Abstract
There is a sudden blast of the “65 plus” population in the last decade, and India is no exception to that. A continuing progress in the medical field has raised the longevity of life. This changing face of population offers the oral professionals to observe unique challenges to treat the rapidly growing segment of the elderly and the dependant overage population— the Homebound residents and the Nursing homebound residents. The old age of the residents is compounded with chronic medical problems they are suffering from and the medications they are taking. This cohort is characteristically different from other elderly due to their dependency to carry even the routine activities such as tooth cleaning which results in increased risk towards the oral ailments. As very few surveys are done regarding the oral health status among this section, the prevalence of oral and dental problems in them is under a cloud. “Dental care at home or at destinations of residents” is yet a novel concept in India, hence not only there is a need to reach to the residents but also to treat them in the holistic manner. The purpose of this paper is to review the existing oral health conditions in the elderly in India.
Keywords: Dependant elderly, Domiciliary dental care, Homebound residents, Nursing homebound residents, Oral health care
INTRODUCTION
India has acquired the label of an aging nation with the elderly population currently being over 77 million. The rapid graying of the population comes with a number of difficulties in terms of general and oral health. The homebound and the nursing home bound residents are the group of elderly who are unable to maintain independence. If the impairment is severe enough; they may not be able to leave the house without assistance or may become institutionalized in the nursing homes. They are considered being frail, impaired and may have at least one chronic medical disability.[1,2] A majority of this population is above 65 years (65+) of age, with female predominance.[1]
Oral health is linked to overall health, happiness, and general well-being of the individual.
This paper aims to assess the oral health conditions and treatment needs in elderly in India through literature reviews with an emphasis on the residents. Also, it reviews the current oral health services with considerations for developments in them. Lastly, it introduces the concept of ‘Domiciliary dental care’ for the residents, which may also be beneficial to the oral health physicians of the countries where ‘Domiciliary dental care’ is the novel concept.
GRAYING OF THE POPULATION AND DEMOGRAPHIC PROFILE
Owing to advanced therapeutic modalities, the life expectancy has increased to 67.9 years leading to an alarming rise in the number of residents with general and oral morbidity.[3,4]
In developing countries, the projected population of those aged 65 years and above will be 470 million by 2020.[5] By 2050, one third of the world population will be over 60 years.[6]
In India, the elderly population was 20 million in 1951 and 57 million in 1991followed by a sharp increase in 2001.[7] According to observed growth rates for this period, the growth of the “‘65+’” population was more than the total population.[2] It is expected to rise to 100 million in 2013; with a projected population in 2050 of 324 million.
The number of centenarians in India is about 2,00,000 and above.[7,8] According to 2010 estimates, out of the 5.2% of the elderly population, 28,816,115 constitutes are males and 31,670,841 females.[9] The two striking features regarding the elderly population of India are as follows: (i) the rate of growth of the elderly population is much faster than the growth of the total population; and (ii) the feminization of the elderly population.[8]
The residents are the neglected segment of the society. Surveys carried out in these strata are haphazard, hence no reliable data are available regarding the total number of residents and their distribution, the period of stay in the residences and their general and oral health status. As of 1998, there were 728 old age homes in India,[10] the number has now increased to over thousands.[11] Of the “‘65+’” population in India, about 75% remain active to carry out one major routine activity of their life, whereas approximately 25%, although not hospitalized face limitations as a result of chronic diseases. At any given time, about 10% are under active medical care in hospitals or nursing homes, while others reside in senior citizen centers, ashrams or old age homes.[2]
MEDICAL DISEASES IN THE ELDERLY
The general conditions which account to dependency in elderly are summarized in Tables 1 and 2.[5,7,8,7,12]
Table 1.
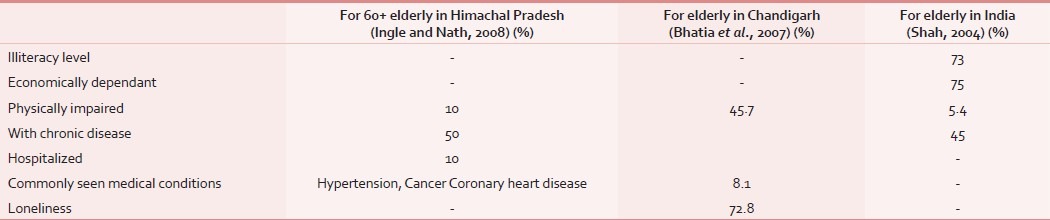
Table 2.
