Abstract
Context:
Prophylactic antibiotics, paired with wound care and surgical intervention, is considered the standard of care for patients with open fracture. Guidelines from the Eastern Association for the Surgery of Trauma (EAST) recommend specific prophylactic antimicrobial therapy based on the type of open fracture.
Aims:
We quantified adherence to EAST guideline recommendations and documented the incidence of infection in patients with open fracture.
Settings and Design:
A retrospective, observational study of all patients with open fracture admitted to our facility from January 2004 to December 2008 was conducted.
Materials and Methods:
Patients were divided into compliant and noncompliant groups according to the EAST guideline recommendations. Compliance was defined as an appropriate spectrum of therapy for guideline suggested duration. We assessed for surgical and non-surgical site infections, and morbidity outcomes.
Statistical Analysis:
Nominal data were explored using summary measures. Continuous variables were compared using the Student t-test or the Mann–Whitney U-test. Dichotomous data were compared using χ2 statistic or Fisher's exact test.
Results:
The final analysis included 214 patients. Prophylactic antibiotics were guideline compliant in 28.5% of patients, and ranged from 10.0% in type 3b fractures to 52.7% in type 1 fractures. The most common reason for non-compliance was the use of guideline recommended coverage that exceeded the suggested duration (71.2%). Patients who received non-compliant therapy required prolonged hospital lengths of stay (6 vs. 3 days, P = 0.0001). The overall incidence of infection was similar regardless of guideline compliance (17.0% vs. 11.5%, P = 0.313).
Conclusions:
Prophylactic antibiotics for open fracture frequently exceeded guideline recommendations in duration and spectrum of coverage, especially in more severe fracture types. Non-compliance with EAST recommendations was associated with increased in-hospital morbidity.
Keywords: Clinical guidelines, Eastern Association for the Surgery of Trauma, open fracture, prophylactic antibiotics, wound
INTRODUCTION
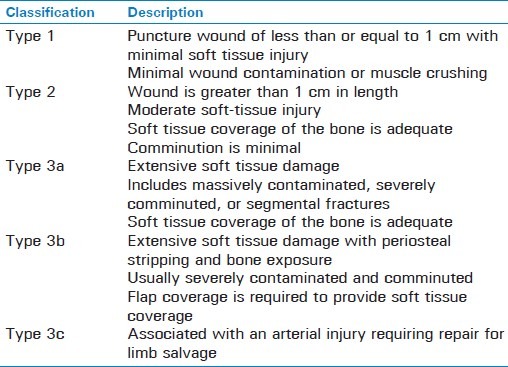
An open fracture is the one in which a wound through adjacent soft tissues allows communication between the site of the fracture and the outside environment.[1] Infection is the most common and serious complication after an open fracture, and can result in sepsis, loss of limb function, amputation or death.[1–8] Antibiotic therapy, in addition to proper wound care, is now the standard of care for all patients with open fractures.[1,5–9] In 1998, the Eastern Association for the Surgery of Trauma (EAST) practice management work group published practice guidelines addressing prophylactic antibiotics for the management of open fractures.[10] The guidelines recommend prophylactic antibiotic strategies based on the severity of the open fracture, as defined by the classification scheme described by Gustilo and Anderson [Table 1].[4]
Table 1.
Gustilo classification of open fractures[4]
Investigations into compliance with prophylactic antibiotic guidelines in a different traumatic injury were conducted by Delgado and colleagues.[11] Their study compared prophylactic antibiotic practice patterns for penetrating abdominal trauma to published EAST guideline recommendations, and found that only 22% of patients received prophylaxis in agreement with the guideline recommendations.[11] Patients not treated in accordance with the guidelines had an associated doubling of the overall infection incidence, despite receiving prolonged antibiotic courses.[11] Therefore, it is currently suspected that noncompliance with the EAST guidelines for open extremity fracture, specifically the extensions of the duration or spectrum of coverage, may result in poorer patient outcomes.
We hypothesized that prophylactic antibiotic therapy for open fractures would exceed the EAST guideline recommended duration, and this practice would be associated with increased incidence of infectious complications, and prolonged hospital length of stay (LOS).[12,13] The objectives of this study were to quantify our adherence to the EAST guideline recommendations, document the incidence of infection, and identify risk factors for infection.
