Abstract
Purpose:
To assess the change in intraocular pressure (IOP) in Egyptian patients after selective laser trabeculoplasty (SLT) as a primary or adjunctive treatment for primary open-angle glaucoma (POAG).
Materials and Methods:
One hundred and six eyes with POAG were enrolled in this prospective study. Patients were divided into two groups: recently diagnosed cases with no preoperative medications (group 1) and; patients with confirmed glaucoma on medical therapy (group 2). All patients underwent 360° SLT. Patients were evaluated to 18 months postoperatively. Data were analyzed on postoperative changes in IOP, number of medications and complications. A P-value less than 0.05 was statistically significant.
Results:
A statistically significant drop in IOP occurred, from 19.55 ± 4.8 mmHg preoperatively, to16.03 ± 2.8 mmHg postoperatively (P< 0.001). Each group had a statistically significant drop in IOP (P< 0.001). There was a statistically significant decrease in the number of medications in group 2 from 2.25 ± 0.97 medications preoperatively to 1.0 ± 1.3 medications postoperatively (P=0.004). No serious complications occurred for the duration of the study.
Conclusion:
SLT can be safely and effectively used as primary or adjunctive therapy for the treatment of POAG.
Keywords: Laser, Primary Open-Angle Glaucoma, Selective Laser Trabeculoplasty, Treatment
INTRODUCTION
Selective laser trabeculoplasty (SLT) is a new and promising treatment that uses the 532-nm frequency-doubled q-switched neodymium:yytrium–aluminum–garnet laser. SLT was developed to selectively target pigmented trabecular meshwork (TM) cells without causing thermal or collateral damage to the nonpigmented cells or structures of the TM.1
Clinical trials of SLT have been encouraging, with reasonable response rates, effective intraocular pressure (IOP) reduction and minimal side effects.2–5 Comparable studies have shown SLT to be as effective as argon laser trabeculoplasty (ALT),6 while histological investigations have demonstrated less damage to the ultrastructure of the TM.7,8 As a result of these studies, SLT has been advocated as a treatment for the management of open-angle glaucoma (OAG) with a role as a possible primary treatment.3 In the current study, we assess the IOP lowering effect and the complications of SLT in Egyptian patients with primary open-angle glaucoma (POAG).
MATERIALS AND METHODS
This study was approved by the institutional review board and ethics committee. All patients consented to participation in the study after a thorough informed consent procedure. Sixty-five patients (106 eyes) were enrolled in this prospective study from June 2007 to January 2009. Patients with a diagnosis of OAG were considered eligible for this study if they were newly discovered on no previous medication (primary group of 41 eyes [group 1]), or had confirmed glaucoma poorly controlled on medications, or requesting a decrease number of medications (adjunctive group of 65 eyes [group 2]).
Patients were excluded from the study if they had evidence of glaucoma other than OAG (angle closure, inflammatory, or neovascular) in the study eye, were younger than 18 years, had any ocular condition in the study eye that hindered adequate visualization and treatment of the TM, (4) had prior glaucoma surgery in the study eye.
Preoperative assessment included ophthalmic examination Snellen visual acuity, IOP measurement by Goldmann applanation tonometry, slit-lamp examination and gonioscopy, and funduscopy with evaluation of cup:disc ratio and pallor. At least two preoperative IOP readings were taken within 2 weeks before the laser treatment was performed. The average of the preoperative IOP was used as the baseline IOP. Visual field testing was performed for all patients to confirm the diagnosis. A drop of miotic (pilocarpine nitrate 2%) and brimonidine tartrate 0.2% (Alphagan®; Allergan Inc., Irvine, CA) were installed in the eye before laser treatment to assist in visualization of TM and to prevent IOP spikes.
Surgery
The procedure was performed with topical benoxinate hydrochloride 0.4% for anesthesia. With the patient seated at the laser slit-lamp system, a Goldmann three-mirror goniolens or Latina lens was placed on the eye with methylcellulose 1%. Patients were treated with the Ellex, SOLO® SLT laser (Ellex Medical Pty. Ltd, Adelaide, Australia) a frequency-doubled q-switched Nd: YAG laser emitting at 532 nm with a pulse duration of 3 nsec and a spot size of 400 μm, coupled to a slit-lamp delivery system. A low-power helium–neon laser served as an aiming beam to provide easy targeting of the treatment area. The laser is capable of delivering pulse energies ranging from 0.2 to 1.7 mJ. Treatment began at 0.4 mJ and was titrated according to the response. If cavitation bubbles appeared the laser energy was reduced by 0.1 mJ until only a few bubbles formed and treatment was continued at this energy level. If no cavitation bubble was observed, the pulse energy was increased by 0.1 mJ until bubble formation and then decreased as described above. Higher energy was required for the treatment of the superior, less pigmented angle. Approximately 100 adjacent, but nonoverlapping, laser spots were placed over 360° of the TM.
