Abstract
Purpose:
The purpose was to estimate the prevalence of blindness due to cataract, assess visual outcomes of cataract surgery, and determine the cataract surgical coverage rate and barriers to uptake of services among individuals aged 50 years or older in Plateau State, Nigeria.
Materials and Methods:
A population-based, cross-sectional survey of 4200 adults 50 years or older was performed. Multistage stratified random sampling, with probability proportional to size was used to select a representative sample. The Rapid Assessment of Cataract Surgical Services protocol was used. Statistical significance was indicated by (P < 0.05).
Results:
The cohort comprised 4115 subjects (coverage: 98%). The prevalence of bilateral blindness due to cataract was 2.1%, [95% confidence intervals (CI): 1.7-2.5%] in the entire cohort, 2.4% in females (95% CI: 1.8-3.8%); and 1.8% in males (95% CI: 1.2-2.4%) (χ2 = 0.85, P > 0.05). The prevalence of monocular blindness due to cataract was 5.9% (95% CI: 5.2-6.6%). The cataract surgical coverage for subjects with visual acuity (VA) less 3/60 was 53.8% in the entire cohort; 60.5% for males and 48% for females (χ2 = 2.49, P > 0.05). The couching coverage for subjects who were blind was 12%. A total of 180 eyes underwent surgical intervention (surgery or couching) for cataract, of which, 48 (26.7%) eyes underwent couching. The prevalence of bilateral (pseudo) aphakia was 1.5%, (95% CI: 1.2-1.9%) and 2.7% (95% CI: 2.2-3.2%) for unilateral (pseudo) aphakia. Visual outcomes of the 180 eyes that underwent surgical intervention were good (VA ≥ 6/18) in 46 (25.6%) eyes and poor (VA < 6/60) in 105 (58.3%) eyes. Uncorrected aphakia was the most common cause of poor outcome (65.1%). Most subjects who underwent cataract surgery were not using spectacles 74 (71.2%). Cost and lack of awareness were the main barriers to uptake of cataract surgery services.
Conclusion:
Couching remains a significant challenge in Nigeria. The outcomes of cataract surgery are poor with the lack of aphakic correction being the main cause of the poor outcomes.
Keywords: Barriers, Blindness, Cataract, Coverage, Outcome
INTRODUCTION
Cataract accounts for 47.8% of the 37 million blind people worldwide.1 Among individuals aged 40 years or older and 50 years or older in Nigeria, the prevalence of blindness is 4.2% and 5.5% respectively.2 Cataract accounts for 43% of blindness, and at least 400, 000 individuals are affected by an operable cataract (i.e. visual acuity of < 6/60 attributable to cataract) in Nigeria.3
Plateau state is in the North-central geopolitical zone of Nigeria and is administratively divided into three senatorial districts with seventeen Local Government Areas (LGAs) and has a population of 3.2 million. Two senatorial districts have six LGAs each while one has five LGAs. Geographic, cultural, ethnic and dietary links exist within each senatorial district. Access to eye care services is relatively similar within each senatorial district. Approximately 15% of the population are 50 years of age or older.4 Comprehensive eye care services including cataract surgical services are provided by nine hospitals comprising one tertiary centre, a state-owned specialist hospital, three mission hospitals and four private hospitals. Only one centre (a mission hospital) is located outside the state capital, Jos. The tertiary centre and two mission hospitals have satellite offices and services that allow referral of patients to the base hospitals for surgery. Surgical eye camps are organized periodically. However, no centre has baseline data for the cataract services it routinely provides.
Both human and material resources are limited in most eye care programmes in Nigeria which necessitates efficient allocation of these resources. Realistically; planning, implementation, monitoring and evaluation cannot be performed without reliable data. Hence, we performed a study to estimate the prevalence of blindness due to cataract, audit the visual outcomes of cataract surgery, assess cataract surgical coverage (CSC) and barriers to uptake of services among individuals 50 years of age or older in Plateau State, Nigeria.
MATERIALS AND METHODS
This was a population-based, cross-sectional survey. Ethics approval was granted from the Medical Ethics Committee of Jos University Teaching Hospital, Nigeria. An informed verbal consent was obtained from each subject. The survey was conducted in three Local Government Areas in January, March and November 2007.