MATERIALS AND METHODS
A retrospective cohort study of all patients, 18 years and older, with open fractures admitted to our university-affiliated, rural, level I trauma center from January 1, 2004 through December 31, 2008 was completed. Patients were identified from our trauma registry using International Classification of Diseases, Ninth Revision (ICD-9) codes for open or comminuted fractures. This study was developed and conducted in accordance with the STROBE statement for cohort studies.[14] Exclusion criteria included: death within 24 h of hospital admission, premorbid antibiotic use expected to be continued longer than 48–72 h, antibiotic courses extended past guideline recommendations due to a documented infection requiring treatment, finger amputation as the cause of open fracture, or if the fracture grading was not documented. The protocol was approved by the Committees on Human Research.
Age, gender, mechanism of injury, location and open fracture type, class of antibiotics received, use of concomitant aminoglycoside-impregnated polymethylmethacrylate beads, use of wound vacuum-assisted closure dressings, number of surgical procedures performed on the open fracture, time to definitive wound closure, occurrence and sites of infection, duration of mechanical ventilation, intensive care unit (ICU) LOS, hospital LOS, amputation status, and final disposition were obtained via a medical chart review by a single investigator (C.B.). The injury severity score (ISS) was calculated prospectively and values for each included patient were obtained from a query of the trauma registry.[15] In the event of multiple open fractures, guideline compliance was based on the most severe open fracture. Treatment was considered to be guideline compliant for type 1 and 2 fractures if an antibiotic with activity against gram-positive organisms was exclusively used for less than or equal to 24 h. Despite the coverage of some gram-negative organisms, we considered therapy with a first generation cephalosporin appropriate for type 1 and 2 therapy. Prophylactic antibiotics for type 3 fractures were considered guideline compliant if the fracture was treated with appropriate therapy for type 1 or 2 fracture with the addition of gram-negative organism coverage for 3 days, or up to 24 h after the time of definitive wound closure, whichever occurred first. Further coverage of anaerobic organisms must have been included if fecal or clostridial contamination was suspected.[10] The total duration of antibiotic use was not assessed once guideline recommended limits were surpassed due to the expected high frequency of discharge prescriptions for oral antibiotics and our inability to quantify the use and adherence after discharge. The spectrum of coverage (gram positive, gram negative, and/or anaerobic organisms) was considered when determining guideline compliance, not the specific choice of antimicrobial prescribed.
Infectious complications were documented and categorized as occurring at either the surgical or nonsurgical site. Surgical site infections (SSIs) were classified as cellulitis, osteomyelitis, or abscess. Nonsurgical site infections (NSSIs) were further categorized as bacteremia, pneumonia, Clostridium difficile infection, urinary tract infection, or other. These infectious complications were defined using Centers for Disease Control and Prevention criteria.[16] The 1998 EAST guideline was used as our reference to determine compliance because it was the only available guideline that encompassed the entire study time period.[10] At the time of our data analysis, the EAST practice management workgroup published an updated prophylactic antibiotic open fracture guideline; however, the update was only minimally different than the original guideline.[17]
STATISTICS
Nominal data, including demographics and predictors of infection, were explored using summary measures. Continuous variables, such as LOS and age, were compared using Student's t-test for normally distributed variables and the Mann–Whitney U test for variables that were not normally distributed. Dichotomous data were compared using the Pearson χ2 statistic or Fisher's exact test wherever appropriate. A P < 0.05 was considered statistically significant. All data management and statistical analysis were computed using Stata/MP, Version 11 (College Station, Texas).
RESULTS
During the 5-year study period, 5491 patients were admitted to our trauma service and 373 (6.8%) were identified as having an open or comminuted fracture. A total of 159 patients were excluded; 67 (42.1%) were admitted for treatment of closed fractures, 35 (22.0%) were admitted for finger amputation, 39 (24.5%) lacked documentation of fracture type, 13 (8.2%) survived less than 24 h, two (1.3%) were continued on previous antibiotics, two (1.3%) were transferred to another facility within 24 h, and one (0.6%) patient's chart was missing. The final analysis included 214 patients.