Postoperative follow-up
Immediately after the laser treatment, prednisolone acetate (1%) drops were administered once in the treated eye then three times daily for 3 days. Alphagan® eye drops were also used to control postoperative IOP spikes. The IOP in the treated eye was assessed and recorded 1 hour after surgery. The same preoperative antiglaucoma medication regimen was continued until the second postoperative visit (1 week). Patients were evaluated at 1 day, 1 week, 2 weeks, 3 weeks, 4 weeks, and at 3, 6, 12 and 18 months. At each visit, the visual acuity and IOP were measured, and slit-lamp examination of the anterior segment was performed. Fundus examination and gonioscopy were repeated after 4 weeks of follow-up. A repeat visual field was performed every 6 months postoperatively. All major and minor complications and complaints were recorded and treated appropriately.
All ophthalmic medications were recorded before surgery and at each subsequent visit. Gradual reduction of antiglaucoma medications was initiated 1 week following the procedure, after ensuring an adequate pressure drop. Combined therapy was considered two medications and each medication was decreased separately. Medically necessary medication changes were made at the physician's discretion.
Statistical analysis
Data are described are range, mean ± standard deviation, frequencies (number of cases) and relative frequencies (percentages) as appropriate. Comparison of IOP over the study period was performed with one-way analysis of variance (ANOVA) with multiple comparisons post hoc for the two groups. Comparison of the number medications was performed with the Kruskal-Wallis analysis of variance (ANOVA) test with multiple comparisons post hoc for the two groups. A probability value (P-value) less than 0.05 was considered statistically significant. All statistical calculations were performed with Microsoft Excel version 7 (Microsoft Corporation, Redmond, WA) and SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL) version 13 for Microsoft Windows, Arcus QuickStat (Biomedical) (Research Solutions, Cambridge, UK).
RESULTS
Intraocular pressure changes
One hundred and six eyes with OAG were enrolled in the study and received 360° laser treatment of TM. Females comprised 53% of the cohort and the mean age of the cohort was 53.2 years (range, 18-78 years).
Mean preoperative IOP was 19.55 ± 4.8 mmHg which dropped significantly after 24 hours post-SLT to 12.03 ± 2.7 mmHg. IOP was 14.32 ±3.0 mmHg, 14.72 ± 2.1 mmHg, 15.16 ± 3.6 mmHg and 16.03 ± 2.8 mmHg at 1, 6, 12, and 18 months of follow-up, respectively. The decrease in mean IOP was statistically significant throughout follow-up (P< 0.001). There was a tendency towards increased IOP with follow-up, yet the mean final IOP at the end of the study was statistically significantly lower than the pretreatment mean IOP (P<0.05). Figure 1 shows the mean IOP and standard deviation (SD) of all patients throughout the study period.
Figure 1.
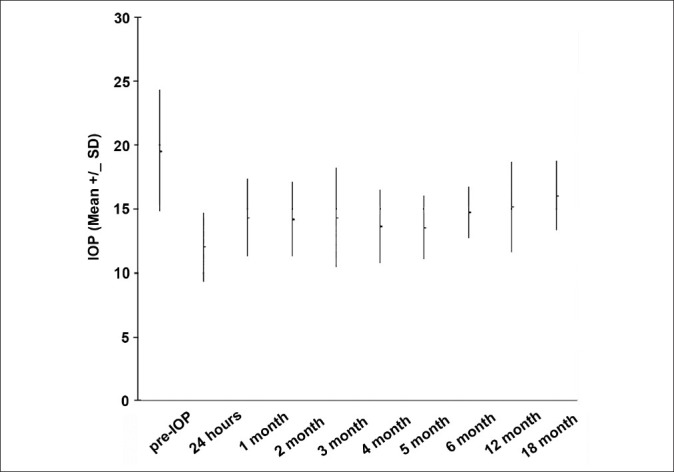
Mean (SD) intraocular pressure (mmHg) of all patients throughout the study
The mean decrease in effective intraocular pressure
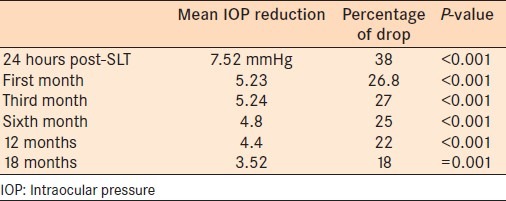
The greatest drop in IOP occurred 24 hours after SLT (7.52 mmHg) which was equivalent to a 38% drop from the baseline IOP. There was a tendency toward and increase in IOP during follow-up, with a mean IOP reduction of 3.52 mmHg (18% from baseline) at 18 months (P= 0.001). Table 1 presents the mean decrease in IOP from baseline IOP.
