Abstract
Background:
Diabetes Mellitus is the commonest endocrine-metabolic disorder in Nigeria similar to the experience in other parts of the world. The aim was to assess the clinical and laboratory profile, and evaluate the quality of care of Nigerian diabetics with a view to planning improved diabetes care.
Materials and Methods:
In a multicenter study across seven tertiary health centers in Nigeria, the clinical and laboratory parameters of diabetic out-patients were evaluated. Clinical parameters studied include type of diabetes, anthropometry, and blood pressure (BP) status, chronic complications of diabetes, and treatment types. Laboratory data assessed included fasting plasma glucose (FPG), 2-h post-prandial (2-HrPP) glucose, glycated hemoglobin (HbA1c), urinalysis, serum lipids, electrolytes, urea, and creatinine.
Results:
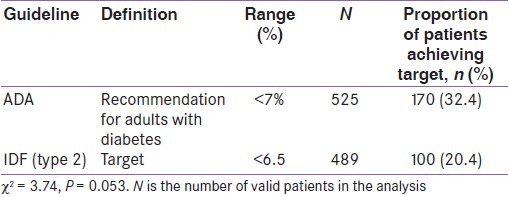
A total of 531 patients, 209 (39.4%) males and 322 (60.6%) females enrolled. The mean age of the patients was 57.1 ± 12.3 years with the mean duration of diabetes of 8.8 ± 6.6 years. Majority (95.4%) had type 2 diabetes mellitus (DM) compared to type 1 DM (4.6%), with P < 0.001. The mean FPG, 2-HrPP glucose, and HbA1c were 8.1 ± 3.9 mmol/L, 10.6 ± 4.6 mmol/L, and 8.3 ± 2.2%, respectively. Only 170 (32.4%) and 100 (20.4%) patients achieved the ADA and IDF glycemic targets, respectively. Most patients (72.8%) did not practice self-monitoring of blood glucose. Hypertension was found in 322 (60.9%), with mean systolic BP 142.0 ± 23.7 mmHg, and mean diastolic BP 80.7 ± 12.7 mmHg. Diabetic complications found were peripheral neuropathy (59.2%), retinopathy (35.5%), cataracts (25.2%), cerebrovascular disease (4.7%), diabetic foot ulcers (16.0%), and nephropathy (3.2%).
Conclusion:
Most Nigerian diabetics have suboptimal glycemic control, are hypertensives, and have chronic complications of DM. Improved quality of care and treatment to target is recommended to reduce diabetes-related morbidity and mortality.
Keywords: Chronic complications, diabetes mellitus, glycemic control, quality of care
INTRODUCTION
Diabetes mellitus is a chronic disease with an increasing prevalence worldwide.[1] It constitutes a significant health and socioeconomic burden for patients and the health care systems. According to the WHO, there were 150 million diabetic patients worldwide by the year 2000, with a projection of 221 million people in 2010 and 300 million in 2025.[1] The International Diabetes Federation (IDF) estimates that over 5 million people suffer from the disease in Africa and the number is expected to increase to 15 million by 2025.[1] The prevalence in Nigeria varies from 0.65 in rural Mangu village to 11.0% in urban Lagos.[2] It is well established that good glycemic control and control of other cardiovascular risks in diabetic patients lead to reduced morbidity and mortality.[3] With the incidence of diabetes in the African population on the rise, the incidence of late diabetic complications is also expected to increase correspondingly.[4,5] This will eventually pose major health care and economic problems. The WHO suggests that Nigeria has the greatest number of people living with diabetes in Africa, with an estimated burden of about 1.7 million which will increase to 4.8 million by 2030. The economic burden of diabetes is enormous in terms of the direct cost of intensive monitoring and control of blood glucose and managing cardiovascular, renal, and neurological consequences.[1,4,5]
Several studies, e.g., the Diabetes Complications and Control Trial (DCCT), the UKPDS and their follow-up studies, found that the adequate management of diabetes improves the outcome in terms of morbidity, mortality, and quality of life.[6–8]
For this reason, it is necessary to follow recommended international and national guidelines in managing diabetic patients.[9,10] These include glycemic targets, systolic and diastolic blood pressure targets, body mass index (BMI) and other anthropometric indices, lipid levels, self-management, and behavioral targets. It has also been documented that diabetes education is critical for ensuring the attainment of targets in patients under treatment.
