Abstract
Linear IgA disease (LAD) is an acquired, autoimmune, subepidermal, blistering disease, characterized by linear deposition of IgA along the dermoepidermal junction on immunofluorescence. Some cases known as ‘mixed immunobullous disease’ show weak staining with other immune reactants like IgG, IgM or C3. We report a rare case of a child having typical manifestations of LAD (chronic bullous disease of childhood), but with IgG predominance rather than IgA. Obviously it is improper to term this as linear IgA disease. Such cases are reported in literature as variants of LAD, with a multitude of terms like mixed immune bullous disease, linear IgG / IgA disease, linear IgA / IgG disease, and so on. In view of the tremendous confusion that these multiple terms cause in the absence of any practical benefit, we propose that the broad term ‘chronic bullous disease of childhood’ be applied to all childhood cases, irrespective of the nature of the immune deposits.
Keywords: Chronic bullous disease of childhood, linear IgA disease, linear IgG / IgA disease, mixed immunobullous disease
Introduction
Linear IgA disease (LAD) is defined as an acquired, autoimmune, subepidermal, blistering disease of unknown etiology, characterized by linear deposition of IgA along the dermoepidermal junction on immunofluorescence.[1,2] The target antigens are BP 180 / collagen XVII and its shed ectodomain [97 kD], BP 230 or LAD285.[3] The disease occurs with slightly different clinical patterns in adults and children, and is also called ‘chronic bullous disease of childhood’ in the latter.[3] Until 1975, this entity was confused with bullous pemphigoid or dermatitis herpetiformis, especially in adults, due to the overlapping clinical features. The distinction between LAD and bullous Pemphigoid / dermatitis herpetiformis is mainly based on the characteristic linear deposition of IgA along the basement membrane zone on immunopathology in the former.[1] Some cases known as ‘mixed immunobullous disease’ show other immune reactants like IgG, IgM or C3, albeit with weaker staining.[2,4] However, there are very few reports of cases presenting with typical clinical manifestations of LAD, but showing a predominant deposition of IgG rather than IgA.[5] Obviously it is improper to term these as linear IgA disease. Whether to consider this as a distinct entity or a variant of bullous pemphigoid is controversial. Alternatively, these cases have been termed by some authors as ‘linear IgG / IgA disease’.[2,4] One such rare case of a child having typical manifestations of chronic bullous disease of childhood showing predominant deposition of IgG rather than IgA is reported here. Also, the discrepancy in the terminology of this uncommon entity is discussed.
Case History
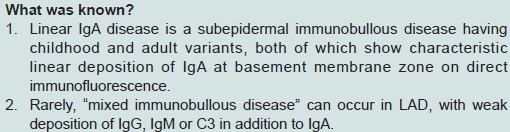
A five-year-old boy presented with recurrent, multiple, itchy, blisters all over the body since two months. The lesions burst open within two to three days, forming erosions with serous discharge and crusting, again followed by new blisters appearing around the healing erosion. There was no history of mucosal involvement, photosensitivity, prior drug intake, trauma, consanguinity or similar lesions in the family. A general physical and systemic examination was normal. On cutaneous examination, multiple grouped vesicles, bullae, and erosions were present all over the body, particularly more over the perioral, perineal, and lower trunk areas [Figure 1]. The palms, soles, external genitalia, and mucosae were spared. The characteristic annular arrangement of the vesicles / bullae around a crusted, erythematous plaque, described as ‘string of pearls sign’ or ‘cluster of jewels’, was seen in many sites [Figures 2 and 3].
Figure 1.

Multiple vesicles, bullae, and erosions present all over the body
Figure 2.

Characteristic annular arrangement of vesicles / bullae around a crusted, erythematous plaque, appearing as a ‘string of pearls’ or ‘cluster of jewels’
Figure 3.