Table 1.
The intraocular pressure reduction expressed as mean and percentage drop from baseline
We further compared the mean IOP for each group individually. Group I (primary treatment with no preoperative medications) had a preoperative mean IOP of 21.54 mmHg that decreased significantly to 17.4 mmHg (P<0.001). IOP decreased significantly in Group II (adjunctive treatment where patients had been using antiglaucoma medications) from 18.29 mmHg preoperatively to 14.89 mmHg by the end of the study (P=0.001). There was a comparable reduction in IOP in both groups using SLT. Figure 2 presents mean IOP changes in both groups over the study period.
Figure 2.
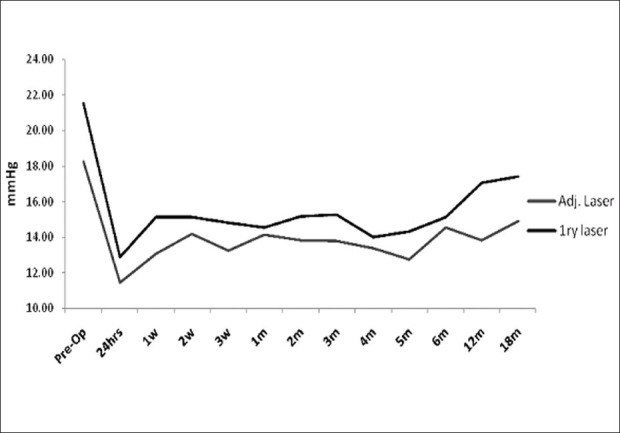
Mean intraocular pressure changes (mmHg) in both primary and adjunctive groups over the study period
Success was defined as IOP < 21 mmHg with at least a twenty percent drop of IOP from baseline and no secondary surgeries. At 1-month follow-up, treatment was successful in 73 eyes (69% of cases). Success remained similar at 18 months postoperatively with 74 eyes attaining the desired drop (70% of cases). Hence despite a mean drop of IOP of 18% at the end of follow-up, 70% of the patients met the success criteria.
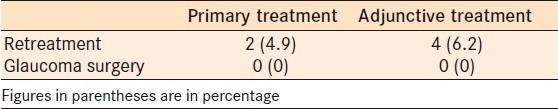
By the end of follow-up, six patients required laser retreatment and none needed any other surgical intervention to lower the IOP. Table 2 presents the type of intervention required in each group.
Table 2.
Number of patients with any intervention in each group
Number of medications used
Among patients using preoperative medications (group II), the mean number of medications used dropped statistically significantly throughout the study from 2.25 ± 0.97 before the procedure to 1.0 (±1.3) at the end of 18 months follow-up (P= 0.004). Figure 3 presents mean number of medications used throughout the study.
Figure 3.
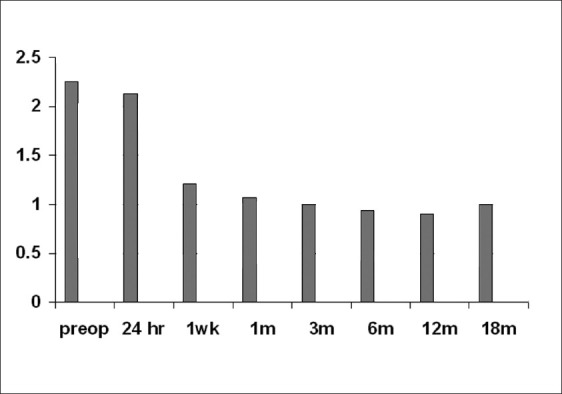
Mean number of medications used in the adjunctive group throughout the study
During the first 24 hours following the procedure, mild flare and cells were noted in the anterior chamber. This resolved spontaneously without treatment except in one case, which was successfully treated with topical steroids and resolved in 1 week.
Some patients reported ocular discomfort during the procedure (21 cases). We had five cases (4.7%) of increased IOP 1 week following the procedure, the increase in IOP ranged from 2 to 10 mmHg, only three eyes had an IOP spike of 5 mmHg or more.