Other countries have studied the status of diabetes control in their populations.[11,12] Some Nigerian studies covered only sections of the population.[13,14]
Nationwide data are desirable for the Nigerian diabetic population and are presently lacking. Being the first of its kind in Nigeria, the study aims to determine the status of diabetes care (quality of DM control, management practices, and presence of late complications of DM) in tertiary health centers in Nigeria. It is hoped that data obtained will be an invaluable resource for diabetes advocacy, program evaluation, planning resource allocation, and improving diabetes services across Nigeria with an eventual improvement in diabetes outcome and a reduction in the disease incidence.
MATERIALS AND METHODS
Study setting and patient population
Seven tertiary health institutions covering the six geopolitical regions of Nigeria constituted the study sites and these included AKTH, Kano; UNTH, Enugu; UPTH, Port Harcourt; LUTH, Lagos; UCH, Ibadan; LASUTH, Lagos; and National Hospital, Abuja.
The study population included consenting adult diabetic patients attending the diabetes clinics of the above-named institutions for a minimum of 12 months. The study was approved by the health research ethics committees of all the participating institutions.
Patient recruitment
Every third consenting patient attending the diabetes clinic was recruited. The study lasted from March to August 2008. Basic patient data such as date of birth, gender, ethnicity, duration of treatment at the clinic, duration of diabetes, type of diabetes, and risk factors for cardiovascular disease (e.g., tobacco use, alcohol consumption and physical inactivity) were documented. Treatment history was taken and drugs for hypertension and dyslipidemia noted.
Clinical measurements such as weight, height, waist circumference, hip circumference, and blood pressure were determined using standard techniques.
Other data collected included the following:
Eye examination – the frequency of eye examinations in the last 1 year, presence of legal blindness, cataract, background retinopathy, advanced diabetic eye disease, and history of photocoagulation were documented.
Lower limb examination – the frequency of feet examinations in the last 1 year, presence of leg amputation, healed ulcer(s), acute ulcer/gangrene, absent foot pulse(s), and bypass/angioplasty were recorded.
Other diabetes complications such as cerebral stroke, signs of neuropathy, myocardial infarction/cardiac bypass/angioplasty, and end-stage renal failure requiring dialysis or transplant were determined.
History of current diabetes management including use of oral anti-diabetics, insulin and other medications (anti-obesity and antiplatelet agents) was documented.
Patient self-monitoring of glycemia (blood and urine glucose).
Diabetes education received by the patients in the past year.
Laboratory tests
On-the-spot assessment of HbA1c was performed for each patient. HbA1c assessment was performed using the HbA1c kit (in2it™ system from Bio-Rad®). The in2it™ HbA1c test device utilizes the finger-stick blood sample in a test cartridge using the boronate affinity method with results delivered in 10 min. Other laboratory data obtained from the patients’ clinic records in the last 1 year included fasting plasma glucose, fasting serum lipids, serum creatinine, microalbuminuria, and proteinuria. The frequency of each test carried out in the last 1 year was also documented.
Statistical analysis
The data were recorded in forms provided for each patient. All data from the centers were centrally collated for analysis. All data were entered into a database (Microsoft® Access) by double data entry. Data analyses were performed using the Statistical Package for Social Sciences (SPSS), version 16.0.
The response rate to all the variables assessed was presented as percentage. Only descriptive statistical analysis was performed. A P-value < 0.5 was considered significant.