Sample size calculation
An electronic copy of the 1998 census data for the state was obtained from the state office of the National Population Commission. The estimated target population was 627,206. To calculate the minimum sample size, the following parameters were used in the Rapid Assessment of Cataract Surgical Services (RACSS) software: an estimated prevalence of blindness due to cataract of 4% observed in a similar study in Northern Nigeria,5 the precision of the prevalence of blinding cataract expected from this study was likely to be within ± 10% of the reference value (4%) in relative terms (i.e. will lie between 3.6-4.4%); 95% confidence intervals (CI) and a design effect of 1.7. The minimum sample size was 4148 subjects. Seventy clusters of sixty individuals (aged 50 years or older) were to be examined.
Selection of clusters
The name of each LGA was written on a piece of paper which was folded and dropped into a ballot box allotted to its senatorial district. One LGA was randomly selected from each senatorial district by balloting. All settlements therein constituted the sampling frame. We were confident that one LGA is representative of each senatorial district because of the similarities that exist within each senatorial district as outlined above. Hence, results from these LGAs could be confidently extrapolated to the whole state. The list of all settlements in the selected LGAs with their population were entered into a Microsoft excel (Microsoft Corp., Redmond, WA, USA) spreadsheet. The first column contained the names of the settlements; the second column contained the total population of each settlement and the cumulative population was calculated in the third column. The total population of the three selected LGAs was 433,367. This figure was divided by 70 to obtain a sampling interval of 6190. A random number 0.655 was generated with the RACSS software which was multiplied by the sampling interval (6190) to obtain the first cluster corresponding to 4054. This number was marked on the cumulative frequency list. The settlement in which this number fell was the settlement where the first cluster was located. To identify the settlement with the second cluster, the sampling interval 6190 was added to the number that identified the first cluster. The settlement in which this number fell was taken as the second cluster. The sampling interval was added again to find the settlement for the third cluster, etc, until all 70 clusters were located.
Data collection procedures
There were four survey teams. Each team was comprised of an ophthalmologist, ophthalmic nurse and a local health worker or village volunteer. The random walk method was used to examine the first sixty subjects in each cluster. The standardized RACSS pro-forma was used to collect data. Visual Acuity (VA) was measured by an ophthalmic nurse using a test distance of 6 meters with an un-illuminated “E” chart in daylight. First, the presenting VA was assessed either unaided or with presenting spectacles. Subjects with a presenting VA < 6/18 were reassessed with pinhole. Subjects must have correctly identified all the letters on the 6/18 line to score a VA of 6/18.
The ocular examination was performed by an ophthalmologist. The crystalline lens was graded as normal, obvious lens opacity, aphakia, pseudophakia without posterior capsule opacification (PCO) or pseudophakia with PCO, and “no view” if the lens could not be examined due to other ocular pathology e.g. dense leucoma. In the absence of ocular pathology, subjects with VA ≥ 6/18 in each eye were discharged. The anterior segment of the eye was examined with penlight (torch examination) and the posterior segment was examined with a direct ophthalmoscope.
The principal cause of visual loss for each eye and for the individual was documented in accordance with WHO guidelines.6 The major cause of visual loss in an eye was attributed to be the primary disorder for the eye. When two primary disorders were present in an eye, the treatable cause of visual loss was selected; otherwise, the preventable cause of visual loss was selected.6 The principal cause of visual loss for the individual was determined using the above criteria if both eyes had different disorders.
Participants with presenting VA < 3/60 in one or both eyes which did not improve with pinhole, in the presence of obvious lens opacity in the same eye (s) were asked a standard question “Why have you not been operated for cataract?” Each participant was allowed to provide four reasons. The responses were matched with a list of predetermined options provided in the RACSS questionnaire. For each eye that had cataract surgery, details about the surgical intervention were obtained. These details included the subject's age at the time of the surgical intervention; the location the procedure was performed, the type and the cost of the procedure, use of spectacles and reasons for not using spectacles.
If an eligible individual was absent, the team returned to the house the same day. If after repeated visits the individual could not be contacted, demographic and visual status information (believed not blind or believed blind) about the person was obtained from relatives or neighbours. The closest settlement was visited to complete sampling if the expected number of subjects could not be obtained in a selected cluster.
Training
All field staff were trained on the study procedure. A reliability study was conducted to measure the level of agreement between examiners in measuring VA and assessing lens status in accordance with guidelines in the RACSS manual. The kappa value indicated very good agreement (κ > 0.61) between examiners.