DISCUSSION
Selective photothermolysis takes place when thermal damage is confined to the target, melanin, by using a specific laser wavelength with a laser exposure time (3 ns) equal to or shorter than the thermal relaxation time of melanin. Thus, pulsed lasers with low threshold radiant exposures can selectively target pigmented TM cells and avoid collateral thermal damage to adjacent non-pigmented cells.9 Histologically, SLT has not been reported to cause coagulative damage to the TM.7,8
The literature has reported variable rates of the short and long-term efficacy of SLT, with mean reductions in IOP ranging from 2 to 14 mmHg at 1 month postoperatively, 3–6 mmHg at 3 months postoperatively, and 5–7 mmHg at 6 months postoperatively.3,4,6,10,11 To our knowledge this is the first study to address the effect of this technique on Egyptian patients whether it was used alone or as an adjunct to medical therapy for glaucoma.
Our study shows SLT to be an effective procedure with continued average IOP lowering over 18 months consistent with the previous studies. Latina et al., studied 101 patients (45 patients on maximum antiglaucoma medication and 56 patients who had a previous failed ALT) treated by SLT.1 They1 found a 70% success rate based on a 3-mmHg (20%) or more reduction in IOP and no additional medication at 6 months after treatment. This outcome is very similar to our results of 69-70% of patients achieving 20% or more reduction in IOP. Latina et al.,1 reported the greatest reduction in IOP occurred on the first postoperative day (30.2%) and by 26 weeks, the average IOP reduction (in percent) from baseline for the entire cohort was 18.7% (4.6 mmHg). Nagar et al.,2 achieved a 20% reduction of IOP in 82% of their patients with 360° SLT and Mc Ilraith et al.,12 achieved similar results. These outcomes are comparable to our results of 38% at day one, 25% by 6 months and 18% at 18 months follow-up.
SLT proved effective for the primary treatment of POAG and ocular hypertention, with a mean drop of IOP of 30 % from baseline at 18 months postoperatively in Melamed et al.,3 study. Prasad et al.,13 achieved a 35% drop of IOP after 2 years of follow-up of primary cases of glaucoma treated with 360° SLT. These results are comparable to our findings in the primary treatment group which showed a mean drop of 19.2% at 18 months.
Saito et al.,14 found a significant drop in IOP in Japanese patients undergoing SLT as adjunctive treatment for POAG which tended to decrease with 1 year follow-up. In a different study on Chinese patients with maximally tolerated medical therapy for POAG, adjunctive SLT achieved IOP drop of 15% at 18-months follow-up.15 Our adjunctive group showed a comparable mean drop of 18.6% at 18 months. As with other studies, treatment failure occurred during the first month of follow-up and it remained the same throughout follow-up. The outcomes of our study do not indicate an advantage for SLT in one group over the other.
The number of medication used by patients dropped significantly in our study from 2.25 ± 0.97 before laser treatment to 1.00 ± 1.3 at the end of follow-up, these results are comparable to Francis et al.'s report,16 showing a decrease in the number of medications after SLT from 2.8 ± 1.1 to 1.5 ±0.9 at 12 months, postoperatively.
Adverse effects included ocular discomfort in 21 patients (19.8%), when the shots were closer to the ciliary body. The same observation was reported by Latina et al.,1 where pain and discomfort was reported in 15% of patients and redness in 9%. Nagar et al.,2 also reported transient pain and discomfort in 39% of patients undergoing 360° SLT. We did not encounter cases of iritis which could be explained by our routine use of pre- and postoperative steroids.
IOP spikes more than 5 mmHg were recorded in three patients (2.8%) in the current study. Reports of IOP spikes in the literature range widely from 0 to 27%,1,2,9 this can be explained by the use of different a preoperative regimen. Latina et al.,1 and Nagar et al.,2 did not premedicate with antiglaucoma drops and both reported IOP spike of 24% and 27%, respectively. However, Johnson et al.,9 (similar to us) used pre- and postoperative α-agonists to control IOP spikes reporting no IOP spikes in 136 eyes.