Common medical conditions with percentage, observed in 257 institutionalized residents of Greece with mean age of 83.7 years[12,7]
CATEGORIES OF RESIDENTS
The various ways in which the elderly residents can be categorized could be based on:
-
Level of independence and functional status of the resident:[2]
- Well elderly – independent living- with one or more chronic medical diseases
- Frail elderly – independent living: With coexistent minor and major chronic debilitating medical disease, dependent on drugs and few institutionalized
- Functionally-dependent elderly – same as category 2 but the independence is not possible – homebound or institutionalized.
- Severely disabled, medically compromised Elderly – health status deteriorated to the degree it requires maintenance, hospital and skilled nursing facility.
-
Ouslander et al.s categorization:[1]
- Short stayers – those who remain in the facility for less than 6 months
- Long stayers – residing in the facility for more than 6 months and can be subdivided into cognitively impaired, physically impaired or a combination of both.
-
Categorization of institutionalized individuals into:[13]
- Group of people with sufficient neuro-motor skills, adequate vision and motivation
- People with inadequate neuro-motor skills, and who need assistance to maintain oral hygiene
- People with poor or inadequate neuro-motor skills, and who are unable to maintain their oral hygiene.
CHARACTERISTICS OF THE RESIDENTS
The elderly people are characterized by their diversity in economy, literacy level and health status. The characteristics of the residents have a dramatic contrast to those living their life independently. Loss of independence, cognitive problems, forgetfulness, lack of motivation, physical disability layered with chronic medical problems in them contribute to diminish the self care ability thereby enhancing their susceptibility to oral diseases.[1,2,12–14]
Macgrath and Bedi interviewed 454 elders to determine whether older people perceive oral health as being important to the quality of life. For 72% of them oral health status was important for a variety of reasons, its impact on eating, and ability to socialize without embarrassment and comfort are considered most significant.[15]
ORAL DISEASES IN RESIDENTS
In India, oral health problems and the treatment needs in the geriatric population are not fully documented in the literature. Indiscriminate studies and paucity of data on residents depicts the proportionate degree of negligence towards the oral health conditions in residents. By and large, there is a hike in the incidence of root caries, edentulousness, periodontal problems and oral mucosal disorders.
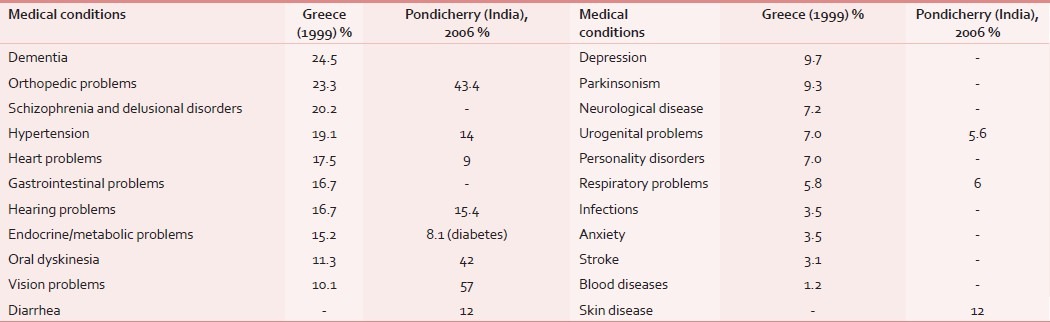
In India, Dental Council conducted National oral health surveys in 65 to 74 year old elderly in urban and rural households in each state in 2002-2003 as per the WHO recommendations. The data collected could be tabulated as in Table 3.[16] Rao et al.[17] assessed the oral health status in 287 institutionalized residents in Mangalore in India. It was observed that none of the subjects had completely healthy periodontium,[17] as shown in Table 4. The community based survey in adults and in elderly in India, revealed that the large segment of the adult population is toothless,[4] as shown in Table 4. Soben Peter studied the prevalence of oral diseases in elderly in India,[18] as shown in Table 4.
Table 3.