Data on 4200 individuals were entered into the RACSS software (based on Epi-info version 6.04d, WHO, Geneva, Switzerland).
Data entry was validated by double entry and crosschecking of the entries. RACSS software was used for data analysis.
The parameters investigated in the study were the prevalence and causes of visual impairment and blindness, prevalence of blinding cataract, aphakia and pseudophakia, cataract surgical coverage, visual outcomes of cataract surgery, major causes of poor visual outcome, barriers to cataract surgery, age at time of surgery, type of surgery, location of surgery, use of spectacles, and reasons for not using spectacles.
RESULTS
A total of 4115 subjects 50 years of age or older were examined across the state (coverage was 98%). Fifty-five (1.3%) individuals were unavailable and 30 (0.7%) refused examination.
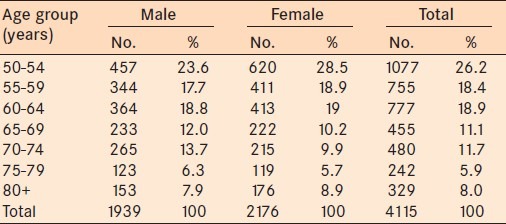
There were more females, 2176 (52.9%), than males in the study cohort [Table 1]. A greater number of females 23 (76.7%) refused examination.
Table 1.
Study Cohort stratified by age and gender
The prevalence of bilateral blindness was 4.2% (95% CI: 4.1-4.3). The main causes of blindness were cataract (57.2%), glaucoma (16.8%), uncorrected aphakia (10.4%), other corneal opacity (6.4%), corneal opacity secondary to trachoma (3.5%), pthisis bulbi/no globe (1.7%), surgical complications (1.2%), macular degeneration (1.2%), and other posterior segment lesions (1.7%).
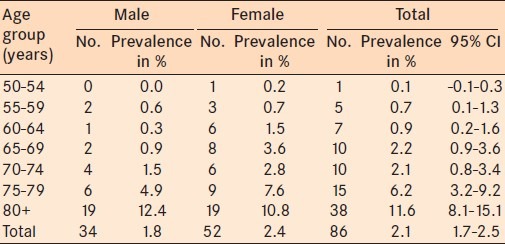
Blindness due to cataract
A total of 86 subjects were blind due to cataract (VA < 3/60 in the better eye), giving a prevalence of bilateral blindness due to cataract of 2.1%, (95% CI: 1.7-2.5%). The prevalence in females was 2.4%, (95% CI: 1.8-3.0%) and 1.8% in males (95% CI: 1.2-2.4%) (χ2 = 0.85, P > 0.05). The prevalence of bilateral blindness due to cataract increased significantly with age from 0.1% (95% C1: –0.1-0.3%) at 50-54 years to 11.6% (95% CI: 8.1-15.1%) in subjects 80 years or older, (χ2 = 197.9, P < 0.001) [Table 2]. An estimated 10,000 individuals 50 years of age or older are blind bilaterally due to cataract in Plateau state.
Table 2.
Prevalence of bilateral blindness due to cataract stratified by age
There were 243 subjects who had monocular blindness due to cataract which corresponds to a prevalence of 5.9% (95% CI: 5.2-6.6%). The prevalence was 6.6%, (95% CI: 5.5-7.7%) in males and 5.3%, (95% CI: 4.4-6.2%) in females. There was statistically significant increase in the prevalence of monocular blindness due to cataract with increasing age (χ2 = 168.5, P < 0.001). An estimated 28,000 individuals 50 years of age or older have monocular blindness due to cataract in the state.
There were 415 (5.0%) eyes that were classified as blind (monocular or bilateral) due to cataract in the study cohort.
Cataract surgical coverage
The CSC in subjects with VA < 3/60 was 53.8%. Males had better CSC (60.5%) than females (48%) (χ2 = 2.49, P > 0.05). The CSC in subjects with VA < 6/60 was 43.8%. Males had better CSC (49.1%) than females (39.1%) (χ2 = 1.1, P > 0.05).
The CSC in eyes with VA < 3/60 was 36.4%. Males had better CSC (40%) than females (32.7%) (χ2 = 4.7, P < 0.05).
The CSC in eyes with VA < 6/60 was 29.4%. Males had better CSC (33.4%) compared to females (25.7%) (χ2 = 5.8, P < 0.05).
