Abstract
Purpose:
To report the incidence, clinical features and natural course of central serous chorioretinopathy (CSR) in pregnant women in Kuwait.
Materials and Methods:
Patients were actively recruited from a private maternity hospital. Out of the 17,000 pregnant women who visited the antenatal care clinics (Al-Orf Hospital, Kuwait) over 3 years, 900 had visual complaints. Patients with visual complaints underwent complete ophthalmological assessment. Medical records of patients with CSR were reviewed, and a full clinical ophthalmological assessment was performed including measurement of best corrected visual acuity, intraocular pressure, slit lamp biomicroscopy, dilated indirect ophthalmoscopy and Amsler grid screening, color and red free fundus photography and retinal optical coherence tomography. All patients were evaluated throughout the course of pregnancy and for 6 months after delivery.
Results:
Four patients had CSR among the 17,000 pregnant women reviewed over 3 years corresponding to an incidence of 0.008 % per year. Two patients (50%) had CSR with white subretinal exudates and 2 (50%) had no exudates. There was complete resolution in all patients (100%) within 3 months after delivery.
Conclusions:
In pregnant women, CSR can present with or without retinal exudates and completely resolves in either case. Further studies with a larger sample size are warranted to investigate the risk factors in pregnant women.
Keywords: Central Serous Retinopathy, Chorioretinopathy, Pregnancy
INTRODUCTION
Central serous chorioretinopathy (CSR) is an idiopathic disease characterized by serous detachment of the neurosensory retina in the macular region secondary to a focal retinal pigment epithelial defect. CSR predominantly affects young and middle-aged males between 20 and 50 years of age. However, there are reports of CSR in females.1–5 Although CSR is generally unilateral, bilateral cases can occur. The presenting symptoms are often blurred vision, central scotoma, micropsia, or metamorphopsia. The disease is generally self-limited, with spontaneous resolution within 3 months.6 Risk factors for CSR include stress, steroids, pregnancy, systemic hypertension, Cushing's syndrome, lupus erythematosus, antibiotic and alcohol use, and allergic respiratory disease.7–11
The primary goal of this study was to determine the incidence of CSR among pregnant women in Kuwait. A secondary goal was to report the clinical features and natural history of CSR during pregnancy.
MATERIALS AND METHODS
The study was conducted in a private maternity hospital (Al-Orf hospital) Al-Jahra, Kuwait. The study was registered with the institution and approval was obtained from the institutional review board (IRB). This study adhered to the tenets of the Declaration of Helsinki. From April 1, 2006 to March 31, 2009, 17,000 pregnant women were assessed and followed up in antenatal care clinics.
All pregnant women were routinely questioned (questionnaire in Arabic language) about any visual symptoms (decreased visual acuity, micropsia, metamorphopsia, scotoma and abnormal color vision). Patients who reported any of these symptoms while pregnant were referred for a thorough ophthalmological assessment.
Comprehensive medical and ophthalmic histories were obtained with a review of the medical records of the patients referred for ophthalmological assessment. Ophthalmic assessment was performed by a single ophthalmologist (K.S.-Ahmed) and included measurement of best corrected visual acuity (BCVA), intraocular pressure (IOP), Amsler grid testing, slit lamp biomicroscopy and dilated indirect ophthalmoscopy. Color fundus photography was performed on suspected CSR cases by the same ophthalmologist (K.S.-Ahmed).
Fluorescein angiography was not performed, although there is no evidence of side effects to the fetus.12 Macular analysis with optical coherence tomography (OCT) was performed for confirmation of the diagnosis and repeated at the end of follow-up. Patients were referred for OCT imaging either to the Ministry of health eye hospital or to a private center in Kuwait city.
All patients were evaluated monthly for 3 months postpartum.
RESULTS
Nine hundred visually symptomatic pregnant women underwent ophthalmological assessment. Four (0.44%) of the 900 women referred were identified with shallow serous elevation of the sensory retina involving the fovea (CSR). Two patients had white subretinal exudates (50%) inferior to the neurosensory detachment and the other two patients did not present with exudates [Figures 1 and 2].
