
| |
| Inadequate Resources | 21% |
| |
| Interdisciplinary Difficulties | 18% |
| |
| Clinical Challenges | 17% |
| |
| Inadequate Training | 8% |
| |
| Time Shortage | 8% |
| |
When asked to describe “three (3) things that would improve your ability to do your job better”, 394 participants provided at least one response. Most frequently mentioned was a desire for larger psycho-oncology staff so that there would be less time per person devoted to administrative work, and a better balance between clinical work with other interests (examples included research (39%). Professionals also desired training opportunities, more guidelines for the care of cancer patients and long-term survivors (18%), and more collaboration and better communication with interdisciplinary team members (15%). They also wanted higher salaries, easier access to grant support (8%), more or better supervision (7%), more workspace (6%), and greater professional recognition within their institutions (4%).
Discussion
To the best of our knowledge, this is the first international, multi-disciplinary study designed to describe the work experiences of professionals providing pediatric psycho-oncology services. The findings illustrate the broad range of work settings, services provided, satisfactions and challenges, and training needs of those providing mental health treatment, survivorship support, and end-of-life care. Having this data marks a milestone in the development of the field of pediatric psycho-oncology.
Our data suggests that provision of clinical care to children with cancer and their family members is challenging, but meaningful work. It is also clear that the majority of subjects do not do service provision full time. A key factor in work satisfaction, mentioned by many participants, is the desire to balance the emotional burdens of the work with other related, fulfilling tasks, such as conducting clinical services, providing supervision or teaching. Many respondents noted that finding a successful career balance is difficult, especially given resource limitations and demands for time spent doing administrative tasks. Considering the intensity of the psychosocial needs of children facing cancer, their families’ needs and the IOM mandate that all patients receive integrated care, there is a need to train a larger cadre of pediatric psycho-oncologists. This was further supported by study respondents’ strong desire for larger communities of caregivers at many institutions.
Over a third of respondents indicated that they participate in psychosocial research. While research involvement was identified as a way to improve the work experience of pediatric psycho-oncologists, balancing the time commitments of clinical work and research was frequently reported as a frustration and challenge to work satisfaction. These pressures may combine with those inherent in working with a population with a high mortality rate and chronic, multi-faceted emotional and practical needs to burden professionals. A study of 549 surgical oncologists [15] found that devoting less than 25% of time to research was associated with greater burnout and lower sense of personal accomplishment. Despite improvements in treatment intensity over recent decades, the stress for professionals of working with very ill children, many of whom survive to experience long-term sequelae of their disease or treatment, continues to make pediatric psycho-oncology an emotionally demanding work setting for mental health professionals. More data is needed to understand the varying strains on professionals with different levels and types of work commitments in pediatric psycho-oncology. Training professionals in the scientist-clinician role can perhaps reduce stress and provide alternative forms of work satisfaction, not all requiring such heavy emotional investment.
Participants in our study described the additional stress of addressing the mental health concerns of other family members, including provision of bereavement care when a child dies. In the current fiscally-conservative environment, characterized by diminishing staff resources, finding ways to help the pediatric psycho-oncology provider prioritize needs and balance work stress with invigorating educational opportunities will become increasingly important to avoid loss of experienced staff due to poor career satisfaction or burnout [14]. Over two-thirds of participants in our study expressed interest in additional clinical training. Training in qualitative and quantitative research methodology and having opportunities for mentorship and participation in multi-institutional studies was endorsed 42% by participants as factors that would enhance their work experience. Training in writing for publication was endorsed by over a quarter of the participants. Future research may help clarify when added roles compensate or moderate the work stress of pediatric psycho-oncologists and when they compound existing pressures.
This study explored treatment modalities used in many countries. Patterns of usage, such as the preference among French and African pediatric psycho-oncologists for psychodynamic psychotherapy rather than cognitive behavioral approaches (CBT) and relaxation methods may reflect patterns of training and cultural preference. International educational programs will need to consider geographic differences in the range of theoretical orientations and skill sets of participants, designing curricula that reflect the local resources and cultural preferences.