Number or percent distribution of 65 to 74 year old subjects in various states in India by their oral health status for 2002-2003[16]
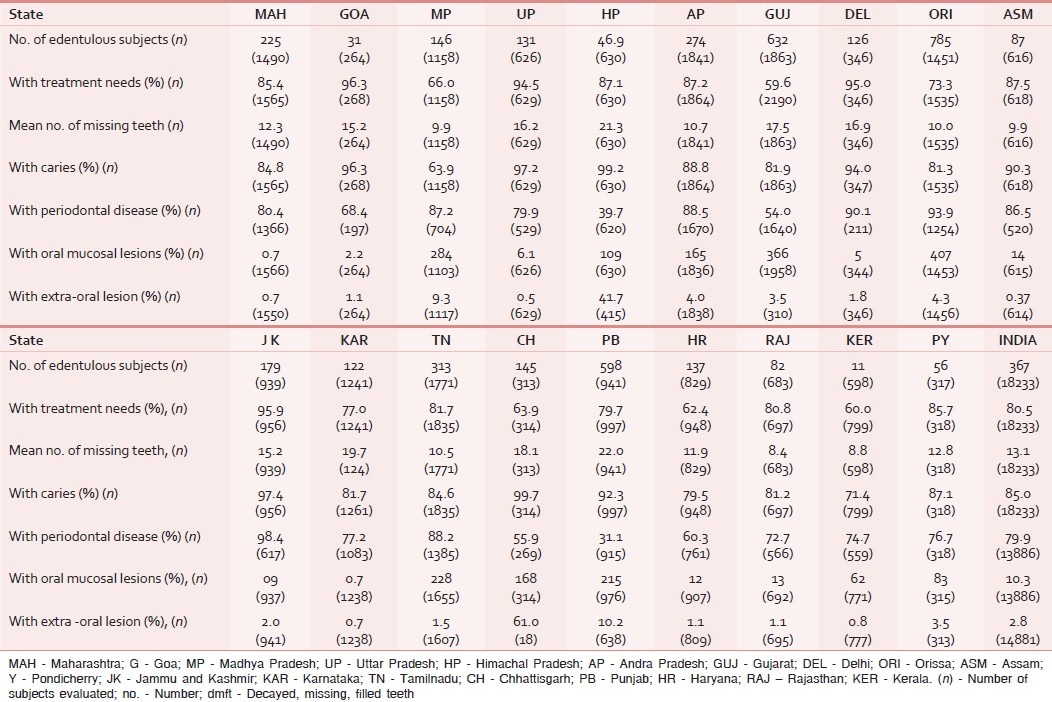
Table 4.
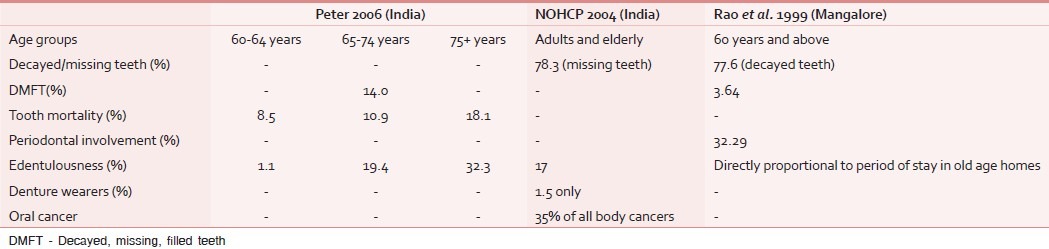
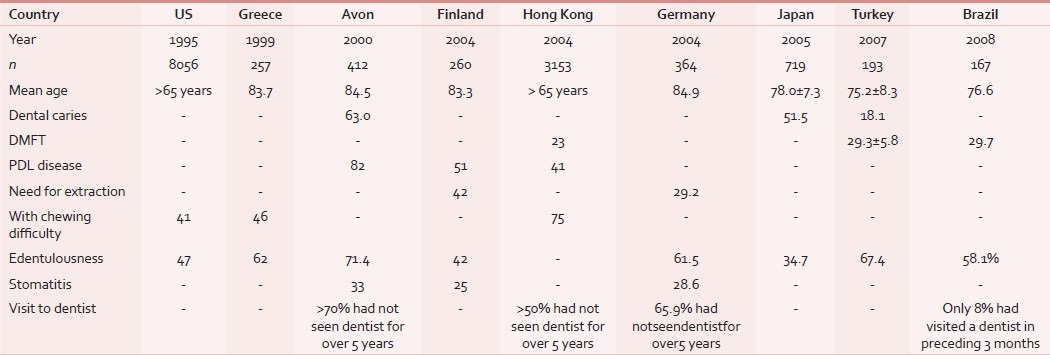
Table 5 shows the archive of the features of the oral health status in elderly residents in various countries which suggests the increased prevalence of dental caries, periodontal disease and edentulousness in them.[12,14,19,25]
Table 5.