Figure 1.
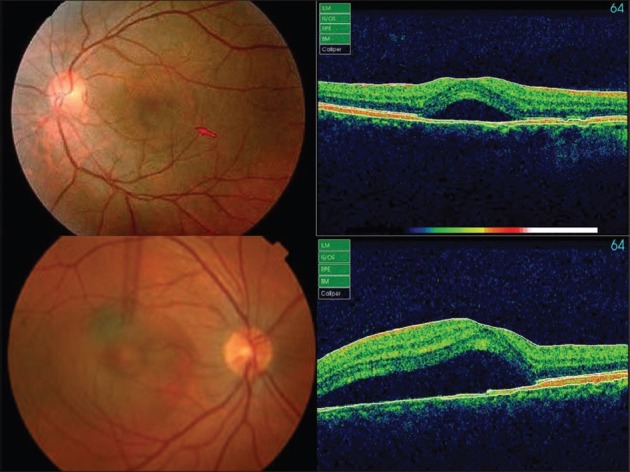
Colored fundus photographs and optical coherence tomography of nonexudative central serous chorioretinopathy in patients No. 1 and 4
Figure 2.
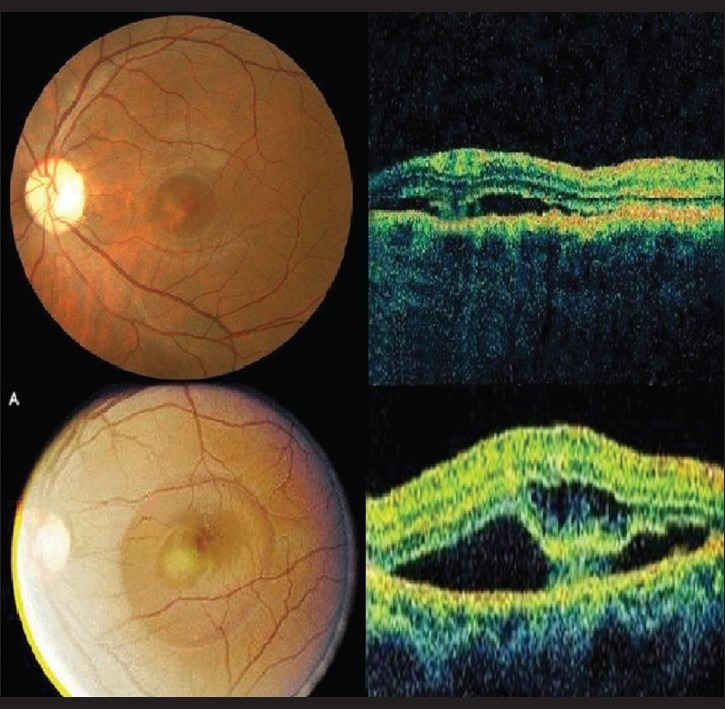
Colored fundus photographs and optical coherence tomography of exudative central serous chorioretinopathy in patients No. 2 and 3
The demographic and medical features of the four patients are summarized in Table 1. The size of the serous detachment varied from 1.5 disc diameters to 2.5 disc diameters. All four patients were Arabs. Patient age ranged from 29 to 36 years (mean 33±3.16 years). Gestational age at onset ranged from 28 to 31 weeks (mean 29±1.82 weeks).
Table 1.
Demographics and medical history of pregnant women with central serous chorioretinopathy
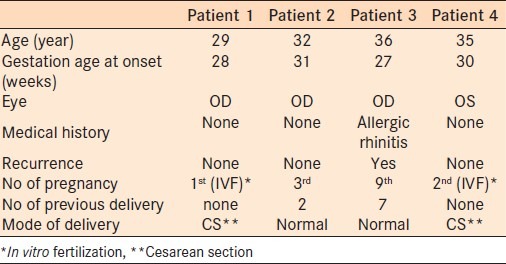
One patient (Patient # 3) had a history of allergic rhinitis and used steroid nasal spray prior to the current pregnancy. This patient gave a history of a similar episode of CSR during a previous pregnancy. Patients 1 and 4 were under intense stress due to a number of factors including multiple failed attempts at conception through in vitro fertilization. None of the patients had hypertension, diabetes mellitus or any other disease of relevance to CSR.