It has been recognized by others that high patient caseloads, cumulative deaths, witnessing patient and family suffering, and experiencing the strain of providing for the medical and psychological needs of pediatric oncology patients and family members are significant stressors for professionals working with oncology settings [16–18]. We hypothesize the finding that younger practitioners work more with newly diagnosed pediatric cancer patients and older practitioners tend more to see survivors or family members reflects the emotional toll over years of practice, with older professionals (who likely have more control over which patients they see) preferring to see the physically healthy family members and not to have a practice of only ill children.
Inter-professional rivalry, the need for greater clarity about professional boundaries, and a desire for increased synergy and collaboration between disciplines were commonly described by participants as factors that compound the challenge of working in pediatric psycho-oncology. The perception that psychosocial interventions are frequently viewed by oncologists and surgeons as optional or of relatively lower importance than medical interventions was cited as a significant challenge to the work satisfaction of pediatric psycho-oncologists. While pediatric programs are often considered to be more multi-disciplinary and better integrated that most adult units, our study results suggest that additional work in inter-professional integration is needed in many settings. Efficacy, role-clarification and job satisfaction can be enhanced with increased collaboration within medical teams and training that addresses the inter-personal aspects of the work. The literature suggests that all team members benefit when systems are in place to identify and manage psychosocial problems. Clear guidelines defining the responsibilities of different professionals for providing clinical services and staff support can be helpful, when they reflect agreed-upon strengths and skills [19].
The profound personal rewards of working in pediatric psycho-oncology and the depth of personal and professional satisfaction of the work were clearly described by participants. Witnessing the strength and resiliency of patients and family members in the face of catastrophic childhood illness was commonly described as “life changing”, in ways that deepen meaning related to their work in the lives of psycho-oncologists. Many comments reflected “the honor of being a participant in one of the most significant events in a person’s life” and spoke to the deep satisfaction many pediatric psycho-oncologists find in the work they do.
Yet, professional isolation was often reported. The data suggest that the limited number of colleagues working in pediatric psycho-oncology at many settings and the high work demands leave little time for needed collegial interaction. The frequently-cited lack of adequate supervision in many settings likely further contribute to isolation and stress for practitioners doing the intensive work which is the norm in this field. The reported sense of isolation may further reflect a lack of clear professional acceptance for the importance of seeking personal and/or professional support to diminish the stress of this work. One participant wrote, “Most people have no idea how much this work affects us - how much it can take from one’s self”. Increasing interaction and involvement in national and international professional groups of pediatric psycho-oncologists can increase professional cohesion and reduce isolation. Forming collaborative networks of pediatric psycho-oncology providers could promote professional growth by providing effective means of sharing clinical methods/tools, research and insights. Improved professional connections may also reduce stress and burnout.
In response to both the findings from this study and comments shared at both American Psycho-Oncology Society (APOS) and the International Psycho-Oncology Society (IPOS) Pediatric Special Interest Group meetings, a webpage has been created by the U.S. National Cancer Institute for pediatric psycho-oncologists to stimulate international communication among professionals with a diversity of clinical and research backgrounds (http://pediatrics.cancer.gov/psycho-oncology/). The goal of the website is foster collaboration among pediatric psycho-oncologists in clinical care, research and education. There is also a need for more research about ways to improve staff interaction and satisfaction, improve clinical effectiveness with limited resources, as well as to develop methods to prevent staff burnout among pediatric psycho-oncologists.
