Abstract
In this article, we report the spontaneous dissolution of a long cotton thread in the laser in situ keratomileusis (LASIK) flap interface. In this observational case report, sequential follow-up of a post-LASIK eye with a long cotton fiber noticed in the LASIK interface was performed. The postoperative course was uneventful, with no evidence of infection, uveitis, or any other complications. The cotton thread underwent spontaneous dissolution. Conservative management of a cotton fiber, not causing any symptoms and noticed after the immediate postoperative follow-up period is over, seems to be a possible alternative to flap relift and intervention.
Keywords: Fiber, Laser In Situ Keratomileusis Interface, Resolution
INTRODUCTION
A case report of a patient who presented with a cotton fiber in the flap interface after laser in situ keratomileusis (LASIK) is presented here. The patient was asymptomatic at presentation. Conservative management was chosen with careful observation, and topical antibiotics, topical steroid, and artificial tears until 1 month post-LASIK, and frequent follow-up till 1 year post-LASIK. The postoperative course was uneventful, with no evidence of infection, uveitis, or any other complications. The cotton thread slowly dissolved over the course of a year.
Careful observation with conservative management is an alternative to flap relift and irrigation in cases of embedded biomaterials such as a cotton fiber in the LASIK flap interface, if the patient is asymptomatic and there is no reaction in the cornea or anterior chamber.
The presence of interface debris has been commonly reported in eyes that have undergone LASIK.1–4 Generally, the debris consists of small metal or plastic fragments present at the interface. The management of these particles ranges from conservative observation to flap relift and irrigation to remove the foreign bodies. We present a case of conservative management of a cotton thread, which dissolved slowly over time. To the best of our knowledge, spontaneous dissolution of a large foreign body present at the LASIK interface has not been reported.
CASE REPORT
A 26-year-old female presented after LASIK for myopia performed elsewhere 10 days earlier. The medical records indicated a preoperative refractive error of –6 DS / –1 DCyl at 120° OD and –7 DS / –3 DCyl at 90° OS. LASIK was performed with a mechanical microkeratome. Ophthalmic history elicited that she was compliant to the topical medication regime, but did not present for postoperative follow-up at the center where LASIK was performed.
On evaluation (postoperative day 10), the patient had a uncorrected visual acuity (UCVA) of 20/20 OD, 20/20 OS, and was asymptomatic except for few areas of subconjunctival hemorrhage, which were resolving. The autorefraction was +0.125 DS / –0.12 DCyl at 115° OD and +0.125 DS OS. On slit-lamp evaluation, a long, cotton fiber was noticed in the intralamellar space, inferotemporal to the pupillary axis OS [Figure 1]. There was no evidence of any reaction or any other debris in the interface. We relayed our findings to the patient and offered a flap relift and irrigation. However, the patient refused any intervention due to the good vision. The patient was kept on frequent follow-up and was prescribed topical prednisolone acetate four times a day, topical ofloxacin twice a day, and preservative-free tear substitutes four times a day. The medications were tapered on subsequent follow-up by the end of 1 month. Between the first and third month follow-up, only artificial tears were prescribed. After the third month, all the topical medications were stopped. The patient was followed up for 1 year and there was no evidence of any reaction, loss of visual acuity, or evidence of infection at any visit. The fiber slowly dissolved from the second month onward [Figure 2]. It completely dissolved with mild pigmentation by the sixth month of follow-up [Figure 3]. Follow-up at 1 year post-LASIK was performed to rule out any late complications. At this visit, there was no evidence of broken or thinned out segments of the fiber even on very high magnification [Figure 4]. The autorefraction values were +0.125 DS / –0.12 D at 115° OD and +0.125 DS OS at 1 year postoperatively. During the entire follow-up period, the patient never developed any discomfort or any other symptoms due to the fiber.
Figure 1.
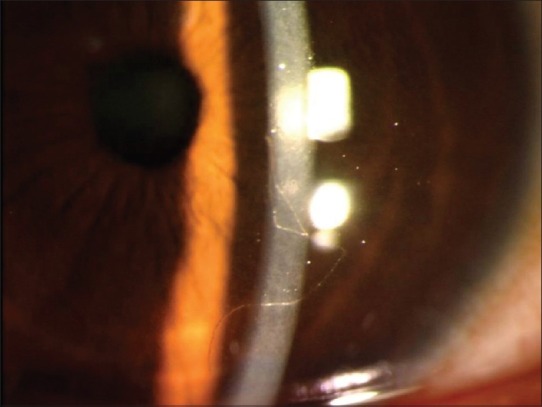
Presence of intralamellar cotton fiber 10 days after laser in situ keratomileusis
Figure 2.