CONCLUSIONS
SLT is a safe alternative or adjuvant to medical treatment in cases of POAG. SLT addresses the problems of compliance in patients being a one-time procedure. It is repeatable with no damage to the ultrastructure of the trabecular meshwork. SLT was also effective in reducing the number of medications used by patients which is an economic advantage in developing countries. There is a tendency of the IOP lowering effect to wane over time hence, regular follow-up is required.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Latina MA, Sibayan SA, Shin DH, Noecker RJ, Marcellino G. Q-switched 532-nm Nd: YAG laser trabeculoplasty (selective laser trabeculoplasty): A multicenter, pilot, clinical study. Ophthalmology. 1998;105:2082–8. doi: 10.1016/S0161-6420(98)91129-0. discussion 2089-90. [DOI] [PubMed] [Google Scholar]
- 2.Nagar M, Ogunyomade A, O’Brart DP, Howes F, Marshall J. A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol. 2005;89:1413–7. doi: 10.1136/bjo.2004.052795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melamed S, Ben Simon GL, Levkovitch-Verbin H. Selective laser trabeculoplasty as primary treatment for open-angle glaucoma: A prospective, non-randomized pilot study. Arch Ophthalmol. 2003;121:957–60. doi: 10.1001/archopht.121.7.957. [DOI] [PubMed] [Google Scholar]
- 4.Kano K, Kuwayama Y, Mizoue S, Ito N. [Clinical results of selective laser trabeculoplasty] Nihon Ganka Gakkai Zasshi. 1999;103:612–6. [PubMed] [Google Scholar]
- 5.Cvenkel B. One-year follow-up of selective laser trabeculoplasty in open angle glaucoma. Ophthalmologica. 2004;218:20–5. doi: 10.1159/000074562. [DOI] [PubMed] [Google Scholar]
- 6.Damji KF, Shah KC, Rock WJ, Bains HS, Hodge WG. Selective laser trabeculoplasty v argon laser trabeculoplasty: A prospective randomized trial. Br J Ophthalmol. 1999;83:718–22. doi: 10.1136/bjo.83.6.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kramer TR, Noecker RJ. Comparison of the morphological changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology. 2001;108:773–9. doi: 10.1016/s0161-6420(00)00660-6. [DOI] [PubMed] [Google Scholar]
- 8.Cvenkel B, Hvala A, Drnovsek-Olup B, Gale N. Acute ultrastructural changes of the trabecular meshwork after selective laser trabeculoplasty and low power argon laser trabeculoplasty. Lasers Surg Med. 2003;33:204–8. doi: 10.1002/lsm.10203. [DOI] [PubMed] [Google Scholar]
- 9.Johnson PB, Katz LJ, Rhee DJ. Selective laser trabeculoplasty: Predictive value of early intraocular pressure measurements for success at 3 months. Br J Ophthalmol. 2006;90:741–3. doi: 10.1136/bjo.2005.086363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gracner T. Intraocular pressure response to selective laser trabeculoplasty in the treatment of primary open-angle glaucoma. Ophthalmologica. 2001;215:267. doi: 10.1159/000050872. [DOI] [PubMed] [Google Scholar]
- 11.Song J, Lee PP, Epstein DL, Stinnett SS, Herndon LW, Jr, Asrani SG, et al. High failure rate associated with 180 degrees selective laser trabeculoplasty. J Glaucoma. 2005;14:400–8. doi: 10.1097/01.ijg.0000176939.43681.c2. [DOI] [PubMed] [Google Scholar]
- 12.McIlraith I, Strasfeld M, Colev G, Hutnik CM. Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J Glaucoma. 2006;15:124–30. doi: 10.1097/00061198-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Prasad N, Murthy S, Dagianis JJ, Latina MA. A comparison of the intervisit intraocular pressure fluctuation after 180 and 360 degrees of selective laser trabeculoplasty (SLT) as a primary therapy in primary open angle glaucoma and ocular hypertension. J Glaucoma. 2009;18:157–60. doi: 10.1097/IJG.0b013e3181752c97. [DOI] [PubMed] [Google Scholar]
- 14.Saito Y, Higashide T, Sugiyama K. [Clinical results of selective laser trabeculoplasty as adjunctive treatment for primary open-angle glaucoma patients] Nihon Ganka Gakkai Zasshi. 2007;111:953–8. [PubMed] [Google Scholar]
- 15.Qian SH, Sun XH. [Selective laser trabeculoplasty in the treatment of primary open-angle glaucoma] Zhonghua Yi Xue Za Zhi. 2007;87:118–20. [PubMed] [Google Scholar]
- 16.Francis BA, Ianchulev T, Schofield JK, Minckler DS. Selective laser trabeculoplasty as a replacement for medical therapy in open angle glaucoma. Am J Ophthalmol. 2005;140:524–5. doi: 10.1016/j.ajo.2005.02.047. [DOI] [PubMed] [Google Scholar]


