Abstract
Glycated hemoglobin (HbA1c) is an important indicator of glycemic control in diabetes mellitus, based on which important diagnostic and therapeutic decisions are routinely made. However, there are several situations in which the level of HbA1c may not faithfully reflect the glycemic control in a given patient. Important among these is the use of certain non-diabetic medications, which can affect the HbA1c levels in different ways. This review focuses on the non-diabetic medications which can inappropriately raise or lower the HbA1c levels, and the postulated mechanisms for the same.
Keywords: Dapsone, diabetes, glycated hemoglobin
INTRODUCTION
Diabetes mellitus has assumed epidemic proportions worldwide, causing much morbidity and mortality on account of its various complications. The development of chronic vascular complications of diabetes such as retinopathy, nephropathy and cardiovascular disease is intimately linked to the level of glycemic control attained by the individual with diabetes. Therefore, it is essential to have an index of the long-term glycemic control in diabetes patients, which in turn can be used to guide therapy and predict the likelihood of complications.
Glycated hemoglobin (HbA1c) was first described by Rahbar et al. in 1969.[1] Subsequent studies showed that the level of HbA1c correlated well with the glycemic control over a period of 2 to 3 months, leading to the gradual incorporation of the test into clinical practice in the 1980s.[2] With the publication of the Diabetes Control and Complications Trial[3] and the United Kingdom Prospective Diabetes Study,[4] both of which correlated the HbA1c levels to the development of diabetes complications, HbA1c estimation has become established as a cornerstone of diabetes management.
Hemoglobin (Hb) is a tetramer formed of two alpha and two beta globin chains. On exposure to high levels of blood glucose, hemoglobin gets non-enzymatically glycated at different sites in the molecule. HbA1c is formed when glucose gets added on to the N-terminal valine residue of the beta chain of Hb.[5] The levels of HbA1c in the blood reflect the glucose levels to which the erythrocyte has been exposed during its lifespan (approximately 117 days in men and 106 days in women). Therefore, the HbA1c is an index of the level of glycemic control over the preceding 2 to 3 months. Of this period, the immediately preceding 30 days contribute 50% to HbA1c.[5]
A number of methods are in use for measuring HbA1c. The most widely used assay utilizes high-performance liquid chromatography (HPLC). Other methods include boronate affinity assay and immunoassays. Efforts are underway to standardize the assay worldwide.[6]
The main use of HbA1c is in the monitoring of patients with diabetes. HbA1c targets of less than 6.5 to 7% have been proposed by various organizations to define good control of diabetes.[7,8] The efficacy of anti-diabetic medications is also assessed based on their HbA1c lowering capacity. Many algorithms for the management of diabetes utilize HbA1c as the basis for major therapeutic decisions. Recently, HbA1c has also been recommended as a tool for the diagnosis of diabetes.[9]
Fallacies in the Use of HbA1c
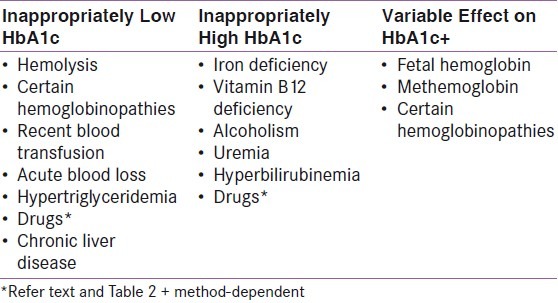
Although HbA1c is, in general, a robust marker of glycemia, there are certain conditions in which the test can be unreliable. Use of the newer assays like HPLC can eliminate some, but not all of these errors. Some of the important factors that can affect the HbA1c levels are listed in Table 1. The remainder of this review will focus on (non-diabetic) drugs which may falsely increase or decrease the HbA1c level.
Table 1.