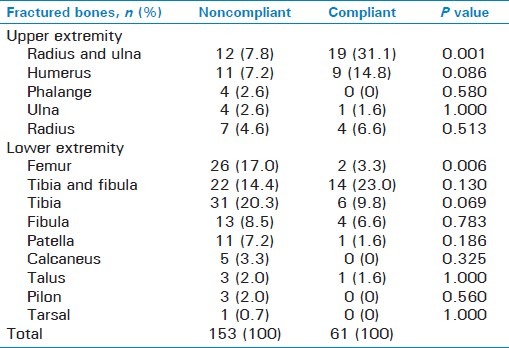
Prophylactic antibiotics were found to be compliant with the EAST guidelines in 61 (28.5%) patients. Compliance was highest in type 1 fractures (52.7%, n = 55) and lowest in type 3b fractures (10.0%, n = 20) [Figure 1]. Age, sex, ISS, and the presence of multiple fractures did not differ with respect to guideline compliance [Table 2]. Compliance was lower in patients who sustained an open fracture from motorcycle or motor vehicle collision as compared to those who sustained their injuries from falls (15.9 vs. 42.6%, P = 0.001). Patients in the compliant group were more likely to have unilateral radius and ulna fractures (7.8 vs. 31.1%, P = 0.001) and less likely to have femur fractures (3.3 vs. 17%, P = 0.006) [Table 3].
Figure 1.
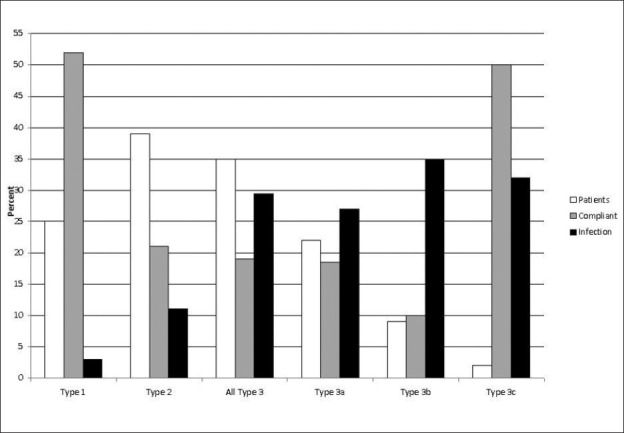
Compliant, antibiotics given in accordance with EAST guidelines
Table 2.
Baseline characteristics of included patients
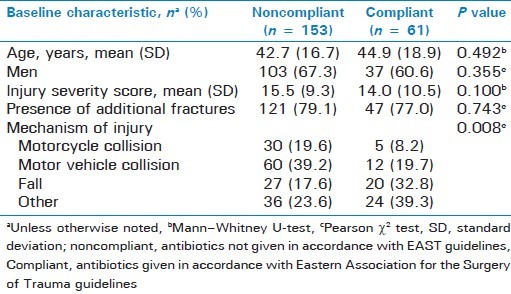
Table 3.
Summary of fractured bones by guideline compliance
The most frequent antibiotics administered were cefazolin (46.7%), followed by concomitant gentamicin and cefazolin (36.4%). Gentamicin was given to a total of 82 patients with 92.7% dosed using traditional methods and 7.3% using a once-daily regimen. The most common reason for noncompliance was use of guideline suggested coverage that extended past guideline suggested duration (71.2%), followed by coverage that exceeded guideline antibiotic choice and duration recommendations (19.6%). All patients received prophylactic antibiotics; therefore, lack of antibiotic utilization was not attributable to noncompliance.