RESULTS
Demographic characteristics
A total of 531 patients, 212 (39.5%) males and 319 (60.5%) females) were evaluated. Complete data for analysis was available for only 509 patients. All the patients (100%) in the study were of African descent. The mean age of the study population was 57.1 ± 12.3 years with a mean age at diagnosis of diabetes mellitus (DM) of 48.3 12.6 years and mean duration of DM 8.8 ± 6.6 years. Majority of the patients studied had type 2 DM (95.4%) compared to type 1 DM (4.6%).
Anthropometric indices
The waist circumference of the patients was categorized by gender to assess the risk of comorbidity based on the International Diabetes Federation (IDF) reference values for males and females.[1] The risk of comorbidity was higher in women with 91.2% having a waist circumference of > 80 cm. Among men, 43.3% had a waist circumference of > 94 cm (χ2 = 52.10, P = 0.0001, relative risk [RR] = 2.12, 95% confidence interval [CI] 1.67-2.67). The mean BMI of the study population was 27.2 ± 5.4 kg/m2.
Modifiable risk factors
Majority of the patients neither smoked cigarettes (92.8%) nor consumed alcohol (81.5%). Adherence to dietary measures was documented in 67% of patients. Only 6.9% of the patients did not follow a diet plan. However, adherence to exercise prescription was poor with only 35.9% of patients claiming to exercise “regularly” and 26.7% not exercising at all.
Quality of glycemic control
Glycosylated hemoglobin (HbA1c)
The number of glycosylated hemoglobin ( HbA1c) measurements per year was available for 49.5%.The mean value suggests that HbA1c was not regularly assessed in diabetes patients, ranging from none in a year to six times in a year. The mean HbA1c value assessed during this study was 8.3% ± 2.2%.
Based on the ADA and IDF guidelines for glycemic control in type 2 DM, the proportion of Nigerian DM patients achieving target HbA1c is shown in Table 1.
Table 1.
HbA1c levels stratified by different guidelines
Plasma glucose
While fasting plasma glucose (FPG) was measured in most of the patients (98.5%) with a mean FPG value of 8.1 ± 3.9 mmol/L, post-prandial glucose (PPG) was measured in only 58.4% of the patients with a mean PPG value of 10.6 ± 4.6 mmol/L. The proportion of Nigerian diabetics achieving target FPG based on the ADA guidelines (FPG ≤7.2 mmol/L) was significantly higher, 52.6%, when compared to those achieving targets using the IDF (<6 mmol/L) guidelines for type 2 DM, 33.9% (χ2 = 7.34, P = 0.007).
Diabetes education and glycemic control
In the preceding 12 months, 26.9% of the patients received more than five sessions of diabetes education, 14.8% received five sessions of education and 17% received four sessions of education. About 10% received two or three sessions of diabetes education and 10.9% had not received any form of diabetes education.
Good glycemic control (HbA1c <6.5%) appeared to be achieved in more patients who received more education sessions (62% received four to more than five sessions of education versus 10% who received no diabetes education at all). This trend was similarly observed in patients with moderate glycemic control (HbA1c ≥ 6.5%–7.5%) or poor glycemic control (HbA1c ≥ 7.5%).
Cardiovascular risk assessment
Fasting plasma lipids
Fasting plasma lipid levels were assessed in 48% of the patients with mean total cholesterol level being 4.9 ± 1.1 mmol/L, HDL-cholesterol 1.2 ± 0.6 mmol/L, and triglycerides 1.2 ± 0.7 mmol/L. Low HDL cholesterol and hypertriglyceridemia were the common lipid abnormalities found. The proportion of patients achieving the ADA HDL-cholesterol targets was 21.1% in males and 13.9% in females. Only 23.7% of the patients met the IDF HDL-cholesterol target of >1.0 mmol/L. Only 39.3% and 45.6% of the patients achieved the ADA and IDF triglyceride targets, respectively.
Only 12.6% (64) of the patients were on treatment (statins) for dyslipidemia.