Conditions causing inappropriately high or low Hba1c[10]
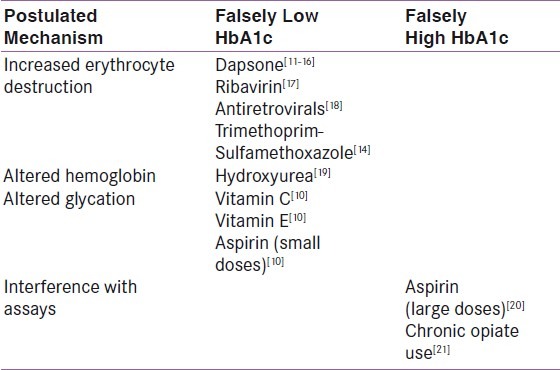
Drugs and HbA1c
Drugs can theoretically interfere with HbA1c levels in several ways [Table 2]. However, only a few instances of drug-induced variability in HbA1c have actually been reported in the literature.
Table 2.
Drugs causing inappropriately low or high HbA1c
Drugs causing hemolysis
Any drug which causes hemolysis can potentially lower the HbA1c by reducing erythrocyte lifespan, thereby increasing the proportion of younger cells in the blood. Dapsone, ribavirin and antiretroviral drugs have been reported to reduce the HbA1c in this manner.
The earliest report of dapsone-induced reduction in HbA1c was from the UK in 1979.[11] The patient in question had been taking dapsone for dermatitis herpetiformis. Over a period of five years, his HbA1c declined to 3.7% in spite of uncontrolled blood glucose levels. Further investigation revealed a raised reticulocyte count, indicating hemolysis. Later, in 2002, there was a report each from France[12] and the US[13] concerning the same phenomenon. The patients in question had been put on dapsone for polychondritis and necrobiosis lipoidica diabeticorum, respectively, and reduction in the dose of dapsone was followed by a return of HbA1c levels to the appropriate range in the latter case. There was no evidence of significant hemolysis in either case, although subclinical hemolysis could not be ruled out. In 2003, Polgreen et al.[14] reported two HIV positive individuals with diabetes who had been put on dapsone for prophylaxis of Pneumocystis carinii infection. Both patients had excellent HbA1c values in spite of high self-reported and lab blood glucose measurements. Concomitant use of dapsone with sulfapyridine has also been reported to lower the HbA1c in patients with type 1 diabetes.[15] In this issue we have reported two cases of dapsone-induced reduction in HbA1c from India.[16] None of the above eight patients had anemia.
Dapsone can also promote the oxidation of hemoglobin to methemoglobin, which may interfere with the HPLC assay used to measure HbA1c. Dapsone has also been postulated to reduce erythrocyte survival independent of its hemolytic effect.[13]
The potential HbA1c lowering effect of dapsone assumes special significance in India in view of the widespread use of this agent in the treatment of Hansen's disease and many other conditions.
Other agents which have been reported to lower the HbA1c levels through hemolysis include ribavirin, antiretroviral agents and sulfonamides. In 2008, Robertson[17] reported the case of a 55-year-old male patient put on ribavirin for chronic hepatitis C infection, who subsequently presented with an HbA1c level of 4.4%, in spite of persistently high blood glucose values. Stoppage of ribavirin was followed by an increase of HbA1c to 6.5%. In a study of 112 HIV-infected individuals, Diop et al.[18] found that the HbA1c underestimated mean fasting glycemia by 12.3% as compared to 1238 non HIV-infected individuals. Treatment with nucleoside analogue antiretroviral agents was found to be associated with macrocytosis and a low serum haptoglobin level, suggesting the presence of subclinical hemolysis in these patients. In the series quoted above, Polgreen et al.[14] also reported on an HIV positive patient who presented with inappropriately low HbA1c levels following administration of trimethoprim-sulfamethoxazole.
In most of the above cases, the degree of hemolysis was not sufficient to produce anemia or jaundice. Other markers of hemolysis like a raised level of lactate dehydrogenase, low serum haptoglobin and increased reticulocyte count, combined with a high index of clinical suspicion, were essential in making the diagnosis.