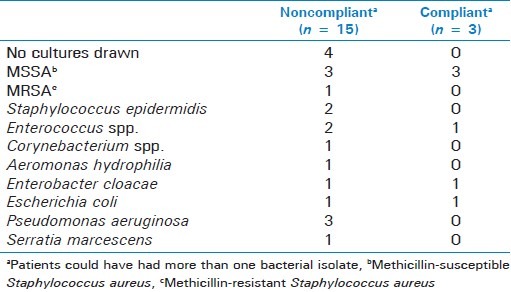
The SSI incidence was 0%, 3.6%, and 16%, for type 1, 2, and 3 fractures, respectively. The SSI incidence in any tibial fracture was 9.2%. The incidence of SSI was 4.9% in the compliant group compared to 9.8% in the noncompliant (P = 0.290). Osteomyelitis and/or abscess occurred in four patients. Staphylococcus aureus was the infecting pathogen in two cases of osteomyelitis, one in a type 3b fracture of the ulna and one in a type 2 fracture of the radius with a concomitant abscess. Staphylococcus epidermidis was documented in the third osteomyelitis case in a type 3a fracture of the tibia. Pseudomonas aeruginosa was cultured in the fourth case of a type 3a tibia fracture with a concomitant abscess. The microbiology of all SSIs by guideline compliance is shown in Table 4.
Table 4.
Microbiology of surgical site infections
The incidence of infection, SSI and NSSI, ranged from 3.6% in type 1 fractures to 35% in type 3b fractures [Figure 1], with an infection incidence of 15.4% for all fracture types. Overall infection occurrence [Figure 2] did not differ between patients who received guideline compliant therapy and those who did not (11.5% vs. 17.0%, P = 0.313). There was also no difference found in the incidence of SSI by guideline compliance when patients were grouped by fracture severity (i.e. type 1 and 2 or type 3) (P = 1.00). A regression model to assess independent risk factors for infection was unable to be performed due to the low incidence of infectious complications.
Figure 2.
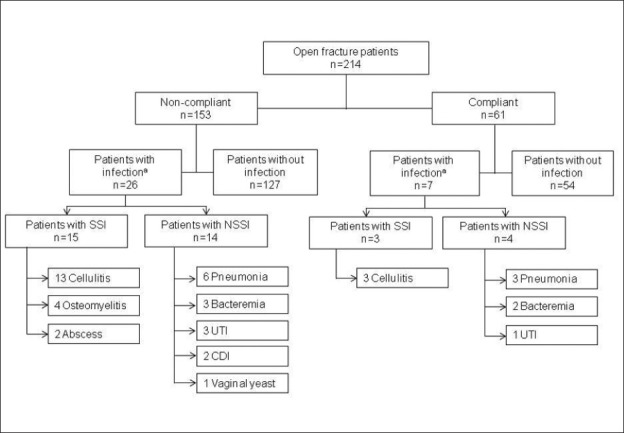
Compliant, antibiotics given in accordance with EAST guidelines. Noncompliant, antibiotics not given in accordance with EAST guidelines; SSI = Surgical site infection, NSSI = Nonsurgical site infection, UTI = Urinary tract infection, CDI = Clostridium difficile infection, aPatients could have had more than one infectious complicationw
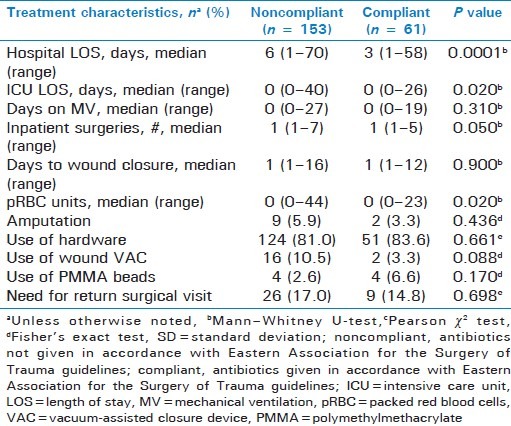
Noncompliance was associated with statistically significant increases in in-hospital morbidity including: ICU and hospital LOS, number of surgeries performed, and the number of units of packed red blood cells transfused [Table 5]. There were no differences in the incidence of amputation or use of implanted hardware between groups [Table 5].
Table 5.