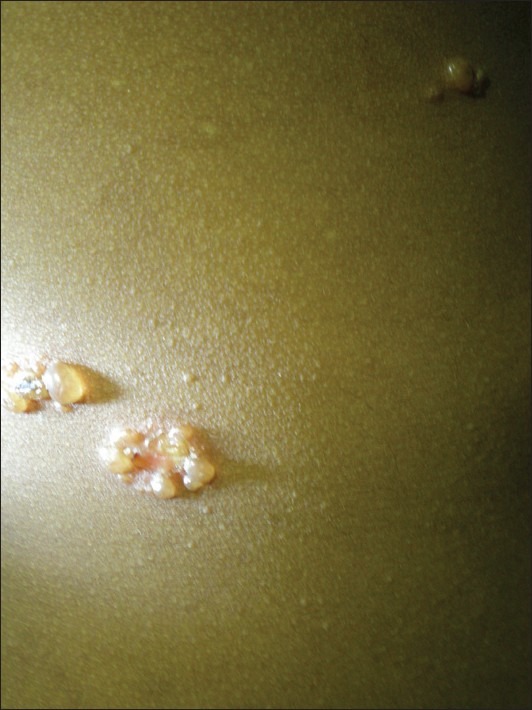
The ‘string of pearls’ or ‘cluster of jewels’ sign, pathognomonic of chronic bullous disease of childhood
Routine hematological and biochemical parameters, Gram stain, and Tzanck smear did not reveal any significant abnormality. Histopathology showed subepidermal bulla with predominantly neutrophilic infiltration within the bulla and the dermis [Figure 4]. Direct immunofluorescence of the perilesional skin revealed linear deposition of IgG [+++], IgA [++], and C3, along the basement membrane zone [Figure 5]. Based on the clinical, histopathological, and immunopathological features, a diagnosis of chronic bullous disease of childhood, but with IgG predominance was made.[3] Dapsone 25 mg / day (body weight was 15 kg)was given, apart from potassium permanganate compresses and symptomatic therapy.[3,4] The patient showed excellent response within 15 days, with minor and short lasting recurrences thereafter for a few months.
Figure 4.
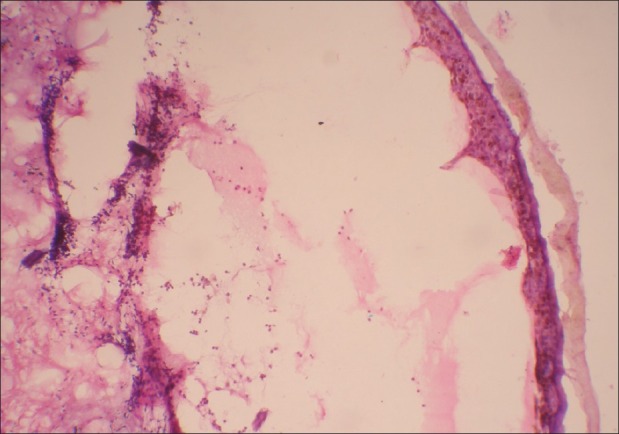
Subepidermal bulla with predominantly neutrophilic infiltration within the bulla and the dermis [H and E, 10×]
Figure 5.
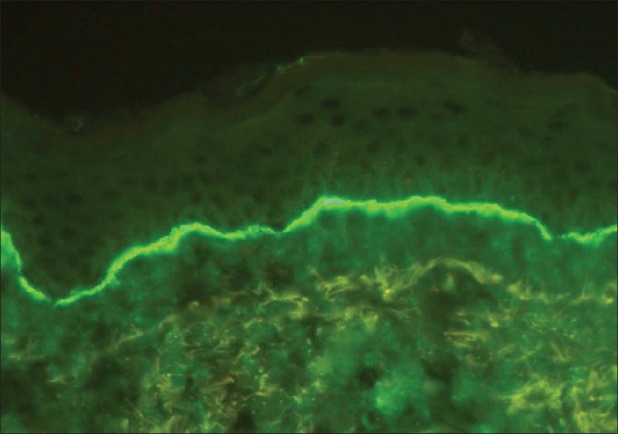
Linear deposition of IgG, IgA, and C3 along the dermoepidermal junction on direct immunofluorescence
Discussion
Linear IgA disease occurs in two different clinical patterns depending on the age of onset. In children, the onset is usually below five years of age. In adults, the peak age of onset is in the fifth decade.[6] The childhood disease (chronic bullous disease of childhood) manifests with an abrupt onset of itchy vesicles or large tense bullae. The annular arrangement of vesicles / bullae around a crusted, erythematous plaque, described as ‘string of pearls sign’ or ‘cluster of jewels sign’ is pathognomonic.[3] There is a predilection for perioral, perineal and lower trunk areas.[3] On the other hand, linear IgA disease of adults shows considerable variation in the morphology and distribution of the lesions. Scattered tense blisters resembling bullous pemphigoid are much more common than the cluster of jewels appearance. Perineal and perioral involvement is less common than in children.[6] Mucosal erosions or ulcers can occur in both the age groups. The childhood disease undergoes spontaneous remission in most cases by the age of six to eight years, whereas, the adult type is more protracted in nature.[3,6]
The current consensus is to consider both the childhood and adult cases with linear deposition of IgA at the basement membrane zone as age wise variants of a single entity termed, ‘Linear IgA disease’.[6] However, confusion arises when immune deposits other than IgA are predominant. Adult cases showing predominant IgG or C3 deposition are usually considered as bullous pemphigoid rather than LAD in view of the overlapping clinical features. However, in children, cases with IgG predominance cannot be included under bullous pemphigoid if the typical ‘string of pearls’ lesions are present. Hence, such cases are considered to be variants of LAD and recorded with a multitude of terms like mixed immune bullous disease, linear IgG / IgA disease, linear IgA / IgG disease, and so on.[2,4]