Archiving of features of oral health status observed in elderly residents in various countries in percentage[12,14,19–25]
Oral health related quality of life was assessed in 255 chronically ill elderly residing in the facility by Peltola et al.[26] as follows:
-
Based on a questionnaire, representing three dimensions with the number of residents—
- Functional limitations e.g. the patient cannot eat normal food – 77
- Pain or discomfort-related limitations e.g. pain or discomfort while eating – 3
- Psychosocial limitations e.g. the patient has been concerned about oral health – 14
-
Categorization based on oral health assessed by clinical examination
- Very Poor and Poor – 48%
- Moderate – 33%
- Good and Excellent – 19%
ORAL HEALTH SERVICES IN INDIA
Oral health services in India are rendered through[27,28] –
Government and private institutions
Private practitioners
Professionals employed by government, e.g. dentists in defense services
Dental services are also being rendered in district hospitals and in nursing home with dental wings etc.
India is currently home to about 1.19 billion people representing about 17% of the earth's population.[29] Over 72% of people live in rural areas.[4,9] The geriatric population constitutes the major portion of the rural population, about 80% of the elderly resides in rural India, and among them 73% are illiterate and 75% are economically dependent.[8] India is a developing nation where rural agriculture has a tremendous impact on the national economy. The flip side is that the majority of the rural population is below poverty line and resides in remote areas where oral health services are bare minimum or non-existent.
The distribution of dentist to meet population requirements is grossly uneven.[4,8] the dentist population ratio in rural India is 1:3,00,000. Eighty percent of dental professionals dwell in urban areas and render services to just 30% of the urban population, whereas the remaining 70% of the rural population is left with meager dental services.[2,28]
The oral health care of necessity is being delivered through primary health care infrastructure because of limited resources and manpower.[4] Additionally, health care services are being rendered in tertiary level hospitals, nursing homes and private sectors; however, these services are poorly organized. There is an unavailability of dental surgeons as well as essential facilities at primary health centers and community health centers in most of the states.[4] Except those in organized sectors like in government jobs, railways, and defense services, the majority of the elderly population has no health security.[8] Dental treatment is expensive in the private sector and considered optional by the majority of elderly and their care providers. Besides, health insurance companies do not reimburse expenses on dental treatment.
There is no separate provision for minimum dental services to even the general population; consequentially, the oral health conditions of the residents can be speculated. Dependant elderly are admitted to nursing homes or other residences where the complete health care is assumed. In contrast, it is pointed out that oral health in them is worse than the community residents, and that emergency dental treatment instead of regular oral care, is the usual reason for dental services provided to them.[14] A poor oral status contributes to eating problems, weight loss, and dehydration aggravating the existing problems of the residents.
COMPONENTS OF ORAL HEALTH SERVICES TO ELDERLY AND THE RESIDENTS
The advancement in the medical field has enabled the elderly disabled people to live longer. However due to the reduced ambulation it may be impractical for these to attend a dental clinic thus there is a rapid growth in the number of people requiring domiciliary dental care services.
Residents are unable to go to dentists by themselves and it is very cumbersome to carry them to a dentist. Hence, the best option left would be that dentist should reach them. Fiske and Lewis define domiciliary careas ‘a service that reaches out to care for those who cannot reach a service themselves’ by.[30]
To give dental care to residents, there could be four basic options:[1]
Residents themselves go to dental clinics
Dentists travelto homes or nursing homes with portable equipments
Use of van or bus to provide treatment operatory – Mobile dental service
Providing dental care in dental operatory inside the facility or nursing home.