Treatment characteristics and outcomes of included patients
DISCUSSION
Prophylactic antibiotic use in open fractures has been considered the standard of care since Patzakis and colleagues reported their trial results in 1974.[5] A cochrane review confirmed the utility of prophylactic antibiotics in this population by reducing overall infection rates by 59%.[6] The work of Patzakis et al. found patients who received a first-generation cephalosporin had fewer infectious complications compared to patients who received penicillin plus streptomycin (2.3% vs. 9.7%, P ≤ 0.05).[5] Nonetheless, gram-negative organisms are frequently isolated in deep-seeded infections, and thus broader coverage should be considered.[4,18] Patzakis and Wilkins published a review of various antibiotic regimens, and found the lowest incidence of infection in patients treated with cefamandole (a second generation cephalosporin) and tobramycin.[3] They concluded that severely contaminated wounds should be treated with broad spectrum antibiotics. Unfortunately, they did not correlate this recommendation with the Gustilo fracture classification.[3]
Fluoroquinolones, in particular ciprofloxacin, have been studied in this setting as they cover both gram-positive and gram-negative organisms and are less nephrotoxic than aminoglycosides. However, when studied prospectively, ciprofloxacin monotherapy was associated with a fourfold increased risk of infection in type 3 fractures.[19] Additionally, in the animal model, ciprofloxacin has been associated with poor fracture healing and exhibited dose-dependent cytotoxicity.[20,21] The incidence of infection has historically varied from 0 to 2%, 2 to 10% and 10 to 50% for type 1, 2 and 3 fractures, respectively, with tibial fractures expected to have twice the average incidence.[22,23] The incidence of SSI at our institution was within expected national estimates.
Controversy remains over the ideal prophylactic antibiotic regimen for prevention of deep-seeded infections in open fractures. Some have advocated covering all open fractures with a combination of a first-generation cephalosporin with an aminoglycoside, while others have advocated coverage of type 1 and 2 fractures with monotherapy using a first-generation cephalosporin with the addition of an aminoglycoside (typically gentamicin) for type 3 fractures.[10,22,24,25] The EAST guidelines reflect the latter recommendation.[10,17] There is a general consensus that anaerobic antimicrobial therapy should be included if contamination with these organisms is suspected.[10,22,25,26]
The optimal duration of antibiotic therapy is equally unclear. Some authors recommend a three day course of antibiotic therapy for all patients with open fractures, regardless of fracture type, while others recommend ending coverage within 24 h of wound closure.[1,10,26] Dellinger et al. found no difference in infectious complications when using a one-day course of antibiotics over a five-day regimen, independent of fracture type.[27] The EAST guidelines recommend no more than 24 h of coverage after definitive wound closure for type 1 and 2 fractures, and no more than 72 h of coverage for type 3 fractures.[10] However, there seems to be reluctance among many orthopedic surgeons to limit prophylaxis to the EAST guideline recommendations, especially in patients with type 3 fractures due to the perceived risk of infection.
The results of our analysis indicate that only 28.5% of patients received guideline compliant therapy, and that noncompliance was associated with increased ICU and hospital LOS and increased antibiotic utilization. The difference in ICU LOS does not appear to be clinically significant, and the hospital LOS difference may be attributable to the disparities in the mechanisms of injury. In addition, other patient factors that we did not investigate may have significantly influenced our results, and it is unlikely that noncompliance alone accounted for the increased LOS. The most common reason for noncompliance was the continuation of appropriate antimicrobial agent(s) beyond their recommended duration. It is possible that orthopedic surgeons at our institution believe that patients with extensive or severely contaminated wounds do not fit into EAST guideline recommendations. It is also plausible that our surgeons do not feel that the scientific evidence used in the creation of the EAST guidelines are clinically viable for application to all patients. In addition, the EAST guidelines do not offer specific suggestions regarding antimicrobial agent choice or dosing regimen. As a result, the misinterpretation of this guideline by providers could contribute to the lack of adherence. At our institution, orthopedic residents often prescribe the initial therapy, and inexperience may result in a lack of awareness of or adherence to guideline recommendations.
A potential limitation of this study is the retrospective design and the use of ICD-9 coding to identify patients. It is possible that some patients were inadvertently excluded using this method of identification.[11] Furthermore, inadequate follow-up care and/or inaccurate documentation may have led to decreased capture of infectious complications. Finally, this was a single center study in a rural population and the results may not be directly applicable to other institutions.