Agents interfering with glycation
High doses of antioxidant agents such as Vitamin C and E have been reported to lower the HbA1c by reducing the rate of glycation of hemoglobin, but the degree to which this occurs with pharmacological doses is uncertain. Camargo et al.[20] did not find any impact on the HbA1c when pharmacological doses of vitamin C or E were administered in patients with diabetes for 4 months. Chronic use of aspirin has been reported to falsely decrease the HbA1c by the same mechanism.[10]
Agents altering erythropoiesis
Patients with anemia due to deficiency of iron and vitamin B12 have high HbA1c levels. This can be reversed with administration of the deficient factor. In some cases, administration of iron and vitamin B12 can lead to falsely lowered HbA1c due to the preponderance of young erythrocytes in the circulation.[20] Treatment with erythropoietin has the same effect.[22]
Agents altering hemoglobin
Hydroxyurea is an antimetabolite which is used for the treatment of myeloproliferative disorders and sickle cell disease. The drug promotes a shift in the hemoglobin pattern from HbA to HbF, with a concomitant apparent decrease in HbA1c levels.[19]
Agents interfering with the HbA1c assay
Chronic use of aspirin in large doses can lead to acetylation of hemoglobin, leading to falsely elevated HbA1c levels due to interference with some of the assays used. Camargo et al.[20] reported an increase of 0.17% in the HbA1c of 28 non-diabetic subjects administered 200 mg of aspirin per day for 4 months. A subsequent study by the same author,[23] however, failed to show any interference of aspirin in the HbA1c (measured by ion-exchange HPLC) in type 2 diabetes patients. In clinical practice, the effect of aspirin on HbA1c is likely to be significant only when large doses are administered over a long period of time.
Chronic opiate use has been reported to increase HbA1c levels,[21] but the exact mechanism remains unknown.
CONCLUSION
HbA1c is now universally accepted as an index of long-term glycemic control and major therapeutic decisions are undertaken based on it. There is increasing interest in using HbA1c for the diagnosis of diabetes as well. While the availability of newer assays has removed many of the technical problems associated with the estimation of HbA1c, several fallacies remain. There are a number of drugs, some of them quite commonly used, which can cause inappropriately high or low HbA1c levels for the degree of glycemia. It is essential that clinicians be aware of these interactions, and exercise caution in interpreting the HbA1c levels of such patients, so that potentially serious errors can be avoided.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rahbar S, Blumenfeld O, Ranney HM. Studies of an unusual haemoglobin in patients with diabetes mellitus. Biochem Biophys Res Commun. 1969;36:838–43. doi: 10.1016/0006-291x(69)90685-8. [DOI] [PubMed] [Google Scholar]
- 2.Gonen B, Rubenstein A, Rochman H, Tanega SP, Horwitz DL. D. Haemoglobin A1: An indicator of the metabolic control of diabetic patients. Lancet. 1977;2:734–7. doi: 10.1016/s0140-6736(77)90237-9. [DOI] [PubMed] [Google Scholar]
- 3.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 4.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood glucose control with sulfonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 5.Goldstein DE, Little RR, Lorenz RA, Malone JI, Nathan D, Peterson CM, et al. Tests of glycemia in diabetes. Diabetes Care. 2004;27:1761–63. doi: 10.2337/diacare.27.7.1761. [DOI] [PubMed] [Google Scholar]