HDL-cholesterol
Only 12.6% patients were treated for hyperlipidemia, and of these 33.3% males and 24.2% females achieved the ADA HDL-cholesterol target of >1.0 mmol/L (>40 mg/dL) for males and >50 mg/dL for females, respectively.
When assessed using the IDF (type 2) guidelines, 38.5% of treated patients achieved target HDL-cholesterol.
Triglycerides
The ADA target triglyceride level of <1.7 mmol/L (<150 mg/dL) was achieved by 63.6% of treated patients. Only 11.5% of patients with elevated triglycerides did not receive treatment. When the IDF (type 2) recommended target triglyceride level of 2.3 mmol/L was applied, 92.3% of treated patients achieved the target.
Blood pressure
The mean systolic and diastolic blood pressures for all the patients were 142 ± 23.7 and 80.7 ± 12.7 mmHg, respectively.
Only 17% and 14.2% of the patients achieved the ADA and IDF blood pressure targets of <130/80 mmHg.
Treatment of hypertension
Systemic arterial hypertension was found in 322 (60.9%) of the patients and majority (81.9%) of these were already receiving treatment for high blood pressure. Most patients were treated with combinations of ACE inhibitors (66.6%), Ca2+ antagonists (33%), or diuretics (27.7%). A small percentage were treated with angiotensin-II receptor blockers (3.1%), β-blockers (2.7%), or α-blockers (1.0%) compared to 9.9% who were treated with “other” types of drugs for hypertension. Of the patients receiving treatment for hypertension, only 11% had good BP control.
Chronic complications of diabetes
Renal function
The estimation of serum creatinine was done in only 50.6% of patients while urine testing for protein was performed in 65.8%. A few patients (3.2%) had serum creatinine >2 mg/dL. Only 8.9% had proteinuria <30 mg/dL and 4.8% had 30 mg/dL of proteins in the urine. Protein levels >100 mg/dL were found in few patients (2.5%). Microalbuminuria was reported in 3.2% of patients.
Eyes
About half (49.4%) of patients had eye examination within the last 1 year. Eye complications observed were background retinopathy in 35.5%, cataracts in 25.2%, advanced eye disease in 5.9%, and legal blindness in 1.3%. Only 0.2% had laser photocoagulation [Table 2].
Table 2.
Diabetic complications by HbA1c categories
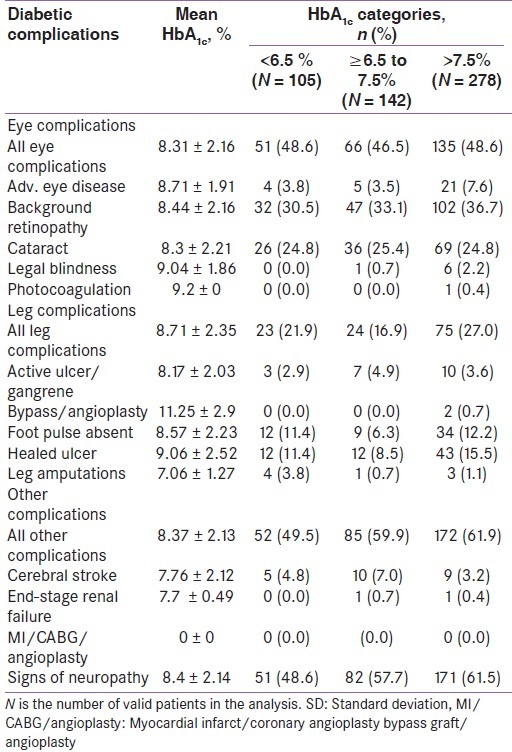
Lower extremities
Over half (57.7%) of the patients had feet examination within the last 1 year. Of these, 13.2% had healed ulcers, 10.7% absent foot pulses, 3.8% active ulcers/gangrene, 1.5% leg amputations, and 0.4% had angioplasty [Table 2].
Other complications of diabetes
The other chronic complications of diabetes found in the study were peripheral neuropathy, 59.2%, stroke (CVD), 4.7%, and end-stage kidney disease, 0.4%. There were no patients with a past history of myocardial infarction/coronary artery by-pass.