Our study is the first of its kind to gauge compliance with EAST guidelines for prophylactic antibiotics for open fracture, and to correlate guideline compliance with infectious complications. We found that infectious complications were not affected by guideline compliance. Nevertheless, our relatively small sample size may have had insufficient power to detect such differences. The majority of patients admitted to our institution with open fractures presented with type 1 or 2 fractures that likely could have been treated appropriately with guideline recommended therapy. Orthopedic surgeons at our facility were more likely to agree with the spectrum of antimicrobial coverage for type 1 fractures, but were much less likely to abide by the guideline recommended duration in more severe fracture types. Future research should be aimed at identifying optimal drug choices and dosing strategies to decrease infectious complications in patients with open fractures.
At our institution, prophylactic antibiotics for open fracture frequently exceeded guideline recommendations in the duration and spectrum of coverage, especially in more severe fracture types. We found that guideline nonadherence was associated with an increase in hospital LOS and increased antibiotic utilization. Further prospective, randomized trials of prophylactic antimicrobials in this patient population are warranted.
ACKNOWLEDGMENTS
The authors would like to thank Jennifer T. Gratton, RN, BSN, and Frances L. Martin for their help in data collection and Matthew E. Barton for his help with figure creation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Okike B, Bhattacharyya T. Trends in the management of open fractures: A critical analysis. J Bone Joint Surg Am. 2006;88-A:2739–48. doi: 10.2106/JBJS.F.00146. [DOI] [PubMed] [Google Scholar]
- 2.Patzakis MJ, Ivler D. Antibacterial and bacteriologic considerations in open fractures. South Med J. 1977;70:46–8. doi: 10.1097/00007611-197710001-00013. [DOI] [PubMed] [Google Scholar]
- 3.Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res. 1989;243:36–40. [PubMed] [Google Scholar]
- 4.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones. J Bone Joint Surg Am. 1976;58:453–8. [PubMed] [Google Scholar]
- 5.Patzakis MJ, Harvey JP, Jr, Ivler D. The role of antibiotics in the management of open fractures. J Bone Joint Surg Am. 1974;56:532–41. [PubMed] [Google Scholar]
- 6.Gosselin RA, Roberts I, Gillespie WJ. Antibiotics for preventing infection in open limb fractures. Cochrane Database Syst Rev. 2004;(1):CD003764. doi: 10.1002/14651858.CD003764.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Souza A, Rajagopalan N, Amaravati RS. The use of qualitative cultures for detecting infection in open tibial fractures. J Orthop Surg (Hong Kong) 2008;16:175–8. doi: 10.1177/230949900801600209. [DOI] [PubMed] [Google Scholar]
- 8.Patzakis MJ, Wilkins J, Moore TM. Use of antibiotics in open tibial fractures. Clin Orthop Relat Res. 1983;178:31–5. [PubMed] [Google Scholar]
- 9.Brown KV, Walker WA, Cortez DS, Murray CK, Wenke JC. Earlier debridement and antibiotic administration decrease infection. J Surg Orthop Adv. 2010;19:18–22. [PubMed] [Google Scholar]
- 10.Luchette FA, Bone LB, Born CT, DeLong WG, Hoff WS, Mullins D, et al. EAST practice management guidelines work group: Practice management guidelines for prophylactic antibiotic use in open fractures. [EAST website] 1998. [Last accessed on 2009 Jul 20]. Available from: http://www.east.org/tpg/archive/html/chap10body.html .
- 11.Delgado G, Barletta JF, Kanji S, Tyburski JG, Wilson RF, Devlin JW. Characteristics of prophylactic antibiotic strategies after penetrating abdominal trauma at a level I urban trauma center: A comparison with the EAST guidelines. J Trauma. 2002;53:673–8. doi: 10.1097/00005373-200210000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Velmahos GC, Toutouzas KG, Sarkisyan G, Chan LS, Jindal A, Karaiskakis M, et al. Severe trauma is not an excuse for prolonged antibiotic prophylaxis. Arch Surg. 2002;137:537–42. doi: 10.1001/archsurg.137.5.537. [DOI] [PubMed] [Google Scholar]
- 13.Hauser CJ, Adams CA, Eachempati SR. Surgical Infection Society Guideline: Prophylactic antibiotic use in open fractures: An evidence-based guideline. Surg Infect (Larchmt) 2006;7:379–405. doi: 10.1089/sur.2006.7.379. [DOI] [PubMed] [Google Scholar]
- 14.STROBE Statement. STROBE statement for cohort studies. [Last accessed on 2011 Oct 17]. Available from: http://www.strobe-statement.org/fileadmin/Strobe/uploads/checklists/STROBE_checklist_v4_cohort.pdf .