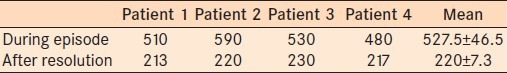
The presenting symptoms were blurred vision in all four patients, central scotoma in one patient and metamorphopsia in another patient [Table 2]. Neurosensory elevation partially involving the fovea was present in all patients. In addition, two patients (#2 and #3) had subretinal whitish exudates, with no signs of intraocular inflammation [Table 2]. OCT examination of the macula was performed within a week of the first examination and after clinical resolution of the neurosensory elevation in all patients. Table 3 presents the mean retinal thickness during CSR and after resolution. The CSR did not resolve during the course of pregnancy in any patients. All patients had spontaneous resolution of the neurosensory detachment and exudates after delivery within the follow-up period (mean 6.3±2.87 weeks). Resolution of the detachment and exudates led to an improvement of BCVA to 20/20 in three patients. Patient 3 regained BCVA to 20/25. This patient had multiple depigmented dots inferior to the fovea suggesting recurrent episodes of CSR. The mean retinal thickness at the end of follow-up was 220±7.3 μ.
Table 2.
Presenting symptoms of pregnant women with central serous chorioretinopathy
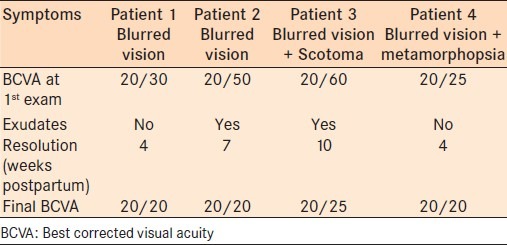
Table 3.
Retinal thickness of pregnant women during and after resolution of central serous chorioretinopathy
DISCUSSION
To our knowledge, this is the first prospective study of the incidence of CSR in pregnant women. Additionally it is the first to document CSR in pregnant women of Arabic ethnicity. There is a unique association between pregnancy and CSR; however, studies on the incidence of CSR in pregnant women are rare. Interestingly, the literature is rife with case reports about pregnant women with CSR. Kitzmann et al.,13 reported the results of a population based study on the incidence of CSR in Olmsted, Minnesota from 1980 to 2002 and found 11 females with CSR confirmed by fluorescein angiography, one of who was pregnant (9%). Kitzmann et al.,13 also reported nine cases of CSR without confirmation by fluorescein angiography, pregnancy was one of the risk factors affecting this group (one patient). In the current study, the incidence rate of CSR in pregnant women was 0.008% per year. The high incidence may be because the patients were non-white. However, this contradicts the findings of Sunness et al.,8 who rejected Gass’11 assumption regarding the higher risk of CSR in non-white pregnant women.
Stress is a well-documented risk factor for CSR.1–13 Our outcomes concur, as two of the study patients with CSR were under intense stress due to repeated failure with in vitro fertilization, this added another risk factor in addition to pregnancy. This observation may explain the high incidence of CSR in the study group as a considerable number of study patients had undergone in vitro fertilization. Gass11 reported six cases of CSR in pregnant women, all with subretinal exudates with no signs of intraocular inflammation. However, Gass did not explain the higher prevalence of exudates in pregnant women.11 Quillen et al.,9 have linked the higher association of subretinal exudates in CSR during pregnancy to the use of steroids. Alternately, Al-Mujaini et al.,5 reported three consecutive cases of CSR in pregnant Arab women, all without subretinal exudates. Sunness et al.,8 reported four cases of CSR in pregnant Caucasian women, three of the women had subretinal exudates. CSR with exudates was also reported in a pregnant black woman by Mayo and Tolentino.4 In the current study, subretinal exudates were found in two (50%) of the patients one of who was using steroid nasal spray prior to the current pregnancy and was discontinued once the patient was pregnant. Neither the influence of race nor the association of steroid use to exudates in CSR during pregnancy could be verified by this study due to the limited number of cases and the uniform race of patients.