Renal complications and blood pressure categories
More patients who had uncontrolled systolic blood pressure had microalbuminuria (4.6% vs. 1.1%). The same result was observed in patients who have uncontrolled diastolic blood pressure (5.4% vs. 1.8%).
Current diabetes management
Most (89.8%) of the patients with type 2 diabetes were on oral antidiabetic (OAD) medications. The most commonly prescribed OADs were biguanides (84.8%) and sulphonylureas (73.2%). Thiazolidinediones were used in only 12.3% of cases. Only 20.8% of the patients were using insulin representing one in five patients with diabetes. Nearly all (99%) the patients were using human insulin. The mean duration of treatment with insulin was 4.0 ± 5.2 years at a mean total daily dose of 38 ± 15.2 units/day (0.58 0.25 units/kg/day). Most patients administered insulin twice a day (89.71%) using disposable syringes and needles (83%) while some patients (17%) use the pen devices.
Combination therapy
OAD therapy was the most common (80.6%) type of therapy in this study population compared to combination therapy of OADs and insulin (9.1%) or insulin monotherapy (9.9%).
Among patients treated with OADs, the majority used two types of OADs (59.3%) and 12% used a single OAD compared with 9.1% who were treated with three OAD classes. Combination therapy of an OAD with insulin is less common: 5.6% were treated with a single OAD and insulin, 3.1% with two OADs and insulin, and 0.4% with three OADs and insulin.
Use of anti-obesity and antiplatelet agents
Only a negligible proportion (<1%) of patients were on anti-obesity drugs. However, two-thirds of the patients (65%) were treated with antiplatelets in the form of low-dose aspirin (75 mg per day).
Glucose self-monitoring
Self-monitoring of home blood glucose using glucose meters was documented in only 27.2% of the patients. Only 2.3% of the patients were performing home urine glucose measurements. Patients measured blood glucose approximately seven times/month (mean 7 ± 9.9 times/month) compared to about twice/month (mean 1.6 ± 5.5 times/month) for urine glucose.
DISCUSSION
This study covered all the geopolitical zones of Nigeria unlike previous ones like the African-American Diabetes Study[13,14] which covered only a section of the country.
Clinical characteristics
The female preponderance (60.5%) observed is striking and does not reflect the pattern observed in studies involving diabetic patients outside the tertiary health centers in Nigeria where the male:female ratio is close to 1:1.[13–15] This figure may be a reflection of the pattern of health care financing in the country. Health care is largely financed by the individual patients (out-of-pocket). Women are more likely to be supported by relations and loved ones with financial assistance toward hospital visits than male patients. Some studies have shown that indigent patients who cannot afford their medications shop around with traditional medicine practitioners, drug sellers, or even avoid medical treatment thereby worsening their conditions.[16] In a qualitative study of diabetic patients in Ghana, Aktins[16] revealed that diabetic patients considered biomedical management as ideal. However, due to the nonaffordability of diabetic medicines and care, they were driven to cure seeking with ethnomedical systems of care which resulted in diabetic complications.
A well-designed population-based study will be able to provide the true sex distribution of diabetics in the population as well as reasons for attending tertiary centers.
The mean age of 57.1 years found in this study is low compared to reports from developed countries where most diabetics were over 64 years of age, but similar to observations from other Sub-Saharan African countries where an age range of 45–64 years was reported.[4,17] The mean diabetes duration of 8.8 years may suggest that most Nigerian diabetics do not survive long enough which is probably a reflection of disease burden and quality of care. The lower mean age and mean duration of diabetes compared with patients in the developed world may be a reflection of the lower life expectancy of Nigerians compared with the developed world, as well as the reduced survival of Nigerian diabetic patients.