While planning the treatment, the provisional treatment plan and the need for investigations are to be discussed with the patient, caregiver or relative. An appropriate treatment plan has to be negotiated and the informed consent should be obtained.[30] The oral professionals must be well-informed about the various medical conditions, the management of medical emergencies, gerodontology and the use of domiciliary equipments. The various skills needed are team work, time management, empathy, planning, assertiveness, flexibility, basic life support, improvization, manual handling, communication, navigation, driving, networking and liaison.[30]
Macentee and Waytt developed the “clinical oral disorders in elders” (CODE) index for disabled elders. This index is based on clinical measures of 27 disorders covering 5 major areas: Jaw movement, dentures, mucosal health, teeth and periodontium. When combined with a psychosocial index, it forms a very comprehensive indicator of oral dysfunction in the elderly.[31]
Kenneth Shay[32] has provided a five point Geriatric Dental Assessment tool called OSCAR,[32]
O, Oral – Teeth, restoration, prostheses, periodontium, pulpal status, oral mucosa, saliva
S, Systemic – normative age changes, medical diagnosis, pharmacologic agents,
C, Capability – functional ability, self-care, oral hygiene, transportation to appointments,
A, Autonomy – decision-making ability, dependence on alternative
R, Reality – Prioritization of oral health, financial ability or limitations.
Dentist must concentrate on “OSCAR” as it influences the treatment plan which needs the meticulous integration of dental and non-dental factors.
Certain factors may act as a barrier against the provision of oral health care to residents. The report by Mcntee and colleagues summarized the attitudes of dentists and their reasons for refusing the care for residents in long term care facilities as follows:[13]
55% had never been asked
33% were too busy to leave the office
25% felt inadequately trained
In 54% the level of financial reimbursement was too low
56% felt encroachment on their leisure time.
Challenges pertaining to oral health care delivery to elderly
With increased longevity, the dental disease pattern and treatment needs are changing; the elderly people are retaining more natural teeth into old age than earlier. Hence there is a proportionate rise in oral illness in elderly with numerous restorations, prostheses and even implants, all of which require specific care. Oral health maintenance for compromised people with aging dentitions will increasingly present problems for dental profession. The unwillingness toward treatment and the suboptimal perception of treatment needs in them, and the limitations on working time could be harassing to dentists. Many are unable to open their mouth or keep it open for long time. Dentists face problem right from the beginning that is in history taking due to communication and cognitive problems as well as in obtaining radiographs and in other diagnostic tests.
In essence, there is a need to modify the approach toward these patients. It may be wise for dentists to perceive why a patient is homebound or resident of a nursing home or old age home. With existing constraints, it is necessary to be extremely patient and empathetic towards them. The manner and demeanor of the oral professional with improved interpersonal skills will aid in fostering the environment with which the residents will be comfortable.
CONSIDERATIONS FOR ORAL HEALTH SERVICES PROVIDED TO ELDERLY IN INDIA
These include the following:
The central focus of preserving the oral health of the elderly and the residents is to enable them to maintain adequate physical and psychosocial functions.
First, there should be universal understanding of the importance of oral health for residents and its relationship with their overall health.
In order to evaluate the oral health status of residents significant data must be gathered, and they must be made available to those who need it.
Measures should be developed to implement and improve the oral health care strategies in the elderly and to evaluate the effectiveness of these measures.
Oral health should be incorporated into routine assessment by care staff, and the continuing dental care should be available to the residents
In view of depressingly low levels of oral health in residents, it is important to integrate the preventive, curative and educational oral health care program into the existing health and educational infrastructure.
There should be an easy access and timely approach to general and specialist dental services and to oral hygiene equipments appropriate to individual needs of residents.
-
Development of domiciliary dental services which[30]–
- enable access to dental care for people unable to travel to dental clinics
- establish liaison between health and social service professionals to identify the people who are unable to access dental care
- involve purchasers who must ensure that resources are provided to purchase necessary equipment and materials for domiciliary care
- provide the training to enable the dental team to develop and maintain the skills required to deliver domiciliary care service
- include domiciliary dental care in the undergraduate and auxiliary teaching curriculum
Screening is recommended as a mean of an initial assessment of oral health needs of residents and to identify the individuals requiring care.
Continuous dental education program must be organized to improve the knowledge, skills and attitudes of health professionals and health care workers regarding the oral health of the geriatric patients.
Dental health education must be focused on the special needs of the disabled, dependant and socioeconomically deprived geriatric population to improve their quality of life.
