Abstract
Aims:
The aim was to assess the dietary pattern during Ramadan season among type 2 diabetic Muslim subjects who underwent fasting and intensive dietary counseling.
Materials and Methods:
The study was conducted among 70 Muslim subjects with type 2 diabetes mellitus who undertook fasting during Ramadan and was part of a randomized control trial using pioglitazone published previously. All subjects were subjected to a dietary assessment and counseling at three stages, i.e., initiation of the study, mid-Ramadan and post-Ramadan, by a trained dietician. Dietary assessment was done by the 24-hour dietary recall method and the food frequency questionnaire. Diabetic diet sheets were dispensed to subjects based on their body mass index (BMI), daily activity, and needs.
Results:
The mean caloric intake between pre-Ramadan (before fasting) and mid-Ramadan (15 days after fasting) were 1506.80 kcal and 1614.29 (P = 0.001) respectively. The distribution of active components pre and during Ramadan were: carbohydrates (g) 260.76 and 265.35 g (P = 0.001), proteins (g) 43.64 and 46.19 (P = 0.001) and fat (g) was 32.88 and 44.16 (P = 0.0001) respectively. The percentage of energy from dietary carbohydrate prior to fasting (64.11 ± 6.73) and during fasting (68.41 ± 4.41) remained almost unchanged but statistically significant when compared at different intervals before and during fasting. Fat intake increased significantly during fasting (P = < 0.001).
Conclusions:
The dietary composition in a type 2 diabetic Muslim population who undertook fasting during Ramadan showed a mean increase in consumption of all components of diet during the period of fasting. Nutritional compliance during such a time seems to be difficult and warrants repeated counseling and regular follow-up to achieve targets.
Keywords: Diet, Ramadan, type 2 diabetes mellitus
INTRODUCTION
Ramadan is a holy month observed by Muslims all over the world, during which fasting is rigorously observed from dawn until sunset. The duration of fasting varies by geographical location and season. During summer and northern latitudes, the fast can last up to 18 hours or more. Fasting begins after a meal before dawn (sahur) and is completed after sunset by usually consuming sweetened water or dates followed by a meal (iftar). Individuals are exempted from Ramadan fasting in circumstances such as illness or menstruation that could adversely affect health outcomes leading to interruption of fasting during such periods. In such cases, fasting is adjourned to a later period of time. During fasting it is generally assumed that the calorie consumption is low and there is a greater tendency for hypoglycemia and irregular glycemic control in subjects with type 2 diabetes mellitus.(T2DM).
The effect of experimental short-term fasting on carbohydrate metabolism has been published in the literature.[1,2] It has been uniformly found that a slight decrease in serum glucose from 3.3 mmol to 3.9 mmol (60 mg/dl to 70 mg/dl) occurs in normal adults a few hours after fasting has begun.[3] However, this reduction in serum glucose tends to cease due to increased gluconeogenesis in the liver during fasting, and related decrease in insulin concentration and a rise in glucagon and sympathetic activity.[2–4] Glycogen stores, along with some degree of gluconeogenesis, may maintain normal serum glucose when a fast follows a large pre-dawn meal.[4]
The EPIDAR study that recruited 12,914 Muslim diabetic subjects from thirteen countries reported prevalence estimates of fasting during Ramadan as 43% for type 1 diabetes mellitus and 86% for T2DM.[5] Although this study was the largest epidemiological report that described diabetes-related practices during Ramadan, the study failed to include a detailed dietary assessment during the fasting period although the authors report unaltered life style practices in about 50% of the individuals during Ramadan. It is generally perceived that calorie consumption is restricted during the fasting period, but there exists some degree of dietary indiscretion during the non-fasting period with excessive compensatory eating, which may contribute to hyperglycemia and weight gain.[6,7] There is paucity of information available on dietary practices and diet components during Ramadan fasting. Since calorie restriction, adherence to dietary counseling and maintenance of balanced diet forms an integral component of general diabetes management and especially during critical periods such as fasting, the current study aimed to evaluate dietary patterns and diet-adherence at different time points during 30-day fasting period of Ramadan amongst Muslims living in South India.