Couching coverage
The couching coverage for subjects with VA < 3/60 was 12%. Males had a higher couching coverage (15.6%) than females (8.9%) (χ2 = 0.01, P > 0.05). For subjects with VA < 6/60, the couching coverage was 9.3%. Males had a higher couching coverage (12%) than females (6.7%) (χ2 = 0.06, P > 0.05).
Cataract procedure
The type of cataract surgery 5 years or more prior to this survey is presented in Figure 1. One hundred and nineteen subjects (2.9%) underwent a procedure for cataract. Sixty-one (51.3%) subjects had bilateral surgery and 58 (48.7%) subjects had unilateral surgery. There were 65 (54.6%) males and 54 (45.4%) females who underwent cataract surgery. Among the male subjects, 37 (56.9%) underwent cataract surgery with intraocular lens (IOL) implantation, 15 (23.1%) underwent cataract surgery without IOL implantation, and 13 (20%) underwent couching. Among the males who underwent cataract surgery with IOL implantation, 20 (54.1%) had the procedure between the age of 50 and 64 years of age. Eight (61.5%) of the males who underwent couching had the procedure at 65 years of age or older, the remaining male subjects underwent couching at less than 65 years of age.
Figure 1.
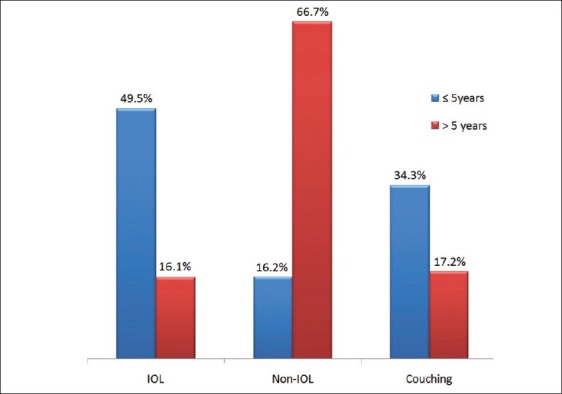
Distribution of type of cataract surgery; 5 years and > 5 years prior to survey
Cataract surgery with IOL implantation was performed in 23 (42.6%) female subjects, 17 (31.5%) females underwent cataract surgery without IOL implantation, and 14 (25.9%) females underwent couching. Ten (43.5%) females underwent IOL surgery between 50 and 64 years of age and 10 (71.4%) females underwent couching at 60 years of age or older.
A total of 180 eyes underwent cataract surgery or couching; 99 (55%) eyes underwent the procedure within 5 years prior to this survey; and 81 (45%) eyes underwent the procedure more than 5 years prior to this survey. There were a statistically significant greater number of IOL implantation (49 eyes; 49.5%) within the 5 years immediately preceding this survey compared to 13 eyes (16.1%) more than 5 years prior to this survey (χ2 = 48.6, P < 0.001). A greater number (54 eyes; 66.7%) of cataract surgeries without IOL implantation were performed more than 5 years prior to this survey. Within 5 years prior to this survey, 34.3% (34/99) of eyes underwent couching which is approximately twice as high (17.2%; 14/81 eyes) as more than 5 years prior to this survey.
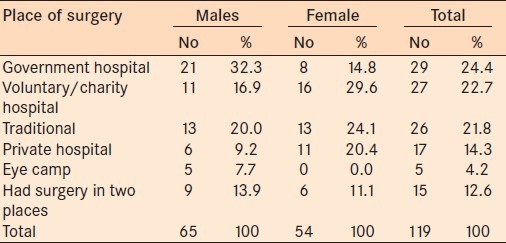
Place of surgery
Fifty-six subjects (47.1%) underwent surgery at a government or mission hospital, 17 (14.3%) in a private hospital, 5 (4.2%) in an eye camp setting, and 26 (21.8%) in a traditional setting. Fifteen (12.6%) subjects who underwent a bilateral procedure had each eye done at a different locale [Table 3].
Table 3.
Location of cataract surgery or couching in the study cohort
Cataract surgical outcome
Of the 180 eyes that underwent a procedure, 62 (34.4%) underwent cataract surgery with IOL implantation, 70 (38.9%) had cataract surgery without IOL implantation, and 48 (26.7%) underwent couching. Forty-six (25.6%) eyes had good outcome (VA ≥ 6/18), 29 (16.1%) had a borderline outcome (VA < 6/18-6/60) while 105 (58.3%) eyes had a poor outcome (VA < 6/60) [Table 4].