The mean age at the onset of type 2 diabetes in this study is lower than the mean age of onset in patients in the developed world.[1,17]
Anthropometric indices
Central obesity, a strong risk factor for cardiovascular adverse event, was common, using cut-off values of 80 cm for females and 94 cm for male waist circumference.[9,10] Other studies have questioned the appropriateness of these figures for non-Caucasian groups.[18] There is a need to confirm that these waist circumference values confer additional cardiovascular risks on Nigerian diabetic patients through longitudinal studies.
Glycemic and other targets
The majority of patients (nearly 70%) did not achieve recommended targets for glycemic control and control of coexisting cardiovascular risk factors. This contrasted with findings in a cross-sectional study assessing quality care for diabetes among 40 medical groups in the USA.[19–21] Leif et al.[12] found the Optimal Diabetes Care Composite of HbA1c 8% to be 69.4%, LDL cholesterol <130 mg/dL to be 68.2%, BP <130/85 mmHg to be 48.5%, regular aspirin use to be 68.1%, and no tobacco use to be 72.1%. The result of the process measures of HbA1c test twice yearly was found to be 91.9%, LDL test yearly 90.4%, BP measurement yearly 94.0%, yearly eye exam 65.3% and microalbuminuria test yearly 67.6%.[12] In a study by Saadine et al.[20] among Americans only 20% had poor glycemic control.
In this study, the mean HbA1C as well as mean FPG and 2HPP plasma glucose levels did not meet target goals in 47.2% of patients studied.[21] A previous study from Nigeria has also documented poor glycemic control among diabetic patients.[14]
The reasons for poor glycemic control among Nigerian diabetic patients are multi-factorial. Financial constraint is a key factor as most patients have to pay out-of-pocket for their drugs and for blood glucose tests, and at a price which has been found to be much higher than the cost of these drugs in other parts of the world.[21] In Nigeria, a substantial portion of health care costs (74.5%) is borne by the patient, as the government provided only 25.5% of health care expenditure in 2003 (according to a WHO report).[22] The WHO report estimates that 90.2% of Nigerians live below the poverty level of $2 per day. Thus, accessing health care is a challenge for people living with diabetes in Nigeria.[23] This difficulty is evident by reports showing a high prevalence of complications due to diabetes.[24,25]
Patients’ nonadherence to therapy is an important factor. Culturally, Nigerians are averse to accepting that a disease is incurable and requires life-long management. They continue searching for permanent cure, a process that often results in poor control. Patient education is the key for counteracting this menace. A third factor is the prescription pattern of health care providers. The prescription of insulin is uncommon for type 2 diabetic patients. Only 20% of the patients had insulin prescribed for them. Health care providers are likely to benefit from continuing education on diabetes management to improve evidence-based practice among them.
Lipids
Lipid profile was performed in only half of the patients studied, and only 21% of males and 13.9% of females achieved the ADA target HDL-C recommendations.[26] Only a third achieved the triglyceride target. In contrast, a study of Americans with diabetes reported hypercholesterolemia in 43% of patients with good glycemic control and hypertriglyceridemia in 17%.[27] However, only 12.6% of our patients were receiving a prescription for hyperlipidemia. Despite this finding, the evidence of macroangiopathy was lacking in the Nigerian diabetics for reasons not clear. It is possible that the low prevalence of cigarette smokers is protective.
Blood pressure
An ADA target BP control of 130/80 mmHg was recorded in 17.2% persons with hypertension in this study, a figure far less compared to 36.5% and 38.2% reported in other similar studies.[28,29]
Modifiable risk factors
It is not certain whether the very high proportion of nonsmokers observed in this study is partly responsible for the low cases of severe atherosclerosis recorded. Other studies report a large percentage of cigarette smokers.[12,20]
Adherence to dietary recommendations was practiced by 67% of patients who claimed to be on a “regular” diet. However, adherence to exercise recommendations was poor with only 35.9% of patients claiming to exercise “regularly” and 26.7% not exercising at all. This is better than the figures obtained from studies of diabetic patients from other populations.[11,12] The seemingly high percentage of patients observing dietary measures in this study did not translate into good quality of glycemic control.