Diabetes management during fasting is challenging since physical activity is restricted and pharmacological therapy is usually lowered in fear of hypoglycemia. Therefore appropriate glycemic control largely relies on appropriate diet modulation of diet that efficiently maintains the blood glucose and counter-balances the fasting effects, especially hypoglycemia, without compromising religious fasting. The importance of dietary management have been strongly underscored by the diabetes control and complications trial (DCCT) and UK prospective diabetes study (UKPDS).[8–10] Although, during Ramadan, the benefits of fasting appear only in patients who maintain their appropriate diets.[11,12] most patients with diabetes find it increasingly difficult to understand and adhere to the nutritional component of their treatment.[11–14] In the current study, we therefore describe the general dietary pattern followed by Muslims during religious fasting and the degree of compliance to the prescribed diet during Ramadan
MATERIALS AND METHODS
Subjects
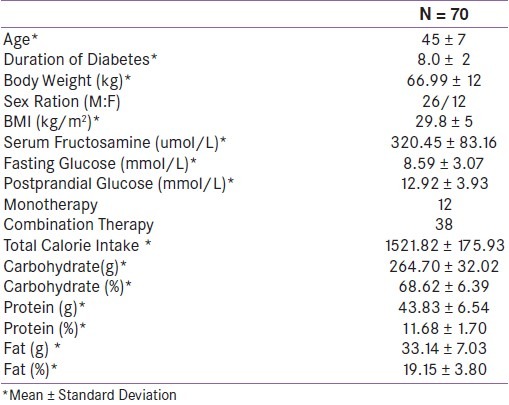
All subjects in this dietary survey were Muslims with T2DM who intended to undertake fasting for the entire holy month of Ramadan (30 days). The participants were recruited from an original multicenter, randomized double blind, placebo controlled trial where Pioglitazone was used along with conventional OHAs to assess the status of glycemic control and incidence of hypoglycemia during Ramadan described elsewhere.[15] Table 1 shows the baseline characteristics of subjects who participated in the study prior to any type of dietary assessment.
Table 1.
Baseline characteristics of subjects who took part in the dietary survey
Study protocol
All subjects were subjected to 24-hour dietary recall and diabetic diet counseling at screening. Follow-up dietary assessment was carried out at three stages, i.e., before initiation of Ramadan fasting, mid-Ramadan (15 days after initiating fasting) and post-Ramadan (1 week after completing the fasting period) by a trained dietician. Diet was assessed using 24-hour dietary recall method and through standard questionnaires based on food frequencies as detailed below. Reinforcement of standard dietary practices was done at all three stages. The flow of patients in the study is summarized in Figure 1.
Figure 1.
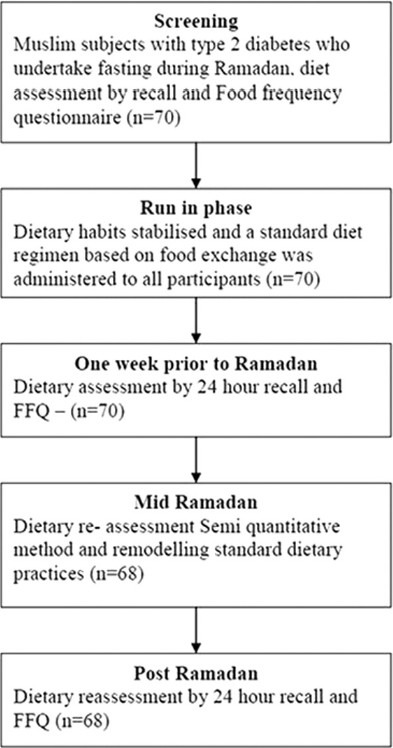
Study design; flow of patients
Dietary Recall and Food Frequency Questionnaire
Regular dietary pattern was obtained by a 24-hour recall method, and quantitative food assessment was done using a food frequency questionnaire. Food frequency questionnaires (FFQ) based on self-reported intake of daily food have been shown to validly measure long-term dietary patterns in epidemiological studies.[16,17] The food frequency questionnaire used for the assessment of nutrient intake in the North Indian population was easy to administer, showed moderate to good correlation with the 5-day diet record, and was reproducible.[18] A set of standardized cups, spoons, and glasses were used to aid the subject to recall the quantity of food prepared and consumed. The amount of food intake and raw ingredients used for each food preparation was obtained individually from each subject using reference standardized cups. Participants were asked to recall their usual intake of foods and beverages over the past 6 months. Both the frequency of intake and the serving size were ascertained. The subject's intake in terms of raw equivalent was calculated as the product of the total raw amount of each ingredient and the amount of cooked food intake divided by the total food cooked per day. This method is useful in obtaining qualitative details of diet and the pattern of food consumption at household level and also includes assessment of the frequency of consumption of different foods on daily, weekly, fortnight or occasional basis.[18] Participants were also queried with regard to the special dietary practices they followed during the fasting period, the use of dietary supplements, and food preparation methods.