Table 4.
Presenting postoperative visual acuity of eyes that underwent cataract surgery or couching
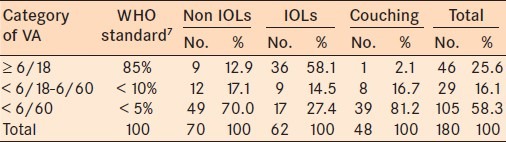
A greater number of eyes (58.1%; 36/62) that had undergone IOL implantation attained good outcome compared to the other procedures [Table 4]. The worst outcomes were achieved in eyes that had undergone couching, 81.2% eyes attaining poor visual outcomes [Table 4].
Seventeen (27.4%) eyes that received an IOL implant had a poor outcome. Of these, seven (41.2%) were due to surgery-related complications, 10 (58.8%) were due to coexisting ocular morbidity. There has been a gradual improvement in the surgical outcome among eyes with an IOL implant. The shorter the duration between the surgery and the survey, the better the outcome in eyes that received an IOL implant. Up to 86.6% of eyes with an IOL implant operated less than 2 years prior to the survey had a good outcome. Only 6.7% had a poor outcome [Figure 2].
Figure 2.
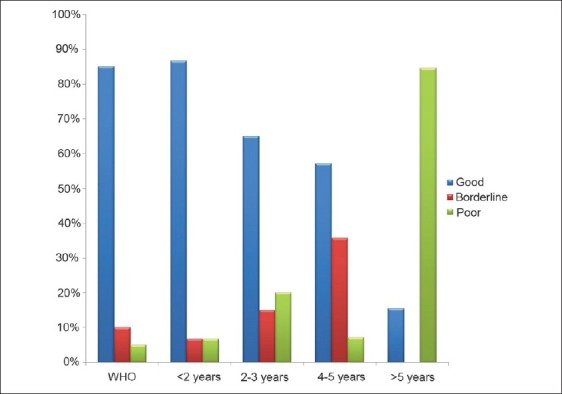
Outcome of IOL surgery with duration
Poor outcomes were due to uncorrected aphakia in 56 (65.1%) subjects while surgery-related complications and coexisting ocular morbidity accounted for poor outcomes in the remaining 12 (14%) subjects and 18 (20.9%) subjects respectively.
Prevalence of pseudo (aphakia)
The prevalence of bilateral pseudo (aphakia) was 1.5% (95% CI: 1.2-1.9%). Males had greater pseudo (aphakia) (1.7%; 95% CI: 1.1-2.3%) than females (1.4%; 95% CI: 0.9-1.9). The prevalence of bilateral pseudo (aphakia) increased statistically significantly with age from 0.1% at 50-54 years to 6.4% for subjects 80 years of age or older (χ2 = 89.2, P < 0.001).
The prevalence of unilateral pseudo (aphakia) was 2.7% (95% CI: 2.2-3.2%). Unilateral (pseudo) aphakia was present in 3.4% (95% CI: 2.6-4.2) of males and 2.1% (95% CI: 1.5-2.7) of females. The prevalence of unilateral (pseudo) aphakia increased statistically significantly with age from 0.9% at age 50-54 years to 7.0% for subjects 80 years of age or older (χ2 = 66.1, P < 0.001). Thirty-seven (0.9%) subjects had one (pseudo) aphakic eye and the other eye blind due to cataract.
Use of spectacles and payment of surgery
Most subjects (74; 71.2%) were not using spectacles after the cataract procedure. Of these, 48 (64.9%) were never provided spectacles while 14 (18.9%) did not require spectacles because of IOL implantation. Eleven (14.9%) subjects who were not using spectacles had undergone bilateral surgery without IOL implantation. Of these, six (54.5%) subjects were never provided with spectacles while five (45.5%) subjects reported their spectacles were damaged.
Most patients 85 (81.7%) paid the entire cost for surgery. Only seven (6.7%) had surgery totally free. No female had free surgery.
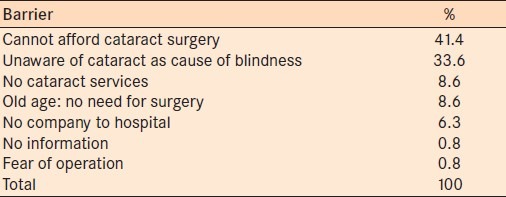
Barriers to uptake of cataract surgical services
Cataract services were unaffordable to most individuals who are blind due to cataract. This was the most frequent reason stated by 53 (41.4%) respondents. Forty-three (33.6%) subjects were unaware of cataract as the cause of blindness [Table 5]. The main barriers to uptake of cataract among the subjects with monocular blindness due to cataract were a lack of awareness of cataract among 113 (38.0%) subjects, followed by the expense of surgery in 109 (36.7%) subjects.