- 6.The American Diabetes Association, European Association for the Study of Diabetes, International Federation of Clinical Chemistry and Laboratory Medicine and the International Diabetes Federation. Consensus statement on the worldwide standardization of the HbA1c measurement. Diabetologia. 2007;50:2042–3. doi: 10.1007/s00125-007-0789-7. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2012;35(Suppl 1):S11–63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodbard HW, Jellinger PS, Davidson JA, Einhorn D, Garber AJ, Grunberger G, et al. Statement by an American association of clinical endocrinologists/ american college of endocrinology consensus panel on type 2 diabetes mellitus: An algorithm for glycemic control. Endocr Pract. 2009;15:540–59. doi: 10.4158/EP.15.6.540. [DOI] [PubMed] [Google Scholar]
- 9.The International Expert Committee. International Expert Committee report on the role of the A1c assay in the diagnosis of diabetes. Diabetes Care. 2009;32:1327–34. doi: 10.2337/dc09-9033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gallagher EJ, Le Roith D, Bloomgarden Z. Review of hemoglobin A1c in the management of diabetes. J Diabetes. 2009;1:9–17. doi: 10.1111/j.1753-0407.2009.00009.x. [DOI] [PubMed] [Google Scholar]
- 11.Kesson CM, Whitelaw JW, Ireland JT. Drug-induced haemolysis and fast haemoglobin A1 in diabetes mellitus. Br Med J. 1979;2:1037–8. doi: 10.1136/bmj.2.6197.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Serratrice J, Granel B, Swiader L, Disdier P, de Roux- Serratrice C, Raccah D, et al. Interference of dapsone in HbA1c monitoring of a diabetic patient with polychondritis. Diabetes Metab. 2002;28:508–9. [PubMed] [Google Scholar]
- 13.Albright ES, Ovalle F, Bell DS. Artifactually low hemoglobin A1c caused by use of dapsone. Endocr Pract. 2002;8:370–2. doi: 10.4158/EP.8.5.370. [DOI] [PubMed] [Google Scholar]
- 14.Polgreen PM, Putz D, Stapleton JT. Inaccurate glycosylated hemoglobin A1c measurements in human immunodeficiency virus-positive patients with diabetes mellitus. Clin Infect Dis. 2003;37:e53–5. doi: 10.1086/376633. [DOI] [PubMed] [Google Scholar]
- 15.Tack CJ, Wetzels JF. Decreased HbA1c levels due to sulfonamide-induced hemolysis in two IDDM patients. Diabetes Care. 1996;19:775–6. doi: 10.2337/diacare.19.7.775. [DOI] [PubMed] [Google Scholar]
- 16.Unnikrishnan R, Anjana RM, Uthra S, Jayashri R, Mohan V. Unexpectedly low HbA1c levels In a diabetes patient following dapsone use. Indian J Endocrinol Metab. 2012;16:658–9. doi: 10.4103/2230-8210.98037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robertson M. Artificially low HbA1c associated with ribavirin. BMJ. 2008;336:505. doi: 10.1136/bmj.39457.828287.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Diop ME, Bastard JP, Meunier N, Thévenet S, Maachi M, Capeau J, et al. Inappropriately low glycated hemoglobin values and hemolysis in HIV-infected patients. AIDS Res Hum Retroviruses. 2006;22:1242–7. doi: 10.1089/aid.2006.22.1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karsegard J, Wicky J, Mensi N, Caulfield A, Philippe J. Spurious glycohemoglobin values associated with hydroxyurea treatment. Diabetes Care. 1997;20:1211–2. doi: 10.2337/diacare.20.7.1211. [DOI] [PubMed] [Google Scholar]
- 20.Camargo JL, Stifft J, Gross JL. The effect of aspirin and vitamins C and E on HbA1c assays. Clin Chim Acta. 2006;372:206–9. doi: 10.1016/j.cca.2006.03.031. [DOI] [PubMed] [Google Scholar]
- 21.Ceriello A, Giugliano D, Dello Russo P, Sgambato S, D’Onofrio F. Increased glycosylated haemoglobin A1 in opiate addicts: Evidence for a hyperglycaemic effect of morphine. Diabetologia. 1982;22:379. doi: 10.1007/BF00253587. [DOI] [PubMed] [Google Scholar]
- 22.Ng JM, Cooke M, Bhandari S, Atkin SL, Kilpatrick ES. The effect of iron and erythropoietin treatment on the HbA1c of patients with diabetes and chronic kidney disease. Diabetes Care. 2010;33:2310–3. doi: 10.2337/dc10-0917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Camargo EG, Pedrini RO, Gross JL, Camargo JL, Silveiro SP. Lack of interference of aspirin in HbA1c measured by ion-exchange HPLC in type 2 diabetic patients: A randomized, double-blind, placebo-controlled study. Clin Chim Acta. 2008;391:120–2. doi: 10.1016/j.cca.2008.01.029. [DOI] [PubMed] [Google Scholar]