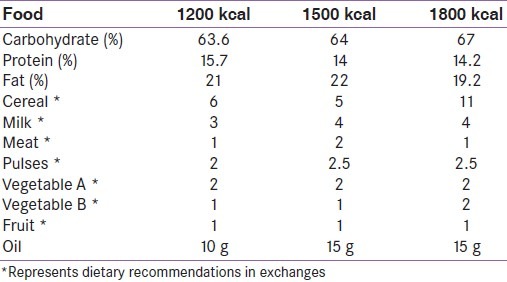
The raw equivalent of the food consumed was then calculated. Energy, carbohydrates, proteins, fat, and fiber were calculated using the food composition table reference from National Institute of Nutrition and Indian Council for Medical Research.[13] Based on the dietary intake pattern, along with anthropometric measurements (height, weight), cultural preferences, beliefs, lifestyle and customary intake, a standard diabetic diet sheet was given to each individual. The dietary recommendations were adapted to the specific needs of the individual based on nutrition assessment, desired treatment outcomes, and modification of usual food intake. All subjects were advised to strictly adhere to a two meal, two snack (one meal and one snack before onset of fasting and one meal and one snack after breaking of fast) pattern during the fasting period of Ramadan. A typical day's meal and snacks aimed at providing 1500 to 2000 calories with 65-70% calories from carbohydrate, 15- 20% from protein and 10--15% from fat.[19] A prototype of dietary recommendation is listed in Table 2.
Table 2.
Prototype dietary recommendation based on body mass index
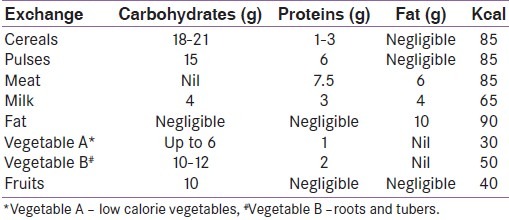
Food exchange system
The food exchange system for planning diabetic diets for the current study was based on the concept of food equivalents. Seven food groups listed in the food exchange system (cereals, pulses, meat, milk, vegetables, fruits, and fat) were included in the diet prescribed to the participants.. The description of food exchanges according to their general composition and characteristics are included in Table 3.
Table 3.
Food exchanges recommended during fasting
Diet counseling
Dietary counseling was given individually and food portions were instructed using standardized cups and spoons. A-days dietary pattern with traditional foods was displayed in portions to ease understanding of dietary recommendations. In this visual method, a plate served as a pie chart to show the proportions of the plate that have to be covered by various food groups.
Biochemical methods
Fasting and 2-hours post prandial blood glucose were measured using Accucheck® active glucometer. Overall glycemic control during 30 days of fasting was assessed using serum fructosamaine, measured by Boehringer Mannheim automated analysis (BM/Hitachi System 912). The intra- and interassay coefficients of variation was 0.53% and 5.21% respectively. Values for optimal glycemic control was based on comparison of serum fructosamaine to HbA1C values performed on non-diabetic controls recruited in the original study. Glycemic control was classified as good, suboptimal and poor if the corresponding serum fructosamine were 185.285 uM/l, 286-485 uM/L and >=486uM/l respectively.
Statistical analysis
The baseline data were presented as Mean ± Standard Deviation. Carbohydrate, protein, and fat intake were expressed as percent contribution to daily energy intake. Repeated measure ANOVA was used to compare the difference in proportions in calorie consumption during different time points of fasting. A “P value” of < 0.05 was considered statistically significant. The statistical analysis was done with the SPSS Version 11, (USA).
RESULTS
The current study examined dietary patterns and adherence to diet prescribed during fasting days of Ramadan in 72 Muslim subjects with T2DM. The descriptive characteristics of the study participants are shown in Table 1. The participants were middle aged (45 ± 9 years) with a shorter duration of diabetes (8.0 ± 2 years) and mean BMI was 29.8 ± 5 kg/m2. All subjects included in the study were on anti-diabetic medications either in the form of monotherapy (n = 12), or combination therapy (n = 38).