Powell et al. observed that irrespective of whether IgA or IgG is predominantly deposited, the clinical features, response to treatment with dapsone, and prognosis of the childhood disease remain the same.[7] This was true in the case described by us too, as the child had a typical ‘string of pearls’ sign and showed excellent recovery with dapsone, despite IgG predominance. Therefore, the classical cases with predominant IgA deposition (linear IgA disease) as well as mixed immune bullous disease (linear IgG / IgA disease or linear IgA / IgG disease) seem to be practically the same entity. The division of this clinically homogeneous entity into the classical form and variants, based on the immunopathology seems artificial, futile, and confusing. Considering all these factors, indiscriminate use of terms like linear IgA disease, linear IgA bullous dermatosis of childhood, mixed immune bullous disease, linear IgG / IgA disease, linear IgA / IgG disease, and so on, should best be avoided in childhood cases.[7,8] Hence, we propose that all cases showing the typical clinical picture of ‘cluster of jewels’ or ‘string of pearls’ sign should be included under the broad term ‘chronic bullous disease of childhood,’ irrespective of the nature of the immune deposits. By implication, probably the childhood disease is a separate entity with variable immune deposits, but with unique clinical features as the unifying factor, as opposed to the linear IgA disease of adults, where the clinical features are variable, but the linear deposition of predominantly IgA is an essential factor.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Wilson BD, Beutner EH, Kumar V, Chorzelski TP, Jablonska S. Linear IgA bullous dermatosis. An immunologically defined disease. Int J Dermatol. 1985;24:569–74. doi: 10.1111/j.1365-4362.1985.tb05853.x. [DOI] [PubMed] [Google Scholar]
- 2.Chan LS, Traczyk T, Taylor TB, Eramo LR, Woodley DT, Zone JJ. Linear IgA bullous dermatosis. Characterization of a subset of patients with concurrent IgA and IgG anti-basement membrane autoantibodies. Arch Dermatol. 1995;131:1432–7. doi: 10.1001/archderm.131.12.1432. [DOI] [PubMed] [Google Scholar]
- 3.Thappa DM, Jeevankumar B. Chronic bullous dermatosis of childhood. Postgrad Med J. 2003;79:437. doi: 10.1136/pmj.79.934.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheridan AT, Kirtschig G, Wojnarowska F. Mixed immunobullous disease: Is this linear IgA disease? Australas J Dermatol. 2000;41:219–21. doi: 10.1046/j.1440-0960.2000.00440.x. [DOI] [PubMed] [Google Scholar]
- 5.Petersen MJ, Gammon WR, Briggaman RA. A case of linear IgA disease presenting initially with IgG immune deposits. J Am Acad Dermatol. 1986;14:1014–9. doi: 10.1016/s0190-9622(86)70125-4. [DOI] [PubMed] [Google Scholar]
- 6.Wojnarowska F, Marsden RA, Bhogal B, Black MM. Chronic bullous disease of childhood, childhood cicatrical pemphigoid, and linear IgA disease of adults: A comparative study demonstrating clinical and immunological overlap. J Am Acad Dermatol. 1988;19:792–805. doi: 10.1016/s0190-9622(88)70236-4. [DOI] [PubMed] [Google Scholar]
- 7.Powell J, Kirtschig G, Allen J, Dean D, Wojnarowska F. Mixed immunobullous disease of childhood: A good response to antimicrobials. Br J Dermatol. 2001;144:769–74. doi: 10.1046/j.1365-2133.2001.04131.x. [DOI] [PubMed] [Google Scholar]
- 8.Madnani NA, Khan KJ. Linear IgA bullous dermatosis of childhood: Response to thalidomide. Indian J Dermatol Venereol Leprol. 2010;76:427–9. doi: 10.4103/0378-6323.66601. [DOI] [PubMed] [Google Scholar]