Complications of diabetes
The prevalence of different microvascular complications of diabetes is similar to figures from other populations in Africa and the developed world.[8,29] However, interventions for coronary artery disease such as coronary artery bypass graft (CABG) or coronary balloon angioplasty did not feature in this study population. This is most probably a reflection of the nonavailability of these interventions in most of the tertiary centers in Nigeria presently.
CONCLUSION
Most Nigerian diabetic patients have suboptimal glycemic control, are hypertensives not meeting BP targets, and have chronic complications of DM. Improved quality of care and treatment are recommended to reduce diabetes-related morbidity and mortality.
Positive behavioral modifications (large proportion of nonsmokers and nontobacco users) observed need to be strengthened.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.International Diabetes Federation. 3rd ed 2006. The improved Diabetes Atlas. [Google Scholar]
- 2.Akinkugbe OO, editor. Final Report of National Survey on Non Communicable Diseases in Nigeria Series 1. Federal Ministry of Health and Social Services, Lagos. 1997 [Google Scholar]
- 3.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachim JM, Orchard TJ, et al. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research group: Intensive Diabetes treatment and Cardiovascular Disease in patients with Type 1 diabetes. N Engl J Med. 2005;353:2643–53. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wild S, Roglic C, Green A, Sicrete R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 5.Zimmet P. The burden of Type 2 Diabetes: Are we doing enough? Diabetes Metab. 2003;29:659–81. doi: 10.1016/S1262-3636(03)72783-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diabetes Control and Complications Trial Research Group. The effect of Intensive treatment of Diabetes on the development of and Progression of long - term complications in Insulin Dependent Diabetes Mellitus. N Engl J Med. 1993;329:977–85. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 7.United Kingdom Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34) Lancet. 1998;352:854–65. [Published erratum appears in Lancet 1998;352:1558] [PubMed] [Google Scholar]
- 8.Schram MT, Chaturvedi N, Schalkwijk C, Giorgino F, Ebeling P, Fuller JH, et al. Vascular risk factors and markers of endothelial function as determinants of inflammatory markers in type 1 diabetes. The EURODIAB Prospective Complications Study. Diabetes Care. 2003;26:2165–73. doi: 10.2337/diacare.26.7.2165. [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association. Standards of medical care in diabetes – 2008. Diabetes Care. 2008;31(Suppl 1):S12–54. doi: 10.2337/dc08-S012. [DOI] [PubMed] [Google Scholar]
- 10.IDF Clinical Guidelines Task Force. Global guideline for type 2 diabetes: Recommendations for standard, comprehensive, and minimal care. Diabetic Med. 2006;23:579–93. doi: 10.1111/j.1464-5491.2006.01918.x. [DOI] [PubMed] [Google Scholar]
- 11.Chuang LM, Tsai ST, Huang BY, Tai TY on behalf of the Diabcare-Asia 1998 Study Group. The status of diabetes control in Asia - a cross-sectional survey of 24 317 patients with diabetes mellitus in 1998. Diabetic Med. 2002;19:978–85. doi: 10.1046/j.1464-5491.2002.00833.x. [DOI] [PubMed] [Google Scholar]
- 12.Leif IS, Stephen EA, Gregory LP, Sarah HS, Sarah CS. Practice systems are associated with high-quality care for diabetes. Am J Manag Care. 2008;14:85–92. [PubMed] [Google Scholar]