The overall calorie consumption during Ramadan varied significantly prior to initiation of fasting, 15 days after initiation of fasting and end of the fasting period (p=0.001). The percentage of energy consumption from dietary carbohydrate prior to fasting (64.11 ± 6.73), during fasting (68.41 ± 4.41), and at the end of fasting (70.46 ± 5.45) remained almost unchanged with marginal statistical significance (p=0.041). Protein and fat consumption varied considerably during fasting (p=0.001 and p=0.0001). Analysis of individual components of diet consumption showed a substantial increase in dietary components during mid-Ramadan fasting [Table 4].
Table 4.
Dietary intake and glycemic control in patients compared from before and after during the fasting period of Ramadan
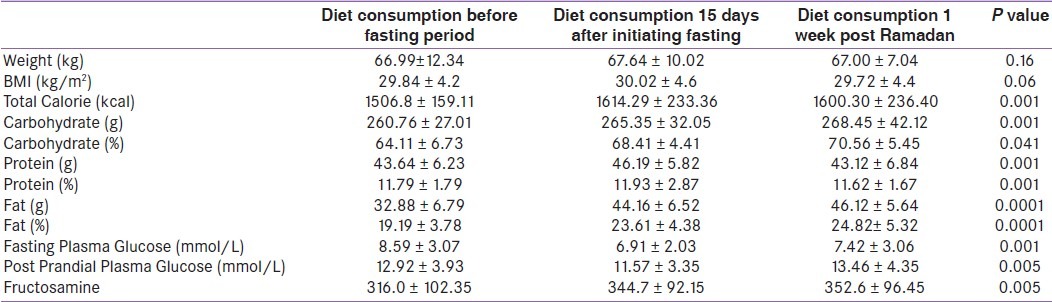
A significant reduction in fasting and post prandial glucose was observed during mid-Ramadan, but the glycemic patterns resumed to baseline values when subjects resumed their normal dietary pattern after Ramadan fasting. Overall glycemic control as assessed by serum fructosamine at the end of the fasting period was optimal (p=0.005).
DISCUSSION
Nearly one-fourth of the world's population constitutes Muslims. Over 50 countries across the globe have majority of Muslim population. The Islamic religion is the second largest community in India. The 2011 population census of India (http://censusindia.gov.in) report an approximate 13.4% (138 million) Muslims living in India clustered in minority communities, which is more than Islamic community in the Arab countries. The exact prevalence of T2DM in different religious communities in India are unknown. However, it is evident from clinical observations an health surveys that most of the Muslims in India practice religious fasting during the holy month of Ramadan. The major changes in life style pattern during Ramadan fasting are chrono-biological and behavioral.[20] Although there is considerable evidence on physiological alterations and diabetes management with oral hypoglycemic drugs or insulin, little emphasis is laid upon dietary management during fasting. In the current study we aimed to investigate the dietary patterns during the Ramadan fasting and also assess adherence to prescribed diets to optimize blood sugar control among South Indian Muslims who undertook 30 day fasting during Ramadan. undertook fasting in the holy month of Ramadan. Results from our study demonstrates that there is an overall increase in calorie consumption during Ramadan fasting despite sufficient dietary counseling in our participants. Although religious fasting permits intake of food only twice a day (before and after sunrise and sunset), there appears to be compensatory overeating in adults as observed by the increase in total calorie intake during fasting. There was a significant increase in the percentage carbohydrates, protein and fats consumed during fasting, most of the later are a part of the traditional foods that are specifically consumed during Ramadan in this population. A similar pattern of high calorie intake was reported previously among healthy Muslims. Contrary to our findings, a study among 22 diabetic Muslims from Malaysia have shown low calorie consumption during Ramadan fasting, however detailed dietary description was not reported among these individuals. The calorie consumption during the entire period of fasting was also not reported among these individuals. We identified a distinct dietary behavioral pattern during the fasting period among our particpants, with regard to type of food groups consumed with a mean increase in consumption of all components of diet during 30-day fasting. This specific pattern of high calorie food intake was independent of the socio-economic strata and educational status. It was evident from the patient-dietician interview that most patients perceived that intake of large quantities of food that yield sufficient energy could help them sustain fasting and prevent hypoglycemia. Khaled et al. observed an increase consumption of dietary fat (35.8%), especially saturated fats (43.3%) among Muslims during fasting periods similar to our observations (44.2%) during mid-Ramadan. Although this dietary practice of high calorie compensation was contrary to actual religious preaching (of non-compensatory eating), the main concern among participants was interruption of continuous 30-day fasting due to hypoglycemia.