Limitations
While strengths of this survey include the large sample size and the wide range of represented countries, a number of limitations exist. Our ascertainment approach makes it difficult to know how representative our sample of 786 subjects is of all pediatric psycho-oncology professionals. Subjects were invited through major national and international pediatric oncology and psycho-oncology professional organizations. However, participation may be biased towards those subjects from more developed or richer nations who are most likely to participate in these organizations. Also, membership in many of these organizations is often paid using personal funds, and those who participated may represent providers with higher personal incomes and may also favor professionals more motivated to obtain further professional training. In turn, if these professionals obtain more training than is typical for psycho-oncologists, then the number and kinds of services provided reported in this study may be an overestimate. Second, our sample was likely biased towards pediatric oncologists who speak English. Lastly, while we provided information on different practice trends between countries, only a few practitioners represented some countries and, therefore, it is difficult to know if the responses given are representative of those at other sites within their country. Nonetheless, most major and many smaller settings where pediatric psycho-oncology is practiced in 63 countries were included in this study, creating a unique set of data about this emerging field.
Conclusions
The field of pediatric psycho-oncology has grown to a point where an international sample of over 750 professionals participated in a survey about their work experience and satisfaction. Results indicate that those providing psycho-oncology services to youth with cancer and their families perform a wide variety of services and generally feel rewarded by enhancing the well-being of current patients, survivors, and their families. Participating professionals also reported feeling emotionally taxed and torn between many competing, compelling professional responsibilities. They feel their work often goes unrecognized or under-appreciated by medical colleagues. These factors contribute to stress and discontent among psychosocial, interdisciplinary team members working in pediatric psycho-oncology. Increased attention to fostering professional collaborations, improving communication within treatment teams and enhancing supervision and professional support may reduce the emotional burden of treating children with cancer and their family members and improve professional satisfaction for pediatric psycho-oncologists.
Supplementary Material
Figure 1.
Clinical Services
Table 2.
Time Spent in Work Activities
| Activity | Percent Time Spent in Activity | ||||
|---|---|---|---|---|---|
| 0% | 1–25% | 26–50% | 51–75% | 76–100% | |
| Psycho-oncology services for children with cancer, parents siblings, survivors (n=559) | 96 (17%) | 214 (38%) | 82 (15%) | 78 (14%) | 89 (16%) |
| Psychological/Neuropsychological testing of children with cancer (n=509) | 371 (73%) | 79 (16%) | 27 (5%) | 22 (4%) | 10 (2%) |
| Research (n=545)* | 160 (29%) | 221 (41%) | 85 (16%) | 41 (8%) | 38 (7%) |
| Teaching/Training/Advising students (n=537) | 111 (21%) | 295 (55%) | 87 (16%) | 33 (6%) | 11 (2%) |
| Consultation with Medical Staff (n=545) | 63 (8%) | 279 (51%) | 139 (26%) | 55 (10%) | 9 (2%) |
| Support Groups for Medical Staff (n=514)* | 322 (63%) | 147 (29%) | 28 (6%) | 13 (3%) | 2 (0%) |
| Consultation with School Teachers of Children with Cancer (n=520) | 275 (53%) | 213 (41%) | 27 (5%) | 4 (1%) | 1 (0%) |
| Administration (n=531)* | 106 (20%) | 242 (46%) | 120 (23%) | 48 (9%) | 15 (3%) |
Percentages do not add to 100% due to rounding.
Table 5.
Ways to improve ability to do job better
| Theme/Examples | N = 380 |
|---|---|
| More staff, more time | 39% |
| |
| Training and guidelines (18%) | 18% |
| |
| Collaboration and communication with interdisciplinary members | 15% |
| |
| Better salary and/or grant support | 8% |
| |
| Better and/increased or availability for supervision | 7% |
| |
| More physical space | 6% |
| |
| Increased institutional recognition | 4% |
| |
Acknowledgments
ACKNOWLEDGEMENT OF FUNDING
This work is supported in part by the intramural Research Programs of the NIH, National Cancer Institute, Center for Cancer Research
The authors would like to acknowledge the support of several individuals who helped make this work possible. Elliot Graham (IPOS) and Martha Grootenhuis (SIOP) were instrumental in the distribution of the survey information. At NCI, we would like to thank Caroline Crum, Nia Billings and Lauren Latella who assisted with the coding of the qualitative data. We also appreciate the insights provided to us by the Pediatric SIG Members at both IPOS and APOS.