Table 5.
Barriers to cataract surgery as indicated by Subjects with bilateral blindness due to cataract
DISCUSSION
In this survey, cataract induced blindness was the major cause of blindness in Plateau state, Nigeria. This outcome is similar to a national Nigerian blindness survey.3 The prevalence of blindness due to cataract in the current study (2.1%) is similar to the national level (1.8%),2 and that reported for Kebbi state Nigeria, (2.1%)8 and Ethiopia (3.2%).9 However the prevalence was higher than that reported for South-Western Nigeria (0.84%).10 This difference can be attributed to the skewed distribution of ophthalmologists in favor of the South-West geo-political zone of Nigeria.11
We found more females had cataract although this was not statistically significant. A significant female preponderance among the cataract blind has been reported in the Nigerian National Survey.3 It is known that more females are blinded by cataract globally due to a slightly higher incidence of cataract, poor access to eye care services, and longer life expectancy.12
More men had access to services. In most African settings, there is a gender gap in terms of access to cataract services mostly attributed to gender-defined social roles.13 Most rural women, have less disposable income and little control over finances. The total cost of surgery, (which includes transportation, living expenses, hospital bill, etc.) is often prohibitive. Programs targeted to health education in a gender-sensitive fashion within the community are required to address this gender inequality. The CSC for subjects with VA < 3/60 was 53.8% which is much better than in other regions of Northern Nigeria. For example, it is 22.1% in Katsina State and 28.9% in Birnin Kebbi.5,8 This difference is probably due to the better availability and accessibility of services in Plateau State. The CSC was however; lower than other countries in Sub-saharan African such as Kenya (78%) where there is a better community-based cataract intervention program.14 Similarly, the CSC for subjects with VA < 6/60 was lower than those reported for Botswana and Nepal. These differences are probably due to better intervention strategies in these countries compared to Nigeria.15,16
The couching coverage observed in the present study is less than that reported by Rabiu (18% and 32.9% in Katsina and Kebbi States, Nigeria, respectively).5,8 Noteworthy from our survey is the observation that couching practices in Plateau state had doubled within 5 years prior to the survey. Unhindered couching which is worse in Northern Nigeria, was also observed in the Nigerian National Survey. However, in contrast to findings from the study, the proportion of eyes that had been couched in the national survey remained constant over time.17 The elderly and females had a greater tendency to pursue couching as an option. This can be attributed to the absence of services, lack of awareness, financial constraints, and the fact that most females require permission from their husbands before they can travel for medical care. Thus, the elderly and females tend to opt for this crude, unacceptable intervention that is continually available in the communities.
Couching apparently appears more affordable in terms of cost and duration of payment as this could be made in cash or kind over several months. Couching thus remains a major challenge to eye care in Nigeria. The message for public ophthalmic care planners including ophthalmologists is that cataract surgical services have to be accessible, affordable, and of high quality to individuals in the community.
The visual outcomes of the present study fell below the WHO recommended values of ≥ 85%, < 10%, and < 5% with good, borderline, and poor outcome with available correction respectively.7 Similar poor results were observed in Ethiopia (23.7%),9 Malawi (23.3%),18 Lower Dir (40.5%),19 Chakwal, Pakistan (32.2%),20 and China (45%).21 This outcome is especially concerning. An audit of cataract outcomes from a population-based study like this includes patients that have undergone procedures recently as well as decades earlier; procedures that have been performed under excellent and unfavorable conditions and; those procedures performed by experienced and relatively in-experienced surgeons even couchers. Additionally, aphakic spectacles may have been lost or damaged. Individuals who previously had a good outcome may have developed other ocular morbidities that reduce vision as they age. Hence the data can be affected by these factors. Population-based outcome data may not provide an accurate snapshot of the recent advances in cataract surgery, yet these surveys portray what the public sees and reflect their expectations and trust on regaining sight after surgery. This study found that a higher proportion of eyes that received an IOL implant (58.1%) had a good outcome consistent with findings from the Nigerian National Survey (54.9%).17 Notably, up to 86.6% of eyes with an IOL implant performed < 2 years prior to the survey had a good outcome. This is encouraging and could increase patient confidence in conventional cataract surgery performed by an ophthalmologist. Greater effort needs to be directed at improving the quality of cataract surgery through improvement in areas such as case selection, postoperative care, training, and ongoing professional development of surgeons and nurses. Cost recovery with patient subsidization is essential so that the poor can have equitable access.