Most dietary guidelines for diabetes management are targeted towards intake of specific macronutrients. In an Indian setting, many individuals find it difficult to make dietary changes based on such numerical criteria. Therefore, our recommendations were based on overall pattern of dietary intake focusing on appropriate food choices. We focused mainly on high-carbohydrate and high-fiber (HCHF) diet during the nonfasting hours, as it is noted that diets which were high in rich complex carbohydrates and dietary fiber, and relatively low in fat, benefited individuals with diabetes mellitus.[21] Despite repeititive counseling on dietary patterns and reinforcing prescribed diet according to patients choices and traditional practices, the compliance to prescribed diet was poor. These conclusions were not supported by questionnaire based assessments but, from overall assessment of the diet diary where the patient recorded foods consumed during fasting. We learn that although targeted counseling is implemented, it is difficult to break the traditional pattern of high-fat and high-protein diet during the period of Ramadan fasting.
Glycemic assessment by serum fructosamine at the end of the study was optimal (P = 0.005) among our participants. Several studies have reported no change in HbA1C or fructosamine in subjects who undertook fasting during Ramadan. It is important to note that the variation in diet pattern during fasting is crucial leading to hypo- and hyperglycemia.
Hypoglycemia is one of the major concerns both among patients and treating physicians who undertake short-term fasting due to religious practices. Hypoglycemia assessment ( based on self-reports) was not seen among our participants similar to previous observations in fasting diabetic patients treated with anti-diabetic drugs or insulin. However, a large epidemiological study demonstrated that the risk of severe hypoglycemia increased by 4.7 and 7.5 folds in subjects with type 1 and type 2 diabetes who undertook fasting during Ramadan. In another muticentric observational study, symptomatic hypoglycemia was observed in 20% of fating diabetic patients. We did not observe significant difference in weight or BMI change before, during or after fasting similar to observations by M’guil et al. among 120 diabetic subjects who practiced Ramadan fasting.
There are some limitations to this study. A power calculation to determine the sample size was not used due to the lack of prior similar studies evaluating the dietary habits during Ramadan. The 24-hour dietary recalls can mostly give an estimate of the average nutrient intake, and this possibly explains the difference in food intake when comparing the two dietary assessment methods. There is some element of bias in the recall of food intake as most subjects volunteered participation. However the present study gives us an insight into the dietary habits, food adherence patterns, and traditional beliefs in a unique group of Muslim subjects who undertook fasting during Ramadan.
CONCLUSIONS
The large proportion of Muslim subjects who undertake fasting during Ramadan represents a challenge to the treating physicians. The present study is one of the first studies that have attempted to present the overall picture of the food pattern in fasting Muslim subjects during Ramadan, and our prototype diet based on regional food practices and a culturally acceptable diet pattern is a recommendation for patients with diabetes who fast during Ramadan in India. There is a overwhelming need for additional studies that could provide assessment and dietary recommendations that are ethnic/culture specific and form mainstay of diabetes management in all religious groups that practice short-term fasting.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Azizi F, Siahkolah B. Ramadan fasting and diabetes mellitus. Int J Ramadan Fast Res. 1998;2:6–10. [Google Scholar]
- 2.Uysal AR, Erdogan MF, Kamel N, Erdoğan G. Clinical and metabolic effects of fasting in 41 type 2 diabetic patients during Ramadan. Diabetes Care. 1998;20:2033–4. doi: 10.2337/diacare.21.11.2033. [DOI] [PubMed] [Google Scholar]