References
- 1.Holland JC. Preface. In: Holland JC, Breitbart WS, Jacobsen PB, Lederberg MS, Loscalzo MJ, McCorkle R, editors. Psycho-Oncology. 2. Oxford University Press; New York: 2010. pp. v–vi. [Google Scholar]
- 2.Ries LAG, Melbert D, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2004. Bethesda, MD: National Cancer Institute; [Accessed February 10, 2012]. Website: http://seer.cancer.gov/csr/1975_2007/ [Google Scholar]
- 3.Waechter EH. Death anxiety in children with fatal illness. Stanford University; Palo Alto: 1969. [PubMed] [Google Scholar]
- 4.Richmond JB, Waisman HA. Psychological aspects of management of children with malignant disease. American Journal of Diseases of Children. 1955;89:42. doi: 10.1001/archpedi.1955.02050110058008. [DOI] [PubMed] [Google Scholar]
- 5.Schowalter JE. The child’s reaction to his own terminal illness. In: Schoenberg B, Carr AC, Peretz D, Kutscher AH, editors. Loss and Grief. Columbia University Press; New York: 1970. [Google Scholar]
- 6.Patenaude AF, Grootenhuis M, Noll R. Pediatric psycho-oncology comes of age: SIOP 2010. Pediatric Blood Cancer. 2011;56(7):1154. doi: 10.1002/pbc.23118. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine of the National Academies. Cancer care for the whole patient: Meeting Psychosocial Health Needs. The National Academies Press; Washington, D.C: Released October 15, 2007. [Google Scholar]
- 8.American Cancer Society. Global Cancer Facts & Figures. 2. Atlanta: American Cancer Society; 2011. [Google Scholar]
- 9.Strauss AL, Corbin JM. Basics of qualitative research: techniques and procedures for developing grounded theory. 2. Sage Publications; London: 2007. [Google Scholar]
- 10.Patton MQ. Qualitative research and evaluation methods. Sage Publications; Thousand Oaks: 2002. [Google Scholar]
- 11.Gubium JF, Holstein JA. Handbook of Interviewing. Sage Publications; Thousand Oaks: 2002. [Google Scholar]
- 12.Auerbach CF, Silverstein LB. Qualitative data: An introduction to coding and analyzing data in qualitative research. New York University Press; New York: 2003. [Google Scholar]
- 13.Levesque R. SPSS Programming and Data Management: A Guide for SPSS and SAS Users. 4. SPSS Inc; Chicago: 2007. [Google Scholar]
- 14.Maslach C, Leiter MP. Early predictors of job burnout and engagement. J Appl Psychol. 2008;93:498–512. doi: 10.1037/0021-9010.93.3.498. [DOI] [PubMed] [Google Scholar]
- 15.Kuerer HM, Eberlein TJ, Pollock RE, et al. Career satisfaction practice patterns and burnout among surgical oncologists: report on the quality of life of members of the Society of Surgical Oncology. Ann Surg Oncol. 2007;14:3043–3053. doi: 10.1245/s10434-007-9579-1. [DOI] [PubMed] [Google Scholar]
- 16.Allegra CJ, Hall R, Yothers G. Prevalence of burnout in the US oncology community. J Oncol Pract. 2005;1(4):140–147. doi: 10.1200/jop.2005.1.4.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kash KM, Holland JC, Breitbart W, Berenson S, Dougherty J, Ouellette-Kobasa S, Lesko L. Stress and burnout in oncology. Oncology. 2000;14:1621–1637. [PubMed] [Google Scholar]
- 18.Escot C, Artero S, Gandubert C, Boulenger JP, Ritchie K. Stress levels in nursing staff working in oncology. Stress Health. 2001;17:273–279. [Google Scholar]
- 19.Loscalzo MJ, Bultz BD, Jacobson PB. Building psychosocial programs: A roadmap to excellence. In: Holland JC, Breitbart WS, Jacobsen PB, Lederberg MS, Loscalzo MJ, McCorkle R, editors. Psycho-Oncology. 2. Oxford University Press; New York: 2010. pp. 569–574. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.