One of the limitations of this study was the reliance on patient symptoms for the referral for ophthalmic assessment which may have missed CSR cases without foveal involvement or cases in which the affected eye was nondominant. However, this was unavoidable because of the impracticality of performing dilated fundus examination on all pregnant women at all antenatal follow-up visits.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gass JD. Stereoscopic Atlas of Macular Disease. 4th ed. St. Louis, Mo: Mosby; 1997. pp. 52–70. [Google Scholar]
- 2.Yannuzzi LA. Type A behavior and central serous chorioretinopathy. Trans Am Ophthalmol Soc. 1986;84:799–845. [PMC free article] [PubMed] [Google Scholar]
- 3.Perkins SL, Kim JE, Pollack JS, Merrill PT. Clinical characteristics of central serous chorioretinopathy in women. Ophthalmology. 2002;109:262–6. doi: 10.1016/s0161-6420(01)00951-4. [DOI] [PubMed] [Google Scholar]
- 4.Mayo GI, Tolentino MJ. Central serous chorioretinopathy in pregnancy. N Engl J Med. 2005;353:e6. doi: 10.1056/NEJMicm040678. [DOI] [PubMed] [Google Scholar]
- 5.Al-Mujaini A, Wali U, Ganesh A, Montana C. Natural course of central serous chorioretinopathy without subretinal exudates in normal pregnancy. Can J Ophthalmol. 2008;43:588–90. doi: 10.3129/i08-097. [DOI] [PubMed] [Google Scholar]
- 6.Klein ML, Van Buskirk EM, Friedman E, Gragoudas E, Chandra S. Experience with nontreatment of central serous choroidopathy. Arch Ophthalmol. 1974;91:247–50. doi: 10.1001/archopht.1974.03900060257001. [DOI] [PubMed] [Google Scholar]
- 7.Haimovici R, Koh S, Gagnon DR, Lehrfeld T, Wellik S Central Serous Chorioretinopathy Case-Control Study Group. Risk factors for central serous chorioretinopathy. Ophthalmology. 2004;111:244–9. doi: 10.1016/j.ophtha.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 8.Sunness JS, Haller JA, Fine SL. Central serous chorioretinopathy and pregnancy. Arch Ophthalmol. 1993;111:360–4. doi: 10.1001/archopht.1993.01090030078043. [DOI] [PubMed] [Google Scholar]
- 9.Quillen DA, Gass DM, Brod RD, Gardner TW, Blankenship GW, Gottlieb JL. Central serous chorioretinopathy in women. Ophthalmology. 1996;103:72–9. doi: 10.1016/s0161-6420(96)30730-6. [DOI] [PubMed] [Google Scholar]
- 10.Loo JL, Lee SY, Ang CL. Can long-term corticosteroids lead to blindness? A case series of central serous chorioretinopathy induced by corticosteroids. Ann Acad Med Singapore. 2006;35:496–9. [PubMed] [Google Scholar]
- 11.Gass JD. Central serous chorioretinopathy and white subretinal exudation during pregnancy. Arch Ophthalmol. 1991;109:677–81. doi: 10.1001/archopht.1991.01080050091036. [DOI] [PubMed] [Google Scholar]
- 12.Sunness JS. Pregnancy and the eye. Ophthalmol Clin North Am. 1992;5:623–40. [Google Scholar]
- 13.Kitzmann AS, Pulido JS, Diehl NN, Hodge DO, Burke JP. The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980-2002. Ophthalmology. 2008;115:169–73. doi: 10.1016/j.ophtha.2007.02.032. [DOI] [PubMed] [Google Scholar]