- 3.Herber D. Endocrine response to starvation, malnutrition and illness. In: De Groot L, editor. Endocrinology. 3rd ed. Vol. 3. Philadelphia: Saunders; 1995. pp. 2663–78. [Google Scholar]
- 4.Cahill GF., Jr Starvation in men. N Engl J Med. 1970;282:668–75. doi: 10.1056/NEJM197003192821209. [DOI] [PubMed] [Google Scholar]
- 5.Salti I, Benard E, Detoumay B, Bianchi-Biscay M, Le Brigand C, Voinet C, et al. EPIDIAR Study Group. A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: Results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27:2306–7. doi: 10.2337/diacare.27.10.2306. [DOI] [PubMed] [Google Scholar]
- 6.Rashed H. The fast of Ramadan: No problem for the well: The sick should avoid fasting. Br Med J. 1992;304:521–2. [Google Scholar]
- 7.Laajam MA. Ramadan fasting and non insulin-dependent diabetes: Effect of metabolic control. East Afr Med J. 1990;67:732–6. [PubMed] [Google Scholar]
- 8.Connor H, Annan F, Bunn E, Frost G, McGough N, Sarwar T, Thomas B. Nutrition Subcommittee of the Diabetes Care Advisory Committee of Diabetes UK. The implementation of nutritional advice for peo ple with diabetes. Diabet Med. 2003 Oct;20(10):786–807. doi: 10.1046/j.1464-5491.2003.01104.x. [DOI] [PubMed] [Google Scholar]
- 9.Winocour PH, Mearing C, Ainsworth A, Williams DR. Association of British Clinical Diabetologists. Survey of specialist diabetes care services in the UK. 4. Dietetic services and nutritional issues. Diabet Med. 2000;19:39–43. doi: 10.1046/j.1464-5491.19.s4.7.x. [DOI] [PubMed] [Google Scholar]
- 10.Delahanty L, Simkins S, Camelon K. Expanded role of a dietician in the Diabetes control and complications trial: Implications for clinical practice. J Am Diet Assoc. 1993;93:758–76. doi: 10.1016/0002-8223(93)91748-f. [DOI] [PubMed] [Google Scholar]
- 11.Mohan V, Saroja R, Sudha V. Experience with dietary management in diabetes mellitus in south Indians. In: Malini S, Siddhu A, editors. Nutrition goals for Asia – Vision 2020. Proceedings IX Asian Congress of Nutrition. New Delhi: Nutrition Foundation of India; 2003. pp. 528–32. [Google Scholar]
- 12.Mafauzy M, Mohammed WB, Anum MY, Zulkifli A, Ruhani AH. A study of fasting diabetic patients during the month of Ramadan. Med J Malaysia. 1990;45:14–7. [PubMed] [Google Scholar]
- 13.Sudha V, Radhika G, Mohan V. Current dietary trends in the management of diabetes. Indian J Med Res. 2004;120:4–8. [PubMed] [Google Scholar]
- 14.Katibi IA, Akande AA, Bojuwoye BJ, Okesina AB. Blood sugar control among fasting Muslim with type 2 diabetes in Ilorin. Niger J Med. 2001;10:132–4. [PubMed] [Google Scholar]
- 15.Vasan SK, Thomas N, Bharani G, Ameen M, Abraham S, Job V, et al. A double blind, randomized, milticenter study evaluating the efficts of Pioglitazone in fasting Muslim subjects during Ramadan. Int J Diabetes Dev Ctries. 2006;26:70–6. [Google Scholar]
- 16.Chen Y, Ahsan H, Parvez F, Howe GR. Validity of food frequency questionnaire for a large prospective study in Bangladesh. Br J Nutr. 2004;92:851–9. doi: 10.1079/bjn20041277. [DOI] [PubMed] [Google Scholar]
- 17.Borrud LG, McPherson RS, Nichaman MZ, Pillow PC, Newell GR. Development of food frequency instrument: Ethnic differences in food sources. Nutr Cancer. 1989;12:201–11. doi: 10.1080/01635588909514020. [DOI] [PubMed] [Google Scholar]
- 18.Pandey D, Bhatia V, Boddula R, Singh HK, Bhatia E. Validation and reproducibility of a food frequency questionnaire to assess energy and fat intake in affluent north Indians. Natl Med J India. 2005;18:230–5. [PubMed] [Google Scholar]
- 19.Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, et al. Nutrition Principles and recommendations in Diabetes. Diabetes Care. 2004;27:S36–46. doi: 10.2337/diacare.27.2007.s36. [DOI] [PubMed] [Google Scholar]
- 20.Roky R, Houlti I, Moussamih S, Qotbi S, Aadil N. Physiological and chronobiological changes during Ramadan intermittent fasting. Ann Nutr Metab. 2004;48:296–303. doi: 10.1159/000081076. [DOI] [PubMed] [Google Scholar]
- 21.Viswanathan M, Ramachandran A, Mohan V, Snehalatha C. High carbohydrate diet, high fibre diet in diabetes. J Diab Assoc India. 1981;21:90–6. [Google Scholar]