- 13.Okoro EO, Adejumo AO, Oyejola BA. Diabetic care in Nigeria: Report of a self-audit. J Diabet Complications. 2002;16:159–64. doi: 10.1016/s1056-8727(01)00145-3. [DOI] [PubMed] [Google Scholar]
- 14.Rotimi CN, Chen G, Oli J, Ofoegbu E, Okafor G, Acheampong J, et al. A Genome - wide search for Type 2 diabetes susceptibility genes in West Africans. Diabetes. 2004;53:838–41. doi: 10.2337/diabetes.53.3.838. [DOI] [PubMed] [Google Scholar]
- 15.Rotimi CN, Chen G, Oli J, Ofoegbu E, Okafor G, Acheampong J, et al. Calpain-10 Gene Polymorphisms and Type 2 Diabetes in West Africans: The Africa America Diabetes Mellitus (AADM) Stud. Ann Epidemiol. 2005;15:153–9. doi: 10.1016/j.annepidem.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 16.Atkins AG. Healer Shopping in Africa: New Evidence from Rural Urban Qualitative Study of Ghanaian Diabetes Experience. BMJ. 2005;331:737–44. doi: 10.1136/bmj.331.7519.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McMichael AJ, Beaglehole R. The Changing Global Concept of Public Health. Lancet. 2000;356:495–9. doi: 10.1016/s0140-6736(00)02564-2. [DOI] [PubMed] [Google Scholar]
- 18.Poirier P. Adiposity and cardiovascular disease: Are we using the right definition of obesity? Eur Heart J. 2007;28:2047–8. doi: 10.1093/eurheartj/ehm321. [DOI] [PubMed] [Google Scholar]
- 19.Jifeng M. Diabetes Care Quality Indicators. The Medicare Quality Improvement Organization for Florida. 2006 [Google Scholar]
- 20.Saadine JB, Cadwell B, Cregg FW, Engelgau MM, Vinicor F, Imperatore G, et al. Improvement in Diabetes Process of Care and Intermediate outcomes: United States, 1988-2002. Ann Intern Med. 2006;144:465–74. doi: 10.7326/0003-4819-144-7-200604040-00005. [DOI] [PubMed] [Google Scholar]
- 21.The diabetes declaration and strategy for Africa: A call to action and plan of action to prevent and control diabetes and related chronic disease. Summary document. 2006 Nov [Google Scholar]
- 22.Geneva, Switzerland: World Health Organization; 2004. [Last accessed on 2008 Oct 31]. WHO 2004 Diabetes Action Now Booklet. Available from: http://www: who.int/diabetes/ booklet . [Google Scholar]
- 23.Ofoegbu EN. Cardiac Autonomic Neuropathy in Nigerian Type 2 Diabetes Mellitus Patients. Glob J Med Sci. 2005;4:52–8. [Google Scholar]
- 24.Richard WG, Paul AP, James BM, Daniel ES. Trends in Complexity of Diabetes Care in the United States from 1991 to 2000. Arch Intern Med. 2004;164:1134–9. doi: 10.1001/archinte.164.10.1134. [DOI] [PubMed] [Google Scholar]
- 25.American Diabetes Association. Management of Dyslipidaemia in Adults with Diabetes.(Position Statement) Diabetes Care. 2002;25(Suppl 1):S574–7. [Google Scholar]
- 26.Loh KC, Thai AC, Lui KF, Ng NY. High Prevalence of Dyslipidaemia Despite Adequate Glycaemic Control in Patients with Diabetes. Ann Acad Med Singapore. 1996;25:228–32. [PubMed] [Google Scholar]
- 27.Gossain VV, Rosenman KD, Gardiner JC, Thawani HT, Tang X. Evaluation of Control of Diabetes Mellitus in a Subspecialty Clinic. Endocr Pract. 2010;16:178–86. doi: 10.4158/EP09202.OR. [DOI] [PubMed] [Google Scholar]
- 28.Reinerhr T, de Sousa G, Andler W. Hyperthyrotropinemia in obese children is reversible after weight loss and is not related to lipids. J Clin Endocrinol Metab. 2006;91:3088–91. doi: 10.1210/jc.2006-0095. [DOI] [PubMed] [Google Scholar]
- 29.Alebiosu BO. Clinical Diabetic Nephropathy in a Tropical African Population. West Afr J Med. 2007;22:152–5. doi: 10.4314/wajm.v22i2.27938. [DOI] [PubMed] [Google Scholar]