Eyes with couching had the worst outcome similar to findings in Kebbi state, Nigeria (90.6%),8 and the Nigerian National Survey (74.6%).17 The extent of couching practices observed (25%) is also similar to findings from the North-central geopolitical zone (20.8%) reported in the Nigerian National Survey.17 There is an urgent need to discourage such practices. Useful measures include purposeful dialog between professionals such as ophthalmologists and their societies, health policy makers, traditional healers, community leaders, and female leaders.
Uncorrected aphakia was the main cause of poor outcome of surgery in the present study. A similar finding has also been reported in Malawi (50%).18 For several years, aphakic spectacles were the main tool for rehabilitation of bilateral aphakia in Nigeria. Once these spectacles were lost or broken, patients rarely replace them due to the cost and the inconveniences of traveling to distant overcrowded eye clinics. Ensuring that patients have and use their prescribed spectacles after surgery will improve the outcome of cataract surgery.
The barriers to uptake of cataract services observed in the present study are all similar to those observed in other parts of Northern Nigeria.5,22 Cost as a barrier, may be reduced by decreasing the cost of surgery by reducing the cost of supplies and equipment and improving efficiency. The clinical "triad" of white lens, white hair, and wrinkled skin has been misinterpreted. People consider these changes including cataract as an inevitable result of aging that need not to be interrupted by therapeutic interventions. Lack of awareness of cataract may also be a result of language barriers and a lack of familiarity with the health system. Community-based education about cataract in the local language is warranted State wide. In our setting, the media and Community Health Extension Workers (CHEWs) who are members of the community can be very useful in this initiative. Patients who are satisfied with postoperative outcome and live in the community can also serve as excellent motivators for others to have surgery.
The findings in this study will help the State Ministry of Health and International Non-Governmental Organizations involved in rendering eye care services to plan, implement, monitor, and evaluate cataract intervention programs in Plateau State.
The main strength of this survey is the significant coverage. A limitation of the study was the lack of age-sex adjusted prevalence of cataract blindness as appropriate census information was not available.
Couching is a major challenge in Plateau State. Outcomes of cataract surgery were poor and the lack of aphakic correction is the main cause of this poor outcome. Appropriate, accessible, affordable, high quality, and gender-sensitive cataract surgical services are required to meet the objectives of “Vision 2020: The Right to Sight.”
ACKNOWLEDGMENTS
We acknowledge Dark and Light Foundation, Netherlands for funding this study and for logistic support, we acknowledge the Local Government Chairmen of Langtang-South, Bokkos and Bassa Local Government Areas of Plateau State, Nigeria where the survey was carried out.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–51. [PMC free article] [PubMed] [Google Scholar]
- 2.Kyari F, Gudlavalleti MV, Sivsubramaniam S, Gilbert CE, Abdull MM, Entekume G, et al. Prevalence of blindness and visual impairment in Nigeria: The national blindness and visual impairment study. Invest Ophthalmol Vis Sci. 2009;50:2033–9. doi: 10.1167/iovs.08-3133. [DOI] [PubMed] [Google Scholar]
- 3.Abdull MM, Sivasubramaniam S, Murthy GV, Gilbert C, Abubakar T, Ezelum C, et al. Causes of blindness and visual impairment in Nigeria: The Nigeria national blindness and visual impairment survey. Invest Ophthalmol Vis Sci. 2009;50:4114–20. doi: 10.1167/iovs.09-3507. [DOI] [PubMed] [Google Scholar]
- 4.United State census bureau-international data base. Nigerian Midyear Population, by Age and Sex. 1998. [Last accessed on 2006 December 15]. Available at http://www.uni.edu/gai/Nigeria/Lessons/Population_Pyramid. html .