One of the suggestions in this direction could be to introduce ‘Geriatric Dentistry’ as an independent faculty in the undergraduate curriculum.
CONCLUSION
The content of this paper reflects the bleak picture of the lack of oral health services for the elderly people in India. The major block in oral health care of elderly and the residents would be the underestimation of the oral health care need by them. The dental care of the residents is often limited to emergency care and is not aimed at retaining teeth. Conversely, with changing attitudes the oral health goal should include: Keeping their teeth, keeping their teeth healthy and keeping their teeth pretty.[33]
The best option to serve the residents would be “Home dentistry or Domiciliary dental care,” however it is yet an infrequent practice in India. Surveys should be conducted in this sector very routinely to spot the residents in the need of oral care circumscribing nursing homes, old age homes, ashrams, secure units and community households.
There is a considerable lack in the sense of responsibility towardthe residents. For disabled elderly without any support the old age homes or nursing homes are becoming a requisite; the gravity of this problem may amplify further. The effective strategy would be a personal commitment. In future we may be one of these dependants to need the health service at our destinations.
Comprehensive oral care of this under-served population is a multidisciplinary approach that involves the conglomeration of health professionals, institutions, health associations, government and non-government agencies, social services, funding agencies, insurance companies and charity organizations to plan the infrastructure at the national level to take a step forward to a path yet unpaved.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Robert GH, Barry C. Practical Consideration in special patient Care, Delivering dental care to nursing home and homebound patients. Dent Clin North Am. 1994;38:537–51. [PubMed] [Google Scholar]
- 2.Chandra S, Chandra S. Text Book of Community Dentistry. 1st ed. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd India; 2004. Geriatric Dental health Care; pp. 239–51. [Google Scholar]
- 3.True knowledge, the internet answer engine. [Last accessed on 2010]. Available from http://www.trueknowledge.com/q/Life expectancy in India .
- 4.Editorial—National oral health care programme (NOHCP) implementation strategies. Indian J Community Med. 2004;29:1–10. [Google Scholar]
- 5.Bhatia SPS, Swami HM, Thakur JS, Bhatia VA. Study of health related problems and loneliness among the elderly in Chandigarh. Indian J Community Med. 2007;4:255–8. [Google Scholar]
- 6.The Challenge of Longevity. Ageing Demographics. [Last accessed on 2009 Mar 16]. Available from: http://www.iahsa.wordpress.com .
- 7.Ingle GK, Nath A. Geriatric health care in India: Concern and Solutions. Indian J Community Med. 2008;33:214–8. doi: 10.4103/0970-0218.43225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah N. Oral health care system for elderly in India. Geriatr Gerontol Int. 2004;4:S162–4. [Google Scholar]
- 9.Demographics of India, from Wikipedia, the free encyclopedia. [last accessed on 2010]. Available from: http://en.wikipedia.org/wiki/Demographics_of_India .
- 10.Venkatesh S. Available from Old Age Homes in India.htm. [Last accessed on Jun 2009] [Google Scholar]
- 11.Old age homes-Housing facility. Available from Citizens National portal of India.htm, india.gov.in, [Last accessed on 2008] [Google Scholar]
- 12.Kossioni AE, Karkazis HC. Socio-medical condition and oral functional status in an older institutionalized population. Gerodontology. 1999;16:21–8. doi: 10.1111/j.1741-2358.1999.00021.x. [DOI] [PubMed] [Google Scholar]
- 13.Ettinger RL, Baum BJ. Oral care for the homebound and institutionalized. Oral and dental problems in elderly. Clin Geriatr Med. 1992;8:659–72. [PubMed] [Google Scholar]