- 15.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. [PubMed] [Google Scholar]
- 16.Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TJ. CDC definitions of nosocomial surgical site infections, 1992: A modification of CDC definitions of surgical wound infections. Am J Infect Control. 1992;20:271–4. doi: 10.1016/s0196-6553(05)80201-9. [DOI] [PubMed] [Google Scholar]
- 17.Hoff WS, Bonadies JA, Cachecho R, Dorlac WC. East Practice Management Guidelines Work Group: Update to practice management guidelines for prophylactic antibiotic use in open fractures. J Trauma. 2011;70:751–4. doi: 10.1097/TA.0b013e31820930e5. [DOI] [PubMed] [Google Scholar]
- 18.Lee J. Efficacy of cultures in the management of open fractures. Clin Orthop Relat Res. 1997;339:71–5. doi: 10.1097/00003086-199706000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Patzakis MJ, Bains RS, Lee J, Shepard L, Singer G, Ressler R, et al. Prospective, randomized, double-blind study comparing single-agent antibiotic therapy, ciprofloxacin, to combination antibiotic therapy in open fracture wounds. J Orthop Trauma. 2000;14:529–33. doi: 10.1097/00005131-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Huddleston PM, Steckelberg JM, Hanssen AD, Rouse MS, Bolander ME, Patel R. Ciprofloxacin inhibition of experimental fracture healing. J Bone Joint Surg Am. 2000;82:161–73. doi: 10.2106/00004623-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Holtom PD, Pavkovic SA, Bravos PD, Patzakis MJ, Shepherd LE, Frenkel B. Inhibitory effects of the quinolone antibiotics trovafloxacin, ciprofloxacin, and levofloxacin on osteoblasic cells in vitro. J Orthop Res. 2000;18:721–7. doi: 10.1002/jor.1100180507. [DOI] [PubMed] [Google Scholar]
- 22.Zalavras CG, Marcus RE, Levin LS, Patzakis MJ. Management of open fractures and subsequent complications. J Bone Joint Surg Am. 2007;89:883–95. doi: 10.2106/00004623-200704000-00027. [DOI] [PubMed] [Google Scholar]
- 23.Singh D, Garg R, Bassi JL, Tripathi SK. Open grade III fractures of femoral shaft: Outcome after early reamed intramedullary nailing. Orthop Traumatol Surg Res. 2011;97:506–11. doi: 10.1016/j.otsr.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 24.Saveli CC, Belknap RW, Morgan SJ, Price CS. The role of prophylactic antibiotics in open fractures in an era of community acquired methicillin-resistant Staphylococcus aureus. Orthopedics. 2011;34:611–6. doi: 10.3928/01477447-20110627-25. quiz 617. [DOI] [PubMed] [Google Scholar]
- 25.Zalavras CG, Patzakis MJ, Holtom PD, Sherman R. Management of open fractures. Infect Dis Clin North Am. 2005;19:915–29. doi: 10.1016/j.idc.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Ojo OD, Oluwadiya KS, Ikem IC, Oginni LM, Ako-Nai AK, Daniel FV. Superficial swab cultures in open fracture management: Insights from a resource-poor setting. J Wound Care. 2010;19:432–5. doi: 10.12968/jowc.2010.19.10.79090. [DOI] [PubMed] [Google Scholar]
- 27.Dellinger EP, Caplan ES, Weaver LD, Wertz MJ, Droppert BM, Hoyt N, et al. Duration of preventative antibiotic administration for open extremity fractures. Arch Surg. 1988;123:333–9. doi: 10.1001/archsurg.1988.01400270067010. [DOI] [PubMed] [Google Scholar]