- 5.Rabiu MM. Cataract blindness and barriers to uptake of cataract surgery in a rural community of northern Nigeria. Br J Ophthalmol. 2001;85:776–80. doi: 10.1136/bjo.85.7.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coding instructions for the WHO/PBL eye examination record (version III) Geneva: WHO; 1988. World Health Organization. Programme for the prevention of blindness and deafness; pp. 1–17. [Google Scholar]
- 7.Limburg H. Monitoring cataract surgical outcomes: Methods and tools. Community Eye Health. 2002;15:51–3. [PMC free article] [PubMed] [Google Scholar]
- 8.Rabiu MM, Muhammed N. Rapid assessment of cataract surgical services in birnin-kebbi local government area of Kebbi state, Nigeria. Ophthalmic Epidemiol. 2008;15:359–65. doi: 10.1080/09286580802399078. [DOI] [PubMed] [Google Scholar]
- 9.Bejiga A, Tadess S. Cataract surgical coverage and outcome in Goro district, central Ethiopia. Ethiop Med J. 2008;46:205–10. [PubMed] [Google Scholar]
- 10.Oluleye TS. Cataract blindness and barriers to cataract surgical intervention in three rural communities of Oyo state, Nigeria. Niger J Med. 2004;13:156–60. [PubMed] [Google Scholar]
- 11.Abiose A. Challenges for Nigerian ophthalmologists. Lecture; National Postgraduate Medical College of Nigeria. 1999:9. [Google Scholar]
- 12.Courtright P, Bassett K. Gender and blindness: Eye disease and the use of eye care services. Community Eye Health. 2003;45:11–2. [PMC free article] [PubMed] [Google Scholar]
- 13.Lewallen S, Courtright P. Gender and use of cataract surgical services in developing countries. Bull World Health Organ. 2002;80:300–3. [PMC free article] [PubMed] [Google Scholar]
- 14.Mathenge W, Kuper H, Limburg H, Polack S, Onyango O, Nyaga G, et al. Rapid assessment of avoidable blindness in Nakuru district, Kenya. Ophthalmology. 2007;114:599–605. doi: 10.1016/j.ophtha.2006.06.057. [DOI] [PubMed] [Google Scholar]
- 15.Nkomazana O. Disparity in access to cataract surgical services leads to higher prevalence of blindness in women as compared with men: Results of a national survey of visual impairment. Health Care Women Int. 2009;30:228–9. doi: 10.1080/07399330802662010. [DOI] [PubMed] [Google Scholar]
- 16.Sapkota YD, Pokharel GP, Nirmalan PK, Dulal S, Maharjan IM, Prakash K. Prevalence of blindness and cataract surgery in Gandaki zone, Nepal. Br J Ophthalmol. 2006;90:411–6. doi: 10.1136/bjo.2005.082503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilbert CE, Murthy GVS, Sivasubramaniam S, Kyari F, Imam A, Rabiu MM, et al. Couching in Nigeria: prevalence, risk factors and visual acuity outcomes. Ophthalmic Epidemiol. 2010;17:269–75. doi: 10.3109/09286586.2010.508349. [DOI] [PubMed] [Google Scholar]
- 18.Courtright P, Metcalfe N, Hoechsmann A, Chirambo M, Lewallen S, Barrows J, et al. Cataract surgical coverage and outcome of cataract surgery in a rural district in Malawi. Can J Ophthalmol. 2004;39:25–30. doi: 10.1016/s0008-4182(04)80049-8. [DOI] [PubMed] [Google Scholar]
- 19.Shaikh SP, Aziz TM. Rapid assessment of cataract surgical services in age group 50 years and above in lower dir district Malakand, Pakistan. J Coll Physicians Surg Pak. 2005;15:145–8. [PubMed] [Google Scholar]
- 20.Haider S, Hussain A, Limburg H. Cataract blindness in Chakwal district, Pakistan: Results of a survey. Ophthalmic Epidemiol. 2003;10:249–58. doi: 10.1076/opep.10.4.249.15907. [DOI] [PubMed] [Google Scholar]
- 21.Wu M, Yip JL, Kuper H. Rapid assessment of avoidable blindness in Kunming, China. Ophthalmology. 2008;115:969–74. doi: 10.1016/j.ophtha.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Mpyet C, Dineen BP, Solomon AW. Cataract surgical coverage and barriers to uptake of cataract surgery in leprosy villages of north eastern Nigeria. Br J Ophthalmol. 2005;89:936–8. doi: 10.1136/bjo.2004.062455. [DOI] [PMC free article] [PubMed] [Google Scholar]