- 14.Frenkel H, Harvey I, Newcombe R. Oral health care amongst nursing home residents in Avon. Gerodontology. 2000;17:33–8. doi: 10.1111/j.1741-2358.2000.00033.x. [DOI] [PubMed] [Google Scholar]
- 15.Macgrath C, Bedi R. The importance of oral health to older people's quality of life. Gerodontol. 1999;16:59–63. doi: 10.1111/j.1741-2358.1999.00059.x. [DOI] [PubMed] [Google Scholar]
- 16.Bali RK, Damle SG, Muglikar SD, Yethwar RR, Mathur VB, Talwar PP, et al. National oral health surveys and fluoride mapping 2002-2003. New Delhi: Dental council of India; 2004. [Google Scholar]
- 17.Rao A, Sequeira P, Peter S, Rajeev A. Oral health status of the institutionalized elderly in Mangalore, India. Indian J Dent Res. 1999;10:55–61. [PubMed] [Google Scholar]
- 18.Peter S. Essential of Preventive Dentistry. 3rd ed. New Delhi: Arya (MEDI) Publishing House India; 2006. Oral health care system: A global perspective; pp. 711–8. [Google Scholar]
- 19.Gift H, Cherry-peppers G, Oldakowski R. Oral health status and related behaviors of U. S. nursing home residents. Gerodontology. 1995;14:89–99. doi: 10.1111/j.1741-2358.1997.00089.x. [DOI] [PubMed] [Google Scholar]
- 20.Peltola P, Vehkalahti M, Wuolijoki-Saaristo K. Oral health and treatment needs of the long-term hospitalized elderly. Gerodontology. 2004;21:93–9. doi: 10.1111/j.1741-2358.2004.00012.x. [DOI] [PubMed] [Google Scholar]
- 21.Lo EC, Luo Y, Dyson JE. Oral health status of institutionalized elderly in Hong Kong. Community Dent Health. 2004;21:224–6. [PubMed] [Google Scholar]
- 22.Knabe C, Kram P. Dental care for institutionalized geriatric patients in Germany. J Oral Rehabil. 1997;24:909–12. doi: 10.1046/j.1365-2842.1997.00196.x. [DOI] [PubMed] [Google Scholar]
- 23.Shimazaki Y, Soh I, Kola T, Miyazaki H, Takehara T. Relationship between dental care and oral health in institutionalized elderly people in Japan. J Oral Rehabil. 2004;3:837–42. doi: 10.1111/j.1365-2842.2004.01320.x. [DOI] [PubMed] [Google Scholar]
- 24.Şengül U, Saadet G, Bahar GD. Oral health status of the elderly in a residential home in Turkey. Gerodontol. 2007;24:22–9. doi: 10.1111/j.1741-2358.2007.00136.x. [DOI] [PubMed] [Google Scholar]
- 25.Luciene G, Maria EL, Jose F, Peter L, Jorg H. Poor dental status and oral hygiene practices in institutionalized older people in northeast Brazil. Int J Dent. 2009;2009:1–6. doi: 10.1155/2009/846081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peltola P, Vehkalahti M, Simoila R. Oral health related well-being of the long-term hospitalized elderly. Gerodontology. 2005;22:17–23. doi: 10.1111/j.1741-2358.2004.00052.x. [DOI] [PubMed] [Google Scholar]
- 27.Vivekanand SK. Dental Public Health, Manual of Community Dentistry. 1st ed. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd India; 2004. [Google Scholar]
- 28.Rao TR Gururaja. In: Textbook of Community Dentistry. New Edition. Chennai: All India Publishers and Distributors; 2004. National Health Care Programme- Implementation of Strategy; pp. 17–24. [Google Scholar]
- 29.True knowledge, the internet answer engine. [Last accessed on 2010]. http://www.trueknowledge.com/q/what_is_the_population_of_india_in_2010 .
- 30.Fiske J, Lewis D. The development of standards for domiciliary dental care services: Guidelines and recommendations. Report of British society for disability and oral health (BSDH) working group. Gerodontology. 2000;17:119–22. doi: 10.1111/j.1741-2358.2000.00119.x. [DOI] [PubMed] [Google Scholar]
- 31.Macentee MI, Waytt CC. An index of clinical oral disorder in elders (CODE) Gerodontol. 1999;16:85–96. doi: 10.1111/j.1741-2358.1999.00085.x. [DOI] [PubMed] [Google Scholar]
- 32.Shay K. Practical Consideration in special patient Care, Identifying the needs of the elderly dental patients-The Geriatric assessment. Dent Clin North Am. 1994;38:499–523. [PubMed] [Google Scholar]
- 33.Niessen L. Geriatric dentistry in next millennium: Opportunities in leadership in next millennium. Overview Lecture. Gerodontology. 2000;17:4–7. doi: 10.1111/j.1741-2358.2000.00003.x. [DOI] [PubMed] [Google Scholar]