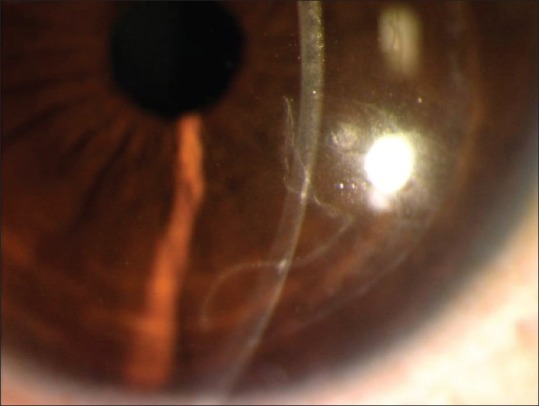
Partial dissolution of an intralamellar cotton fiber 2 months after laser in situ keratomileusis
Figure 3.
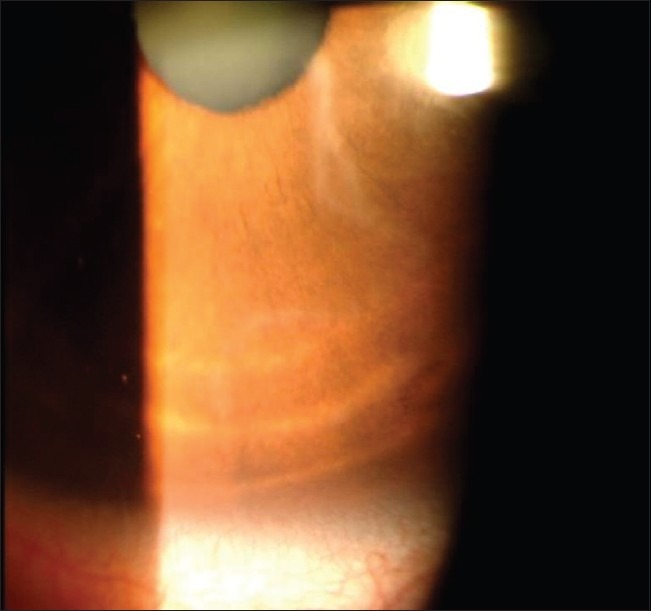
Totally dissolved intralamellar cotton fiber, with pigmentation and scarring in the area, 6 months after laser in situ keratomileusis
Figure 4.

High magnification (×40) image of the of the pigmentation, showing no evidence of a cotton fiber 1 year after laser in situ keratomileusis. The flap edge scar is visible inferiorly
DISCUSSION
Foreign bodies in the interface after LASIK are generally detected early and the management plan depends on the nature and reactivity to the foreign body, its size, and location, and the symptoms. A recent study suggested that microscopic plastic and metallic fragments are generated during microkeratome oscillation and are deposited at the interface.3 The authors noted unaltered persistence of these particles for at least 1 year.3 Larger particles of plastic have also been reported.1 As plastic and metal are not biodegradable, the decision to observe or remove is clinically tenuous at best.
As the fiber in our case was located away from the pupillary axis, the patient remained asymptomatic. Cotton is derived from plants and is therefore biodegradable. Thus, keratocytes could have disintegrated and dissolved it over time. The tissue response to the foreign body also plays an important role in the management plan. As there was no clinical evidence of significant inflammation, the role of conservative management was further justified. The corneal stroma around the thread showed mild scarring and pigmentation, which was not causing any symptoms or reduction in contrast sensitivity. We further recommend confocal microscopy, if available, for these cases to enhance the evaluation.
This case highlights the importance of conservative management and the possible outcome of cases with small organic foreign bodies in the LASIK interface that are not causing any signs or symptoms.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Eisemann J, Carkeet A, Swann PG. Large interface particles from LASIK surgery. Clin Exp Optom. 2006;89:253–6. doi: 10.1111/j.1444-0938.2006.00046.x. [DOI] [PubMed] [Google Scholar]
- 2.Crowther KS, Ellingham RB. Complicated removal of corneal foreign bodies 18 months after laser in situ keratomileusis. J Cataract Refract Surg. 2005;31:851–2. doi: 10.1016/j.jcrs.2004.10.054. [DOI] [PubMed] [Google Scholar]
- 3.Ivarsen A, Thogersen J, Keiding SR, Hjortdal JO, Moller-Pedersen T. Plastic particles at the LASIK interface. Ophthalmology. 2004;111:18–23. doi: 10.1016/j.ophtha.2003.05.021. [DOI] [PubMed] [Google Scholar]
- 4.Porges Y, Landau D, Douieb J, Levinger S. Removal of corneal foreign bodies following laser in situ keratomileusis. J Refract Surg. 2001;17:559–60. doi: 10.3928/1081-597X-20010901-10. [DOI] [PubMed] [Google Scholar]


